HANCOCK PARK REHABILIATION AND NURSING CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Hancock Park Rehabilitation and Nursing Center has a Trust Grade of D, indicating below-average performance with some concerns about care quality. It ranks #156 out of 338 in Massachusetts, placing it in the top half of facilities in the state, and #17 out of 33 in Norfolk County, meaning there are few better local options. The facility appears to be improving, reducing issues from 9 in 2023 to 7 in 2024. Staffing is relatively stable with a turnover rate of 33%, which is better than the state average, and it has average RN coverage. However, there are some troubling incidents, including failure to provide necessary interventions for a resident's deteriorating pressure injury and inadequate nutritional support for another resident that led to significant weight loss. While there are strengths in staffing stability and a decent quality measure rating, the facility does face serious challenges that families should consider.
- Trust Score
- D
- In Massachusetts
- #156/338
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ○ Average
- 33% turnover. Near Massachusetts's 48% average. Typical for the industry.
- Penalties ⚠ Watch
- $33,348 in fines. Higher than 89% of Massachusetts facilities, suggesting repeated compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 31 minutes of Registered Nurse (RN) attention daily — about average for Massachusetts. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 36 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (33%)
15 points below Massachusetts average of 48%
Facility shows strength in quality measures, fire safety.
The Bad
Near Massachusetts average (2.9)
Meets federal standards, typical of most facilities
13pts below Massachusetts avg (46%)
Typical for the industry
Below median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 36 deficiencies on record
Oct 2024
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
Based on observation, record review, interview, and policy review, the facility failed to ensure the proper care and treatment of a peripherally inserted intravenous (IV) line device (a thin flexible ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure staff implemented dialysis care and services consistent with professional standards of practice for two Residents (#47 and #32), out...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and policy review, the facility failed to ensure all drugs and biologicals were stored in a safe and secure manner as required. Specifically, the facility failed for o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
Based on record review, hospice contract review, and staff interview, the facility failed to ensure for one Resident (#23), out of a total sample of 24 residents, hospice services were provided in acc...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure a resident with pressure ulcers received necessary treatment and services, consistent with professional standards of practice, to pr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on interviews and review of facility menus, the facility failed to ensure a repetitive menu was not provided to the residents resulting in complaints about the lack of variety in food options. S...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to follow professional standards of practice for food safety and sanitation to prevent the potential spread of foodborne illness to residents wh...
Read full inspector narrative →
Oct 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews for one of three sampled residents (Resident #1) who had a physician's order dated 9/27/23, for nursing to obtain a urine sample for a suspected urinary tract ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews for one of three sampled residents (Resident #1) who had a physician's order dated 9/27/23, for nursing to obtain a urine sample for a suspected urinary tract ...
Read full inspector narrative →
Jul 2023
7 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
Based on observation, record review, and interview, the facility failed to implement treatment interventions for a deep tissue injury (DTI- a pressure-related injury to subcutaneous tissues under inta...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, record review, policy review, and interview, the facility failed to ensure dignity was maintained for residents on the Four East Unit, out of a total of six nursing care units.
F...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on observation, record review, policy review, and interview, the facility failed to ensure an injury of unknown source was reported to facility administration and the State Agency for one Reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #328 was re-admitted to the facility in July 2023 with diagnoses including right hip fracture and multiple skin tear...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
3. Resident #1 was admitted to the facility in February 2022 with unspecified atrial fibrillation, chronic obstructive pulmonary disease, and acute respiratory failure.
Review of Resident #1's most re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observations, record reviews, policy review, and interviews, the facility failed to ensure it was free from a medication error rate of greater than 5 percent. Two out of four nurses observed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations, policy review, and interviews, the facility failed to ensure medications with shortened expiration dates were labeled and dated after being opened for 2 out of 3 medication cart...
Read full inspector narrative →
Aug 2021
20 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
Based on observations, records reviewed, and interviews, the facility failed to ensure that timely interventions were identified and provided for one Resident (#54), based on the comprehensive assessm...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interview, the facility failed to implement their policy for Advance Directives for two Residents (#13 and #80), out of a total sample of 24 residents. Speci...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to notify the physician of a weight increase of four pounds in a 24 hour period, per the physician's orders, for one Resident (#48), out...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0603
(Tag F0603)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and records reviewed, the facility failed to ensure the staff did not involuntarily seclude one Resident (#105), out of a sample of 24 residents.
For Resident #105,...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review, staff interview, and observation, the facility failed to complete a restraint assessment ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observations, interview, and record review, the facility failed to implement the plan of care and provide 1 to 8 supervision during meal times for one Resident (#13), out of a total sample of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
2. Resident #105 was admitted to the facility in October 2019.
Review of the physician's orders for Resident #105 included an order for Depo-Provera (contraceptive injection) 150 milligrams per millil...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0675
(Tag F0675)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record review the facility failed to ensure one Resident (#105), out of a sample of 24 residents, was provided an environment to enhance a sense of well-being an...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to provide two Residents (#105 and #49), out of a tota...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure one Resident (#61) with a pressure ulcer received necessary treatment and services, consistent with professional standards of practi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0691
(Tag F0691)
Could have caused harm · This affected 1 resident
Based on record review, observations, and interviews, the facility failed to ensure staff adhered to professional standards of care for a resident with a nephrostomy (an opening in the back that allow...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide the necessary respiratory care and services in accordance with professional standards of practice and the medical pla...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on record reviews and interviews, the facility failed to ensure that residents who require dialysis receive such services, consistent with professional standards of practice, through ongoing com...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0741
(Tag F0741)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review, the facility failed to ensure staff had the skills necessary to provide beh...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure proper storage and disposal of medications in the medication cart.
