FUTURE CARE CANTON HARBOR




Over 2 years since last inspection. Current conditions may differ from available data.
Future Care Canton Harbor in Baltimore, Maryland has a Trust Grade of C, which means it is average-neither great nor terrible compared to other facilities. It ranks #63 out of 219 in the state, placing it in the top half, and #5 out of 26 in the county, indicating that only four local options are better. The facility is improving, having reduced its issues from four in 2024 to three in 2025. Staffing is rated 4 out of 5 stars, but it has a turnover rate of 48%, which is around the state average, suggesting that while some staff stay, there is still room for improvement. There have been notable concerns, including a critical incident where a cognitively impaired resident was not protected from physical abuse by staff, leading to immediate action by the facility to correct this issue. Another finding showed that the facility did not adequately adjust care plans when residents' needs changed, which could lead to inadequate care. While the facility has some strengths, such as good quality measures and RN coverage, these incidents highlight significant weaknesses that families should consider.
- Trust Score
- C
- In Maryland
- #63/219
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 48% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $13,627 in fines. Lower than most Maryland facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 48 minutes of Registered Nurse (RN) attention daily — more than average for Maryland. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 58 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Near Maryland avg (46%)
Higher turnover may affect care consistency
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 58 deficiencies on record
Apr 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on complaint and reviews of a closed medical record, it was determined that the facility staff failed to follow a physicia...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on complaint, reviews of a closed medical record, reviews of the resident's electronic medical records, and interviews wit...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on complaints, reviews of active and closed medical records, reviews of the residents' electronic medical records, and int...
Read full inspector narrative →
Apr 2024
4 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, administrative record review, and staff interview; it was determined that the facility failed to...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, administrative record review, and staff interview; it was determined that the facility failed to...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on review of facility reported incident investigations and interview, it was determined the facility staff failed to thoroughly investigate allegations of abuse. This was evident for 1 (Resident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on tour, observation, and interview, it was determined that the facility failed to secure and monitor chemicals in an acti...
Read full inspector narrative →
Sept 2023
11 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
2) The surveyors reviewed the care plan for Resident # 146 on 9/12/23 at 11:44 AM. There was no intervention found in the care plan for combative behaviors.
The surveyors requested a care plan for co...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and medical record review it was determined that facility staff failed to provide an explanation in the resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on interviews and resident record reviews, it was determined that the facility failed to provide scheduled showers to residents. This was evident of 2 of 2 residents (Resident #398 and #108) rev...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, it was determined that the facility staff failed to ensure skin alterations were doc...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on interviews and record review, it was determined that the facility failed to provide respiratory care consistent with professional standards for oxygen administration. This was found evident o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined that the facility failed to administer pain medications consistent with professional standards. This was found evident of 1 of 5 (Resident # 41) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) On 9/6/23 at 11:20 AM, the surveyor observed a medication cart that was unattended and unlocked located on the first floor ha...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation and interview with facility staff, it was determined that the facility failed to ensure that infection control practices and guidelines were followed. This was found to be evident...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
Based on reviews of a Facility Reported Incident (FRI) and interviews, it was determined that the facility failed to thoroughly investigate allegations of abuse. This was evident for 6 (#4, #21, #57, ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation and interview with facility staff it was determined that the facility failed to serve food at appetizing temperatures. This was evident during 1 of 1 food test tray samples review...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations, interviews with facility staff and review of facility records it was determined that the facility failed to: 1) store food in accordance with professional standards for food ser...
