WESTGATE HILLS REHAB & HEALTHCARE CTR



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Westgate Hills Rehab & Healthcare Center has a Trust Grade of C, which means it is average, placing it in the middle of the pack among nursing homes. It ranks #178 out of 219 facilities in Maryland, indicating it's in the bottom half of state options, and #21 out of 26 in Baltimore City County, suggesting there are better local choices. The facility's situation is worsening, with issues increasing from 17 in 2020 to 30 in 2025. Staffing is a concern; it received a 1-star rating and has a turnover rate of 54%, which is significantly higher than the state average of 40%. While the center has not incurred any fines, which is positive, there are notable incidents such as failure to report allegations of abuse in a timely manner and inaccuracies in resident assessments that could impact care quality. Overall, while there are some strengths, such as no fines and average RN coverage, the increasing issues and poor staffing ratings are significant weaknesses to consider.
- Trust Score
- C
- In Maryland
- #178/219
- Safety Record
- Low Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 54% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Maryland facilities.
- Skilled Nurses ○ Average
- Each resident gets 39 minutes of Registered Nurse (RN) attention daily — about average for Maryland. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 64 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Maryland average (3.0)
Below average - review inspection findings carefully
Near Maryland avg (46%)
Higher turnover may affect care consistency
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 64 deficiencies on record
Apr 2025
18 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and interviews, it was determined the facility failed to provide written notice with the reason for tran...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, and interviews it was determined the facility failed to provide the resident and/or Representati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on record review, and interviews, it was determined that the facility failed to accurately document assessments in a Resident's medical record. This was found evident of 2 (Resident #31 & #113) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, it was determined that the facility failed to inform residents of a summary of the residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review and interviews it was determined that the facility failed to develop a comprehensive person-centered care plan. This was found evident of 2 (Resident #101 & #99) out of 16 resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on record review, and interview it was determined that the facility failed to conduct care plan meetings after each resident assessment and failed to invite a resident to participate in their ca...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observation, medical record review and interview, it was determined that the facility failed to provide meaningful on-going personalized activities for the residents who were confined in thei...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on interviews and record review, it was determined that the facility failed to provide services to maintain a resident's vision. This was evident for 1 (Resident #66) out of 11 residents reviewe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interviews it was determined that the facility failed to provide treatment to prevent further decreased range of motion for a resident. This was found evident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observations, interviews with staff, and record review, it was determined that the facility failed to implement an intervention, determined to be necessary, for a resident who was identified ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected 1 resident
Based on record review and interviews it was determined that the facility failed to have the medical provider thoroughly review and accurately prescribe medications after a resident's readmission. Thi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews, it was determined that the facility failed to provide medication as ordered. This was evident for 1 (Resident #74) out of 5 residents reviewed for change...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review and interviews it was determined that the facility failed to have a process in place that ensured a resident's medication irregularity reports were reviewed by the primary care ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview, and medical record review, it was determined that the facility failed to have a documented condition that indicated the use of psychotropic medications for a resident . This was fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews with staff, it was determined that the facility failed to store medication in a locked comp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected 1 resident
Based on observation and interviews, it was determined that the facility failed to maintain the outdoor garbage storage area in a manner to prevent the harboring pests.
The findings include:
On 3/24/...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and staff interviews, it was determined that the facility failed to ensure that the residents' clean cloth...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations and interviews it was determined that the facility staff failed to properly store food in accordance with professional standards for food service and safety. This was found evide...
Read full inspector narrative →
Jan 2025
12 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on documentation review and interview it was determined the facility staff failed to promptly notify the physician of a resident's change in condition. This was evident for 1 (#61) of 63 residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on review of facility reported incidents with documentation review and interview, it was determined the facility failed to thoroughly investigate allegation of abuse for residents (Resident #1 a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, medical record review, and interviews, it was determined that the facility staff failed follow the care plan, and failed to evaluate and revise a resident's care plan to reflect ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on complaint, medical record review and interview, it was determined that the facility staff failed to provide needed activities of daily living for a resident dependent on assistance with care ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on review of complaint, medical record review, and staff interview, it was determined the facility failed to provide care to meet the needs of a resident's physical, mental, and psychosocial hea...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined the facility failed to provide timely treatment/services to prevent/heal pressures ulcers. This was evident for 1 (#31) of 31 resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, the facility staff failed to assess and evaluate the nutrition needs of residents ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interviews, it was determined that the facility staff failed to ensure that a resident's medication regimen was free from unnecessary medication. This was evid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0840
(Tag F0840)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, the facility staff failed to follow up with a consultant physician (Resident #22). This was evident for 1 of 63 residents reviewed during a complaint surv...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility staff failed to
keep complete and accurate medical records. This was evident for 2 (#1 and #50) of 50 residents...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
Based on review of facility reported incidents with documentation and interview, it was determined the facility failed to report 1) allegation of misappropriation of property, 2) an injury of unknown ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined the facility staff failed to ensure Minimum Data Set (MDS)...
