MANOKIN NURSING AND REHAB




Over 2 years since last inspection. Current conditions may differ from available data.
Manokin Nursing and Rehab has received a Trust Grade of F, which indicates poor performance with significant concerns. It ranks #211 out of 219 in Maryland, placing it in the bottom half of facilities statewide, and #2 out of 2 in Somerset County, meaning there is only one other local option that is better. The facility is currently improving, with issues decreasing from 51 in 2023 to 4 in 2025, but it still has serious deficiencies. Staffing is rated below average at 2 out of 5 stars, with a turnover rate of 49%, which is concerning. Additionally, the facility has incurred fines totaling $197,970, which is higher than 98% of Maryland facilities, suggesting ongoing compliance issues. Specific incidents include failing to remove expired food items and ensure proper food safety standards, which could affect all residents, and a failure to protect residents from physical abuse, putting them at risk for serious harm. Another incident involved inadequate supervision when positioning a resident in bed, which resulted in harm to that resident. While the facility has some strengths, such as a trend toward improvement, the serious issues noted should be carefully considered by families researching options.
- Trust Score
- F
- In Maryland
- #211/219
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 49% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $197,970 in fines. Lower than most Maryland facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 27 minutes of Registered Nurse (RN) attention daily — below average for Maryland. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 68 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Maryland average (3.0)
Significant quality concerns identified by CMS
Near Maryland avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 68 deficiencies on record
Sept 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined the facility staff failed to maintain a medical record in the most accurate form. This was evident for 1 (Resident #100) of 6 residents ...
Read full inspector narrative →
Jun 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on reviews and staff interviews, the facility failed to protect resident property and provide a safe environment by not ma...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review of R35's face sheet showed an admission was dated 07/20/2022; diagnoses included Generalized anxiety disorder, ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and staff interviews, the facility failed to provide adequate supervision and implement intervention to ...
Read full inspector narrative →
Aug 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on complaint, reviews of the facility policies, review of medical record, as well as staff interviews, it was determined t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on complaint, reviews of the facility policies and a medical record, as well as staff interviews, it was determined that t...
Read full inspector narrative →
Aug 2023
42 deficiencies
2 IJ (1 facility-wide)
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
Based on clinical and administrative record reviews, and interviews, the facility failed to protect residents' right to be free from physical abuse by other residents. The facility's failure to implem...
Read full inspector narrative →
CRITICAL
(L)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Food Safety
(Tag F0812)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
Based on observation and interview with facility staff, it was determined that the facility failed to remove expired food items and label opened stored food items and in a manner that maintains profes...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review and staff interviews, it was determined that the facility staff failed to ensure adequate superv...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on record review and staff interview it was determined that the facility staff failed to ensure that a resident's right to make decisions was honored. This was evident for 1 (#164) out of 68 res...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observations and interviews it was determined the facility failed to ensure that the resident's call light was within reach to allow access to assistance when needed. This was evident for 3 (...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0569
(Tag F0569)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview it was determined that the facility staff failed to ensure that nursing home staff fu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on clinical record review and staff interviews, it was determined that the facility staff failed to ensure clarity regarding whether Advance Directives had been formulated by a resident. This wa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on clinical record review and staff interview it was determined that the facility nursing staff failed to ensure a resident's family was notified of a hospitalization and to ensure only an autho...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and review of facility documentation, it was determined the facility failed to report a critical unusual occurrence that affected the health and safety of all residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on review of faciity records and interview, it was determined that the facility failed to conduct a thorough investigation. This was found to be evident for 2 (# 25, # 32) out of 20 facility rep...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined the facility failed to ensure that Minimum Data Set (MDS) assessments were complete. These concerns with incomplete assessments wer...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on clinical record review and staff interview it was determined that the facility staff failed to ensure a resident had baseline care plans created and initiated for a resident. This was evident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, it was determined that the facility failed to provide incontinence care. This was evident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, it was determined that the facility staff failed to ensure that activities were provided that met a resident's needs. This was evident for 1 (#32...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on resident and staff interviews, observations, and medical record review, it was determined that the facility staff failed to provide a resident with a multi podus boot, as ordered. This was ev...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, it was determined that the facility staff failed to ensure that consent was obtained prior to utilizing bed rails. This was evident for 1 (#212) of 68 resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0710
(Tag F0710)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, it was determined that the facility failed to ensure the physician provided supervision for a resident with significant weight loss. This was found to be eviden...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0742
(Tag F0742)
Could have caused harm · This affected 1 resident
Based on record reviews and interviews, it was determined that the facility failed to consistently monitor the behavior of a resident. This was found to be evident for 1 (#28) out of 1 resident review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and staff interview it was determined that the facility staff failed to ensure that medication carts were locked and secured. This was evident for 1 of 3 nursing units.
