CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to MI00145581.
Based on interview and record review, the facility failed to prevent the elopement and ens...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to MI00145581.
Based on interview and record review, the facility failed to prevent the elopement and ensure the safety in 1 of 2 residents (Resident #305) reviewed for elopements, resulting in an Immediate Jeopardy when on 6/13/2024 at approximately 8:34 PM, Resident #305, who was cognitively impaired exited the facility by facility staff when he was mistaken for a visitor and traveled on foot along a busy road with a speed limit of 40 miles per hour looking for his sister. Resident #305 was found by community members who returned him to facility staff who were searching for him and they brought him back to the facility. This deficient practice placed Resident #305 and other residents identified as at risk for elopement at risk for serious harm, injury, and/or death.
Findings include:
Review of the Face Sheet and Minimum Data Set (MDS) dated [DATE] revealed R305 admitted to the facility on [DATE] with diagnoses of mild cognitive impairment and psychomotor agitation (unintentional and purposeless motions and restlessness sometimes accompanied by emotional distress). Brief Interview for Mental Status (BIMS) reflected a score of 5 out of 15 which indicated R305 was severely cognitively impaired (00 to 07 is severe cognitive impairment).
Review of the Elopement and Wandering Residents Policy with an Implementation Date of 3/2008 and a Review/Revision Date of 5/2024 revealed Policy Explanation and Compliance Guidelines: 5. The facility shall establish and utilize a systematic approach to monitoring and managing residents at risk for elopement or unsafe wandering, including identification and assessment of risk, evaluation and analysis of hazards and risks, implementing interventions to reduce hazards and risks, and monitoring for effectiveness and modifying interventions when necessary. 6. Monitoring and Managing Residents at Risk for Elopement or Unsafe Wandering: a. Residents will be assessed for risk of elopement and unsafe wandering upon admission and throughout their stay.
Review of Agency Licensed Practical Nurse (LPN) II's progress noted dated 6/13/2024 after R305's elopement revealed, At 8:48pm the writer was alerted by staff that the resident mentioned was not in his room and had been let outside of the building around 30 minutes prior. He was seen going north bound in the parking lot towards Forest Hill Ave. The elopement protocol was initiated and the writer vocalized to the staff that she was going to start heading north and go east down Forest Hill Ave while the other staff headed west in search of said resident. Meanwhile the remaining staff accounted for all other residents in the building and did and all clear to ensure that (R305) was the only one unaccounted for. While heading eastbound on forest hill ave the writer spotted the resident on the corner of [NAME] Dr SE and Forest Hill Ave with two individuals. The writer approached the group and identified herself. The individuals stated that he was confused and tried to enter their home. He was able to call his sister from the male's cell phone and the two parties agreed to meet at Forest Hills Food at 9pm. They were heading there when I approached them. The writer thanked them for their help and both the writer and resident returned to the facility. Once at the facility the writer accessed the resident for injuries and pain. The resident denied any pain and reported being hot and tired.
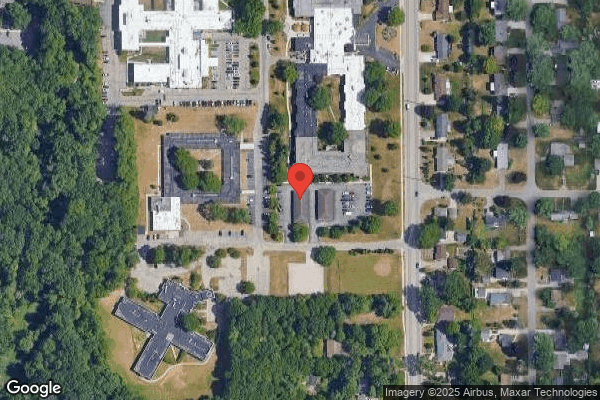
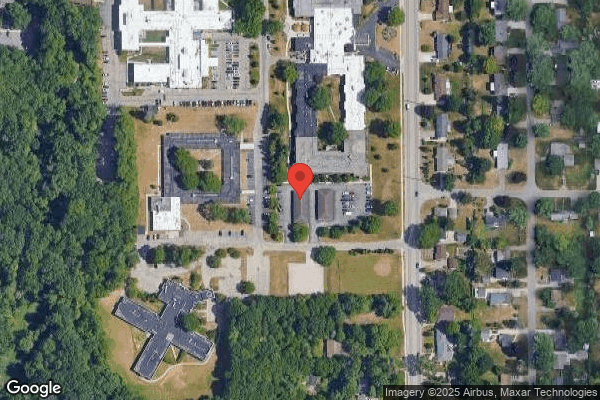
In an observation on 7/11/2024 at 4:15 PM, noted the route that R305 took was from the parking lot at the facility going north and uphill to main road which was a busy road with a speed limit of 40 mph. R305 then headed East to where the sidewalk ended approximately 0.25 miles down. R305 walked down to the road approximately 0.6 miles away from the facility unsupervised until community members found him.
During an interview on 7/12/2024 at 11:48 AM, Licensed Practical Nurse (LPN) DD stated that on 6/13/2024 she stayed over to complete Relias training (educational training) since she was still in orientation. LPN DD said that she clocked out at 8:34 PM and was getting ready to go out the door when staff sitting at the nurse's station asked her to let 2 gentlemen out of the facility. She stated that she knew one was a resident who was going out to smoke and the other one she didn't know (R305) and assumed he was okay to let out since staff told her to let him out.
During an interview on 7/12/2024 at 10:58 AM, Certified Nursing Assistant (CNA) D stated that she came in on 6/13/2024 around 7 PM and around 8:15/8:30 PM, R305 approached her at the nurses' station and asked her to call his sister because he wanted to know if she was coming in later that night. CNA D said she called R305's sister and his sister said she wasn't coming in that night and would be in the next morning. CNA D stated that R305 walked back to his room and that was the last time she saw him. Then, approximately 15 to 20 minutes later a code search was implemented for R305.
During an interview on 7/12/2024 at 2:39 PM, CNA BB stated on 6/13/2024 she was doing her Relias training at the nurses' station when R305 went up to her and said he needed to go to the hospital. CNA BB said she thought R305 was a visitor and was going to see family at the hospital. She noticed at that time that LPN DD was leaving and asked if she was leaving and then saw R305 go out with her.
During an interview on 7/12/2024 at 3:10 PM, CNA E stated on 6/13/2024 she was doing her Relias training at the nurses' station Relias with CNA BB when she saw LPN DD and a man (R305) leaving with her. CNA E said that she didn't know he was a resident until 30 minutes later when she found out he was a resident and was missing. CNA E stated that R305 was missing for 20 to 30 minutes before anyone realized he was missing.
Review of the Admission/readmission assessment dated [DATE] under Section D. Safety/Fall Risk revealed that R305 had a history of falls and fell in the last month prior to admission at the facility. Under Section E. Elopement Risk Assessment showed that R305 didn't have any elopement attempts at previous residence, didn't have a history of wandering at previous residence and didn't have 1 or more attempts to elope in the last 90 days. Under 6. Behavioral Symptoms, a. Intrudes into other resident rooms. Has delusions, such as need to go out and [NAME] the lawn; Expressions of confusion, Fear, Disorientation; Short attention span; Excessive motor activity; Wanders was checked yes. Under 7. Other Diagnosis Affecting Cognitive Status or Memory, a. Dementia, Depression, Anxiety, Delusional Disorder, mental Illness, Closed Head Injury, Other was checked yes. Under 9. Elopement Risk a. Is the Resident At Risk for Elopement? was checked no.
Review of the Elopement Risk assessment dated [DATE] after R305 eloped under 1. History of Wandering and/or Elopement revealed d. Resident has made one (1) or more attempts to elope from either previous or current residence in the last 90 days was checked yes. Under 9. Elopement Risk a. Based upon the assessment above, the resident is determined to be at risk for elopement? was checked yes.
Review of the Inpatient Bedside Nurse Warm Handover to Subacute Nurse form that is completed by the nurse for all new admissions prior to admission from discharging facility revealed a section at the bottom titled safety risks.
During an interview on 7/12/2024 at 10:04 AM, Registered Nurse (RN) T stated that prior to admission a report is received from the hospital and they fill out the Inpatient Bedside Nurse Warm Handover to Subacute Nurse form to make sure all information is captured prior to admission. RN T said that elopement risk wasn't brought up with R305 from the hospital and hasn't been brought up since she has worked at the facility or with any new admits prior to R305 eloping.
During an interview on 7/12/2024 at 2:36 PM, Director of Nursing B stated that she wasn't sure if she could find the Inpatient Bedside Nurse Warm Handover to Subacute Nurse form for R305. DON B also stated that they had wander guards available in the facility prior to 6/13/2024 if they needed to put one on a resident.
Review of Practitioner Progress notes dated 6/14/2024 completed by Nurse Practitioner (NP) YY revealed, Patient is seen today by provider following admission to facility. Medications, labs, nursing notes, and plan of care reviewed with patient and nursing. Extensive time spent reviewing patient and plan of care with IDT and nursing. Pt arrived to facility on 6/13/24 and shortly there after eloped from the facility. Pt was found and returned to the facility unharmed. Review of hospital paperwork showed elopement behaviors upon initial arrival to hospital, suspected to be d/t change (due to) of environment, but did not continue throughout hospital stay.
During an interview on 7/16/2024 at 9:49 AM, NP YY stated that the day after R305 eloped they had a IDT (interdisciplinary team) and the team was looking into R305's elopement and someone found information about his elopement behaviors at the hospital. NP YY said that elopement risk wasn't on the referral from the hospital since it happened initially at the hospital and not afterwards otherwise, they would have discussed the change of environment at the facility and put interventions into place.
During an interview on 7/12/2024 at 2:36 PM, Nursing Home Administrator (NHA) A stated that Social Worker Advocate (SWA) C was the only one in the facility that has access to EPIC (hospital electronic medical record). NHA A stated that SWA C was able to find R305's hospital notes in EPIC regarding his elopement behaviors at the hospital.
During an interview on 7/16/2024 at 10:03 A, SWA C stated that she found R305's hospital notes through EPIC the day after R305's elopement since they were discussing R305 at IDT and she started digging into his notes and found that he had elopement behaviors. SWA C said that she looks at EPIC with discharge planning and for her profession only. SWA C stated that the facility has an admissions team off site that gives information to nursing and should be doing a thorough review prior to admitting a resident.
