MEDWAY COUNTRY MANOR SKILLED NURSING & REHABILITAT



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Medway Country Manor Skilled Nursing & Rehabilitation has received a Trust Grade of F, indicating significant concerns about the facility's quality of care. It ranks #299 out of 338 nursing homes in Massachusetts, placing it in the bottom half of facilities statewide, and #30 out of 33 in Norfolk County, meaning there are only two options in the county that are worse. The facility has shown some improvement, reducing its reported issues from 24 in 2024 to 6 in 2025, but it still suffers from a concerning staffing turnover rate of 61%, which is much higher than the state average of 39%. Additionally, the home has incurred $242,885 in fines, suggesting repeated compliance issues, and has less registered nurse coverage than 87% of facilities in the state, which limits the quality of care. Specific incidents include staff not using proper personal protective equipment for residents requiring special precautions, and delays in notifying physicians about critical lab results regarding infectious diseases, which potentially put other residents at risk. While there are some signs of improvement, the facility has serious weaknesses that families should carefully consider.
- Trust Score
- F
- In Massachusetts
- #299/338
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 61% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $242,885 in fines. Lower than most Massachusetts facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 21 minutes of Registered Nurse (RN) attention daily — below average for Massachusetts. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 89 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Licensed Facility · Meets state certification requirements
-
No fines on record
This facility meets basic licensing requirements.
The Bad
Below Massachusetts average (2.9)
Significant quality concerns identified by CMS
15pts above Massachusetts avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
13 points above Massachusetts average of 48%
The Ugly 89 deficiencies on record
Feb 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents (Resident #1), who had moderate cognitive impairmen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of three sampled residents (Resident #1), who had moderate cognitive impairment and was dependent on staff to meet his/her care needs, the Facility fa...
Read full inspector narrative →
Jan 2025
4 deficiencies
4 IJ (4 facility-wide)
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0726
(Tag F0726)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
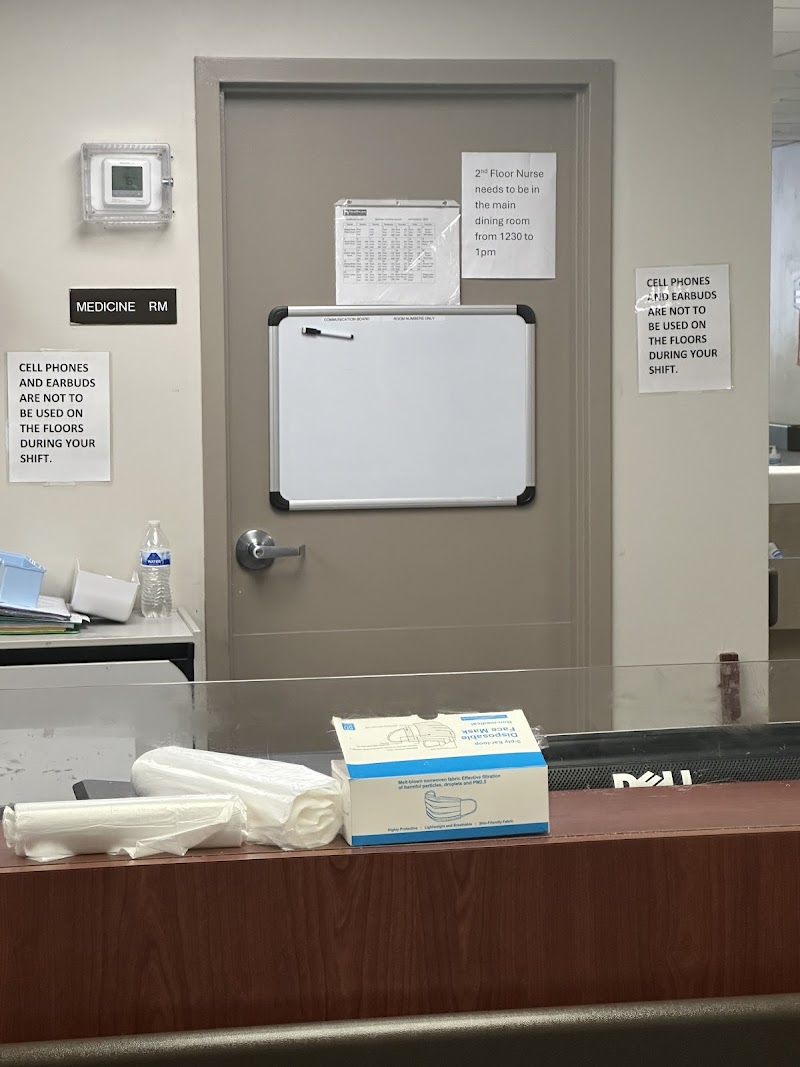
Based on observations, records reviewed and interviews, for three of seven sampled residents (Resident #3, Resident #5, Resident #6), who required transmission based precautions to be utilized by nurs...