Read full inspector narrative →
Feb 2019
33 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observationt it was determined that the facility staff failed to treat a resident with respect and dignity by standing to feed a resident and not being at eye level. This was evident for 1 (#...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on observation and interview with residents, it was determined that the facility failed to ensure that residents were treated with respect and dignity as evidenced by the failure of staff to kno...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with facility staff, it was determined that the facility staff failed to provide written notification of room/roommate change. This was evident for 1 (#437...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, it was determined that facility staff failed to assure that resident medical records remained private and confidential as evidenced by resident information being left visible on ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on review of resident and facility records and interviews with staff, it was determined that the facility staff failed to provide a safe resident environment free from abuse by failing to addres...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on review of resident and facility records and staff interviews, it was determined that the facility staff failed to immediately report allegations of abuse to the facility administrator and sta...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on review of resident and facility records and staff interviews, it was determined that the facility staff failed to investigate alleged abuse and prevent further potential abuse by failing to a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
3) On 2/1/19, review of Resident #130's medical record revealed the resident had been transferred to an acute care facility. On 1/27/19 at 4:00 PM, the nurse documented in a nursing home to hospital t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, family and staff interview and medical record review, it was determined that the facility staff failed to provide the appropriate care for activities of daily living to residents...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on review of residents' medical records and interview with facility staff, it was determined that the facility failed to ensure that a physician's order for twice-daily blood glucose checks was ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on resident and staff interview and medical record review, it was determined the facility failed to arrange follow-up consultation with eye care practitioner to ensure that the resident received...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, medical record review and staff interview, it was determined the facility failed to ensure a resident with urinary incontinence received the appropriate services to achieve or ma...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on review of the medical record and interview with staff, it was determined that the facility's consultant pharmacist failed to identify and report irregularities in the physicians orders during...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on review of the medical record and interview with staff, it was determined that the facility staff failed to ensure the residents drug regimen was free from unnecessary drugs. This was evident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interviews, it was determined that the facility staff failed to ensure that a resident's medication regimen was free from unnecessary psychotropic medication b...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observations of the facility's food service operations and staff interviews, it was determined that the facility failed to properly store an ice machine dispensing scoop and failed to utilize...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on review of the medical record and interview with staff, it was determined that the facility staff failed to maintain accurate medical records by failing to ensure a resident's smoking assessme...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
5) On 1/24/19 at 10:07 AM, an observation of the 300 Hall was completed. Surveyor noted that Resident # 388 was in bed. Behind the resident, (approximately 3 feet) a cord for the overhead light hung a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5) On 1/24/19 at 9:42 AM in room [ROOM NUMBER]-2, observation revealed that the laminate on the bedside table was noted to be fr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected multiple residents
Based on medical record review and staff interview, it was determined the facility staff failed to conduct an accurate, comprehensive assessment by failing to assess a resident's cognition and mood on...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
2) Review of the medical record for Resident #31 on 1/28/19 revealed that the facility failed to assess the resident's Cognition and Mood in Sections C and D on the quarterly MDS, with an assessment A...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5) On 2/1/19, review of Resident #25's December 2018 MAR (medication administration record) documented the resident received an ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected multiple residents
Based on record review, the facility failed to ensure that resident's pain was managed for 1 ( #131) of 3 residents reviewed for pain.
The findings include:
A record review for Resident #131, on 1/29...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0710
(Tag F0710)
Could have caused harm · This affected multiple residents
Based on medical record review and staff Interview, it was determined that the facility failed to ensure that a physician or nurse practitioner supervised the immediate care and needs for a resident w...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected multiple residents
#4) Record review on 1/30/19 at 10:48 AM, revealed that Resident #131's progress notes were not in the chart at the time of the physician visit. The physician encounter date on 11/3018 was not faxed t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation on [DATE] at 09:25 AM, it was determined the facility failed to properly store medications as evidenced by ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and staff interview, it was determined that the facility staff failed to follow infection control practices...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected most or all residents
12) During record review on 1/29/19 at 8:14 AM of the care plan for Resident #131, it was noted that the facility staff failed to capture strict spinal precautions. In an interview on 1/30/19 at 11:35...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected most or all residents
Based on observation and review of medical records, it was determined that the facility failed to perform appropriate revision to care plan goals and interventions as resident care needs became appare...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on staff interview, observations and review of the medical record, it was determined that the facility staff failed to have an effective quality assessment and assurance (QAA) program based on r...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Transfer Notice
(Tag F0623)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined the facility failed to notify the resident/resident repres...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0625
(Tag F0625)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview with facility staff, it was determined that the facility failed to provide notice o...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0655
(Tag F0655)
Minor procedural issue · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 9) In an interview on 1/28/19 at 11:02 AM, Resident #78 stated that a baseline care plan or medication list was not given, withi...