On 7/12/2024 at 9:18 AM, NHA A was notified of an Immediate Jeopardy that began on 6/13/2024 when R305 exited the facility when he was mistaken for a visitor.
On 7/12/2024, this surveyor verified the facility completed the following to remove the Immediate Jeopardy. The Abatement was accepted on 7/12/2024 at 4:04 PM.
1.
R305 was placed on a 1:1 supervision upon return to the facility. - 6/13/24
2.
Employee placed on administrative leave. - 6/13/24. Upon return from administrative leave, this staff member was provided 1:1 education on the elopements and wandering residents policy.
3.
All newly admitted residents that have a guardian or activated DPOA were identified as being at risk for this deficient practice. - 6/13/24
4.
All resident's elopement risk assessments reviewed and any identified elopement risks residents that were currently residing in the facility were reviewed to ensure appropriate interventions were in place. - 6/13/24
5.
External door checks were completed by the Administrator. - 6/13/24
6.
All-staff re-education was initiated. - 6/13/24
7.
On 6/13/24, education was completed to all-staff on elopement and wandering residents policy was initiated; any facility staff member and agency staff member who did not receive education by 6/13/24 will receive education prior to the start of their next shift. All facility staff and agency staff who were present at the time of the incident were immediately educated. As of 6/13/24, all facility staff and agency staff have completed the necessary required education. Education is completed for all new hires prior to their next shift.
8.
Administrator/designee audited daily door alarms checks as of 6/13/2024 to ensure proper functioning of the egress and wander guard system. The audits have been conducted weekly for four weeks and then monthly for two months.
9.
Elopement drill has been completed on 06/26/2024 and 06/17/2024.
10.
Director of Nursing/designee audited new admission elopement risk assessments as of
6/13/2024 to ensure proper interventions have been placed if a resident triggers as an elopement risk and to verify a wander guard is in place for the first 7-days if the resident has a legal decision maker. The audit has been conducted weekly for four weeks and then monthly for two months.
During an interview on 7/12/2024 at 1:56 PM, NHA A stated that door alarm checks are supposed to be done daily by maintenance and someone is delegated on weekends/holidays. While reviewing the daily door alarm checks it was noticed that several days were missed and not checked and NHA A said that he audits the door alarm checks weekly and knows there are holes on the sheets. NHA A stated that someone is delegated on weekends and holidays to do door alarm checks, usually a housekeeper who failed to do it and maintenance failed to check and make sure he handed it down to the housekeeper. NHA A was unable to find sheets for the missing days in the maintenance office.
Although the immediate jeopardy was removed on 7/12/2024, the facility remained out of compliance with a scope of isolated and severity of no actual harm with the potential for more than minimal harm that is not immediate jeopardy due to daily door alarm checks not being completed and sustained compliance had not yet been verified by the state agency.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0760
(Tag F0760)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to Intake MI00145186
Based on interview, and record review, the facility failed to ensure residents were...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to Intake MI00145186
Based on interview, and record review, the facility failed to ensure residents were free from significant medication errors in 1 of 1 resident (R404) reviewed for medication administration resulting in an Immediate Jeopardy when, beginning on 5/23/2024 at approximately 7:46 AM, R404 was administered another residents medications and was found unresponsive. Resident #404 was hospitalized in the ICU (Intensive Care Unit - provides care and life support for acutely ill/injured patients) on BiPAP (Bilevel Positive Airway Pressure - a device that helps with breathing) with a Narcan drip (a medication used to treat an opioid overdose) and the likelihood of further life-threatening deterioration in his medical condition.
Findings include:
Review of facility policy, Medication Administration-General Guidelines dated June 2019, revealed, Medications are administered as prescribed in accordance with good nursing principles and practices .The Five Rights (Right Resident, Right Drug, Right Dose, Right Route, and Right Time) are applied for each medication being administered .12. Medications supplied for one resident are never administered to another resident .
Review of Licensed Practical Nurse (LPN) WW written statement by proxy of Nursing Home Administrator (NHA) A dated 5/23/24 at 1030 AM, indicated she had dispensed (prepped) and administered morning medications to R404 at approximately 7:30 AM. The resident had been in the Garden room and was noted to be tired with his head on a tray table. At approximately 7:45 AM LPN WW prepped R7's medications and handed the cup of medications to LPN XX and told him the room number. LPN WW stated she was unclear if she had given LPN XX the wrong room number or if he had heard her wrong but at approximately 8:35 AM R7 reported to her that he had not received his 8:00 AM medications. LPN WW informed R7 that he had received his medications, however, R7 continued to insist that he had not. LPN WW asked LPN XX if he had administered R7's to him and LPN XX stated, A bigger guy? LPN WW stated, No, that is not (R7). The medication error was reported to the former Unit Manager/Clinical Care Coordinator (UM/CCC) VV who gave direction to complete an incident report with exact times and to notify the Medical Director (MD). Nurse Practitioner (NP responded with orders to monitor R404's vital signs (VS) every 6 hours x (for) 24 hours.
Review of LPN XX written statement by proxy of NHA A dated 5/23/24 at approximately 11:45 AM, indicated he offered to run the medications for LPN WW. When LPN WW handed him the medications for R7 she told him These are for (R7's first name which was the same first name as R404) and when he asked for a room number, LPN WW responded room [ROOM NUMBER]. LPN XX stated when he entered room [ROOM NUMBER], he spoke to a resident and asked if he was the man with the first name he was given. The resident responded to the name. The LPN then informed R404 that he had his medications, and the resident did not dispute taking them.
Review of LPN WW written statement by proxy of NHA A dated 5/23/24 at 2:27 PM, gave further clarification on the incident that happened earlier in the day involving R404 and other residents. LPN WW indicated she had prepped medications for three residents with LPN XX administering them. LPN WW stated LPN XX had administered medications to the remainder of the residents on the 300 Hall. LPN WW stated all residents on the 400 Hall she had prepped medications and administered with LPN XX. LPN WW then stated immediately upon identifying the medication error of R404, she and LPN XX the facility stopped having her prepping medications and LPN XX administering them.
Review of LPN XX written statement by proxy of NHA A dated 5/29/24 4:01 PM indicated the LPN did not remember if R404 had already received his medications and that he had not given the resident his medications twice. The LPN verified he had shown LPN WW which resident he had given R7's to.
Review of LPN WW written statement by proxy of NHA A dated 5/29/24 at 4:06 PM, indicated she verified only LPN XX had administered medications once to R404 She also stated she and LPN XX did walk to R404's room in order to show her which resident he gave medications to.
R404
According to the Minimum Data Set (MDS), dated [DATE], R404 scored 15/15 (cognitively intact) on his BIMS (Brief Interview Mental Status).
Review of R404's Medication Administration Record/Treatment Administration Record (MAR/TAR) dated 5/23/24 at 8:00 AM indicated Licensed Practical Nurse (LPN) WW documented administration of:
-allopurinol 100 mg 1 tablet by mouth for gout
-glipizide ER (extended release) 10 mg 1 tablet by mouth
-lisinopril-hydrochlorothiazide 10-12.5 mg 1 tablet by mouth for hypertension
-multivitamin men 50+ 1 tablet by mouth for supplement
-apixaban (blood thinner) 5 mg by mouth for Afib
-metformin HCL 1000 mg 1 tablet my mouth for diabetes
This indicated Resident #404 had received his ordered morning medications.
R7
According to the Minimum Data Set (MDS), dated [DATE], R7 scored 13 /15 (cognitively intact) on his BIMS (Brief Interview Mental Status).
Review of R7's MAR/TAR dated 5/23/24 indicated at 8:00 AM, LPN WW indicated documented administration of:
-Gabapentin 400 mg 1 capsule by mouth for neuropathy
-methocarbamol 500 mg 2 tablets by mouth for muscle spasms/phantom pain
-aspirin 81 mg by mouth for prophylaxis (preventative)
-lotrel 5-20 mg 1 capsule by mouth for hypertension
-Miralax17 grams by mouth for constipation
-Apixaban (blood thinner) 5 mg 1 tablet by mouth for prophylaxis
-hydromorphone HCL (dilaudid) 4 mg by mouth for chronic pain
-levetiracetam 750 mg 2 tablets by mouth for seizure disorder
-lidocaine External gel 4% topically for right shoulder pain
Review of facility medication administration audit received 7/12/24 at 11:27 AM, indicated on 5/23/24 LPN WW signed out medications with LPN XX having administered them:
-7:36 AM to resident in room [ROOM NUMBER] bed 1
-7:41 AM to resident in room [ROOM NUMBER] bed 1
-7:46 AM to R7 (incident involving R404 received the medication not R7)
-7:52 AM to resident in room [ROOM NUMBER] bed 1
During an interview on 7/10/24 at 3:38 PM, R7 stated, The facility overdosed the guy in the room across the hall from me a while back. The staff gave him my meds (medications). He was not my roommate. They (nurses/facility) were worried about their own asses and not the man they overdosed.
During an interview on 7/11/24 at 2:10 PM, LPN WW stated, I worked at the facility for a little over a month by 5/23/24. I kinda sorta had orientation when I started. It consisted of a walk-through of the facility. There was no orientation on policy. I have been a nurse since 2002. I know the rights of medication (meds) administration. On May 23 rd (2024), I was passing meds with an agency nurse (LPN XX). We were working out of the same med cart. I gave (LPN XX) medications I had pulled to give to (R7). I do not know if I gave the LPN the wrong room number or he heard me wrong, but he gave the wrong person the wrong meds. Once (R7) came to the med cart and said he did not get his morning meds, (LPN XX) and I went looking for the resident that got (R7's) medications. (LPN XX) told me did not give the meds to (R7). I had been pulling meds that morning and (LPN XX) was giving them. I was working behind because the med pass was heavy and falling behind. I delegated the meds to (LPN XX) because I was getting behind, I was a newer nurse to the facility. (LPN XX) just started to work that morning. (LPN XX) was learning the residents and so was I. When a nurse pulls up the MAR it tells you the resident's room number and gives their picture. There was also a printed sheet with resident room numbers. I knew I did wrong by pulling the medications and having the other LPN administer them. The meds were given by (LPN XX) around 8:30 AM. (R7) came to the med cart around 8:30 AM asking for his meds. I told him he already got them, and he argued with me. (LPN XX) said he gave the meds to a bigger guy (R404) and I told him that was not (R7). I gave (R404) his meds at 7:30 AM in the Garden Room. He was drowsy and laying across a bedside table. I had a hard time waking him, he took the meds, and went back to sleep. I left him there. (R404) was not in a wheelchair. He must have walked back to his room where (LPN XX) found him and gave him (R7's) meds. When (R404) was found in his room later that morning by (LPN XX and I. He was sitting in a chair. He was alert and (LPN XX) verified he had given (R7's) medication to (R404). We went immediately to (Unit Manager (UM) VV) reporting the wrong meds had been given to the wrong person. I went back to passing meds at the same med cart. The DON (Director of Nursing) came to see me about 20-30 minutes later and sent me home.
