FROSTBURG VILLAGE REHAB CENTER




Over 2 years since last inspection. Current conditions may differ from available data.
Frostburg Village Rehab Center has received a Trust Grade of F, indicating poor performance and significant concerns. They rank #202 out of 219 facilities in Maryland, placing them in the bottom half, and #6 out of 8 in Allegany County, meaning only two local options are worse. While the facility is improving-increasing from 25 issues in 2022 to 14 in 2025-there are still serious concerns, including a staffing rating of just 1 out of 5, with a 68% turnover rate that is much higher than the state average. Although they have not incurred any fines, which is a positive sign, the RN coverage is concerning, as it is less than 92% of Maryland facilities, meaning residents may not receive adequate medical oversight. Specific incidents include a resident suffering a fracture due to improper staff assistance during transfers and multiple instances where no RN was present on duty for over 60 hours, raising alarms about the adequacy of care. Overall, families should weigh these strengths and weaknesses carefully when considering this facility.
- Trust Score
- F
- In Maryland
- #202/219
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 68% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Maryland facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 26 minutes of Registered Nurse (RN) attention daily — below average for Maryland. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 61 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Maryland average (3.0)
Significant quality concerns identified by CMS
21pts above Maryland avg (46%)
Frequent staff changes - ask about care continuity
Part of a multi-facility chain
Ask about local staffing decisions and management
20 points above Maryland average of 48%
The Ugly 61 deficiencies on record
Aug 2025
14 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on medical record reviews, interviews, and review of facility investigation documents, it was determined that the facility failed to ensure residents were free from accidents as evidenced by the...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined that the facility failed to ensure staff informed the physician or nurse practitioner when a resident exhibited violent and aggressive be...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to protect residents from abuse. This was evident for 2 (#358494 and #358463) out of 16 facility reported incidents rev...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on record reviews and interviews, it was determined that the facility failed to ensure Minimum Data Set (MDS) assessments were accurately coded. This was evident for 1 (Resident #25) of 1 reside...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on medical record review, interview and observations it was determined that the facility failed to ensure care was provided in accordance with professional standards of practice. This was eviden...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observations, record review and staff interviews, it was determined that the facility failed to administer oxygen as ordered by the physician. This was evident for 1 resident (Resident #5) re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined that the facility failed to ensure residents were free from significant medication errors. This was found to be evident for one (Resident...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
Based on record review and interview, it was determined that the facility failed to report injuries of unknown origin. This was evident for one facility reported incident (#358490) of sixteen facility...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
Based on record review and interview, it was determined that the facility failed to thoroughly investigate allegations of abuse and injuries of unknown origin. This was evident for 2 residents (Reside...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on review of medical records and other pertinent documentation, and interviews it was determined that the facility failed to ensure staff had adequate training. This was evident for one geriatri...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0807
(Tag F0807)
Could have caused harm · This affected multiple residents
Based on a review of pertinent documents, observations and interviews, the facility failed to have a place to ensure residents were provided with water and other fluids to support their hydration and ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected multiple residents
Based on pertinent document review, observation and interview, it was determined that the facility failed to provide a nutritional snack to Residents when meals were scheduled more than 14 hours apart...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on review of pertinent documentation and interviews it was determined that the facility failed to ensure a registered nurse was working for at least 8 consecutive hours every day. This was found...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected most or all residents
Based on review of pertinent documentation and interviews it was determinted that the facility failed to ensure annual evaluations were being completed for geriatric nursing assistants (GNA). This was...
Read full inspector narrative →
Sept 2022
25 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on interview with residents and staff and review of resident records it was determined that the facility failed to promote and facilitate resident self-determination by failing to provide reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined the facility staff failed to reveal evidence that the resident or resident representative was informed of their right to formulate...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on record review and staff interview it was determined that the facility failed to develop and implement abuse policies and procedures as evidenced by the failure to report injuries of unknown o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
On 9/20/22 at 11:32 AM a review of the medical record for Resident #104 failed to reveal a copy of the transfer form related to the hospital transfer that occurred on 3/9/22 or the notice of appeal re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined that the facility failed to orient, prepare, and document a resident's preparation for a transfer to the hospital. This was evident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined the facility failed to ensure residents were made aware of a facility's bed-hold and reserve bed payment policy when transferred to...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
Based on record review and staff interview it was determined that the facility failed to conduct an initial comprehensive assessment that included an assessment of a resident's preferences for customa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on observation, medical record review and staff interview, it was determined the facility staff failed to ensure Minimum Data Set (MDS) assessments were accurately coded. This was evident for 1 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined that the facility staff failed to evaluate and update a resident's plan of care after each assessment. This was evident for 1 (#35)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined the facility failed to have an effective system in place to ensure restorative nursing interventions were implemented and incorporated in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
3.) On 9/13/22 at 1:30 PM the review of the medical record revealed Resident #21 was diagnosed with renal failure, diabetes, and bilateral lower extremity amputations and attends dialysis three days p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Review of resident # 352's medical record revealed a diagnosis of congestive heart failure (CHF) and cardiomyopathy.
