LIONS REHAB CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Lions Rehab Center in Cumberland, Maryland has a Trust Grade of F, indicating poor performance with significant concerns. It ranks #208 out of 219 facilities in the state, placing it in the bottom half, and #7 out of 8 in Allegany County, with only one facility performing worse locally. The facility is experiencing a worsening trend, increasing from 32 issues in 2023 to 38 in 2025. While staffing is a relative strength with a 3 out of 5 rating and 0% turnover, the facility has concerning fines totaling $98,631, which is higher than 93% of Maryland facilities. Specific incidents include a resident developing a serious stage 4 pressure ulcer due to inadequate care and the failure to monitor dishwasher and food temperatures, raising sanitation concerns. Overall, while there are some strengths in staffing, the facility has serious weaknesses that families should carefully consider.
- Trust Score
- F
- In Maryland
- #208/219
- Safety Record
- Moderate
- Inspections
- Getting Worse
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ✓ Good
- $98,631 in fines. Lower than most Maryland facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 48 minutes of Registered Nurse (RN) attention daily — more than average for Maryland. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 92 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Maryland average (3.0)
Significant quality concerns identified by CMS
Well above median ($33,413)
Moderate penalties - review what triggered them
The Ugly 92 deficiencies on record
May 2025
8 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined that the facility failed to notify resident's physician when medications were held. This was evident for 1 (R#62) of 3 residents reviewed for not...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined that the facility failed to complete thorough investigations of allegations of abuse. This was evident for 1 (#MD00217463) of 7 facility reported...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on record review and interviews it was determined that the facility failed to maintain medical records in accordance with professional standards. This was evident for 1 (MD00215206) of 7 facilit...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review and interviews, it was determined that the facility failed to ensure that residents received ordered medications or treatments. This was evident for three (Resident #36, #12, an...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observations, record reviews and interviews, it was determined that the facility failed to ensure that a resident's urine collection bag was secured off the floor. This was evident in 1 (Resi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on medical review and staff interview, it was determined that the facility failed to document the reasons for administering as-needed (PRN) pain medications, failed to document the pain assessme...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, it was determined that the facility failed to ensure a resident received their medications according to the attending physician's orders. This was evident f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on record review, observation, and staff interview, it was determined that the facility failed to implement Enhanced Barrier Precautions (EBP) as part of the infection prevention and control pro...
Read full inspector narrative →
Jan 2025
30 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
2) Resident #64 was admitted to the facility in early 2024. During the initial tour of the facility on 1/8/25 at 12:37 PM, the resident was observed in bed and the urine collection bag was on the righ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interviews, it was determined that the facility failed to ensure that call devices were kept within reach of the resident. This was evident for 1 (Resident #40...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0568
(Tag F0568)
Could have caused harm · This affected 1 resident
Based on interviews and record review, it was determined that the facility failed to provide residents with quarterly statements in writing of their personal funds account managed by the facility. Thi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined that the facility failed to ensure they informed residents of their right to formulate an advance directive. This was evident for one re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on staff interviews, and record reviews, it was determined that the facility failed to notify the physician when a medication was held several times for low systolic blood pressure (SBP). This w...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on interviews and record review, it was determined that the facility failed to implement its abuse policy. This was evident for one ( #3) of two residents who alleged misappropriation of propert...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interviews and record review, it was determined that the facility failed to report an incident of alleged misappropriation of resident's property to the Office of Health Care Quality.This was...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0635
(Tag F0635)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interviews it was determined that the facility failed to ensure essential care upon admission. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review and staff interviews, it was determined that the facility failed to provide a person-centered comprehensive care plan developed and implemented to meet residents' needs. This wa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on staff interviews, and record review, it was determined that the facility failed to follow the physician's orders for weights. This was evident for 1 (Resident #44 ) of 6 residents reviewed fo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview it was determined that the facility failed to provide necessary treatment and servi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observations, records review and interviews, it was determined that the facility failed to ensure fall mats were in proper placement. This was evident for 1 (Resident #10) in 3 residents revi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on record review, interviews,and observations, it was determined that the facility failed to provide appropriate treatment and services for care of residents with indwelling catheter. This was e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0710
(Tag F0710)
Could have caused harm · This affected 1 resident
Based on record review and interviews, it was determined that the facility failed to ensure that a resident's care was overseen by a physician. This was evident for 1 (#24) of 6 residents reviewed for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interviews, it was determined that the facility failed to ensure that physician's notes were complete, accurate, signed, and dated at each visit and part of th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to ensure nursing staff were competent with their skills set. This was evident for 2 Registered Nurses (RN #19 and RN #...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined the facility did not have a Director of Nursing who worked on a full-time basis. This was evident during the recertification survey and had the ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews, it was determined that the facility failed to ensure that Irregularities identified by the pharmacist were reviewed and acted upon timely by the attendin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record reviews and staff interviews, it was determined that the facility failed to keep residents' drug regimens free from unnecessary medications by failing to ensure residents received thei...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, it was determined that the facility failed to 1) accurately document the r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected 1 resident
Based on staff interviews and record review, it was determined that the facility failed to have a qualified dietary staff. This was evident for 1 of 1 Director of Food Services.