Read full inspector narrative →
Feb 2020
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observations and interviews with facility staff it was determined the facility failed to ensure that a resident call light was accessible to him/her. This was found to be evident for 1 reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observations and interviews of facility staff it was determined the facility failed to ensure that residents reside in a clean, comfortable and homelike environment. This was in found to be e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on medical records review and interview with resident and staff it was determined that the facility failed to report allegations of abuse to the appropriate state agency. This was evident for 1 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interviews, it was determined that the facility staff failed to initiate a care plan to address a resident with contractures of the right and left knee. This w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with the facility staff it was determined that the facility failed to ensure Minimum Data Set (MDS) assessments accurately reflected the residents' status ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interviews, it was determined that the facility staff failed to initiate a care plan to address resident's contractures. This was evident for 1 of 8 residents ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on administrative review and interviews with the resident and facility staff it was determined the facility failed to follow the resident care plan and report when a resident was resistive to ca...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and staff interview it was determined that facility staff failed to administer the correct d...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with facility staff, it was determined that the dietitian failed to do timely assessments on residents with multiple comorbidities requiring monitoring. Th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on review of resident medical records and interview with facility staff, it was determined that the facility failed to ensure that a resident with as-needed pain medication regimens received pai...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on medical record review, facility competency training records and staff interview it was determined that the facility failed to ensure all licensed nursing staff had the specific competencies a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected 1 resident
Based on observations and interviews with facility staff it was determined the facility failed to have the assignment board that posts the staff assignments reflective of the actual staff working. Thi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on review of medical records and interview with staff it was determined that the facility failed to: 1.) ensure pharmacist recommendations resulting from identified irregularities during the mon...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. An observation was conducted on the Avalon unit on 2/23/20 at 6:07 AM and surveyors observed nightshift Nurse Supervisor RN #...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected 1 resident
Based on review of pertinent facility documents and interview with facility staff, it was determined that the facility failed to develop a facility assessment that included information related to staf...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. The facility staff failed to maintain a complete and accurate personal belongings inventory record for Resident #468.
A revi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and staff interviews, it was determined that the facility's staff failed to maintain a clean, safe and san...
Read full inspector narrative →
Aug 2018
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview it was determined the facility staff failed to ensure an advance directive was in p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined that the facility failed to have a system in place to ensure that the resident and resident's representative were notified in ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on review of medical record and staff interview, it was determined the facility staff failed to develop comprehensive care plan which addressed smoking for Resident (#42). This was evident for 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, the facility failed to obtain an ophthalmology consultation as ordered by the physician for Resident (#86). This is evident for 1 out of 33 residents sele...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, the facility staff failed to perform and/or document weekly skin assessments for a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, the facility failed to obtain a podiatry consultation as ordered by the physician for Resident (#86). This is evident for 1 out of 33 residents selected f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on record review, observation and interview, it was determined the facility staff failed to apply fall mats to both sides of the bed for Resident (# 86) as ordered. This was evident for 1 of 33 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record review, observation and interview, it was determined the facility staff failed to obtain a quantitative calorie count as ordered for Resident (#21) and provide 1:1 assistance and faile...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0742
(Tag F0742)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined the facility staff failed to obtain psychiatric consultations as ordered by the physician for residents # 13. This is evident for 1 out o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined the facility staff failed to attempt a Gradual Dose Reduction and failed to identify specific targeted behaviors to monitor and assess f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
Based on clinical record review and staff interview it was determined that the facility staff failed to ensure laboratory tests were obtained as ordered (# 18). This was true for 1 out of 33 residents...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
Based upon resident interview, staff interview and medical record review it was determined that facility staff failed to assist a resident in obtaining routine and emergency dental care. This was evid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review and interview the facility staff failed to provide specialized rehabilitation servic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on medical record review and interview and observation, it was determined the facility staff failed to maintain the medical record in the most accurate form as possible for Residents (# 21 and #...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
3. During interview with Resident #8 on 8/6/18 at 10:15 AM, the Resident stated he/she couldn't remember last time he/she had a care plan meeting. Review of the Resident's medical record on 8/8/18 rev...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
3. Review of Resident #13's medical record revealed the Resident was ordered by the physician on 5/23/18 for follow up appointment with Urology every 4 weeks. Further review of the medical record reve...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, it was determined the Consultant Pharmacist failed to identify and bring to the at...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • No fines on record. Clean compliance history, better than most Maryland facilities.