The findi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interviews it was determined that the facility failed to provide routine dental services identified as need for a resident. This was found evident of 1 of 5 (R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews it was determined that the facility failed to keep complete and accurate medical records. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected 1 resident
Based on staff interviews and record review, the facility failed to designate a qualified Infection Control Preventionist (IP), who had completed specialized training in infection prevention and contr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interviews and record review, it was determined that the facility staff failed to ensure that a resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected 1 resident
Based on the record reviews and interviews, it was determined that the facility failed to ensure that a Geriatric Nursing Assistant (GNA) received the required 12 hours of in-service training. This wa...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observation and staff interview, it was determined that facility staff failed to treat each resident in a dignified manner by 1) standing over a resident while feeding the resident, and 2) pu...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, it was determined that the facility failed to ensure resident rooms were maintained in a h...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
Based on medical record review and staff interview it was determined the facility failed to ensure that Minimum Data Set (MDS) assessments were complete. These concerns with incomplete assessments wer...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
2) During a complaint investigation on 8/21/23 at 11:05 AM the surveyors reviewed a care plan for Resident # 28 for interventions related to the resident exposing him/herself and masturbating. The sur...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
2) During a phone interview conducted on 07/27/2023 at 11:32 AM, the complainant stated the facility had not held care plan meetings.
During an interview on 8/10/23 at 9:00 AM, the surveyor asked Soci...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5)During a review of a complaint conducted on 8/9/2023 at 3:15 PM, the complainant stated that Resident #462 had not received a ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected multiple residents
Based on medical record review and staff interview it was determined the physician progress notes were not in the resident medical records the day the resident was seen. This was evident for 5 (#41, #...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on the review of facility administrative records and interviews, it was determined that the facility failed to ensure a sufficient number of staff to meet the needs of the residents. This defici...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review and staff interview it was determined that the facility staff failed to provide pharmaceutical s...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
Based on recorded review and interviews it was determined that the facility failed to have monthly medication regimen reviews by a licensed pharmacist and failed to have a process in place to ensure t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation of medication administration it was determined that the facility staff failed to ensure medications were administered in a safe, appropriate, and timely manner. This was evident f...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Social Worker
(Tag F0850)
Could have caused harm · This affected multiple residents
Based on interviews and review of the facility's policies it was determined that the facility failed to have a qualified, full-time social worker employed to oversee the social service duties. This wa...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0924
(Tag F0924)
Could have caused harm · This affected multiple residents
Based on observations and facility staff interviews, the facility failed to ensure that all corridors had firmly installed handrails on each side.
The findings include:
On 07/25/2023 at 11 AM, survey...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected multiple residents
Based on staff interview and record review, it was determined that the facility failed to ensure that the dementia training provided to staff included managing challenging behaviors. This was evident ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on staff interview and observation it was determined the facility failed to ensure that the facility kitchen was managed by fully certified and competent staff, when since October 1, 2023, the f...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected most or all residents
Based on interviews, observations, and documentation review, facility administration failed to effectively allocate resources to meet resident needs and to ensure their highest practicable well-being ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on staff interviews and record review, it was determined that the facility failed to ensure that the infection line lists were updated and proper hand hygiene was performed during a medication a...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected most or all residents
Based on observation, interviews, and documentation review, it was determined the facility failed to ensure that essential equipment was operational and safe (1) when the facility hot water heater tha...
Read full inspector narrative →
Jan 2023
7 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, review of medical records, facility investigative file, and staff and resident interviews it was determine...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review the facility failed to notify Responsible Party of weight loss for resident # 9. This was evident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on complaint from daughter and medication administration record and staff interview, the facility failed to give or sign o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations and staff interviews the facility failed to maintain a safe and effective system for securing medication, treatment supplies, and hazardous medical equipment in their designated ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
Based upon observation and staff interviews, it was determined that facility staff failed to take steps to repair the facility Hoyer lift scales. This was evident for 3 of 3 mechanical lifts with a sc...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on observation and staff interview, it was determined that the facility staff failed to maintain the resident call system in working order. This was evident for 1 of 4 nursing units observed dur...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on reviews of medical records and staff interviews, it was determined the facility staff failed to maintain a medical records in the most accurate form. This was evident for 4 (Residents #1, #2,...
Read full inspector narrative →
Feb 2019
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observations and interview of facility staff. it was determined that the facility staff failed to promote and enhance a resident's dignity while assisting the resident with their breakfast an...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined that the facility staff failed to provide a written notice for emergency transfers to the resident and/or the resident represe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
2. Review of the medical record for Resident #108 on 2/13/19 revealed Resident #108 had physician orders to obtain pre and post-dialysis vitals and weights. Monitoring a dialysis patient's weight help...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined the facility staff failed to administer oxygen to Resident #6 in accordance with the standard of practice. This was evident for 1 o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined the facility staff failed to conduct AIMs testing on Residents (# 65). This was evident for 1 of 1 resident selected for review during t...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and staff interview it was determined that the facility staff failed to ensure staffing hours for nursing s...