Read full inspector narrative →
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0773
(Tag F0773)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews for one of seven sampled residents (Resident #1), who per Laboratory test results repor...
Read full inspector narrative →
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
Based on records reviewed and interviews, for two of three nursing units (West and Second) after a staff member Certified Nurse Aide (CNA) #1 tested positive for Group A Streptococcal (GAS, a bacteriu...
Read full inspector narrative →
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Infection Control
(Tag F0880)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, records reviewed and interviews for five of seven sampled residents (Resident #1, Resident #2, Resident #...
Read full inspector narrative →
Nov 2024
20 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to develop and implement an individualized, person-centered care plan to meet the physical, psychosocial, and functional needs f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and records reviewed for one Resident (#42) of 22 sampled residents, the facility failed to e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record review, the facility failed to ensure wound treatments were conducted for one Resident (#353), in a total sample of 22 residents. Specifically, for Reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and records reviewed for one Resident (#66) of 22 sampled residents, the facility failed to ensure that pain management was provided to the Resident consistent with ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interviews, the facility failed for one Resident (#48), out of a total sample of 22 residents, to ensure professional standards of care and treatment for hemod...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to assess and eliminate triggers for a Resident (#99) with a history of trauma, to avoid potential re-traumatization, out of a total sample of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on document review and interview, the facility failed to ensure the monthly medication regimen review (MRR) reports for two Residents (#51 and #68), out of a total sample of 22 residents, were i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and records reviewed for one Resident (#42) of 22 sampled residents, the facility failed to ensure the Resident's drug regimen was free from unnecessary drugs and wa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure one Resident's (#51) drug regimen was free from unnecessary psychotropic medications, out of a total sample of 22 residents. Specifi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure it was free from a medication error rate of greater than five percent when one of two nurses made three errors out of ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and policy review, the facility failed to ensure drugs and biologicals were stored in accordance with accepted professional principles of practice. Specifically, the f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0924
(Tag F0924)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, the facility failed to ensure the handrail in the corridor of the [NAME] Unit was secured ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0712
(Tag F0712)
Could have caused harm · This affected multiple residents
2. Resident #66 was admitted to the facility in August 2024.
Review of the Physician's Progress Notes indicated Resident #66 was seen by the MD on 8/7/24. The next visit was conducted on 8/26/24. The...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected multiple residents
Based on observation, record review, interviews, and review of the facility assessment, the facility failed to provide sufficient support personnel with appropriate competencies and skills to safely a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected multiple residents
C. Resident #19 was admitted to the facility in December 2023 with diagnoses including dementia and dysphagia.
Review of the M assessment, dated 9/17/24, indicated Resident #19 was severely cognitive...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to follow professional standards of practice for food safety and sanitat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
Based on record review and staff interviews, the facility failed to ensure that pneumonia vaccines were administered to 12 Residents (#29, #53, #8, #54, #24, #85, #91, #17, #79, #19, #353, #63) with s...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected most or all residents
Based on observation, interview, and documentation review, the facility failed to ensure nursing staff were able to demonstrate the appropriate competencies and skill sets for 4 out of 5 licensed nurs...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected most or all residents
Based on employee record review and interview, the facility failed to complete performance reviews of Certified Nursing Assistants (CNAs) at least once every 12 months and provide regular in-service e...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected most or all residents
Based on staff interview and record review, the facility failed to ensure the Certified Nursing Assistants (CNA) completed the required 12 hours (no less than) of annual training, which at a minimum m...
