AUTUMN LAKE HEALTHCARE AT GLADE VALLEY




Inspected within the last 6 months. Data reflects current conditions.
Autumn Lake Healthcare at Glade Valley has received a Trust Grade of D, indicating below-average performance with some concerning issues. Ranking #137 out of 219 facilities in Maryland places it in the bottom half, and #7 out of 8 in Frederick County suggests only one local option is better. The facility's trend is worsening, with the number of reported issues increasing significantly from 4 in 2023 to 30 in 2025. Staffing is a concern, with a rating of 2 out of 5 stars and a 49% turnover rate, which is around the Maryland average, meaning staff may not be consistently familiar with residents' needs. Additionally, the facility has accumulated $37,265 in fines, indicating more compliance problems than 79% of facilities in the state. Specific incidents include a serious finding where a resident was harmed during a mechanical lift transfer because it was improperly conducted by one staff member instead of the required two. Other concerns include a lack of annual performance evaluations for nurse aides, which can impact care quality, and insufficient training for staff on handling residents with mental health issues. While there are some strengths, such as average quality measures, the overall picture shows significant weaknesses that families should consider.
- Trust Score
- D
- In Maryland
- #137/219
- Safety Record
- Moderate
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 49% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ⚠ Watch
- $37,265 in fines. Higher than 80% of Maryland facilities, suggesting repeated compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 32 minutes of Registered Nurse (RN) attention daily — about average for Maryland. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 75 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Maryland average (3.0)
Below average - review inspection findings carefully
Near Maryland avg (46%)
Higher turnover may affect care consistency
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 75 deficiencies on record
May 2025
30 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, it was determined that the facility failed to provide privacy to a resident during a dressin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, pertinent document review and interviews, it was determined that the facility failed to have an effective ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on record review and interviews, it was determined that the facility failed to ensure that Beneficiary Protection Notifications were issued to residents discharged from Medicare Part A services ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and observation it was determined that the facility failed to maintain a clean home-like environment. This w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on record review and interviews, it was determined that the facility failed to identify a Grievance Official in the facility's grievance policy, and failed to ensure that grievances were followe...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on a record review and interview it was determined that the facility failed to report a resident's allegation of missing money. This was evident for 1 (Resident #263) and was discovered during t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on record review, interviews, and observation, it was determined that the facility failed to ensure that Minimum Data Set (MDS) assessments were accurately recorded. This was evident for 2 (Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on pertinent document review and interviews, it was determined that the facility failed to perform a Pre-admission Screening and Resident Review (PASSAR) screen within 40 days of the resident ad...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, it was determined that the facility failed to develop and implement a baseline care plan...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, it was determined that the facility failed to develop and implement a comprehensive care...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on record review and interviews, it was determined that the facility failed to ensure that care plans were reviewed and revised after a change in a resident's condition. This was evident for 1 (...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on record reviews, interviews and observations, it was determined that the facility failed to ensure that residents who required assistance with Activities of Daily Living (ADL) were provided wi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review, and interviews, it was determined that the facility failed to ensure that medications and treatments were administered per physician orders. This was evident in 1 (Resident #36...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on pertinent document review and interviews, it was determined that the facility failed to provide treatment for a pressur...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on Interview and record review, it was determined that the facility failed to have an effective process in place to ensure...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, it was determined that the facility failed to provide proper urinary catheter care. This was evident for 1 (Resident #108) reviewed during the initi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews and interviews, it was determined that the facility failed to have an order in place for o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on review of employee files and staff interviews, it was determined that the facility failed to conduct annual nursing staff performance reviews ensuring competencies in their skills. This was e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on review of Geriatric Nursing Assistant (GNA) personnel files and staff interview, it was determined that the facility staff failed to conduct yearly performance reviews and ensure twelve (12) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on record reviews and interviews, it was determined that the facility failed to ensure that a controlled substance logbook was signed by 2 licensed staff at change of shifts. This was evident fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews, it was determined that the facility failed to ensure that the attending physician reviewed irregularities identified by the pharmacist, acted upon them i...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on records review and interviews, it was determined that the facility failed to ensure non-pharmacological interventions were provided or attempted prior to administering a psychotropic medicati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations and record reviews, it was determined that the facility failed to ensure medications were stored and labeled properly as evidenced by failing to discard expired medications and f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, observation and pertinent document review, it was determined that the facility failed to have a process in p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review, observation, and staff interview, it was determined that the facility failed to ensure care documentation was accurate. This was evident for 1 (Resident #108) of 4 residents re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, it was determined that the facility failed to ensure infection prevention and control practices were followed when 1) an unlabeled, uncovered bedpan ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
Based on interview and observation it was determined that the facility failed to maintain a Residents shower rooms in good repair. This was evident for 1 out of 2 resident shower rooms observed during...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected 1 resident
2) On 4/24/25 at 2:43 PM, the review of Intake # MD00211246 revealed an allegation of employee to resident abuse.
4/24/25 04:33 PM The Director of Human Resources (Staff #37) provided the employee fil...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected 1 resident
Based on a record review of a facility reported incident, employees' file and staff interviews, it was determined that the facility failed to ensure Geriatric Nurse Assistants (GNA's) received trainin...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4) On 4/24/25 at 2:43 PM, a review of Intake # MD00211246 revealed an allegation of employee to resident abuse. Further review r...
