NORTHWEST HEALTHCARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Northwest Healthcare Center has received a Trust Grade of F, indicating significant concerns about the quality of care provided. They rank #120 out of 219 nursing homes in Maryland, placing them in the bottom half of facilities in the state, and #14 out of 26 in Baltimore City County, meaning only 13 local options are better. Unfortunately, the facility is worsening, with the number of issues increasing from 8 in 2019 to 13 in 2024. Staffing is a relative strength, with a 4 out of 5-star rating and a turnover rate of 38%, which is below the state average. However, there are troubling incidents, including a critical finding where a resident with high elopement risk was not adequately protected, and concerns regarding food safety practices that could potentially lead to food-borne illnesses.
- Trust Score
- F
- In Maryland
- #120/219
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ○ Average
- 38% turnover. Near Maryland's 48% average. Typical for the industry.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Maryland facilities.
- Skilled Nurses ○ Average
- Each resident gets 39 minutes of Registered Nurse (RN) attention daily — about average for Maryland. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 58 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (38%)
10 points below Maryland average of 48%
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Near Maryland average (3.0)
Meets federal standards, typical of most facilities
Near Maryland avg (46%)
Typical for the industry
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 58 deficiencies on record
Aug 2024
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, and policy review, the facility failed to ensure residents either had an advanced directive i...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined the facility staff failed to notify a resident representative of a resident-to-resident assault.
This was evident for 1 (#20) of 50 residents rev...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3.) Administrative record review of a facility investigation of alleged employee verbal abuse of a resident on 8/26/24 at 8:00 A...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview it was determined the facility staff 1) failed to report an incident of resident-to-residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4) Review of administrative records on 8/20/24 at 9:54 AM which revealed a facility reported incident (MD00196696) which alleged...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined the facility staff failed to provide written discharge/transfer notice to the resident and their representative. This was evident for 2 (#22 and ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined the facility staff failed to ensure residents were prepared and oriented to ensure safe and orderly transfer from the facility.This was evident f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to provide a comprehensive care plan for a resident (resident #902) with a history of substance use disorder. This was ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview with staff it was determined that the facility staff failed to review and revise resident c...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined the facility staff failed to develop and implement an effective discharge planning process which addressed each resident's dis...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to place a provider discharge summary on a resident's (resident #911 and #913) medical record after discharge. This was...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined the facility staff failed to maintain complete and accurate medical records by 1) failing to ensure X-Ray reports were filed in the medic...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, staff interviews, and policy review, the facility failed to ensure food was properly stored, prepared, distributed, and served in accordance with professional standards for food...
Read full inspector narrative →
Jun 2019
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on medical record review, interview and observation, it was determined the facility staff failed to promote care for residents in an environment that maintains or enhances each resident's dignit...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on a review of the facility's Beneficiary Protection Notifications and staff interview it was determined that the facility staff failed to ensure residents received a notification of an end to M...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility investigation, medical record review, and facility staff and resident interviews, it was determined that the f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on a review of the clinical records and staff interview it was determined that the facility staff failed to document the administered of pain medication and monitor the effectiveness. This was t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation of the facility's kitchen, it was determined that food service employees failed to ensure that sanitary practices were followed, and equipment was maintained in order to reduce th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor observation and resident interviews, it was determined that the facility failed to provide a safe, clean, comf...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
2) Observation of the medication carts and treatment carts on 06/24/19 at 08:38 AM revealed the following:
1. Artificial tears had no date to indicate when it was opened on Treatment Cart #1 on main h...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0923
(Tag F0923)
Minor procedural issue · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor observation, it was determined that the facility failed to have adequate ventilation to ensure good air circul...