During an interview on 7/11/24 at 2:43 PM, LPN XX stated, I am an agency LPN. I have been a nurse for 17 years. May 23 rd (2024) was my first day at the facility. I did not get any orientation. The first day I arrived, I was paired up (LPN WW) who was in her orientation process. We decided she would pull meds and I would pass them. (R404) was about the 4th resident we did this together. (LPN WW) would tell me the resident name and room number and I repeated it back to her and she would say yes. After the incident with (R404) we maybe did 5 more residents the same way. (R7) came up to the med cart saying he had not gotten his meds yet that morning. (LPN WW) told him we had given him his meds already. I told her that I had not given medications to (R7). (LPN WW and I found (R404) and she told me he was the wrong resident. We told the Unit Manager right away that we had a med error. The Unit Manager told us to call the doctor who told us to monitor (R404) and do vital signs (VS) every 4 hours. I got a first set a VS on (R404) who was stable. We went back to the med cart and on to the next resident where she passed meds and I watched. The Unit Manager told me to go sit with (R404) and do vital signs every 15 minutes. The second time VS were taken (R404) was slurring his speech and lethargic. I told a CNA (certified nursing assistant) to get the Unit Manager. The doctor came to the room, ordered Narcan, and it was administered. (R404) responded and then started to decline. A second Narcan was ordered and 911 was called. (R404) came around but was confused. EMS (Emergency Medical Services) arrived and gave oxygen. The resident's POX (oxygen level) was in the high 80s. 87-90. I do not know what the medications I gave him. I know the 5 Rights of Medication Administration. I did the best of my ability May 23 rd. I took the meds and went to what I though was (R7's) room. (R404) responded when and went into the room. I did not pull the meds. I watched the MAR as (LPN WW) pulled meds and saw a first name but not a picture in the medical record. I watched the LPN pull a med out of the narcotic (controlled substance) drawer, but I did not look at what med it was or the name on the card. I do not know what meds were pulled. I was told by the Unit Manager the facility normally does have names on room doors or wrist bands. He did not have on a wrist band, a name on the room door, or a picture in medical record. I know better than to administer medications the way I did. A nurse new to a facility should never orient with a nurse that is on orientation too. Ever.
During an interview on 7/11/24 at 3:35 PM, R404 stated, I was a resident at the facility in May (2024). I went to the room that was a lounge that morning, was given my medications by a lady, who said she was a nurse then I went back to my room. About 5 minutes later a man nurse came to my room and called out my first name. I said my first name. He did not ask me my last name. He said he had meds for me. I said I got my meds a short time ago by the lady nurse. He said the meds were mine. He said he had been a nurse for about 25 years and should know how to pass meds and that he knew they were my meds. He insisted he had my medications. I got tired of arguing with the nurse. He should have checked my ID. I still had the hospital bracelet on from the day before. I took the medications he insisted were mine. The next thing I knew I was in the hospital. I was told I was unresponsive. I was given something to work against the meds. I remember I thought I was in some kind of fantasy world because of the wrong meds. I groped the nurse and that was not me. I apologized to the nurse. Once I got out of the ER (emergency room) and they put me in ICU (intensive care unit). Then I was sent back to the nursing home for two weeks and finally went home. I originally went to the nursing home because I had Afib. And was sent to rehab at the nursing home.
During an interview on 7/12/24 at 9:00 AM, NHA A stated, I do not know all of the medications that (R404) was given. I did not know (R404) got a muscle relaxer that was meant for (R7).
During an interview on 7/12/24 at 9:15 AM, Director of Nursing (DON) B stated, I do the staff training. (LPN WW) worked here for almost a month when the incident happened. She had a couple of mentors. I never saw her orientation check list. I do not know what the mentors documented on it about her. She needed more time to learn the flow of the building and. It was not the intention to have (LPN XX) pass medications with her. It was his first day. He was to be doing treatments and new admissions if any came in. He did not have an orientation check list. Agency are on their own when come to work at the facility.
Review of R404's Practitioner Progress Note dated 5/23/24 at 1:54 PM, revealed, .called to see new resident urgently this morning due to hypoxia and altered mental status .had inadvertently been given the medication of a different resident. These included dilaudid, Gabapentin, and Keppra (muscle relaxant) .breathing more shallow, less responsive, and diaphoretic (sweating) .was not able to speak .gave Narcan 4 mg nasally .pulse weakened .given second dose of Narcan .lungs with crackles and decreased breath sounds lower half .heart irregular .EMS arrived .transported to ED .
Review of R404's ED (Emergency Department) Provider Note dated 5/23/24, revealed, .Patient presented with unintentional medication overdose. Was given Dilaudid and Gabapentin. Was hypoxic (low level of oxygen in body tissues) and required Narcan (medication to treat narcotic overdose) in field. On arrival here, we did give him multiple doses of Narcan. Eventually started on Narcan drip. Was still sleepy. Noted to have hypercapnia (buildup of carbon dioxide in bloodstream). Did require hospitalization .Diagnosis: Acute hypercapnic respiratory failure . mistakenly given another patient's medication .At approximately 8:30 AM, he was given 4 mg of PO (by mouth) dilaudid and 800 mg Gabapentin that was intended for a different patient. Shortly thereafter he became unresponsive and desatted (blood oxygen levels dropped) to 70s Over the course of an hour (R404) became more somnolent (solemn state) and harder to arouse . gave him a total of 2 mg of Narcan .Toxicology was consulted in the emergency department. They recommended to start a Narcan drip .started the drip at 0.4 milligrams/hour, but incrementally increased the dose .ordered a VBG (venous blood gas test) which showed pH of 7.08 (7.32-7.42) pCO2 132 (38-52), bicarb 36.5 (22-32). He was started on BiPAP FiO2 40%. A second VBG approximately 40 minutes later showed minimal improvement. He was transferred to the intensive care unit for further management .Based on last blood pressure taken in the ED of (!) 191/176 .admitted to hospital for acute hypoxic respiratory failure and chest pain. Cardiology believed chest pain was likely type 2 MI (myocardial infarction (heart attack)) .05/23/24 1646 (4:46 PM) INSERT ARTERIAL LINE .CRITICAL CARE ARTERIAL BLOOD GAS - Abnormal; requiring BiPAP
-pH, Arterial 7.19 (7.35 -7.45)
-pCO2, Arterial 88.1 (35.0-45.0)
-Bicarbonate, Arterial 32.7 (20.0-28.0)
-Base Excess, 4.5 (2.0 - 2.0)
Assumed care from previous physician care at 1:00 pm .Blood gas showed he is significantly acidotic with CO2 retention .Toxicology was consulted .quickly transitioned over to BiPAP and patient was frequently stimulated to try to maintain respirations .required near constant stimulation to keep him awake however and is at high risk for intubation .admitted to the intensive care unit on Narcan drip and BiPAP with close respiratory monitoring, but remains at high risk for decompensation .Critical care time was required due to the life threatening nature of this patient's condition .Heparin gtt (IV drip) started .Lines: Art, PIV .Airways: BiPAP .SUBJECTIVE: Upon presentation to the emergency department the patient was hemodynamically stable but requiring 4 L nasal cannula to maintain appropriate saturations which eventually escalated to BiPAP. The patient received 5 doses of Narcan and subsequently placed on a Narcan drip with some improvement in his mentation. Lab work was significant for a significant respiratory acidosis. The patient was evaluated by toxicology in the emergency department and recommended supportive measures and titratable Narcan in an effort to avoid intubation .Objective .in acute distress .cardiovascular rhythm irregular .Pulmonary .Tachypnea and accessory muscle usage present .
Review of R404's Hospital Toxicology Consultation Note dated 5/23/24, revealed, Accidental narcotic ingestion .received total of 5 doses of Narcan and presently is on a Narcan drip .UA not known if the Narcan will be sufficient to return around his respiratory issues and he may require intubation. He remains poorly responsive and requires stimulation to continue participation with the BiPAP. The Narcan may be of little benefit at this point but it will not hurt the patient to increase the dose if attempting to prevent intubation. Care otherwise remains supportive symptomatic. Ingestion includes Neurontin (Gabapentin) and Dilaudid (hydromorphone) .he has severe hypercapnia with a pCO2 of 121 and pH of 7.1. He presently is on BiPAP and a Narcan drip .
On 7/11/24, NHA A was notified of the Immediate Jeopardy that began on 5/23/24 due to the facility failing to prevent a serious medication error for Resident #404 requiring hospitalization and admission to the intesive care unit.
On 7/11/24, this surveyor verified the facility completed the following to remove the Immediate Jeopardy:
1.
Newly hired nurses to only be assigned to follow facility nurses as of 05/23/2024.
2.
Medication Administration Guidelines policy was reviewed by the administrator and Director of Nursing and deemed appropriate on 05/23/2024.
3.
Medication Administration - General Guideline to be followed at each medication pass.
4.
On 5/23/24, daily schedules were reviewed by the DON and scheduler to ensure appropriate nurse orientation practice is occurring.
5.
On 5/23/24, education was completed to nurses on medication administration-general guidelines was initiated; any facility staff member and agency staff member who did not receive education by 5/23/24 will receive education prior to the start of their next shift. All facility staff and agency staff who were present at the time of the incident were immediately educated. As of 5/23/24, all facility staff and agency staff have completed the necessary required education. Education is completed for all new hires prior to their first shift.
6.
Medication administration audits began the week of 05/23/2024 and were completed weekly x 2 weeks then monthly x 2 months to ensure the Medication Administration Guidelines were being completed.
7.