Read full inspector narrative →
Sept 2017
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0242
(Tag F0242)
Could have caused harm · This affected 1 resident
Based on review of medical record, interview of facility staff and resident interview, it was determined that the facility staff failed to honor the resident's right to have showers as often as she/he...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0272
(Tag F0272)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff, it was determined that the facility failed to accurately assess the resident's dental status on the Minimum Data Set assessment. This was found...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0329
(Tag F0329)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with the facility staff, it was determined that the facility failed to consistently monitor a resident's blood pressure prior to the administration of a me...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0241
(Tag F0241)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. An interview was conducted with Resident #95 on [DATE] at 1:10 pm. During the interview, Geriatric Nursing Assistant (GNA) #1...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0309
(Tag F0309)
Could have caused harm · This affected multiple residents
2. Review of Resident #306's medical record revealed admission physician's order dated September 14, 2017 for Trazodone 100 mg to be administered at bedtime for anxiety. Trazodone is an antidepressant...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0520
(Tag F0520)
Could have caused harm · This affected multiple residents
Based on review of facility documentation and interview with facility staff, it was determined that the facility failed to maintain a quality assessment and assurance (QAA) program that sufficiently d...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0356
(Tag F0356)
Minor procedural issue · This affected most or all residents
Based on observation and interview with facility staff, it was determined that the facility failed to post adequate information about nursing staff in a prominent place readily accessible to residents...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s). Review inspection reports carefully.
- • 58 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $13,627 in fines. Above average for Maryland. Some compliance problems on record.
- • Grade C (56/100). Below average facility with significant concerns.
About This Facility
What is Future Care Canton Harbor's CMS Rating?
CMS assigns FUTURE CARE CANTON HARBOR an overall rating of 4 out of 5 stars, which is considered above average nationally. Within Maryland, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Future Care Canton Harbor Staffed?
CMS rates FUTURE CARE CANTON HARBOR's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 48%, compared to the Maryland average of 46%.
What Have Inspectors Found at Future Care Canton Harbor?
State health inspectors documented 58 deficiencies at FUTURE CARE CANTON HARBOR during 2017 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 53 with potential for harm, and 4 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Future Care Canton Harbor?
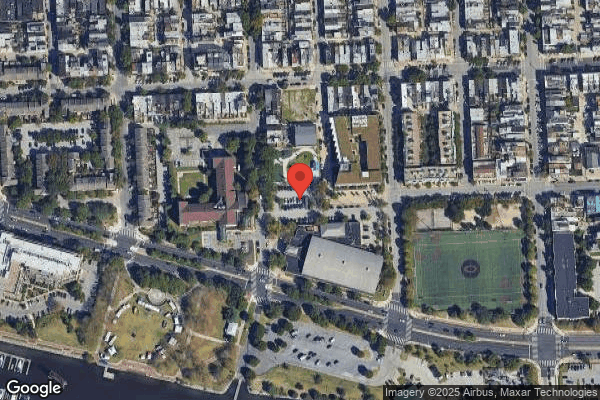
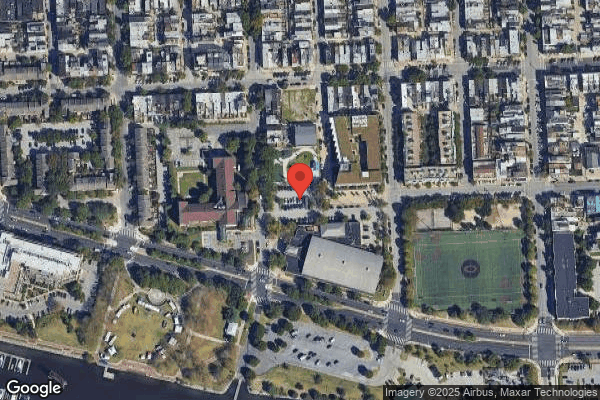
FUTURE CARE CANTON HARBOR is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by FUTURE CARE/LIFEBRIDGE HEALTH, a chain that manages multiple nursing homes. With 160 certified beds and approximately 149 residents (about 93% occupancy), it is a mid-sized facility located in BALTIMORE, Maryland.
How Does Future Care Canton Harbor Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, FUTURE CARE CANTON HARBOR's overall rating (4 stars) is above the state average of 3.0, staff turnover (48%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Future Care Canton Harbor?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Future Care Canton Harbor Safe?
Based on CMS inspection data, FUTURE CARE CANTON HARBOR has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 4-star overall rating and ranks #1 of 100 nursing homes in Maryland. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Future Care Canton Harbor Stick Around?
FUTURE CARE CANTON HARBOR has a staff turnover rate of 48%, which is about average for Maryland nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Future Care Canton Harbor Ever Fined?
FUTURE CARE CANTON HARBOR has been fined $13,627 across 1 penalty action. This is below the Maryland average of $33,215. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Future Care Canton Harbor on Any Federal Watch List?
FUTURE CARE CANTON HARBOR is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.