Read full inspector narrative →
Mar 2018
37 deficiencies
1 IJ
CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
Based on observation, staff interviews, and review of medical records and other pertinent documentation, it was determined that the facility failed to maintain a safe environment for a resident with d...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on resident interviews, facility report review, and staff interviews it was determined that the facility staff failed to treat residents with respect and dignity while transporting residents. Th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected 1 resident
Based upon resident interviews, resident council record reviews, and facility staff interviews it was determined that the facility staff failed to put a system in place to ensure that resident council...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0577
(Tag F0577)
Could have caused harm · This affected 1 resident
Based on observation, resident and staff interview it was determined that the facility staff failed to provide easy access for residents to view the facility's survey reports, and post notice of avail...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined that the facility failed to ensure that a copy of the resident's advance directive was in the resident's medical record. This ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) On [DATE] Resident #239's medical records were reviewed. This review revealed that the resident was admitted to the facility ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on Beneficiary Protection Notification Review and interview with the facility staff, it was determined that the facility failed to document notification to a resident or representative (RP) rega...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on review of medical record, facility investigation and interviews it was determined that the facility failed to protect a resident from verbal abuse. This was found to be evident for one out of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on facility report review and interview with staff it was determined that the facility staff failed to report an alleged abuse related to misappropriation of resident property. This was evident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
2) Facility reported incident #MD00120040 was reviewed on 2/28/18. Upon review Resident #20 reported that a Geriatric Nurse Assistant (GNA-Staff #18) hit him/her two times in the mid-back. According t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined that the facility failed to have a system in place to ensure that residents or resident representatives were notified in writi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined that the facility failed to have a system in place to ensure that residents or resident representatives were given written not...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
3) Review on 2/28/18 at 1:56 PM of the admission MDS Assessment for Resident #81 with an assessment reference date of 1/18/18, revealed that Resident #81 did not have broken or cracked dentures. On 3/...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined that the facility staff failed to develop and implement care plans to address a resident's individualized needs that was identified...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined that the facility failed to have a system in place to provide the residents and their representatives with a summary of the baseline care...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on record review and staff interview it was determined that the facility staff failed to ensure that services being provided meet professional standards of quality by not following-up an un-witn...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with facility staff, it was determined that the facility failed to complete a discharge summary in a timely manner and failed to include a summary of the r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observations of residents, review of medical records and staff interview it was determined that the facility staff failed to ensure residents are provided with activities that meet the reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on medical record review and interview of facility staff it was determined the facility staff failed to promptly send a resident to the hospital following a head injury and failed to document a ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on medical record review and interview of facility staff it was determined the facility staff failed to ensure Resident #14 received appropriate care and services related to the administration o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review it was determined the facility staff failed to ensure appropriate care was provided to Resident #...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, medical record review and interview with staff it was determined that the facility failed to follow a physician order regarding the oxygen concentration level to be administered ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on review of employee education records on 3/7/18 at 8:31 AM, it was determined that the facility failed to perform competencies and perform skills check lists for nursing staff. This was eviden...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
3) Review of Resident #75's medical record on 3/7/18 at 9:34 AM revealed the resident was admitted in March 2017 and is currently on hospice. Resident #75 had a history of end stage renal disease, Maj...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0776
(Tag F0776)
Could have caused harm · This affected 1 resident
Based on medical records review and interview with staff it was determined that the facility failed to obtain a radiology test in a timely manner causing a potential delay in treatment. This was evide...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0777
(Tag F0777)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined that the facility staff failed to obtain diagnostic radiology services as ordered by the resident's physician. This was true for 1 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) Resident #81 was admitted to the facility 1/2018. On 2/27/18 at 8:12 AM an interview was conducted with the resident. S/He st...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation and staff interview it was determined that the facility staff failed to follow proper sanitation and food handling practices for the preparation, distribution and service of food ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected 1 resident
Based on review of the Facility Assessment and interview it was determined that the facility failed to address all of the required components of this regulation; specifically in regard to staff compet...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On [DATE] at 12:13 PM a record review for Resident #11 was conducted. Review of Nurse #23's progress notes indicated that the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0843
(Tag F0843)
Could have caused harm · This affected 1 resident
Based on review of pertinent documentation and interview with staff it was determined that the facility failed to have a transfer agreement with a local hospital. This was found to be evident during t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected 1 resident
Based on a review of the [NAME] report on 3/9/18 at 2:40 PM, the facility failed to implement appropriate action plans in order to correct repeat deficiencies. This was evident for 4 of 4 repeat defic...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 2/27/18 at 10:21 AM during observation of the Main Hallway Unit, surveyor noted a 4-plug access electrical socket box was ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2b) On 2/28/18 at 1:56 PM a medical record review was completed for Resident #81 for dental. There was no care plan for oral den...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review and interview with staff it was determined that the facility failed 1) to update and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation and staff interview it was determined that the facility staff failed to put a system in place to ensure that staff were appropriately trained and an ongoing system of surveillance...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Drug Regimen Review
(Tag F0756)
Minor procedural issue · This affected most or all residents
Based on review of the facility's Medication Monitoring and Management policy and interview with staff it was determined that the facility failed to have time frames for the different steps in the pro...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Maryland facilities.