Beginning on 05/23/2024, DON completed daily schedule audits when there was a nurse on orientation to ensure that they are scheduled with a facility nurse - ongoing
8.
NHA/designee began to complete resident identifiers audits starting 05/23/2024 to ensure there was a picture uploaded to PCC (electronic medical records) and room is identified with the resident name once weekly x 2 weeks then monthly x 2 months.
9.
Results of audits have been reviewed with the QAA committee on May 30th and June 20th to ensure compliance and any further recommendations.
During an observation on 7/9/24 at 7:55PM, Resident #15 was observed to have plastic cup with medications left at her bedside.
Review of the medical record revealed Resident #15 had a medication administration review on 6/22/2013 that indicated she was unsafe to self-administer medicaitons. This required additional training for nursing on the medication administration policy.
10.
Additional education provided on the Medication Administration - General Guidelines policy (2023) to 8 out of 21 licensed nurses, including licensed agency nurses on 07/12/2024. All licensed nurses including agency nurses will have education on the Medication Administration - General Guidelines policy completed prior to the beginning of their next shift.
Although the immediate jeopardy was removed on 7/12/24, the facility remained out of compliance at a scope of isolated and severity of actual harm that is not Immediate Jeopardy because education had not yet been completed and sustained compliance had not yet been verified by the State Agency.
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0658
(Tag F0658)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to MI00145186
Based on observation, interview, and record review the facility failed to follow profession...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to MI00145186
Based on observation, interview, and record review the facility failed to follow professional standards of practice for nursing for 1 of 18 residents (R404) reviewed for significant medication errors resulting in R404 receiving another resident's medications including opioids, experienced respiratory failure, and sent to the hospital for life-sustaining treatment.
Findings include:
R404
According to the Minimum Data Set (MDS), dated [DATE], R404 scored 15/15 (cognitively intact) on his BIMS (Brief Interview Mental Status).
R7
According to the Minimum Data Set (MDS), dated [DATE], R7 scored 13 /15 (cognitively intact) on his BIMS (Brief Interview Mental Status).
Review of R7's MAR/TAR dated 5/23/24 indicated at 8:00 AM, LPN WW indicated documented administration of:
-Gabapentin 400 mg 1 capsule by mouth for neuropathy
-methocarbamol 500 mg 2 tablets by mouth for muscle spasms/phantom pain
-aspirin 81 mg by mouth for prophylaxis (preventative)
-lotrel 5-20 mg 1 capsule by mouth for hypertension
-Miralax17 grams by mouth for constipation
-Apixaban (blood thinner) 5 mg 1 tablet by mouth for prophylaxis
-hydromorphone HCL (dilaudid) 4 mg by mouth for chronic pain
-levetiracetam 750 mg 2 tablets by mouth for seizure disorder
-lidocaine External gel 4% topically for right shoulder pain
Review of Licensed Practical Nurse (LPN) WW written statement by proxy of Nursing Home Administrator (NHA) A dated 5/23/24 at 1030 AM, indicated she had dispensed (prepped) and administered morning medications to R404 at approximately 7:30 AM. At approximately 7:45 AM LPN WW prepped R7's medications and handed the cup of medications to LPN XX and told him the room number. LPN WW stated she was unclear if she had given LPN XX the wrong room number or if he had heard her wrong but at approximately 8:35 AM R7 reported to her that he had not received his 8:00 AM medications. LPN WW informed R7 that he had received his medications, however, R7 continued to insist that he had not. LPN WW asked LPN XX if he had administered R7's to him and LPN XX stated, A bigger guy? LPN WW stated, No, that is not (R7). The medication error was reported to the former Unit Manager/Clinical Care Coordinator (UM/CCC) by both nurses, R404 had received R7's medications.
Review of LPN XX written statement by proxy of NHA A dated 5/23/24 at approximately 11:45 AM, indicated he offered to run the medications for LPN WW. When LPN WW handed him the medications for R7 she told him These are for (R7's first name which was the same first name as R404) and when he asked for a room number. LPN XX stated when he entered the stated room, he spoke to a resident and asked if he was the man with the first name he was given. The resident responded to the name. LPN XX then informed R404 that he had his medications.
During an interview on 7/11/24 at 3:35 PM, R404 stated, I was a resident at the facility in May (2024). I went to the room that was a lounge that morning, was given my medications by a lady, who said she was a nurse then I went back to my room. About 5 minutes later a man nurse came to my room and called out my first name. I said my first name. He did not ask me my last name. He said he had meds for me. I said I got my meds a short time ago by the lady nurse. He said the meds were mine. He said he had been a nurse for about 25 years and should know how to pass meds and that he knew they were my meds. He insisted he had my medications. I got tired of arguing with the nurse. He should have checked my ID. I still had the hospital bracelet on from the day before. I took the medications he insisted were mine. The next thing I knew I was in the hospital. I was told I was unresponsive.
Review of LPN WW written statement by proxy of NHA A dated 5/23/24 at 2:27 PM, gave further clarification on the incident that happened earlier in the day involving R404 and other residents. LPN WW indicated she had prepped medications for three residents (R34, R353, and R49) with LPN XX administering them. LPN WW stated LPN XX had administered medications to the remainder of the residents on the 300 Hall. LPN WW stated all residents on the 400 Hall she had prepped medications and administered with LPN XX.
During an interview on 7/10/24 at 3:38 PM, R7 stated, The facility overdosed the guy in the room across the hall from me a while back. The staff gave him my meds (medications). He was not my roommate.
During an interview on 7/11/24 at 2:10 PM, LPN WW stated, I have been a nurse since 2002. I know the rights of medication (meds) administration. On May 23 rd (2024), I was passing meds with an agency nurse (LPN XX). We were working out of the same med cart. I gave (LPN XX) medications I had pulled to give to (R7) he gave the wrong person the wrong meds. Once (R7) came to the med cart and said he did not get his morning meds. (LPN XX) told me did not give the meds to (R7). I had been pulling meds that morning and (LPN XX) was giving them. I delegated the meds to (LPN XX). I knew I did wrong by pulling the medications and having the other LPN administer them. The meds were given by (LPN XX) around 8:30 AM. (R7) came to the med cart around 8:30 AM asking for his meds. I told him he already got them, and he argued with me. (LPN XX) said he gave the meds to a bigger guy (R404) and I told him that was not (R7). I gave (R404) his meds at 7:30 AM in the Garden Room. He was drowsy and laying across a bedside table. I had a hard time waking him, he took the meds, and went back to sleep. I left him there. He must have walked back to his room where (LPN XX) found him and gave him (R7's) meds. We went immediately to (Unit Manager (UM) VV) reporting the wrong meds had been given to the wrong person. I went back to passing meds at the same med cart.
During an interview on 7/11/24 at 2:43 PM, LPN XX stated, I have been a nurse for 17 years. The first day I arrived, I was paired up (LPN WW) who was in her orientation process. We decided she would pull meds and I would pass them. (R404) was about the 4th resident we did this together. (LPN WW) would tell me the resident name and room number and I repeated it back to her and she would say yes. After the incident with (R404) we maybe did 5 more residents the same way. The Unit Manager told me to go sit with (R404) and do vital signs every 15 minutes. The second time VS were taken (R404) was slurring his speech and lethargic. The doctor came to the room, ordered Narcan, and it was administered. (R404) responded and then started to decline. A second Narcan was ordered and 911 was called. I do not know what the medications I gave him. I took the meds and went to what I thought was (R7's) room. (R404) responded when I went into the room. I did not pull the meds. I watched the MAR as (LPN WW) pulled meds and saw a first name but not a picture in the medical record. I watched the LPN pull a med out of the narcotic (controlled substance) drawer, but I did not look at what med it was or the name on the card. I do not know what meds were pulled. (R404) did not have on a wrist band, a name on the room door, or a picture in medical record. I know better than to administer medications the way I did.
Review of R404's ED (Emergency Department) Provider Note dated 5/23/24, revealed, .Patient presented with unintentional medication overdose. Was given Dilaudid and Gabapentin. Was hypoxic (low level of oxygen in body tissues) and required Narcan (medication to treat narcotic overdose) in field. On arrival here, we did give him multiple doses of Narcan. Eventually started on Narcan drip. Was still sleepy. Noted to have hypercapnia (buildup of carbon dioxide in bloodstream). Did require hospitalization .Diagnosis: Acute hypercapnic respiratory failure . mistakenly given another patient's medication .At approximately 8:30 AM, he was given 4 mg of PO (by mouth) dilaudid and 800 mg Gabapentin that was intended for a different patient. Shortly thereafter he became unresponsive and desatted (blood oxygen levels dropped) to 70s Over the course of an hour (R404) became more somnolent (solemn state) and harder to arouse . gave him a total of 2 mg of Narcan .Toxicology was consulted in the emergency department. They recommended to start a Narcan drip Lab work was significant for a significant respiratory acidosis. The patient was evaluated by toxicology in the emergency department and recommended supportive measures and titratable Narcan in an effort to avoid intubation .Objective .in acute distress .cardiovascular rhythm irregular .Pulmonary .Tachypnea and accessory muscle usage present .
Review of R404's Toxicology Consultation Note dated 5/23/24, revealed, Accidental narcotic ingestion .received total of 5 doses of Narcan and presently is on a Narcan drip .UA not known if the Narcan will be sufficient to return around his respiratory issues and he may require intubation .
Review of facility policy, Medication Administration-General Guidelines dated 2/2019, revealed, Medications are administered as prescribed in accordance with good nursing principles and practices .The Five Rights .Right Resident, Right Drug . are applied for each medication being administered. A triple check of these five Right Rights is recommended at three steps in the process of preparation of a medication for administration .B. Administration .5) The person who prepares the dose for administration is the person who administers the dose. 6) Residents are identified before medication is administered. Methods of identification include:
a. checking a photograph attached to the medical record
b. checking an identification band
c. asking the resident to verify his/her name
d. verifying resident identification with other facility personnel .
12. Medications supplied for one resident are never administered to another resident .the nurse who administers the medication records the administration on the resident's MAR immediately after the medication is given .
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
This citation pertains to intake: MI00145580
Based on record review and interview, the facility failed to ensure residents recieved care in accordance with residents needs in 2 of 18 residents (Reside...