Read full inspector narrative →
Sept 2017
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0241
(Tag F0241)
Could have caused harm · This affected 1 resident
Based on resident observation and staff interview it was determined the facility staff failed to ensure residents were fed in a dignified manner (# 146). This was true for 1 out of the 29 residents in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0246
(Tag F0246)
Could have caused harm · This affected 1 resident
Based on record review and resident interviews, it was determined that the facility staff failed to provide showers to Residents as ordered and per facility policy (# 28 and # 128). This was evident f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0278
(Tag F0278)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined that the facility staff failed to document accurate assessments for Residents (# 92, # 12 and # 146) on the MDS. This was evident f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0279
(Tag F0279)
Could have caused harm · This affected 1 resident
Based on review of medical record and staff interview, it was determined the facility staff failed to develop comprehensive care plan addressing insomnia for Resident (# 163). This was evident for 1 o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0309
(Tag F0309)
Could have caused harm · This affected 1 resident
Based on medical record review, observation, and interview, it was determined the facility staff failed to administer a medication as ordered by the physician for Resident # 58. This was evident for 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0431
(Tag F0431)
Could have caused harm · This affected 1 resident
Based on observation and staff interview it was determined that the facility staff failed to ensure the security of residents' medications and privacy. This was true for 2 out of the 5 units in the fa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0514
(Tag F0514)
Could have caused harm · This affected 1 resident
Based upon record review and staff interview it was determined that facility staff failed to ensure the resident's medical record was accurate and complete. This is evident for 1 of 29 resident's (# 9...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 2 life-threatening violation(s), 2 harm violation(s), $197,970 in fines, Payment denial on record. Review inspection reports carefully.
- • 68 deficiencies on record, including 2 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $197,970 in fines. Extremely high, among the most fined facilities in Maryland. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Manokin Nursing And Rehab's CMS Rating?
CMS assigns MANOKIN NURSING AND REHAB an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Manokin Nursing And Rehab Staffed?
CMS rates MANOKIN NURSING AND REHAB's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 49%, compared to the Maryland average of 46%.
What Have Inspectors Found at Manokin Nursing And Rehab?
State health inspectors documented 68 deficiencies at MANOKIN NURSING AND REHAB during 2017 to 2025. These included: 2 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 2 that caused actual resident harm, 63 with potential for harm, and 1 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Manokin Nursing And Rehab?
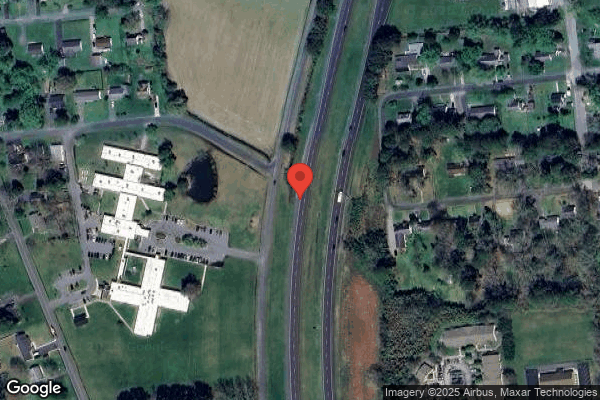
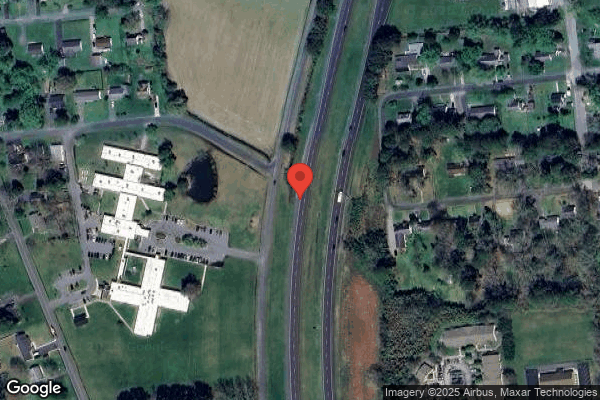
MANOKIN NURSING AND REHAB is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by KEY HEALTH MANAGEMENT, a chain that manages multiple nursing homes. With 135 certified beds and approximately 107 residents (about 79% occupancy), it is a mid-sized facility located in PRINCESS ANNE, Maryland.
How Does Manokin Nursing And Rehab Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, MANOKIN NURSING AND REHAB's overall rating (1 stars) is below the state average of 3.0, staff turnover (49%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Manokin Nursing And Rehab?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the substantiated abuse finding on record, and the below-average staffing rating.
Is Manokin Nursing And Rehab Safe?
Based on CMS inspection data, MANOKIN NURSING AND REHAB has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). Inspectors have issued 2 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Maryland. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Manokin Nursing And Rehab Stick Around?
MANOKIN NURSING AND REHAB has a staff turnover rate of 49%, which is about average for Maryland nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Manokin Nursing And Rehab Ever Fined?
MANOKIN NURSING AND REHAB has been fined $197,970 across 2 penalty actions. This is 5.6x the Maryland average of $35,059. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Manokin Nursing And Rehab on Any Federal Watch List?
MANOKIN NURSING AND REHAB is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.