Read full inspector narrative →
Nov 2023
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on medical record review and interview, it was determined that the facility failed to ensure that residents were safe from accidents during mechanical lift transfers which resulted in harm to re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to ensure that their residents were free of misappropriation of property as evidenced by a staff member taking a reside...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0680
(Tag F0680)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to employ a qualified Activity Director. This was evident for 1 of 1 Activity Director.
The findings include:
On 11/14...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, it was determined that the facility failed to provide a resident quality care based on sta...
Read full inspector narrative →
Oct 2021
29 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observations and interviews, it was determined that the facility failed to ensure that residents received their meals in a timely manner. This was found to be evident for 2 (resident # 349 & ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Based on review of medical records, facility documentation and interviews, it was determined that the facility failed to ensure residents were free from misappropriation of property as evidenced by th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined that the facility failed to have an effective system in pl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews, it was determined that the facility failed to provide evidence of the implementation of an ongoing program of activities that met the needs of Residents ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, record reviews and interviews, it was determined the facility failed to ensure the safety of the resident by not implementing fall precautions. This was found to be evident for 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview with facility staff, it was determined that a facility physician failed to include ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview and review of records and policies, it was determined that the facility failed to 1) ensure that counts of controlled substances were completed by two nurses at the cha...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility staff failed to ensure that residents were not prescribed unnecessary medication as evidenced by a physician's order for pain ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that facility staff failed to ensure that a resident's medication regimen was free of unnecessary psychotropic medications as evid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation and medical record review, it was determined that the facility failed to ensure a medication error rate of less than 5% as evidenced by the identification of 3 errors out of 31 op...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
2) An observation of Resident #84's hands wasmade during an interview with Resident #84 on 10/4/21 at 9:27 AM. Resident #84's hands were contracted on both sides.
A medical record review on 10/12/21 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, it had been determined that the facility failed to ensure that Geriatric Nursing Assistants (GNA) had the required 12 hours of in-service training based on ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor observation and resident interview, it was determined that the facility failed to provide a safe, clean, comfo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 6) On 10/8/21 at 8:07 AM review of the facility investigation documentation for facility-reported incident (FRI) MD00156190 reve...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0608
(Tag F0608)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** J) A review of the facility's policy and procedure regarding abuse it was noted that the policy was a guide to what the facility...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 10) On 10/15/2021 at 7:00 am, the Surveyor reviewed the facility self-report for resident #88 for allegations of abuse that was ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 6) On 10/15/2021 at 7:00 am, review of the Facility Reported Incident (FRI) revealed documentation that resident #88 told the As...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4) Review of Resident #95's medical record on 10/13/21 at 9:33 AM revealed that the resident was admitted to the facility on [DA...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) A medical record review for Resident #62 on 10/4/21 at 12:42 PM, revealed a history and physical that had been completed by t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4) A tracheostomy is a hole in your windpipe that a doctor makes to help you breathe. The doctor usually puts a tracheostomy tub...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
Based on review of medical records and other pertinent documentation, and interview, it was determined that the facility failed to ensure that nursing staff did not erroneously document the administra...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident and staff interview, and medical record review , it was determined the facility failed to ensure ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
2) During a facility tour on 10/4/21 8:48 AM, the surveyor observed the nurse (staff #21) walk away from his/her assigned medication cart into the dining area. The medication cart was sitting across t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) During a tour conducted on 10/04/2021 at 8:32 am on the Covid-19/Observation Nursing unit Catoctin. The Surveyor observed Ger...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
Based on observations and interviews with staff, it was determined that the facility failed to ensure that residents had a means of directly contacting staff. This was evident for 2 showers in the Sug...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected most or all residents
Based on record review and staff interview, it was determined that the facility failed to have a process in place to ensure that nurse aides were receiving performance evaluations annually and that in...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0741
(Tag F0741)
Could have caused harm · This affected most or all residents
Based on record review and staff interview, it was determined that the facility failed to provide training to staff related to mental and psychosocial disorders that affected residents with trauma and...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on observation, record review, and staff interview, it was determined that the facility staff failed to document and calculate nurse staffing information daily basis, therefore had not retained ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0838
(Tag F0838)
Minor procedural issue · This affected most or all residents
Based on review of facility records and interview with staff, it was determined that the facility failed to conduct and document an accurate facility-wide assessment as evidenced by the failure to pro...
Read full inspector narrative →
Sept 2018
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor observation and interview with staff, it was determined that the facility staff failed to maintain bedroom and...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
2) Review of Resident #100's modification of admission MDS (minimal data set), with an assessment reference date (ARD) of 9/2/18, revealed that Section O, 0100. Special Treatments, Procedures, and Pro...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, medical record review and staff interview, it was determined that the facility failed to develop and implement comprehensive person-centered care plans. This was evident for 1 (#...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined the facility failed to timely act on a pharmacy recommendation. This was evident for 1 (#16) of 5 residents reviewed for unnecessa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and staff interview, it was determined that facility staff failed to store medication according to professional standards. This was evident for 1 of 3 medication carts observed.