Read full inspector narrative →
This citation pertains to intake: MI00145580
Based on record review and interview, the facility failed to ensure residents recieved care in accordance with residents needs in 2 of 18 residents (Resident #27 and Resident #406) review for quality of care, resulting in Resident #27 not receiving appropriate assessment and treatment for a injury of unknown origin, and Resident #406 not attending follow up appts with surgeon following spinal fusion surgery.
Findings include:
Resident #27:
Review of an admission Record revealed Resident #27 was a male with pertinent diagnoses which included dementia, abnormal posture (added 5/25/24), pain in right hip (added 6/25/24), pain in right knee (added 6/18/24), stroke, polyneuropathy (damage/disease affecting peripheral nerves on both sides of the body featuring weakness, numbness, and burning pain), dysphagia (damage to the brain responsible for production and comprehension of speech), dorsalgia (back pain), muscle weakness, unsteadiness on feet, lack of coordination, paralysis, cognitive communication deficit (progressive degenerative brain disorder resulting in difficulty with thinking and how someone uses language) and fracture of right hip.
Review of current Care Plan for Resident #27, revised on 3/9/23, revealed the focus, .I am at an increased risk for falls r/t (related to) orthostatic hypotension, muscle weakness, polyneuropathy, open area to left foot . with the intervention .Be sure my call light is within reach and encourage me to use it for assistance as needed. I need prompt response to all requests for assistance .Enable bar on right side of bed .Ensure that I am wearing non-skid footwear .I need a specialty wheelchair: Regr with pummel cushion and right-side lateral support, and left side arm rest to help reduce my risk for falls. A Device Assessment will be documented per policy to ensure proper use of such equipment (5/21/24) .PT/OT wheelchair /room evaluation .Reduce my risk for falling by cleaning up spills or clutter from my floor, provide glare-free lighting, accessible working call light, bed set at height deemed appropriate by PT/OT/Nurse (as applicable), my personal items within reach .Review information on past falls and attempt to determine cause of falls. Record possible root cause(s) and remove any potential causes as applicable .Staff to check and change resident and offer assistance to use toilet if awake .Fall Interventions: Offer to assist resident to get up in wheelchair for all meals. Bed against wall, enabler bar and fall mat to left side of bed (6/5/24) .
Review of Nursing Progress Note dated 5/11/2024 at 7:00 PM, revealed, .Event occurred on 05/11/2024 at 6:50 PM. Resident fell out of wheelchair trying to propel self out of room into the hallway .
Review of Nursing Progress Note dated 5/11/2024 at 11:19 PM, revealed, .Resident returned from (Local Hospital) ER department via stretcher by (Transport services). Head CT negative. Left eyebrow laceration glued together and covered with a bandaide. No new orders written, monitor laceration site for s/sx of infection .
Review of Practitioner Progress Note dated 5/14/24 at 10:29 AM, revealed, .Pt is 67 y/o male with PMH significant for dementia, hx of CVA, anxiety, depression, HTN, HLD, hx of substance abuse and hemiparesis of L side. Pt is seen today by provider to follow up post ED visit for fall over the weekend. Nursing reports that patient fell out of his wheelchair trying to propel himself down the hallway. He did end up hitting his head and was evaluated in the ED. Pt did sustain a laceration to his left eye brow without need for sutures and head CT was negative for acute changes. Pt reports that he is feeling scared after the fall. He denies any pain or injuries as a result of the fall. I fell out of my wheelchair. He denies headache, neck pain, vision changes, or pain anywhere else. He continues to express that he feels scared as a result of the fall .
Review of Nursing: Antigravity Team Note dated 5/15/2024 at 1:24 PM, revealed, .Root Cause(s) of Fall: IDT met and discussed residents most recent fall. Per resident's medical record the resident experienced a fall in the doorway of his room going into the hallway. Resident was unable to express what had happened however interview of staff notes that the resident will frequently use items in his environment to assist with propelling his w/c and it is felt that the resident had used the doorframe of his bedroom in an attempt to pull himself into the hallway ultimately pulling himself out of his w/c. Resident had on proper footwear, the call-light had not been activated due to the resident being in the doorway and the call-light being located on the bed. Assessment of the resident's w/c notes a standard w/c with a standard cushion. Review of resident's diagnoses note a diagnosis of embolic stroke with residual left sided weakness .New Interventions: - seating and positioning eval with noted addition of pummel cushion, right-side lateral support, left side arm rest .
Review of Secure Conversation dated 6/14/24, revealed, .HI (first name of NP), resident has been complaining of pain on his right leg. No swelling or injury . Response: .Okay, thank you, please utilize prn (as needed) pain medicine. This is chronic .
Review of Medication Administration Note dated 6/18/24 at 08:27 AM, .Give 2 tablets by mouth every 6 hours as needed for PRN (as needed) for pain .Resident requested for Right leg pain .
Review of Medication Administration Note dated 6/18/24 at 12:53 PM, .Give 2 tablets by mouth every 6 hours as needed for PRN (as needed) for pain .PRN Administration was Ineffective .
Review of Nursing Progress Note dated 6/18/24 at 9:10 PM, revealed, .Resident was slapping his right leg with his hand and yelling out throughout the morning. This nurse spoke with NP (nurse practitioner) in building and requested Right knee x-ray d/t (due to) resident nodding his head to feeling new and sharp pain in right thigh. X-ray resulted with -FINDINGS: Multiple views of the right knee show normal alignment without acute fractures or dislocations .Med staff notified of results and order Voltaren gel to Right knee TID (three times a day) for pain management. This nurse requested something different d/t (due to) resident rubbing leg constantly and being observed rubbing his face throughout the day. Med staff wished to continue with order. Resident declined lunch and dinner. Resident also declined any pain meds d/t him stating, they make me sleepy. This nurse spoke with med staff regarding his most recent return from hospital with no order for his Lyrica that he has been on in the past. Resident allowed this nurse to administer PRN Tylenol this morning with difficulty, with minimal effect. Resident allowed this nurse to apply Lidocaine patches to knee and thigh area of Right leg. This nurse assessed resident after dinner d/t CNA stating resident declined to eat dinner as well. Resident was observed Diaphoretic (sweating heavily), clammy, VS (vital signs) obtained with temp via forehead of 102.6, BP 161/84 P 108 O2 97% RA. Resident was able to be calmed down with reassurance by med staff. This nurse called on call med staff .spoke with her regarding the above and encouraged Voltaren gel be applied and then light weight pants so resident wouldn't touch his leg then his eye/face area. This nurse stated that resident is observed to be in pain r/t facial grimacing and moaning when med staff attempted to reposition him. Med staff ordered UA with C&S, Motrin and encourage ice packs as he allows. This nurse passed on the above to the oncoming nurse. Med staff stated, if he has any change in LOC (level of consciousness), increased pain or becomes non-verbal to call again and speak with on call .
In an interview on 07/10/24 at 11:06 AM, Registered Nurse (RN) EE reported Resident #27 had a fall with a fracture of his right hip.
Review of Incident Summary dated 6/25/24 at 5:20 PM, revealed, .NHA (Nursing Home Administrator) was notified at approximately 4:37pm that a resident has an intertrochanteric fracture (the area of the body where the hip and thigh meet) of unknown origin in his right hip. Resident was having complaints of pain, an x-ray was ordered, and a fracture was identified. Resident being sent out for further evaluation .
Review of interview conducted by facility, revealed, .Spoke to (LPN TT) on 7/1/24 at approximately 1530. Per (LPN TT) she had been working with (CNA N) CENA on Tuesday 6/18/24 and (CNA N) reported that resident (Resident #27) had begun to complain of increased pain around the Thursday/Friday timeframe the week before and that he was experiencing even more pain today (6/18/24). Per (LPN TT), (CNA N) spoke to (NP YY) NP about this resident and (NP YY) assessed and ordered a knee x-ray and other pain interventions. When (LPN TT) was asked if the resident had had any abnormal occurrences or behaviors prior to this day (LPN TT) stated that she did not recall any but she did note that he began smacking his leg more and verbally complaining of increased pain on 6/18/24 .
In an interview on 07/16/24 at 09:42 AM, Licensed Practical Nurse (LPN) TT reported Resident #27 had increased pain the last 4-5 days prior to 6/18/24, I went in there and he was hitting his leg. When she asked him about his pain, he indicated his leg hurt from his knee to his hip. LPN TT reported she reported the increase in pain to the nurse practitioner and the CNA reported to her as well. LPN TT reported she felt bad as he had a fractured hip and pain for a week and half at least and the staff were performing cares on him, turning him and attempting to get him up while he had a fractured hip. LPN TT reported he was getting aggressive with his behaviors with staff due to his increased pain.
In an interview on 07/12/24 at 10:59 AM, CNA N reported she noticed his pain was more than his normal and reported to the nurse and reported it to the nurse practitioner too that from his knee to his hip was hurting him. CNA N reported she worked with the resident frequently and was familiar with him and she reported she could tell without asking him that he had increased pain by his response to the cares. CNA N reported she wanted him to be comfortable and his pain was not under control. CNA N reported now he had scheduled pain medications and the pain seem to be under better control. CNA N reported they just started the scheduled pain medications on Wednesday (7/10/24).
Review of interview conducted by facility, revealed, .Spoke to (CNA N) on 6/28/24 at approximately 1430. Per (CNA N), (Resident #27) has a history of hitting his leg so this behavior was not abnormal for him however a couple of days before the x-ray was taken she had reported to the nurse that touching the residents leg resulted in him expressing a lot of pain. The following day (CNA N) reports that the resident continued to express the same thing however on this day the resident was insistent that he wanted to get up in his chair and they utilized the sit-to-stand to assist with the transfer and this was completed without concern. Per (CNA N), when she returned to work on Tuesday the resident was noted to be grinding his teeth and his facial expressions appeared as if the resident was experiencing increased pain. (CNA N) stated that she notified the NP, (NP YY), of her concern however the resident would not talk to her so (CNA N) asked the resident questions in the presence of (NP YY). (CNA N) asked the resident if his hip hurt and the resident nodded yes, she then asked if his knee hurt and he nodded yes and per (CNA N) she verified with (Resident #27) that he hurt from his hip to his knee and he nodded yes. Further interview of (CNA N) asking if there were any abnormal behaviors or occurrences since resident had returned from the hospital on 6/5/24 resulted in (CNA N) reporting that she had noted that the residents right foot kept dropping off the foot pedal which is new for this resident .