Findings include:
On 08/11/21 at 12:26 P.M., the surveyor inspected...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation, interviews, and 2 out of 3 test tray results, the facility failed to ensure foods provided to all residents were appetizing and served at palatable temperatures.
Findings includ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected multiple residents
Based on observations, interviews, policy review, and review of meal schedule times, the facility failed to ensure residents on all six units are offered an evening snack and that the time span betwee...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected multiple residents
Based on interview and review of personnel files and training documentation, the facility failed to ensure 2 Employees (#3 and #5) out of 6 employees were provided with training on dementia management...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0680
(Tag F0680)
Could have caused harm · This affected most or all residents
Based on interviews and review of the Activity Director's personnel file, the facility failed to ensure the activity program was directed by a qualified activities professional.
Findings include:
On ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
2. On 8/12/21 at 8:22 A.M., the surveyor observed a laboratory person in a resident's room. The signs outside of the resident's room indicated the resident is on quarantine/ Transmission-Based Precaut...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 33% turnover. Below Massachusetts's 48% average. Good staff retention means consistent care.
- • 36 deficiencies on record, including 2 serious (caused harm) violations. Ask about corrective actions taken.
- • $33,348 in fines. Higher than 94% of Massachusetts facilities, suggesting repeated compliance issues.
- • Grade D (45/100). Below average facility with significant concerns.
About This Facility
What is Hancock Park Rehabiliation And Nursing Center's CMS Rating?
CMS assigns HANCOCK PARK REHABILIATION AND NURSING CENTER an overall rating of 3 out of 5 stars, which is considered average nationally. Within Massachusetts, this rating places the facility higher than 99% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Hancock Park Rehabiliation And Nursing Center Staffed?
CMS rates HANCOCK PARK REHABILIATION AND NURSING CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 33%, compared to the Massachusetts average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Hancock Park Rehabiliation And Nursing Center?
State health inspectors documented 36 deficiencies at HANCOCK PARK REHABILIATION AND NURSING CENTER during 2021 to 2024. These included: 2 that caused actual resident harm and 34 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Hancock Park Rehabiliation And Nursing Center?
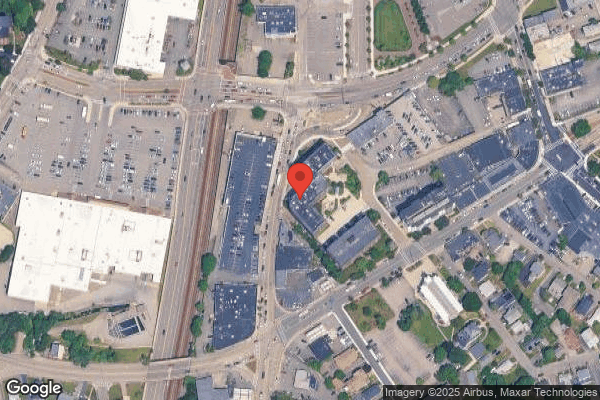
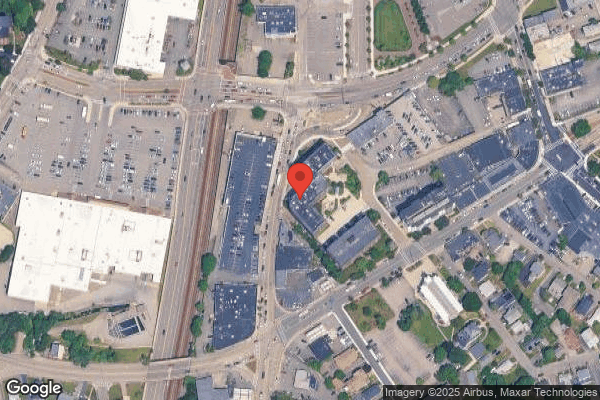
HANCOCK PARK REHABILIATION AND NURSING CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by BANECARE MANAGEMENT, a chain that manages multiple nursing homes. With 142 certified beds and approximately 124 residents (about 87% occupancy), it is a mid-sized facility located in QUINCY, Massachusetts.
How Does Hancock Park Rehabiliation And Nursing Center Compare to Other Massachusetts Nursing Homes?
Compared to the 100 nursing homes in Massachusetts, HANCOCK PARK REHABILIATION AND NURSING CENTER's overall rating (3 stars) is above the state average of 2.9, staff turnover (33%) is significantly lower than the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Hancock Park Rehabiliation And Nursing Center?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Hancock Park Rehabiliation And Nursing Center Safe?
Based on CMS inspection data, HANCOCK PARK REHABILIATION AND NURSING CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in Massachusetts. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Hancock Park Rehabiliation And Nursing Center Stick Around?
HANCOCK PARK REHABILIATION AND NURSING CENTER has a staff turnover rate of 33%, which is about average for Massachusetts nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Hancock Park Rehabiliation And Nursing Center Ever Fined?
HANCOCK PARK REHABILIATION AND NURSING CENTER has been fined $33,348 across 1 penalty action. This is below the Massachusetts average of $33,412. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Hancock Park Rehabiliation And Nursing Center on Any Federal Watch List?
HANCOCK PARK REHABILIATION AND NURSING CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.