CHESTERTOWN NURSING AND REHAB




Over 2 years since last inspection. Current conditions may differ from available data.
Chestertown Nursing and Rehab has received a Trust Grade of F, indicating poor performance with significant concerns about the facility's quality of care. Ranking #192 out of 219 facilities in Maryland places it in the bottom half, and it is the third choice out of three in Kent County, meaning only one local option is better. Although the facility’s trend is improving, with issues decreasing from 29 in 2023 to 6 in 2025, there are still serious concerns. Staffing is a weakness, with a low rating of 1 out of 5 stars and a turnover rate of 54%, which is higher than the state average. Specific incidents include a lack of hot water for several days impacting residents' hygiene and a failure to ensure that nearly two-thirds of residents had working phones in their rooms. On a positive note, the facility has average RN coverage, which can help catch potential problems. However, the overall environment and management practices need significant improvement.
- Trust Score
- F
- In Maryland
- #192/219
- Safety Record
- Low Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 54% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $3,418 in fines. Higher than 70% of Maryland facilities. Some compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 36 minutes of Registered Nurse (RN) attention daily — about average for Maryland. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 54 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Maryland average (3.0)
Significant quality concerns identified by CMS
Near Maryland avg (46%)
Higher turnover may affect care consistency
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 54 deficiencies on record
Aug 2025
6 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Number of residents sampled:
Number of residents cited:
Based on record review and interview, it was determined that the facility failed to ensure that a resident was free from abuse. This was evident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Number of residents sampled:
Number of residents cited:
Based on record review and interview, it was determined that the facility failed to report an allegation of abuse within two hours. This was evi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Number of residents sampled:
Number of residents cited:
Based on record reviews and interviews, it was determined that facility staff failed to ensure a thorough investigation was conducted for an all...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview with facility staff, it was determined that the facility failed to 1) initiate a care plan ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on review of a facility reported incident , record reviews and staff interviews, it was determined that the facility failed to 1) revise a care plan to accommodate the need after medication was ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0691
(Tag F0691)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on the review of Complaint Number 310737, medical records, and interviews with facility staff, it was determined that the ...
Read full inspector narrative →
Sept 2023
29 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on resident interview and observation it was determined the facility staff failed to treat residents with respect and dignity. This was evident for 4 (#16, #48 #75, #228) of 24 residents reviewe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview it was determined that the facility failed to provide written notice to a resident prior to c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected 1 resident
Based on observation, staff, resident interview and review of facility policy and procedure it was determined the facility failed to provide the ability for Resident (#58) to have access to his/her pe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0576
(Tag F0576)
Could have caused harm · This affected 1 resident
Based on observations and interviews with the resident and facility staff it was determined the facility staff failed to ensure that the resident right to privacy was maintained by delivering mail uno...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined the facility failed to give Resident #49 at least 48 hours' notice before the end of his/her Medicare covered Part A facility stay. This was evid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on administrative record review and interviews with facility staff it was determined the facility failed to keep a resident safe from verbal abuse. This was found to be evident for 1 (Resident #...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on observations, interviews with the resident family and facility staff, it was determined the facility failed to report allegations of abuse immediately to the state agency. This was found to b...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on record reviews and interviews it was determined the facility failed to complete a thorough investigation of an alleged employee to resident verbal and physical abuse incident and failed to re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined the facility failed to notify the resident/resident representative in writing of the bed hold policy when the resident was transfer...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on record review and interviews it was determined that the facility failed to have Quarterly care plan meetings as required for resident (#52) and failed to update the resident care plan to incl...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on the medical record review and staff interview it was determined the facility failed to ensure that medication was administered to a resident within a timeframe of professional standards of pr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, interviews with family, observations, interviews with facility staff and a review of facility vi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined that the facility failed to have an effective system in place to ensure communication of assessment information was conveyed between the ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews it was determined that the facility failed to ensure staffing information was complete and ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on a review of the medical record and interviews with facility staff it was determined that the facility failed to respond to the pharmacy recommendations after a monthly clinical review was don...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews it was determined that the facility physician prescribed an antibiotic to a resident without adequate indication of use. This deficient practice was evide...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews with facility staff, it was determined the facility failed to keep a resident free from unnecessary psychotropic medications. This was found to be evident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on medication administration observation, medical record review, and staff interview, it was determined the facility staff failed to ensure a medication error rate of less than 5%. This was evid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on record review and staff interview it was determined the facility failed to secure a narcotic medication and limit access to unauthorized persons. This was evident for 1 resident (#329) out of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected 1 resident
Based on observations and administrative record reviews and interviews with facility staff it was determined the facility failed to ensure that the Dietary Manager License was active and not expired. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
Based on observations and interviews with facility staff it was determined the facility failed to ensure that menus were being followed when preparing food for the residents. This was found to be evid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interviews it was determined that the facility staff failed to: 1.) document the temper...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation and staff interview it was determined that the facility failed to correctly store clean personal protective equipment for resident's rooms (#109, #404) to prevent infection and fa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined that the facility failed to offer all residents the opportunity to receive the pneumococcal vaccines. This deficient practice was evident...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
2.) On 09/10/23 at 9:58 am during observation rounds, the surveyor asked Resident #228 if he/she had a phone in the room. Resident #228 verbalized only having a personal cell phone.