On 9/19/22 at 2:38 PM a review of the medical record revealed the following documen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined the facility failed to have an effective system in place to ensure wound specialist recommendations were reviewed and implemented. This w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews it was determined the facility failed to ensure non-pharmacological interventions were attempted prior to the administration of narcotic pain medication a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview it was determined that facility staff failed to ensure that before side rails...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0710
(Tag F0710)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews it was determined the facility failed to ensure the primary care physician effectively supervised resident care when the physician 1) failed to ensure ace...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
Based on observation, record review, and staff interview it was determined that the facility staff failed to develop and implement a resident - centered dementia care plan with achievable care plan go...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on review of medical records, Narcotic Count sheets and interviews it was determined that the facility failed to: 1) ensure staff completed the controlled drug count at the change of shift as ev...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review and staff interview it was determined that the facility failed to develop and implement policies and procedures for medication regimen reviews, as evidenced by, the failure to e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected 1 resident
Based on staff interview and review of facility documentation, it was determined the facility failed to ensure that effective quality assessment and assurance performance improvement interventions wer...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected 1 resident
Based on record reviews and staff interviews it was determined that the facility failed to have a fully trained infection preventionist on duty. This is evidenced by the current staff member in the po...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected 1 resident
Based observation and interview it was determined that the facility failed to ensure regular inspections of all bed side rails. This was evident for 1 (Resident #20) of 11 residents reviewed for accid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
The MDS (Minimum Data Set) is part of the Resident Assessment Instrument that was Federally mandated in legislation passed in 1986. The MDS is a set of assessment screening items employed as part of a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected multiple residents
Based on medical record review and staff interview, it was determined that the facility staff failed to ensure physician progress notes were written, signed, and dated at each visit. This was evident ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
3) On 9/16/22 at 9:16 AM, a review of Resident #70's EMR (electronic medical record), under the miscellaneous tab revealed a Psychiatry Note, which documented the resident was seen by the CRNP-PMH (Ce...
Read full inspector narrative →
Oct 2018
22 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
3) The facility failed to ensure that Resident #65's urinary bag was covered from view from people walking past his/her room.
A urinary catheter is a medical device that bypasses the urethra and drai...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) A review of Resident #91's medical record was conducted on 10/24/18 at 11:46 AM. A change in condition evaluation dated 10/14...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined the facility failed to develop an individualized discharge...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined the physician failed to write a discharge summary that sum...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility staff 1) failed to provide an activity program to meet the needs and preferences of the residents, 2) failed to ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, medical record review and family/staff interviews, it was determined the facility failed to ensure that a resident did not have further decrease in range of motion as evidenced b...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation and interview with facility staff, it was determined that the facility failed to ensure that resident rooms were free from accident hazards as evidenced by medication not prescrib...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on interview with residents and review of medical records, it was determined that the facility failed to ensure that residents received adequate pain management as evidenced by the failure to as...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on medication administration observation, medical record review and staff interview, it was determined the facility staff failed to ensure a medication error rate of less than 5 percent for 2 (#...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined the facility failed to keep residents free from significant medication errors. This was evident for 1 (#253) of 1 residents review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0773
(Tag F0773)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility staff failed to promptly notify the ordering physician or clinical practitioner of laboratory results. This was ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on medical record review and interview with facility staff, it was determined that the facility failed to ensure that resident care plans were developed in a way that was specific and resident c...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
5) Review of Resident #86's medical record revealed the resident had a comprehensive assessment on 6/30/18, and a quarterly assessment on 9/30/18. Review of Resident #86's activity care plan, the resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
Based on medical record review and staff interview, it was determined the facility failed to monitor a resident's weight per the plan of care. This was evident for 1 (#22) of 10 residents reviewed for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and documentation review, it was determined that facility staff failed to date and label insulin when opene...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on medical record review and interview with facility staff, it was determined that the facility failed to maintain complete and accurate medical records. This was true for 1 (#301, #158) of 2 re...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
3) The facility failed to ensure that Resident #65's urinary bag remained off of the ground and away from sources of infectious microorganisms.