Review of Practitioner Progress Notes dated 6/18/24 at 12:39 PM, revealed, .Pt is seen today by provider at the request of nursing. Nursing reports acute on chronic right knee and hip pain. Nursing reports chronic pain to his right thigh with worsening over the last day or so .Upon assessment, pt states that he is having right knee pain. He describes the right knee pain as new and sharp. He reports pain with palpation and movement. He denies recent injury, fall or hearing a popping noise recently. Nursing and nursing aide denies event of injury occurring .
In an interview on 07/17/24 at 08:22 AM, Nurse Practitioner (NP) YY reported when she examined Resident #27 she did not perform palpation or assessment of the right hip area as he was seated in his broda chair. NP YY reported she had only performed range of motion on his right knee. When queried if the NP had staff lie the resident down in his bed for a more thorough examination she reported she did not have staff lie him down. NP YY reported she prescribed a lidocaine patch as well as re-prescribed Lyrica for Resident #25. Note: the medication was discontinued at the hospital and not re-prescribed when he returned from the hospital on 6/5/24.
Review of interview during investigation revealed, .Spoke to (RN EE) RN on 7/1/24 at approximately 1715 (5:15 PM) via phone .Per (RN EE) she can only recall that staff have been reporting that the resident is noting to be more resistant to turning and that he is grabbing at their arms, being belligerent and agitated when care is being provided and that this started a couple of weeks ago. Resident has been more receptive to taking his medication when (RN EE) notifies him that his pain medications are in with the other medications, and this has been a change in the residents behaviors over the last 2 weeks as well .
Review of Nursing Progress Note dated 6/23/24 at 10:15 AM, revealed, .This nurse was notified in shift-to-shift nurse report @0920 a.m. that resident's right knee is very red, warm to the touch and swollen. This writer called the on-call provider number and spoke with (Nurse Practitioner name) NP. Reviewed residents' history and recent right knee xray results as negative. New order received and noted for a uric acid level to be drawn in the a.m. tomorrow, 6/24/24, and administer prn Ibuprofen .
Review of eMar - Medication Administration Note dated 6/23/24 at 10:15 AM, revealed, .Behaviors noted r/t (related to) pain .
Review of Practitioner Progress Note dated 6/24/24 at 12:48 PM, revealed, .Chief complaint: R knee pain duration unknown .HPI: Pt says his right knee has been painful for 6 months. Worse with movement. Staff reported knee is red, warm and swollen. No fever. No hx gout. Uric acid level was drawn.Review of Systems: was not completed Poor historian .Musculoskeletal: Poor Strength, keep R knee flexed. Tender to palpation. no effusion. not red or warm. He wouldn't let me straighten the knee. no edema or calf tenderness .Diagnosis: M25. 561 - Pain in right knee: I don't see deformity or effusion. Cont. Ibuprofen and voltaren gel and observe for now. consider xray and CBC/WSR. Uric acid pending (ordered by on call provider) .
Review of Practitioner Progress Notes dated 6/25/24 at 12:04 PM, revealed, .Chief complaint: Ongoing pain .HPI: Pt is 67 y/o male with PMH significant for dementia, hx of CVA, anxiety, depression, HTN, HLD, hx of substance abuse and hemiparesis of L side. Pt is seen today by provider to f/u to right knee and right hip pain. Uric acid ordered by on call provider resulted as normal at 4. 3. Nursing states that pain continues but ibuprofen does help his pain. Time spent reviewing with IDT. Pt is awaiting sign on to hospice, family is working on ppwk for this transition of care. Right knee xray revealed mild osteo arthritis. Suspect arthritis of right hip as well .Musculoskeletal: Poor Strength, No gross deformities, pain with palpation of right hip .M25. 561 - Pain in right knee: -continue prn ibuprofen and Voltaren gel .New diagnoses: M25. 551 - Pain in right hip .Plan: -suspect osteoarthritis of R hip, obtain xray of hip to r/o fx or dislocation. Low suspicion -continue prn ibuprofen -Add voltaren gel to right hip .
Review of Nursing Progress Note dated 6/25/24 at 4:45 PM, revealed, .Resident had been experiencing pain since 6/14/24. Multiple assessments and diagnostic testing completed and 6/25/24 order for right x-ray ordered and noted to be positive .Immediate intervention implemented: Res transfer status changed to total lift, family requested to hospice .
Review of Practitioner Progress Note dated 6/26/24 at 11:49 AM, revealed, Pt is seen today by provider to f/u (follow up) to positive hips xray. Pt has been experiencing increased pain to right leg, hip xray completed on 6/25/24 resulting as positive for fx (fracture) .He does endorse pain to right hip .Procedure: Hip RT (right) 2v (views): Findings: Intertrochanteric fracture is demonstrated on the right. Some displacement is seen. No dislocation is noted .Impression: Mildly displaced intertrochanteric fracture on the right .Plan: pt not a surgical candidate, goal to optimize pain and comfort .
In an interview on 07/16/24 at 11:08 AM, CNA FFF reported she went to help another CNA with Resident #25. CNA FFF reported the other CNA informed her to be careful as he was in a lot of pain and to go easy on him when they turn him and move him. CNA FFF reported Resident #25 told CNA GGG he was still in pain, and to tell the nurse he had to go to the hospital as the pain was unbearable. CNA FFF reported she believed CNA GGG reported the pain and Resident #25's request to go the hospital but she was not sure what happened after as she was on the other hallway.
This writer attempted to contact CNA GGG but was unable to reach them.
Review of interview conducted by facility, revealed, .Per (CNA GGG) she could recall working with (CNA FFF) and providing care for (Resident #27) and he was grabbing at her arm and expressing increased pain with movement. (CNA GGG) believed that this increase in behavior and verbalization of pain had occurred around the June 20th timeframe. Per (CNA GGG) when she had asked the resident to rate his pain from 1-10 he stated it was a 20 and he was expressing that he was wanting to go to the hospital. (CNA GGG) stated that it was at this time that she noted that the residents hip was kind of swollen and she reported this to (RN AA), the nurse with the long dark hair. (CNA GGG) stated that she could recall (RN AA) stating that she was aware and working on getting an x-ray .
Review of the provided schedule for 6/20/24 revealed, CNA GGG, CNA FFF, and RN AA worked that day.
In an interview 07/17/24 at 10:14 AM, UM W reported LPN TT was walking up the hallway and she appeared upset, she was upset the provider did not want to do an xray on Resident #27's upper leg/hip as she did not feel it was clinically necessary. UM W reported she went to speak to the provider and NP YY reported to her she felt there was nothing to clinically support that she had examined him and did not see anything that would warrant further unnecessary testing. UM W reported the NP indicated him slapping his leg was not unusual for him. UM W reported when she went to examine Resident #27, who was in bed at this time, she attempted to straighten his leg a little bit and he said No and started slapping his leg. UM W reported she had maybe lifted it a couple of inches. UM W reported she did not observe the NP perform her examination on Resident #27.
In an interview on 07/17/24 at 10:20 AM, Unit Manager (UM) W reported pain assessments were completed on every shift in the medication administration record (MAR). UM W reviewed the documented pain levels in mid-June 2024 for Resident #27's and his pain levels were documented in the range of 4-5 on a scale from 0-10 with 10 being the worst. UM W reported when she went to assess Resident #27 originally, she was barely able to lift his right leg up 2 inches and Resident #25 yelled No and appeared to be in extreme pain. UM W reported with the expression of his pain she observed the documentation of a range of 4-5 appeared to not be correct unless he was not moved at all when assessed and he had had pain medication administered.
Resident #406:
Review of an admission Record revealed Resident #406 was a female with pertinent diagnoses which included spinal stenosis (space inside the bones of the spine get too small), wedge compression fracture of fifth lumbar vertebra (spinal compression fracture that occurs when the front of a vertebra collapses, but the back does not), wedge compression fracture of first lumbar vertebra, fusion of spine (surgical procedure that permanently joins two or more vertebra together so there is no movement between them), muscle weakness, difficulty in walking, unsteadiness on feet, and lack of coordination.
Review of Care Conference Summary dated 5/28/2024 at 2:59 PM, revealed, .Summary of Discussion: Initial care conference held to discuss admission, goals, and discharge planning. Resident admits into subacute rehabilitation post hospitalization at (Local Hospital) r/t spinal stenosis (L4-5) and compression fracture of L5. Resident is s/p orthopedic surgery and TOC states to follow up with OAM in 2 weeks .
In an interview on 07/17/24 at 10:00 AM, Health Information Coordinator (HIC) M reported urogynecologist indicated they do not need to see Resident #406 with no explanation to this writer. HIC M was queried whether Resident #406 was scheduled to see a gastroenterologist and HIC M reported she was unsure and she would need to take a look and reported she was not scheduled to see the gastroenterologist. When queried whether Resident #406 was scheduled to see the spinal surgeon, HIC M reported she had contacted them on Monday (July 15, 2024) and today but had not returned a phone call back to her. When queried when the resident returned from the hospital, it was reported she returned on 7/2/24 and had been back in facility for approximately 2 weeks. When queried if it was HIC Ms responsibility to follow up on scheduling appointments for residents, she stated, Sure. When queried if Resident #406 had seen the spinal surgeon since her admission, HIC M reported she would have to refer to her notes and when she looked she did not have a note in reference to the appointment. When asked if she had scheduled an appointment for Resident #406 to see the spinal surgeon on 6/8/24 per the discharge instructions from the hospital she reported she did not schedule the appointment.
In an interview on 07/17/24 at 12:01 PM, Therapy Director (TD) PP reported there was no order for changes to the spinal precautions and the staff should be following the precautions until otherwise changed by the spinal surgeon. The spinal surgeon would be the provider who would discontinue the precautions for Resident #406.
In an interview on 07/17/24 at 12:17 PM, Director of Nursing (DON) B reported the HIC M would be the staff member to follow up and initiate the scheduling of appointments with the spinal surgeon and other discharge appointments.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
This citation pertains to intake MI00143238
Based on observation, interview, and record review the facility failed to maintain resident dignity in 1 (Resident #15) of 9 residents review for dignity re...
Read full inspector narrative →
This citation pertains to intake MI00143238
Based on observation, interview, and record review the facility failed to maintain resident dignity in 1 (Resident #15) of 9 residents review for dignity resulting in feelings of frustration and anger.