Read full inspector narrative →
Jul 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of three sampled residents (Resident #1), who was diagnosed with dementia, had an activated Health Care Proxy, and had physicians orders for the admin...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents (Resident #1), after facility staff were made aware...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of three sampled residents (Resident #1), the Facility failed to ensure that after an administrative staff member (Director of Nurses) was made aware ...
Read full inspector narrative →
Jan 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Transfer
(Tag F0626)
Could have caused harm · This affected 1 resident
Based on interviews and records reviewed, for one of three sampled residents (Resident #1), who was a long-term care resident without any discharge plans, the Facility failed to permit Resident #1 to ...
Read full inspector narrative →
Aug 2023
4 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Notification of Changes
(Tag F0580)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents (Resident #1), who was admitted to the Facility wit...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents (Resident #1), who was admitted to the Facility wit...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents (Resident #1), who upon admission was assessed to b...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews for three of three sampled residents (Resident #1, Resident #2 and Resident #3), the Fa...
Read full inspector narrative →
Aug 2023
24 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on observation, record review, and staff interview, the facility failed to identify and assess the use of locking a wheelchair and placing mobile residents at the table as a potential restraint ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on policy review, record review, and interview, the facility failed to ensure staff implemented the facility's abuse policy for one Resident (#60), of a total sample of 28 residents. Specificall...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to identify and complete a Significant Change in Status Minimum Data Set assessment (MDS) assessment for one Resident (#18), who...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interview, the facility failed to develop and implement an effective person-centered baseline care plan within 48 hours of admission to the facility for one ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interviews, the facility failed to develop and implement care plans for two Residents (#36 and #14), out of a total sample of 28 residents. Specifically, the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure that the care plan for one Resident (#84) was reviewed and revised by an interdisciplinary team to include new interve...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
2. Review of the facility's policy titled Administering Medications, revised 4/19, indicated the following:
-The following information is checked/verified for each resident prior to administering medi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
2. Resident #18 was admitted to the facility in November 2022 with diagnoses including edema, restlessness and agitation, and cognitive decline.
Review of the most recent MDS assessment, dated 5/30/2...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #64 was admitted to the facility in March 2023 with diagnoses including peripheral vascular disease, urine retention...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and policy review, the facility failed to properly manage the enteral tube feeding for one Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, policy review, and record review, the facility failed to provide care and maintenance of a peripherally inse...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
2. Review of the facility's policy titled Oxygen Administration, dated as revised October 2010, indicated the following:
-Verify that there is a physician's order for this procedure.
-Review the phy...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to ensure there was ongoing communication and collaboration with the dialysis facility regarding dialysis care and services for one Resident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interviews, the facility failed to implement a trauma informed care plan for one Resident (#36), out of a sample of 28 residents. Specifically, the facility ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on observation, record review, policy review, and interview, the facility failed to ensure two Nurses (#2 and #3) were competent and had the required skill set to prepare and administer the corr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on records reviewed, policy review, and interviews, the facility failed to ensure that as needed (PRN) orders for psychotropic medications are limited to 14 days unless the prescribing practitio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
2. On 8/8/23 at 9:48 A.M., the surveyor and Nurse #4 observed a box of Solanpas on Resident #19's bedside table. Nurse #4 said that Resident #19 likes his/her Solanpas kept at the bedside and he/she l...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, policy review, and interview, the facility failed to a) store food, and b) handle food, in accordance with professional standards for food service safety.
Findings include:
The...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interview, the facility failed to ensure the facility developed a hospice plan of care as required for one Resident (#18), out of a total sample of 28 reside...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on record review, policy review, and interviews, the facility failed to ensure that concerns addressed by the Resident Council Group had sufficient follow-up to address and prevent recurrence. S...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
3. Resident #64 was admitted to the facility in March 2023 with diagnoses including peripheral vascular disease, urine retention, diabetes, and hemiplegia.