...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on review of the medical record and facility documentation and interview with facility staff, it was determined that the facility failed to maintain complete and accurately documented medical re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) On 9/11/18 at 12:01 PM, an observation of room [ROOM NUMBER]'s shared bathroom revealed there was a clear, plastic graduated ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
3) Review of Resident #16's medical record on 9/17/18 revealed a physician's order that was written on 7/30/18 which stated Eliquis 2.5 mg (milligrams) bid (2 times per day) for afib (atrial fibrillat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on surveyor observation and interview with staff, it was determined that the facility staff failed to ensure that the refrigerators and freezer in the kitchen were maintained in safe operating c...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected most or all residents
Based on review of Geriatric Nursing Assistant (GNA) personnel files and staff interview, it was determined the facility failed to conduct yearly performance reviews at least every 12 months for 6 out...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor observation and interview with facility staff, it was determined that the facility staff failed to store, prep...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0809
(Tag F0809)
Minor procedural issue · This affected multiple residents
Based on review of facility records and interview with staff, it was determined that the facility failed to provide meals with no more than 14 hours between a substantial evening meal and breakfast th...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • 75 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $37,265 in fines. Higher than 94% of Maryland facilities, suggesting repeated compliance issues.
- • Grade D (40/100). Below average facility with significant concerns.
About This Facility
What is Autumn Lake Healthcare At Glade Valley's CMS Rating?
CMS assigns AUTUMN LAKE HEALTHCARE AT GLADE VALLEY an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Autumn Lake Healthcare At Glade Valley Staffed?
CMS rates AUTUMN LAKE HEALTHCARE AT GLADE VALLEY's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 49%, compared to the Maryland average of 46%. RN turnover specifically is 59%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Autumn Lake Healthcare At Glade Valley?
State health inspectors documented 75 deficiencies at AUTUMN LAKE HEALTHCARE AT GLADE VALLEY during 2018 to 2025. These included: 1 that caused actual resident harm, 71 with potential for harm, and 3 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
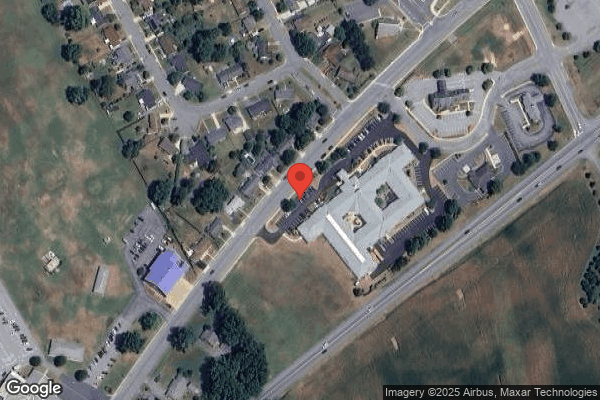
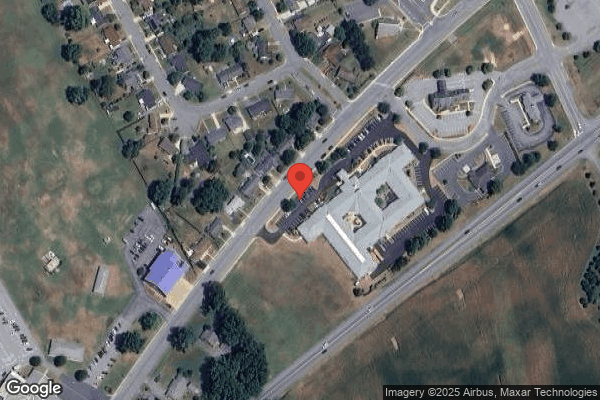
Who Owns and Operates Autumn Lake Healthcare At Glade Valley?
AUTUMN LAKE HEALTHCARE AT GLADE VALLEY is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by AUTUMN LAKE HEALTHCARE, a chain that manages multiple nursing homes. With 124 certified beds and approximately 110 residents (about 89% occupancy), it is a mid-sized facility located in WALKERSVILLE, Maryland.
How Does Autumn Lake Healthcare At Glade Valley Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, AUTUMN LAKE HEALTHCARE AT GLADE VALLEY's overall rating (2 stars) is below the state average of 3.0, staff turnover (49%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Autumn Lake Healthcare At Glade Valley?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Autumn Lake Healthcare At Glade Valley Safe?
Based on CMS inspection data, AUTUMN LAKE HEALTHCARE AT GLADE VALLEY has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Maryland. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Autumn Lake Healthcare At Glade Valley Stick Around?
AUTUMN LAKE HEALTHCARE AT GLADE VALLEY has a staff turnover rate of 49%, which is about average for Maryland nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Autumn Lake Healthcare At Glade Valley Ever Fined?
AUTUMN LAKE HEALTHCARE AT GLADE VALLEY has been fined $37,265 across 1 penalty action. The Maryland average is $33,452. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Autumn Lake Healthcare At Glade Valley on Any Federal Watch List?
AUTUMN LAKE HEALTHCARE AT GLADE VALLEY is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.