On 09/28/23 at 2:...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected multiple residents
Based on observation, medical record review and staff interview it was determined the facility failed to ensure a resident was free of significant medication error as evidenced by failure of the nurse...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews with facility staff it was determined the facility failed to document adequately on the dis...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on record review and staff interview it was determined that the facility staff failed to develop and implement policies and procedures for a Quality Assurance Performance Improvement (QAPI) prog...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, records reviews, and staff interviews, the facility failed to provide and maintain a clean, co...
Read full inspector narrative →
Feb 2019
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
2)
The facility's admission record face sheet is a document that provides the facility staff with contact information about who to contact in the event of any change in physical or mental conditions ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) On [DATE] at 8:15 AM a closed record review was conducted. Resident # 71was admitted to the facility in [DATE]. She had a dia...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on the medical record and staff interviews, the facility staff failed to provide necessary written notices for Resident #54, or the Resident's responsible party, of a transfer out of the facilit...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on the medical record and staff interviews, the facility staff failed to provide the required written notice to Resident #54, or the resident's responsible party, of the bed hold policy during a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on record review and interview with staff the facility failed to implement a baseline care plan for Resident #221. This was evident for 1 out of 29 residents.
The findings include:
Resident #221...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on medical record review and resident and staff interview it was determined that the facility failed to develop a care plan for pain management for Resident #52. This was evident for 1 of 29 res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2)
02/14/19 11:01 AM Resident # 221 was admitted to the facility on [DATE] for rehabilitation after suffering a broken right an...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation and staff interviews it was determined that the facility failed to ensure that: 1) An accurate refrigerator temperature log was kept in the month of January 2019. 2) Facility staf...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined that the facility staff failed to keep a complete and accurate medical record. Specifically, the facility failed to document a resi...
Read full inspector narrative →
Oct 2017
10 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0155
(Tag F0155)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined that the facility staff failed to have a system in place t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0156
(Tag F0156)
Could have caused harm · This affected 1 resident
Based on medical record documentation review and staff interview, it was determined that the facility staff failed to notify the resident's responsible party of their rights regarding a pending discha...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0225
(Tag F0225)
Could have caused harm · This affected 1 resident
Based on review of medical record and interview with facility staff, it was determined that the facility staff failed to fully investigate a fall for Resident #53, as evidenced by the report being una...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0278
(Tag F0278)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility staff failed to ensure that the information used to complete the Minimum Data Set (MDS) comprehensive assessment...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0279
(Tag F0279)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined the facility staff failed to: 1) develop and implement a care plan based on a comprehensive assessment that addressed Resident #91...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0309
(Tag F0309)
Could have caused harm · This affected 1 resident
3) The facility staff failed to clarify a physician's order for Novolog (insulin) for Resident #59.
Review of Resident #59's medical record, revealed a physician's order for Novolog written upon resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0329
(Tag F0329)
Could have caused harm · This affected 1 resident
The facility staff failed to provide an indication for the use of Ritalin for Resident #67.