An indwelling urinary catheter is a medical device that...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0559
(Tag F0559)
Minor procedural issue · This affected most or all residents
Based on medical record review and interview with staff, it was determined the facility failed to notify a resident/resident representative in writing of a new roommate. This was evident for 1 (#19) o...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0582
(Tag F0582)
Minor procedural issue · This affected most or all residents
Based on review of facility records and interview with staff, it was determined the facility failed to provide residents with required Skilled Nursing Facility Advanced Beneficiary Notice of Noncovera...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Transfer Notice
(Tag F0623)
Minor procedural issue · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) The facility failed to provide Resident #102 with a transfer summary for his/her hospitalization on 5/21/18.
Resident #102's...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0625
(Tag F0625)
Minor procedural issue · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) The facility failed to provide Resident #102 or his/her representative with a bed hold policy for his/her hospitalization on ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0655
(Tag F0655)
Minor procedural issue · This affected most or all residents
Based on interview with residents and facility staff, it was determined that the facility failed to give residents a list of their admission medications with a copy of their baseline care plan. This w...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Maryland facilities.
- • 61 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade F (30/100). Below average facility with significant concerns.
- • 68% turnover. Above average. Higher turnover means staff may not know residents' routines.
About This Facility
What is Frostburg Village Rehab Center's CMS Rating?
CMS assigns FROSTBURG VILLAGE REHAB CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Frostburg Village Rehab Center Staffed?
CMS rates FROSTBURG VILLAGE REHAB CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 68%, which is 21 percentage points above the Maryland average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 57%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Frostburg Village Rehab Center?
State health inspectors documented 61 deficiencies at FROSTBURG VILLAGE REHAB CENTER during 2018 to 2025. These included: 1 that caused actual resident harm, 55 with potential for harm, and 5 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Frostburg Village Rehab Center?
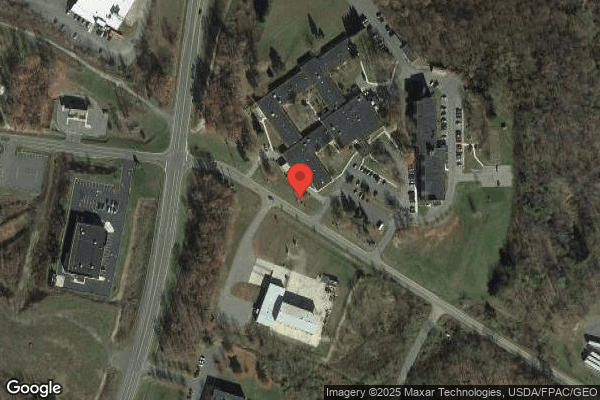
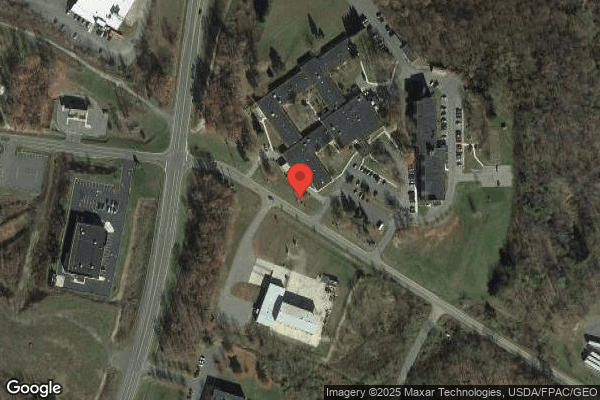
FROSTBURG VILLAGE REHAB CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by STERLING CARE, a chain that manages multiple nursing homes. With 122 certified beds and approximately 101 residents (about 83% occupancy), it is a mid-sized facility located in FROSTBURG, Maryland.
How Does Frostburg Village Rehab Center Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, FROSTBURG VILLAGE REHAB CENTER's overall rating (1 stars) is below the state average of 3.0, staff turnover (68%) is significantly higher than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Frostburg Village Rehab Center?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's high staff turnover rate and the below-average staffing rating.
Is Frostburg Village Rehab Center Safe?
Based on CMS inspection data, FROSTBURG VILLAGE REHAB CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Maryland. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Frostburg Village Rehab Center Stick Around?
Staff turnover at FROSTBURG VILLAGE REHAB CENTER is high. At 68%, the facility is 21 percentage points above the Maryland average of 46%. Registered Nurse turnover is particularly concerning at 57%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Frostburg Village Rehab Center Ever Fined?
FROSTBURG VILLAGE REHAB CENTER has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Frostburg Village Rehab Center on Any Federal Watch List?
FROSTBURG VILLAGE REHAB CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.