The findings include:
...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0836
(Tag F0836)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined that the facility failed to comply with
State regulations when the facility failed to 1) employ a qualified social worker, 2) monitor
employee's ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record review, it was determined that the facility failed to maintain complete, accurate and legible medical records. This was evident for 3 (#26, #36, #12) out o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and pertinent document review, it was determined that the facility failed to: 1) ensure a glucometer was adequately disinfected between different resident uses in a ma...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined that the facility failed to provide the 2024-2025 COVID-19 immunization to residents and staff. This was evident for 1) five residents (Resident...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) On 1/16/25 review of Resident #75's medical record revealed the resident was originally admitted to the facility on [DATE]. R...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Care plans are developed to guide residents' care in the facility. They must be created within 7 days of completion of a residen...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, it was determined that the facility failed to 1) provide residents with the amount of as...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected multiple residents
Based on medical record review and interviews, it was determined that the facility failed to document the reasons for administering as-needed (PRN) pain medications, failed to document pain assessment...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record review, it was determined that the facility failed to monitor temperatures for the dishwasher machine to ensure adequate sanitation, and ensure temperatur...
Read full inspector narrative →
Mar 2023
32 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
Based on observation, interview and medical record review, it was determined the facility failed to prevent the development of a stage 4 pressure ulcer, failed to notify the physician when a weekly wo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of Resident #19's medical record revealed that the resident was admitted to the facility on [DATE].
During an intervie...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and medical record review, it was determined the facility failed to ensure that nursing staff notified the physician that a pressure wound was continuing to worsen and develop possi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined that the facility failed to ensure that residents received the written Notice of Medicare Non-Coverage prior to the date the services we...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0603
(Tag F0603)
Could have caused harm · This affected 1 resident
Based on review of facility documentation, resident records, and interviews, it was determined the facility failed to ensure that the residents had an environment that was free from involuntary seclus...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on review of facility documents and staff interview, it was determined the facility 1) failed to report an allegation of an injury of unknown injury to the State Agency, the Office of Health Car...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on review of facility reported incident investigations and interview, it was determined the facility failed to thoroughly investigate allegations of abuse, including an injury of unknown injury....