Review of the most recent MDS assessment, d...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observations, records reviewed, policy review, and interviews, the facility failed to ensure it was free from a medication error rate of greater than 5% when 3 out of 4 nurses observed made 4...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
2. Review of the facility's policy titled Administering Medications, dated as revised April 2019, indicated medications are administered in a safe and timely manner and as prescribed.
23. As required...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
Based on record reviews, policy review, and staff interview, the facility failed to provide education, assess for eligibility, and offer pneumococcal vaccines (help prevent pneumococcal disease) for t...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on interviews and records reviewed, for two of three sampled residents (Residents #1 and #2) the Facility failed to ensure staff implemented and followed the Facility Abuse, Neglect, Exploitatio...
Read full inspector narrative →
Jan 2023
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
Based on records reviewed and interviews, for one of three sampled residents (Resident #1), who was receiving Hospice Services due to end of life care needs, the Facility failed to ensure that based o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interviews and records reviewed, for one of three sampled residents (Resident #1) who was found to have new areas of bruising on at least two separate occasions, the Facility failed to ensure...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents, (Resident #1), who had a physician order dated 11/...
Read full inspector narrative →
Jun 2022
27 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure residents and/or their representatives were fully informed in advance and given information necessary to make health care decisions ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on policy review, record review, and interview, the facility failed to ensure staff implemented written policies and procedures for an allegation of abuse. Specifically, the facility failed to e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on policy review, record review, and interview, the facility failed to ensure staff reported an allegation of unwanted kissing between two residents to the Department of Public Health (DPH) with...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on policy review, record review, and interview, the facility failed to ensure staff thoroughly investigated an allegation of unwanted kissing between two residents for one Resident (#64), out of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
3.) Resident #64 was admitted to the facility in November 2020 with diagnoses that included chronic obstructive pulmonary disorder (COPD), anxiety, and dementia with behavioral disturbance.
Review of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
2.) Resident #4 was admitted to the facility in August 2020 with diagnoses that included end stage renal disease and on dialysis, diabetes, and diabetic retinopathy.
Review of the Minimum Data Set (MD...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, interview, record review, and policy review, the facility failed to ensure Residents were provided care in accordance with professional standards of practice for three Residents ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to implement and follow the physician's orders for bladder scans to monitor for urine retention and to obtain a urine osmolality test, resulti...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on policy review, observation, medical record review, and interview, the facility failed to ensure that respiratory equipment was managed in accordance with professional standards of practice fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure the bed was reassessed for entrapment and the bed dimensions were appropriate after the bed mattress was removed and replaced with an ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interviews, the facility failed to ensure that antibiotics were not administered without adequa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record review, the facility failed to ensure that one Resident (#69), was free from significant medication errors, out of a total sample of 21 residents. Specifi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and staff interview the facility failed to maintain medical records that are complete, accurate and systemically organized within accepted professional standards and practice fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
3. Resident #63 was admitted to the facility in July 2020 with diagnoses including dementia, abnormal weight loss, and moderate protein-calorie malnutrition.
Review of the Minimum Data Set (MDS) asses...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observations, interview, and policy review, the facility failed to establish and maintain an infection prevention and control program designed to prevent the development and potential transmi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0910
(Tag F0910)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure one Resident's (#43) room had a functioning toilet for the Resident's comfort and privacy.
Findings include:
During an interview on 6/...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #63 was admitted to the facility in July 2020 with diagnoses including dementia, abnormal weight loss, and moderate ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
5. Resident #70 was re-admitted to the facility in May 2022 with diagnoses including depression and anxiety.
Review of the May 2022 Physician's Orders indicated a new order for Ativan 0.5 mg twice a ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2.) Review of the facility's policy titled Falls-Clinical Protocol, revised April 2007, indicated the staff will evaluate and do...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
On 06/13/22 at 04:30 P.M., the first-floor treatment cart to the right of the nurses' station was observed to be unlocked and unsupervised.