- • 64 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • Grade C (50/100). Below average facility with significant concerns.
About This Facility
What is Westgate Hills Rehab & Healthcare Ctr's CMS Rating?
CMS assigns WESTGATE HILLS REHAB & HEALTHCARE CTR an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Westgate Hills Rehab & Healthcare Ctr Staffed?
CMS rates WESTGATE HILLS REHAB & HEALTHCARE CTR's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 54%, compared to the Maryland average of 46%. RN turnover specifically is 61%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Westgate Hills Rehab & Healthcare Ctr?
State health inspectors documented 64 deficiencies at WESTGATE HILLS REHAB & HEALTHCARE CTR during 2018 to 2025. These included: 64 with potential for harm. While no single deficiency reached the most serious levels, the total volume warrants attention from prospective families.
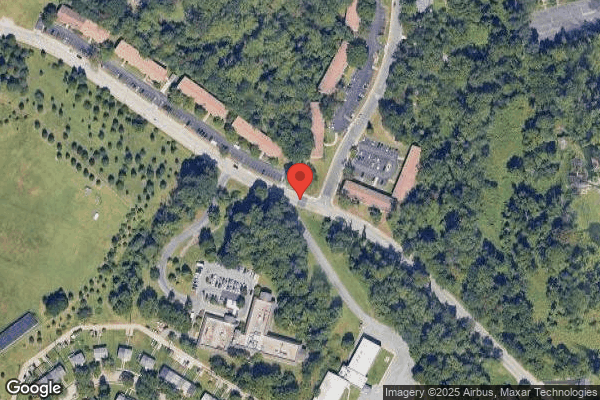
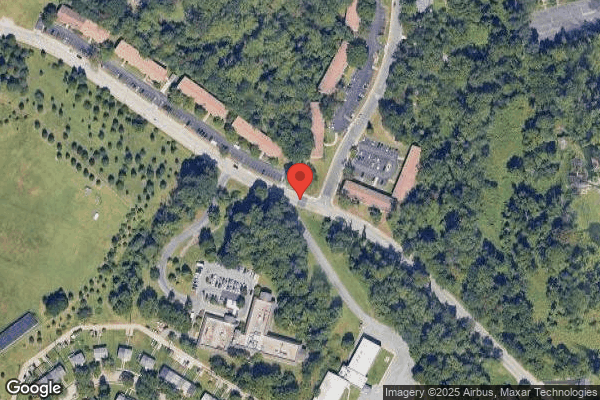
Who Owns and Operates Westgate Hills Rehab & Healthcare Ctr?
WESTGATE HILLS REHAB & HEALTHCARE CTR is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by MARQUIS HEALTH SERVICES, a chain that manages multiple nursing homes. With 120 certified beds and approximately 112 residents (about 93% occupancy), it is a mid-sized facility located in BALTIMORE, Maryland.
How Does Westgate Hills Rehab & Healthcare Ctr Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, WESTGATE HILLS REHAB & HEALTHCARE CTR's overall rating (2 stars) is below the state average of 3.0, staff turnover (54%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Westgate Hills Rehab & Healthcare Ctr?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Westgate Hills Rehab & Healthcare Ctr Safe?
Based on CMS inspection data, WESTGATE HILLS REHAB & HEALTHCARE CTR has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Maryland. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Westgate Hills Rehab & Healthcare Ctr Stick Around?
WESTGATE HILLS REHAB & HEALTHCARE CTR has a staff turnover rate of 54%, which is 8 percentage points above the Maryland average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Westgate Hills Rehab & Healthcare Ctr Ever Fined?
WESTGATE HILLS REHAB & HEALTHCARE CTR has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Westgate Hills Rehab & Healthcare Ctr on Any Federal Watch List?
WESTGATE HILLS REHAB & HEALTHCARE CTR is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.