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility failed to document the information conveyed to a receiving acute care provider when a resident was transferred t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility failed to orient, prepare, and document a resident's preparation for a transfer to the hospital. This was eviden...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0642
(Tag F0642)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined that the facility failed to ensure that the individual who completed a portion of the Minimum Data Set assessment signed and ceritified ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to complete a PASSAR during the original admission period for a resident. This was found to be true for 1 (Resident #38) of 3 residents revie...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, it was determined that the facility failed to ensure the safety of a cognitively impaired resident by failing to provide adequate supervision as evidenced b...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined that the facility failed to ensure staff assessed and developed a care plan to address a resident's needs related to dialysis; and faile...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, it was determined that the facility failed to ensure that alternatives to side rails were attempted prior to the initation of side rails. This was fo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on review of employee files and interviews, it was determined that the facility failed to ensure that performance reviews were completed for nurse aides at least once every 12 months. This was f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0741
(Tag F0741)
Could have caused harm · This affected 1 resident
Based on review of employee files and interview, it was determined that the facility failed to ensure that staff received training related to caring for residents with behavioral health care needs. Th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined the facility failed to keep a resident's drug regimen free from unnecessary drugs by failing to ensure that prescribed medications...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on medical record review, it was determined that the facility failed to ensure that an as needed psychotropic medication order was limited to 14 days. This was found to be evident for one (#8) o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interview, it was determined that the facility failed to develop and implement infection control polic...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on record review, review of policy, and staff interview, it was determined that the facility failed to have a process in place to ensure that the flu vaccine and pneumonia vaccine was offered to...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and staff interview, it was determined that the facility failed to develop and implement policies and procedures to ensure that their, 1) residents were offered ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0888
(Tag F0888)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, it was determined that the facility failed to develop and implement policies and procedures to ensure that 100% of staff were fully vaccinated, had an appro...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, it was determined that the facility failed to ensure that advance directives were ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) During an interview conducted on 3/06/23 1:10 PM, GNA #43 stated that Resident# 19 was admitted to hospital on [DATE] due to ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) During an interview conducted on 03/06/23 01:10 PM the GNA # 43 stated that that Resident #19was admitted to hospital on [DAT...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
Based on medical record review and interview, it was determined that the facility failed to ensure the Minimum Data Set assessments accurately reflected the resident's status as evidenced by failure t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
3) On 3/16/23 at 5:49 AM Resident #21 was heard requesting a shower from Geriatric Nursing Assistant (GNA) #38 and she replied that it was too early for a shower.
A medical record review on 3/17/23 a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Based on medical record review and interview, it was determined that the facility failed to have an effective system in place to ensure that interdisciplinary team care plan meetings were scheduled to...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
Based on medical record review, observation and interview, it was determined that the facility failed to ensure activities to meet the needs of the residents. This was found to be evident for 2 (#46, ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on review of staffing information, complaints allegations, medical records and interviews, it was determined that the facility failed to ensure sufficient nurse staffing. This was found to be ev...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review, and interview, it was determined that the facility 1) failed to ensure that nursing...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0838
(Tag F0838)
Minor procedural issue · This affected most or all residents
Based on review of the facility assessment and interview, it was determined that the facility failed to ensure that the faciltiy assesment addressed the staff competencies that are necessary to provid...
Read full inspector narrative →
Nov 2018
22 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, medical record review and staff interview, it was determined that the facility staff failed to ensure access to the nurse call bell for a resident who was totally dependent on nu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5) An inoperable heating unit built into the bathroom wall of room [ROOM NUMBER] was covered with duct tape which was peeling in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on facility documentation review and staff interview it was determined the facility failed to timely report a suspected abuse to the Survey Agency, which was the Office of Health Care Quality (O...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) The MDS is part of the Resident Assessment Instrument that was Federally mandated in legislation passed in 1986. The MDS is a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0642
(Tag F0642)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the medical record and interview with staff, it was determined that the facility failed to ensure that a regi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility staff failed to ensure that each resident received treatment and care in accordance with professional standards ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, medical record review and staff interview it was determined the facility failed to ensure that residents with a limited range of motion received the appropriate treatment and ser...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, staff interview and medical record review, it was determined the facility failed to ensure that a resident was placed on oxygen per physician's orders and failed to develop a res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
Based on record review and staff interviews, it was determined that the facility failed to maintain a resident centered dementia treatment and services care plan. This was evident for 1 (#18) of 4 res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record reviews and staff interviews, it was determined that the facility failed to have a process in place to ensure recommendations from the monthly pharmacy review were responded to in a ti...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
3) Review of Resident #18's medical record, on 11/28/18, revealed that the September, October, and November 2018 behavior monitoring log failed to have specific behaviors that were being monitored, an...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on record review and interviews with staff, it was determined that the facility failed to allow 2 residents to be involved in the planning of their care by not providing notice of care plan meet...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected multiple residents
3) Review of the medical record for Resident #41 on 11/26/18 documented that the resident was sent to an acute care facility on 3/24/18, 5/8/18, 10/23/18 and 11/26/18. There was no documentation found...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on medical record review, observations, and staff interviews it was determined that facility failed to ensure a resident's environment was free from accident hazards. This is evident for 1 (#63)...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) On 11/27/18, a review of Resident #35's medical record revealed physician progress notes were not in the medical record on th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
4) On 11/29/18 at 8:00 AM, the medical record for Resident #22 was reviewed. During this review, it was noted that Resident #22's record under Resident Forms contained a Physician's Certification That...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) Review of the care plans for Resident #63 on 11/27/18 revealed a care plan for at risk for falls due to ankle fracture, visua...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4) Review of the care plan for dementia care for Resident #18 on 11/27/18 revealed evaluations of the care plan, however, the la...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0559
(Tag F0559)
Minor procedural issue · This affected multiple residents
Based on medical record review and interview with staff, it was determined the facility failed to notify a resident/resident representative in writing of a new roommate. This was evident for 1 (#74) o...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0577
(Tag F0577)
Minor procedural issue · This affected most or all residents
Based on observation, document review, resident interview and staff interview, it was determined the facility failed to 1) ensure that survey results were posted in a place readily accessible to resid...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Transfer Notice
(Tag F0623)
Minor procedural issue · This affected most or all residents
Based on medical record review and staff interview, it was determined the facility failed to notify the resident/resident representative in writing of a transfer/discharge of a resident along with the...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Infection Control
(Tag F0880)
Minor procedural issue · This affected most or all residents
Based on observation, it was determined that the facility staff failed to follow infection control practices and guidelines to prevent the development and transmission of disease by failing to ensure ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 harm violation(s), $98,631 in fines, Payment denial on record. Review inspection reports carefully.