Findings include:
Review of an admission Record revealed Resident #15 had pertinent diagnoses which included: muscle weakness, dependence on wheelchair, morbid (severe) obesity.
Review of a Minimum Data Set (MDS) assessment for Resident #15, with a reference date of 6/8/2024 revealed a Brief Interview for Mental Status (BIMS) score of 15/15 which indicated Resident #15 was cognitively intact.
In an interview on 7/9/24 at 7:30 PM., Certified Nurse Assistant (CNA) D CNA I and CNA O reported that typical staffing is two CNAs for the B side. CNA D reported that her normal assignment was about 14 residents for the shift and that there were maybe 27 residents on B side. CNA D reported that there was not enough staff to do what the residents need us to do for them.
In an interview on 7/10/24 at 10:45 AM., Resident #15 reported that she had sat in a wet and soiled brief on more than one occasion for one or two hours waiting for assistance for incontinent care and to have her brief changed. Resident #15 reported that she has had to wait for over an hour for her call light to be answered. Resident #15 reported that having to wait long time for her call light to be answered makes her angry. Resident #15 reported that she has taken notes on her cell phone of specific dates that she had to wait extended time for her call light to be answered. Resident #15 reported that on March 8, 2024, and April 18, 2024, she waited for 2 hours for her call light to be answered when she needed incontinent care for a bowel movement. Resident #15 reported that would be acceptable to wait 15 minutes to have incontinence care done but an hour or two was too long to wait.
In an interview on 7/11/24 at 1:44 PM., Resident #15 reported that last night during night shift she had to wait over an hour for her call light to be answered.
During an observation on 7/12/24 at 1:40 PM., Resident #15's call light was noted to be on.
In an interview on 7/12/24 at 1:50 PM., this surveyor entered Resident #15's room after knocking and with permission and Resident #15 reported that she had turned on her call light requesting assistance with incontinence care. Resident #15 reported that her call light had been on for about 10 minutes.
During an observation on 7/12/24 at 1:54 PM., Resident #15's call light was answered, and care was provide as requested by Resident #15.
Review of Kardex for Resident #15 revealed . toileting, incontinent .I prefer to wear a brief . bladder/bowel . brief use . I use bariatric disposable briefs. I will notify staff when I need to be changed . per my preference, I choose not to use a bed pan or toilet, I prefer to void and have BM (bowel movement) in my brief and call for staff assistance for changing .
Review of Care plan for Resident #15 revealed .focus . I am continent but void in my brief and will tell staff when I need to be changed .initiated 5/23/24 .goal . I will be continent during waking hours and through review date .initiated 5/25/22 .interventions .brief use I use bariatric disposable briefs. I will notify staff when I need to be changed . initiated 5/25/2022 .
In an interview on 7/16/24 at 11:22 AM., Resident #15 reported that last night she turned on her call light requesting incontinence care for a bowel movement at 12:15 AM and she waited over an hour for her call light to be answered. Resident #15 reported that the call light was answered at 1:20 AM.
In an interview on 7/16/24 at 1:30 PM., Resident #15 reported that she was angry and frustrated when she had to wait over an hour for staff to answer her call light when she needs incontinence care.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to provide an environment free from psychosocial abuse in 2 (Resident #2 and Resident #36) of 2 residents reviewed for abuse resulting in feeli...
Read full inspector narrative →
Based on interview and record review the facility failed to provide an environment free from psychosocial abuse in 2 (Resident #2 and Resident #36) of 2 residents reviewed for abuse resulting in feelings of frustration, mental anguish, and a loss of autonomy (freedom from external control or influence).
Findings include:
Resident #2
Review of an admission Record revealed Resident #2 had pertinent diagnoses which included: acquired absence of the right leg above the knee, acquired absence of the left leg above the knee, and paraplegia.
Review of a Minimum Data Set (MDS) assessment for Resident #2, with a reference date of 6/14/2024 revealed a Brief Interview for Mental Status (BIMS) score of 13/15 which indicated Resident #2 was cognitively intact.
In an interview on 7/9/24 at 7:18 PM., Resident #2 stated .I can't go out the side door or the front door and there is a tracker on my power wheelchair .I was forced to quit (smoking) because I can't leave the property .
In an interview on 7/10/24 at 9:57 AM., Resident #2 stated .I am on house arrest . when asked by this surveyor when he meant, he explained that the facility was his home, and he couldn't leave and that was what house arrest was. Resident #2 reported he was being punished and he cannot leave the facility anymore. Resident #2 reported that Nursing Home Administrator (NHA) A told him he was on house arrest until he discharged from the facility. Resident #2 reported that he could leave the facility to smoke by himself when he first got here, but now he cannot leave to smoke anymore. Resident # reported that no one has offered to go outside with him. Resident #2 reported that no one has guardianship over him.
In an interview on 7/11/24 at 10:29 AM., Social Services Advocate (SSA) C reported that Resident #2 was not happy with the facility because NHA A had to take away his ability to go outside. SSA C reported that Resident #2 used to go outside often. SSA C reported that the provider and Resident #2's family member did not want him to go outside and smoke for his safety. SSA C reported that Resident #2's ability to go outside was changed on 7/1/24.
Review of Physician Orders for Resident #2 revealed .LOA - may take therapeutic LOA ordered 6/17/24 .May smoke independently ordered 6/24/24 .Verify wander guard placement q shift, back of electric wheelchair every shift ordered 7/2/24 .Pt is not permitted to go LOA d/t (due to) substance abuse .
In an interview on 7/12/24 at 10:33 PM., Resident #2 stated I'm still mad I can't leave the building, but I don't smoke anymore so I don't need to go outside . Resident #2 reports he knows he cannot leave the building.
In an interview on 7/16/24 at 9:22 AM., Resident #2 stated I know I cannot leave the building, I don't smoke anymore, and I would leave to smoke. Resident #2 stated I got my 30-day walking papers . This surveyor asked what Resident #2 meant by 30-day walking papers and Resident #2 replied that he had 30 days to find somewhere else to live. Resident #2 reported that he quit smoking, he does get a nicotine patch, and mints to help, and he doesn't need to go outside anymore.
Review of Administrative Note for Resident #2 dated 6/28/24 10:55 AM., revealed .spoke with resident regarding concern of resident smoking cigarettes in his room .was unable to see smoke in the room .Resident stated that this was the only time .re-educated on smoke free environment .willingly handed over smoking paraphernalia .
Review of Release of Responsibility for Leave of Absence for Resident #2 revealed .6/28 12:45 . Resident #2 signed himself out of the building on LOA (leave of absence).
Review of Social Service Progress Note dated 7/1/24 at 14:22 PM., revealed .about 1.3 miles away from the facility .observe resident in his power chair, heading south in the middle of the right side of the road .asked resident to pull off the road .NHA would be walking down to get resident .he believed he was heading back to the facility .just out for a stroll .
Review of Social Service Progress Note dated 7/2/24 at 14:28 PM., revealed .spoke with residents brother .regarding recent behaviors/incidents .that the provider has put in an order that resident may not go LOA d/t exhibiting concerning behaviors and risk to his safety .shared that resident has had a substance abuse problem his entire life .as soon as resident is considered a resident of (Name Omitted) for 30 days, he (resident's brother) will be petitioning for Guardianship .
Review of Nursing Progress Note dated 7/2/24 15:19 PM., revealed .wander guard placed to back of wheelchair with resident permission .
Review of Practitioner Progress Note dated 7/3/24 11:34 AM., revealed .nursing reports concerns r/t (related to) incident .pt was observed by staff member in his PWC (power wheelchair) driving down the middle of the main road, about 1.5 miles from the facility .IDT has been in communication with pt's family who expresses concerns r/t hx (history) of drug abuse. Decision made to revoke LOA privileges d/t (due to) safety concerns and illicit drug use .pt was irritable and minimally conversive. Pt. repeated that he was on house arrest despite consistent educations. Shortly after f2f (face-to-face) visit with pt. it was reported that pt was found smoking cigarettes in his room despite continued efforts of education .pt is his own medical decision maker .
Review of IDT Review Note dated 7/3/24 at 13:22 PM., revealed .met today and reviewed resident due to his more recent behaviors .Resident currently is his own responsible party however per SSD (social services director) the resident's brother is actively pursuing a guardianship .unable to petition the court for this guardianship until the resident has resided in (Name Omitted) for 30 days .Initially upon admission resident was compliant and understating of the smoking policy however as of recent the resident has become more verbal about his dissatisfaction with the policy, per the SSD the brother has verbalized his desire is for the resident to not smoke while here at the facility due to the fact that resident would need to go off campus .but he (the brother) is understanding that he is unable to stop it at this time .concerns for resident safety an order was received that resident is unable to leave LOA without family or staff supervision .potential of him forgetting that this order was in place and the use of a wander guard to remind him could be an additional safety intervention .the resident was verbally informed that a 30 day involuntary d/c (discharge) is being pursued and if there were any places that he would like to go to please notify the administrator .
Review of Care Plan for Resident #2 revealed .focus .I have a wander guard to the back of my motorized wheelchair r/t behavioral symptoms .initiated 7/2/24 . goal .my risk for elopement will be minimized .initiated 7/2/24 .interventions .elopement risk assessment on admission, quarterly, and PRN (as needed) .I need direct supervision while outside the facility .place information in the elopement book per policy .initiated 7/2/24 .focus .I choose to quit smoking by using a nicotine patch .initiated on 7/3/24 .goal .successfully quit smoking .initiated on 7/3/24 .interventions .I may need random checks to search for smoking paraphernalia .initiated 7/3/24 .focus .I choose to smoke independently despite the education provided to me .initiated on 6/24/24 .interventions .I smoke independently .I need to properly sign in and out as I leave the facility property .
Review of Safe Smoking Assessment dated for 6/23/24 at 10:11 AM., revealed .resident may smoke independently .
There was no noted additional smoking assessment in Resident #2's record.
In an interview on 7/16/24 at 9:27 AM., SSA C reported Resident #2 can make his own decisions. SSA C reported that Resident #2 was educated that if he were to leave the building it would be considered AMA (against medical advice), and APS (adult protective services) would be called, and Resident #2 would not be allowed to return to the building. SSA C reported that the restrictions for independent LOA for Resident #2 are in place. SSA C reported that Resident #2's 30-day walking papers were not issued, he was placed on restrictions, and I talked NHA A off a ledge before he issued the involuntary discharge. SSA C reported that she was working with Resident #2's brother for a discharge to a less restrictive place, and that Resident #2 was told that his power wheelchair could be taken away.