Based on observation and interview, the facility failed to ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to:
1. Allow residents to make individualized meal choi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interviews, the facility failed to maintain a safe and sanitary kitchen environment consistent with professional standards. Specifically, the facility failed to:
1.) Ensure th...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on record review and interviews, the facility failed to define, implement, and maintain a comprehensive quality assurance and performance improvement (QAPI) plan to address the full range of car...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0885
(Tag F0885)
Could have caused harm · This affected most or all residents
Based on interviews and document review, the facility failed to ensure staff followed the Centers for Medicare and Medicaid Services (CMS) published final rule, updated 9/10/21, for Long Term Care (LT...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected most or all residents
Based on interview, policy review, and record review, the facility failed to conduct COVID-19 outbreak testing in a manner consistent with professional standards of practice. Specifically, the facilit...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected most or all residents
Based on policy review, observations, and interviews, the facility
1. Failed to regularly inspect all bed frames, mattresses, and bed rails in the facility for possible risk of entrapment since March ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0888
(Tag F0888)
Minor procedural issue · This affected most or all residents
Based on policy review and interview, the facility failed to ensure the facility policy and procedures related to staff COVID-19 vaccinations included all the Federal requirements.
Findings include: ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 4 life-threatening violation(s), Special Focus Facility, 3 harm violation(s), $242,885 in fines. Review inspection reports carefully.
- • 89 deficiencies on record, including 4 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $242,885 in fines. Extremely high, among the most fined facilities in Massachusetts. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Medway Country Manor Skilled Nursing & Rehabilitat's CMS Rating?
CMS assigns MEDWAY COUNTRY MANOR SKILLED NURSING & REHABILITAT an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Massachusetts, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Medway Country Manor Skilled Nursing & Rehabilitat Staffed?
CMS rates MEDWAY COUNTRY MANOR SKILLED NURSING & REHABILITAT's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 61%, which is 15 percentage points above the Massachusetts average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 76%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Medway Country Manor Skilled Nursing & Rehabilitat?
State health inspectors documented 89 deficiencies at MEDWAY COUNTRY MANOR SKILLED NURSING & REHABILITAT during 2022 to 2025. These included: 4 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 3 that caused actual resident harm, 81 with potential for harm, and 1 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Medway Country Manor Skilled Nursing & Rehabilitat?
MEDWAY COUNTRY MANOR SKILLED NURSING & REHABILITAT is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by SHIMON LEFKOWITZ, a chain that manages multiple nursing homes. With 123 certified beds and approximately 110 residents (about 89% occupancy), it is a mid-sized facility located in MEDWAY, Massachusetts.
How Does Medway Country Manor Skilled Nursing & Rehabilitat Compare to Other Massachusetts Nursing Homes?
Compared to the 100 nursing homes in Massachusetts, MEDWAY COUNTRY MANOR SKILLED NURSING & REHABILITAT's overall rating (1 stars) is below the state average of 2.9, staff turnover (61%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Medway Country Manor Skilled Nursing & Rehabilitat?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the facility's high staff turnover rate, and the below-average staffing rating.
Is Medway Country Manor Skilled Nursing & Rehabilitat Safe?
Based on CMS inspection data, MEDWAY COUNTRY MANOR SKILLED NURSING & REHABILITAT has documented safety concerns. Inspectors have issued 4 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility is currently on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes nationwide). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Massachusetts. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Medway Country Manor Skilled Nursing & Rehabilitat Stick Around?
Staff turnover at MEDWAY COUNTRY MANOR SKILLED NURSING & REHABILITAT is high. At 61%, the facility is 15 percentage points above the Massachusetts average of 46%. Registered Nurse turnover is particularly concerning at 76%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Medway Country Manor Skilled Nursing & Rehabilitat Ever Fined?
MEDWAY COUNTRY MANOR SKILLED NURSING & REHABILITAT has been fined $242,885 across 4 penalty actions. This is 6.8x the Massachusetts average of $35,508. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Medway Country Manor Skilled Nursing & Rehabilitat on Any Federal Watch List?
MEDWAY COUNTRY MANOR SKILLED NURSING & REHABILITAT is currently an SFF Candidate, meaning CMS has identified it as potentially qualifying for the Special Focus Facility watch list. SFF Candidates have a history of serious deficiencies but haven't yet reached the threshold for full SFF designation. The facility is being monitored more closely — if problems continue, it may be added to the official watch list. Families should ask what the facility is doing to address the issues that led to this status.