The findings include:
2) During a review of Resident #67's medical record that took place on 10/17/2017 at...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0272
(Tag F0272)
Could have caused harm · This affected multiple residents
Based on medical record documentation review and staff interview, it was determined that the facility staff failed to ensure that the Comprehensive or Annual Minimum Data Set (MDS) assessment and Quar...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0323
(Tag F0323)
Could have caused harm · This affected multiple residents
Based on observation, medical record documentation review and interview with the facility staff, it was determined that the facility staff failed to ensure that the residents' environment remained as ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0514
(Tag F0514)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) The facility staff failed to have complete and accurate documentation in the medical record for Residents #46 and #64.
Revie...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • $3,418 in fines. Lower than most Maryland facilities. Relatively clean record.
- • 54 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • Grade F (38/100). Below average facility with significant concerns.
About This Facility
What is Chestertown Nursing And Rehab's CMS Rating?
CMS assigns CHESTERTOWN NURSING AND REHAB an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Chestertown Nursing And Rehab Staffed?
CMS rates CHESTERTOWN NURSING AND REHAB's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 54%, compared to the Maryland average of 46%. RN turnover specifically is 75%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Chestertown Nursing And Rehab?
State health inspectors documented 54 deficiencies at CHESTERTOWN NURSING AND REHAB during 2017 to 2025. These included: 54 with potential for harm. While no single deficiency reached the most serious levels, the total volume warrants attention from prospective families.
Who Owns and Operates Chestertown Nursing And Rehab?
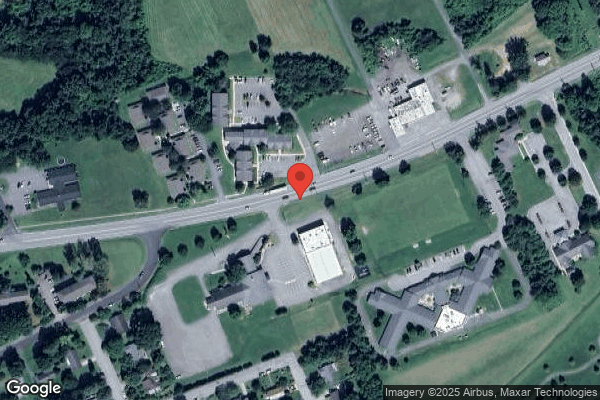
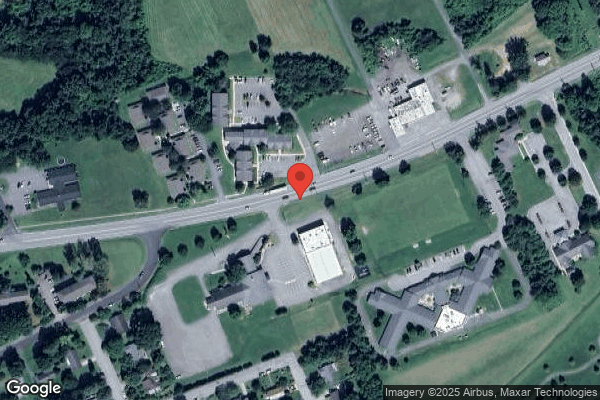
CHESTERTOWN NURSING AND REHAB is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by KEY HEALTH MANAGEMENT, a chain that manages multiple nursing homes. With 92 certified beds and approximately 85 residents (about 92% occupancy), it is a smaller facility located in CHESTERTOWN, Maryland.
How Does Chestertown Nursing And Rehab Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, CHESTERTOWN NURSING AND REHAB's overall rating (1 stars) is below the state average of 3.0, staff turnover (54%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Chestertown Nursing And Rehab?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Chestertown Nursing And Rehab Safe?
Based on CMS inspection data, CHESTERTOWN NURSING AND REHAB has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Maryland. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Chestertown Nursing And Rehab Stick Around?
CHESTERTOWN NURSING AND REHAB has a staff turnover rate of 54%, which is 8 percentage points above the Maryland average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Chestertown Nursing And Rehab Ever Fined?
CHESTERTOWN NURSING AND REHAB has been fined $3,418 across 1 penalty action. This is below the Maryland average of $33,113. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Chestertown Nursing And Rehab on Any Federal Watch List?
CHESTERTOWN NURSING AND REHAB is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.