HELLENIC NURSING & REHABILITATION CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Hellenic Nursing & Rehabilitation Center in Canton, Massachusetts has a Trust Grade of D, indicating below average performance with some significant concerns. It ranks #157 out of 338 facilities in the state, placing it in the top half but still indicating there is room for improvement. The facility is on an improving trend, with issues decreasing from 22 in 2023 to 13 in 2024. Staffing is a notable strength, rated at 5 out of 5 stars with a low turnover rate of 17%, suggesting that staff are experienced and familiar with the residents. However, there are concerning incidents reported, including a failure to adequately assess and manage a resident's pain following a fall, which resulted in a serious fracture requiring hospitalization. Another resident with advanced dementia did not receive timely pain management, reflecting potential gaps in care standards. While there are some strengths, families should weigh these serious deficiencies when considering this facility for their loved ones.
- Trust Score
- D
- In Massachusetts
- #157/338
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ✓ Good
- 17% annual turnover. Excellent stability, 31 points below Massachusetts's 48% average. Staff who stay learn residents' needs.
- Penalties ✓ Good
- $7,901 in fines. Lower than most Massachusetts facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 40 minutes of Registered Nurse (RN) attention daily — about average for Massachusetts. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 67 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Staffing Rating · Excellent nurse staffing levels
-
Low Staff Turnover (17%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (17%)
31 points below Massachusetts average of 48%
Facility shows strength in staffing levels, staff retention, fire safety.
The Bad
Near Massachusetts average (2.9)
Meets federal standards, typical of most facilities
Below median ($33,413)
Minor penalties assessed
The Ugly 67 deficiencies on record
Aug 2024
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure that residents and/or their representatives were fully informed in advance and given information necessary to make health care decis...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure the Physician/Practitioner was notified of a change in treatment for one Resident (#17), out of a total sample of 27 residents. Spec...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observations and interviews, the facility failed to maintain a clean, safe, comfortable, and homelike environment for the residents at the facility, for 1 of 3 nursing units.
Findings includ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure staff developed a baseline or comprehensive care plan within 48 hours of the resident's admission, which included the instructions n...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and records reviewed for two Residents (#35 and #52), out of 27 sampled residents, the facili...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review, the facility failed to ensure residents were provided care in accordance wi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide the necessary care and services to attain or maintain the highest practicable physical, mental, and psychosocial well...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to provide an ongoing program of individual and group activities designed to meet the interests of and support the physical, mental and psychoso...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure residents were free from accident hazards for two Residents (#32 and #62), out of a total sample of 27 residents. Spec...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interview, the facility failed to monitor adverse consequences (side effects) of anticoagulant medications (used to prevent the blood from clotting; a blood ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure one Resident's (#56) drug regimen was free from unnecessary psychotropic medications, out of a total sample of 27 residents. Specifi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure staff implemented dialysis care and services consistent with professional standards of practice for one Resident (#10), out of 27 sa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to store, prepare and serve food in accordance with professional standar...
Read full inspector narrative →
Jun 2023
19 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to provide a dignified existence for one Resident (#16), out of a total ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
2. Resident #54 was admitted to the facility in March 2020 with diagnoses which included cognitive communication deficits, major depressive disorder recurrent, moderate and adjustment disorder, unspec...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on observations, interviews, policy review, and record review, the facility failed to provide meal choices and preferences for one Resident (#27), out of a total sample of 26 residents.
Finding...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
2. Resident #54 was admitted to the facility in March 2020 with diagnoses including hemiplegia and hemiparesis following cerebral infarction affecting the left non-dominant side and cognitive communic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interviews, the facility failed to revise the plan of care related to advanced directives for one Resident (#451), out of a total sample of 26 residents.
Fin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
2a. Resident #4 was admitted to the facility in November 2022 with diagnoses including right fibula fracture, diabetes and heart disease.
Review of the Minimum Data Set (MDS) assessment, dated 4/16/2...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interview, the facility failed to ensure quality care was provided to one Resident (#4...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, policy review, and interviews, the facility failed to ensure that routine devices (hearing...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interview, record review, and policy review, the facility failed to follow the Weight Surveillance policy for one Resident (#87), out of a total sample of 26 residents. Specifica...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
2. Review of the facility's policy titled Administering Medications through a Small Volume (Handheld) Nebulizer, undated, indicated the purpose of this procedure is to safely and aseptically administe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interviews, the facility failed to ensure that pharmacy recommendations were reviewed and addressed for three Residents (#21, #12, and #86), out of a total s...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observations, record reviews, policy review, and interviews, the facility failed to ensure it was free from a medication error rate of greater than 5 percent. Two out of four nurses observed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure one Resident (#4) was free from a significant medication err...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations, policy review, and interviews, the facility failed:
1. To ensure medications were stored securely in 2 out of 4 resident care units, and
2. To ensure medications with shortened...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interview, the facility failed to ensure they maintained a complete and accurate medical record for one Resident (#4), out of a total sample of 26 residents....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on record review, policy review, and interview, the facility failed to ensure that concerns addressed by the Resident Council Group have sufficient follow-up to address and prevent recurrence.