- • 38% turnover. Below Maryland's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: Federal abuse finding, 1 life-threatening violation(s). Review inspection reports carefully.
- • 58 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • Grade F (33/100). Below average facility with significant concerns.
About This Facility
What is Northwest Healthcare Center's CMS Rating?
CMS assigns NORTHWEST HEALTHCARE CENTER an overall rating of 3 out of 5 stars, which is considered average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Northwest Healthcare Center Staffed?
CMS rates NORTHWEST HEALTHCARE CENTER's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 38%, compared to the Maryland average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Northwest Healthcare Center?
State health inspectors documented 58 deficiencies at NORTHWEST HEALTHCARE CENTER during 2018 to 2024. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 55 with potential for harm, and 2 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
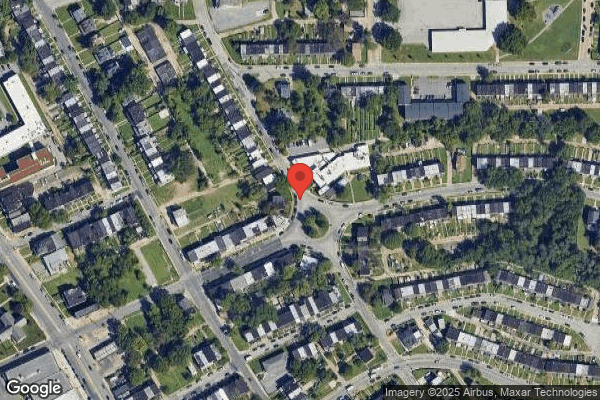
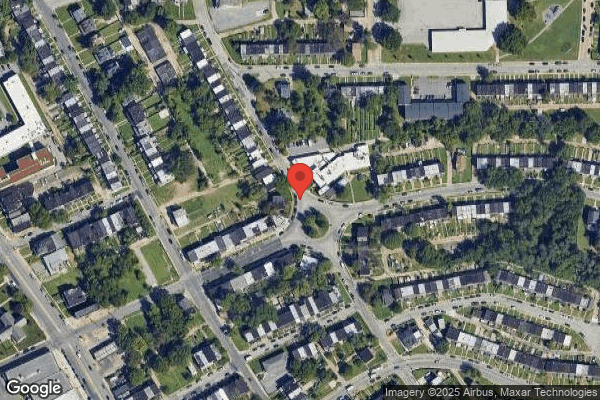
Who Owns and Operates Northwest Healthcare Center?
NORTHWEST HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by COMMUNICARE HEALTH, a chain that manages multiple nursing homes. With 91 certified beds and approximately 84 residents (about 92% occupancy), it is a smaller facility located in BALTIMORE, Maryland.
How Does Northwest Healthcare Center Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, NORTHWEST HEALTHCARE CENTER's overall rating (3 stars) is below the state average of 3.0, staff turnover (38%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Northwest Healthcare Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the substantiated abuse finding on record.
Is Northwest Healthcare Center Safe?
Based on CMS inspection data, NORTHWEST HEALTHCARE CENTER has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in Maryland. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Northwest Healthcare Center Stick Around?
NORTHWEST HEALTHCARE CENTER has a staff turnover rate of 38%, which is about average for Maryland nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Northwest Healthcare Center Ever Fined?
NORTHWEST HEALTHCARE CENTER has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Northwest Healthcare Center on Any Federal Watch List?
NORTHWEST HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.