- • 92 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $98,631 in fines. Extremely high, among the most fined facilities in Maryland. Major compliance failures.
- • Grade F (25/100). Below average facility with significant concerns.
About This Facility
What is Lions Rehab Center's CMS Rating?
CMS assigns LIONS REHAB CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Lions Rehab Center Staffed?
CMS rates LIONS REHAB CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes.
What Have Inspectors Found at Lions Rehab Center?
State health inspectors documented 92 deficiencies at LIONS REHAB CENTER during 2018 to 2025. These included: 1 that caused actual resident harm, 86 with potential for harm, and 5 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
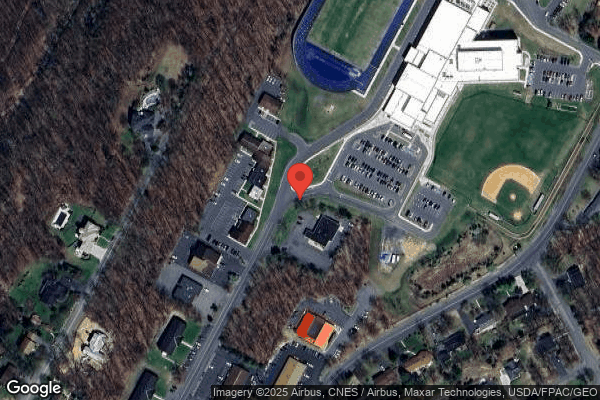
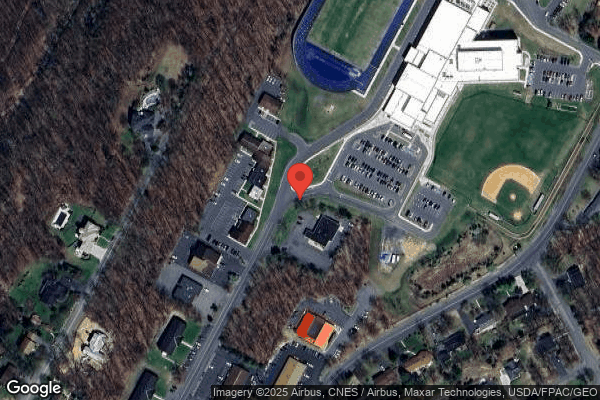
Who Owns and Operates Lions Rehab Center?
LIONS REHAB CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 101 certified beds and approximately 70 residents (about 69% occupancy), it is a mid-sized facility located in CUMBERLAND, Maryland.
How Does Lions Rehab Center Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, LIONS REHAB CENTER's overall rating (1 stars) is below the state average of 3.0 and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Lions Rehab Center?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Lions Rehab Center Safe?
Based on CMS inspection data, LIONS REHAB CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Maryland. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Lions Rehab Center Stick Around?
LIONS REHAB CENTER has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Lions Rehab Center Ever Fined?
LIONS REHAB CENTER has been fined $98,631 across 1 penalty action. This is above the Maryland average of $34,065. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Lions Rehab Center on Any Federal Watch List?
LIONS REHAB CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.