...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected multiple residents
Based on observation, record review, policy review, and interview, the facility failed to ensure four Residents (#75, #46, #31, and #21) were free from restraints, out of a total sample of 26 resident...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2b. Resident #54 was admitted to the facility in March 2020 with diagnoses including dysphagia, hemiplegia and hemiparesis follo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations, policy review, and interviews, the facility failed to store food in sanitary conditions, specifically, label and date leftover food items and dispose of food items after their u...
Read full inspector narrative →
Apr 2023
2 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0658
(Tag F0658)
A resident was harmed · This affected 1 resident
Based on records reviewed and interviews for one of three sampled residents (Resident #1), who during December 2022 was noted to have increased pain during rehabilitation therapy session which continu...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
Based on records reviewed and interviews for one of three sampled residents (Resident #1), who on 12/09/22 had experienced a fall from his/her wheelchair, the Facility failed to ensure that after Reha...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of three sampled residents (Resident #1), the Facility failed to ensure staff implemented and followed their Abuse policy, when on 12/13/22 during the...
Read full inspector narrative →
May 2021
32 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interview, record review, and policy review, the facility failed to recognize, re-evaluate and ensure tre...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on policy review, and resident and staff interviews, the facility failed to ensure that residents' rights were protected and promoted when the facility failed to adhere to the smoking schedule, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review, and staff interview, the facility failed to ensure that advanced directive information fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to ensure that staff notified the attending physician of continued weight loss of one Resident (#1B), with a recent history of significant we...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to ensure that a notice of transfer or discharge was provided to the resident and/or the resident's representative and to a representati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to ensure that the resident or resident representative was informed of the facility's bed hold policy and received written notification ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on record review and staff interviews, the facility failed to review and revise the comprehensive care plan for two Residents (#4 and #24), out of a total of 21 sampled residents. Specifically, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, record review, and staff interview, the facility failed to ensure staff obtained a physician's order for respiratory care and services according to accepted standards of clinical...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure that residents were provided an environment that was free from accident hazards on 1 unit (Dementia Special Care Unit/DSCU) out of 3 u...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed for one Resident (#1B), who had been identified as having had unplanned weight loss prior to admission, and remained at risk for weight loss, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure standards of practice for a resident receiving dialysis ser...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review, the facility failed to ensure that nursing staff possessed the specific com...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0741
(Tag F0741)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and record review, the facility failed to ensure that staff had the skills necessary to provide appropriate dementia care services for one Resident (#18) out of 29 re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview, and policy review, the facility failed to ensure medications were available and accessible to meet the needs of one Resident (#85) out of a total sample of 21 resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review and staff interviews, the facility failed to ensure that for two Residents (#24 and #25) psychotropic medications were accurately monitored to prevent the use of unnecessary med...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to ensure that for two Residents (#18 and #66), out of a total sample of 21 residents, that each resident's drug regimen was free of unn...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and staff interview, the facility failed to ensure that medication error rates were five pe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, record review, and staff interview, the facility failed to ensure that medications were stored at proper temperatures to preserve their integrity in 1 out of 4 medication room re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and test trays, the facility failed to ensure that food was served in a manner that was palata...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, staff interviews, and policy review, the facility failed to ensure that staff prepared and served food under sanitary conditions in the main kitchen.
Findings include:
Review of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on policy review, staff and resident interviews, and review of Resident Council Minutes, the facility failed to ensure that residents' right to participate in resident groups in the facility was...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. For Resident #191, the facility failed to ensure that a comprehensive person-centered care plan was developed and implemented...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected multiple residents
5) Review of Resident #21's MDS assessment, dated 1/28/21, indicated that the Resident required total dependence for bed mobility.
On 4/28/21 at 9:09 A.M., the surveyor observed Resident #21 lying in...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected multiple residents
5) Review of Resident #21's MDS assessment, dated 2/14/21, indicated that the Resident was receiving hospice services.
Review of the physician's order, dated 2/5/21, indicated Resident #21 be evaluat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure that seven Residents (#4, #21, #31, #40, #66, #74, #77), out of a total sample of 21 residents, were screened for and provided (if a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on observations and staff interview, the facility failed to ensure that all mechanical, electrical, and patient care equipment was in safe operating condition on 1 (Dementia Special Care Unit (D...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected most or all residents
Based on policy review, employee education documentation, and staff interviews, the facility failed to ensure that abuse training for all facility staff includes all components of the abuse policy. Sp...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on record review and staff interview, the facility failed to designate a person who met the minimum qualifications to serve as a director of food and nutrition services to ensure the function of...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected most or all residents
Based on document review and staff interview, the facility failed to conduct and accurately document a facility-wide assessment to determine what resources are necessary to care for its residents. Spe...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observations, interviews, record review, and policy review, the facility failed to establish and maintain an infection prevention and control program designed to provide a safe, sanitary, and...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected most or all residents
Based on documentation review and staff interview, the facility failed to ensure that staff developed a system to conduct inspections of residents' bed rails and mattresses and that manufacturers' rec...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0637
(Tag F0637)
Minor procedural issue · This affected multiple residents
Based on record review and staff interview, the facility failed to complete a Significant Change in Status Assessment within the required time frame of 14 days for one Resident (#40) that was admitted...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 17% annual turnover. Excellent stability, 31 points below Massachusetts's 48% average. Staff who stay learn residents' needs.
- • Multiple safety concerns identified: 3 harm violation(s). Review inspection reports carefully.
- • 67 deficiencies on record, including 3 serious (caused harm) violations. Ask about corrective actions taken.
- • Grade D (48/100). Below average facility with significant concerns.
About This Facility
What is Hellenic Nursing & Rehabilitation Center's CMS Rating?
CMS assigns HELLENIC NURSING & REHABILITATION CENTER an overall rating of 3 out of 5 stars, which is considered average nationally. Within Massachusetts, this rating places the facility higher than 99% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Hellenic Nursing & Rehabilitation Center Staffed?
CMS rates HELLENIC NURSING & REHABILITATION CENTER's staffing level at 5 out of 5 stars, which is much above average compared to other nursing homes. Staff turnover is 17%, compared to the Massachusetts average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Hellenic Nursing & Rehabilitation Center?
State health inspectors documented 67 deficiencies at HELLENIC NURSING & REHABILITATION CENTER during 2021 to 2024. These included: 3 that caused actual resident harm, 63 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Hellenic Nursing & Rehabilitation Center?
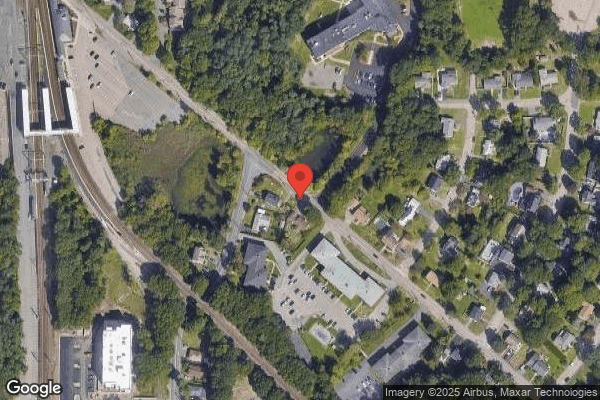
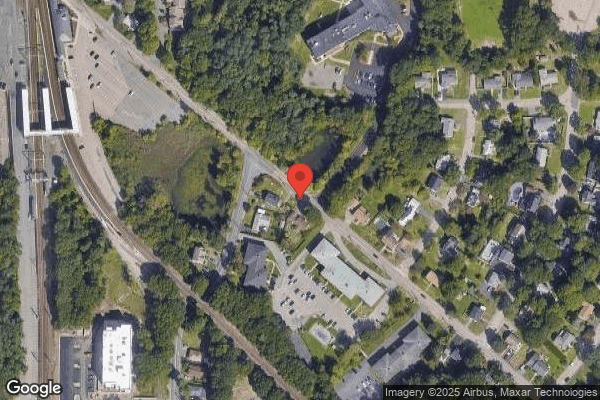
HELLENIC NURSING & REHABILITATION CENTER is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 154 certified beds and approximately 106 residents (about 69% occupancy), it is a mid-sized facility located in CANTON, Massachusetts.
How Does Hellenic Nursing & Rehabilitation Center Compare to Other Massachusetts Nursing Homes?
Compared to the 100 nursing homes in Massachusetts, HELLENIC NURSING & REHABILITATION CENTER's overall rating (3 stars) is above the state average of 2.9, staff turnover (17%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Hellenic Nursing & Rehabilitation Center?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Hellenic Nursing & Rehabilitation Center Safe?
Based on CMS inspection data, HELLENIC NURSING & REHABILITATION CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in Massachusetts. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Hellenic Nursing & Rehabilitation Center Stick Around?
Staff at HELLENIC NURSING & REHABILITATION CENTER tend to stick around. With a turnover rate of 17%, the facility is 28 percentage points below the Massachusetts average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly. Registered Nurse turnover is also low at 20%, meaning experienced RNs are available to handle complex medical needs.
Was Hellenic Nursing & Rehabilitation Center Ever Fined?
HELLENIC NURSING & REHABILITATION CENTER has been fined $7,901 across 1 penalty action. This is below the Massachusetts average of $33,158. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Hellenic Nursing & Rehabilitation Center on Any Federal Watch List?
HELLENIC NURSING & REHABILITATION CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.