In an interview on 7/16/24 at 9:57 AM., NHA A reported that Resident #2 was his own responsible person. NHA A reported that Resident #2's brother didn't want him outside of the building, and the provider mentioned that Resident #2 wasn't safe by himself outside of the building. NHA A reported that Resident #2 can choose to leave the building but if he does it is considered AMA. NHA A reported that SSA C started the process for guardianship for Resident #2. NHA A reported that he told Resident #2 that we were beginning the process of the eviction. NHA A reported that he never filed Resident #2's involuntary discharge paperwork.
In an interview 7/16/24 at 10:02 PM., Regional Clinical Nurse (RCN) KK stated .we are not taking his (Resident #2) choice away from him but if he chooses to leave the building it will be considered leaving AMA.
In an interview on 7/16/24 at 11:12 AM., Nurse Practitioner (NP) YY reported that she spoke with the IDT team regarding the discharge process for Resident #2, and the disenrollment process has begun. NP YY reported that Resident #2 does not have a safe place to discharge to at this time.
In an interview on 7/16/24 at 11:32 AM., Resident #2 reported that he was still under house arrest, he cannot go outside, and he was still mad about that. Resident #2 reported that when NHA A told him he would not be able to go outside he was mad, he wanted to say vulgar words, but knew if he did it would only make his punishment worse. Resident #2 stated I can't leave the building. If I leave the building, I can't come back in. I have to stay here, I have no option, and I will do it with a smile. Resident #2 stated If the facility didn't tell me I would be homeless if I left again, then I would still be going outside. I am a sun worshiper, and I would love to be able to go outside again.
Resident #36:
Review of an admission Record revealed Resident #36 was a male with pertinent diagnoses which included dementia, anxiety, muscle weakness, diabetes, and adjustment disorder with anxiety.
Review of current Care Plan for Resident #36, revealed no care plan for smoking for the resident.
Review of Safe Smoking Assessment dated 9/24/23, revealed, .Resident understand the smoking process and demonstrates the ability to follow safety precautions .Yes .Resident is able to communicate why oxygen and oxygen equipment must always be removed before going to smoking area .yes .Resident smokes safely ie. Does not allow ashes or lit material to fall on self or others while smoking, remains alert and aware while smoking, does not endanger self or others while smoking, does not burn furniture, clothing, skin, self or others while smoking .yes .Summary of Evaluation: Smoking status: May Smoke Independently .
Review of the medical record revealed no other safe smoking assessments completed for Resident #36.
In an interiew on 07/09/24 at 09:12 PM, Resident #36 reported the facility had blocked him from going outside, and now he can't go outside to smoke, unless someone is with him. Resident #36 reported he had been able to go outside and smoke for the last 18 months and now they changed the rules and were stopping him from going out. Resident #36 reported he attended therapy 3 times per week. He reported he had a prosthetic leg which he kept in therapy and works on walking with a walker there. Resident #36 reported he had no sores on his bottom as he gets up out of bed every day.
In an interview on 07/11/24 09:49 AM, Unit Manager (UM) W reported he can go out to smoke, he had a guardian who had given him permission to sign himself out to go smoke. UM W reported he was safer than some residents who were allowed to go out and smoke. UM W reported he had been provided with a 30 day notice and after that he would only be allowed to go out and smoke if he was signed out by his guardian or guardian approved person. UM W reported Resident #36 was able to manuever his wheelchair just fine but because he had a guardian he would need to have a responsible person take him even if the guardian gave persmission for him to sign himself out.
In an interview 07/17/24 at 10:14 AM, UM W reported the smoking assessment was completed quarterly and upon admission.
Review of policy, Smoke Free Environment revised on 2/24 revealed, .Residents who are able to and want to smoke may do so off premises. Assess for resident smoking safety. Residents who smoke will be further assessed, using the Resident Safe Smoking Assessment, to determine they can smoke safely. They must sign out at the clinical care station and request their smoking materials .All Smoking paraphernalia to be kept at clinical care station including but not limited to; Lighters, Cigarettes, Other paraphernalia .Clinical safe smoking assessment/evaluation will be completed at least quarterly or with significant change.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake #MI00145579.
Based on interview, and record review, the facility failed to prevent the misappr...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake #MI00145579.
Based on interview, and record review, the facility failed to prevent the misappropriation of resident medications in 1 of 3 residents (Resident #36) reviewed for abuse, resulting in loss of resident's diabetes medication, a delay in treatment of diabetes, and the potential for the resident to not reach their highest practical well-being.
Findings include:
Resident #36
Review of an admission Record revealed Resident #36 was originally admitted to the facility on [DATE], with pertinent diagnoses which included: type 2 diabetes (problem in the way the body regulates and uses sugar).
Review of a Minimum Data Set (MDS) assessment for Resident #36, with a reference date of 3/14/24 revealed a Brief Interview for Mental Status (BIMS) score of 15, out of a total possible score of 15, which indicated Resident #15 was cognitively intact.
Review of a Facility Reported Incident dated 5/9/24 at 5:53 PM revealed, .potential missing medication, Ozempic (improves blood sugar) .(Director of Nursing (DON) B) sent (Unit Manager (UM) W an email on 5/8/24 stating that (Resident #36) had not received his Ozempic and to look into this .the unit manager verified that the resident had not received the medication. The pharmacy was contacted, and the pharmacy stated that the medication was delivered on 05/01/2024, however we were unable to locate the medication. Immediately following being unable to find the medication, the unit manager reported to Nursing Home Administrator (NHA) and Medical Director that they are potentially missing a medication .
Review of Resident #36's Medication Administration Record for April 2024 revealed, Ozempic (2mg/dose) subcutaneous solution pen-injector 8 mg/ml inject 2 mg subcutaneously (injection) one time a day every Tuesday for Type 2 Diabetes. Start Date 4/23/24, D/C (discontinue) date 4/30/24 . The record indicated that Resident #36 missed a dose on 4/23/24 and on 4/30/24.
Review of Resident #36's Medication Administration Record for May 2024 revealed, Ozempic (2mg/dose) subcutaneous solution pen-injector 8 mg/ml inject 2 mg subcutaneously one time a day every Thursday for Type 2 Diabetes. Start Date 5/2/24, D/C (discontinue) date 5/13/24 . The record indicated that Resident #36 missed a dose on 5/2/24 and on 5/9/24.
In an interview on 07/12/24 at 03:01 PM, Licensed Practical Nurse (LPN) R reported that on 5/1/24 at approximately 7:20 AM the pharmacy delivered a tote of medications to A hall. LPN R reported that she verified that all medications were received, prior to the pharmacy staff leaving. LPN R reported that she then removed the medications for A hall, and delivered the rest of the medications to B hall. LPN R reported that Resident #36's Ozempic was in the tote, but that she had forgotten to remove it with the rest of the A hall medications, prior to delivering it to B hall. LPN R reported that she left the tote in the B hall medication room and notified (third shift nurse) Registered Nurse (RN) MM that the pharmacy delivery had arrived.
In an interview on 07/16/24 at 11:20 AM, RN MM reported that on 5/1/24 at 7:20 AM she was packed up and getting ready to leave for the day when LPN R brought over a tote from the pharmacy, and sat it on the desk. RN MM reported that she did not have time to put it all away, but that she quickly put the stat safe (back up) medications and the narcotic medications away before she left for the day. RN MM reported that she did not see Resident #36's Ozempic in the tote.
In an interview on 07/12/24 at 12:41 PM, UM W reported that she had received an email from DON B requesting that she investigate why Resident #36 had not been receiving his Ozempic. UM W reported that the original prescription was written on 4/19/23, but the medication was not delivered until 5/1/24. UM W reported that during her investigation on 5/9/24, she had found a pharmacy tote in the B hall medication room, and Resident #36's box of Ozempic was in the tote, but the syringes containing the medication were gone. UM W reported that the empty box was labeled and dated, and matched the medication that was listed on the pharmacy delivery sheet. UM W reported that when nursing staff received a delivery from the pharmacy, they were supposed to verify with the delivery sheet and the pharmacy staff that each individual medication was received, before signing the delivery sheet. UM W reported that the delivery sheet from 5/1/24 was signed by LPN R. UM W reported that at first RN MM denied putting away the medications for B hall. UM W reported that she could see on the computer that RN MM had opened the stat safe medication cart on 5/1/24, and then when re-interviewed, RN MM admitted that she did put away the medications, but did not see Resident #36's Ozempic. During the interview with UM W a phone call was placed to the pharmacy, to verify that Resident #36's Ozempic was included in the shipment that the facility had received on 5/1/24.
In an interview on 07/16/24 at 10:32 AM, LPN CCC reported that when she arrived for her shift on 5/1/24 around 7:00 AM, the door for the B hall medication room was propped open and remained propped open with a trash can until approximately noon that day, when maintenance staff brought a new key. LPN CCC reported that on 5/1/24 at approximately 7:30 AM, LPN R brought a pharmacy tote to B hall and sat it on the desk, and that RN MM put the medications away.
In an interview on 07/16/24 at 10:51 AM, LPN G reported that in the late evening hours on 5/1/24 she was cleaning in the B hall medication room, and she found an empty box of Ozempic in the fridge. LPN G reported that when she determined that there were no syringes in the box, she tossed it into the pharmacy tote on the floor. LPN G reported that she did not know that it was Resident #36's, until later that week when UM W asked about the empty box of Ozempic that was found in the pharmacy tote.
In an interview on 07/16/24 at 11:03 AM, DON B reported that she was in the facility on 5/1/24 and was not made aware of any concerns with the B hall medication room being propped open, and/or a missing key. DON B reported that when she was auditing medication administration records, she identified that Resident #36 had not been receiving his Ozempic. DON B reported that she was leaving for vacation and delegated UM W to investigate why the resident had missed multiple doses of the medication.
In an interview on 07/16/24 at 01:03 PM, Environmental Service Manager (ESM) L reported that a couple of months ago he had to get extra keys made for the B hall medication room, because the previous unit manager had not turned her keys in.
Review of a facility receipt dated 5/1/24 at 10:33 AM, indicated Keys for Nursing.
In an interview on 07/17/24 at 10:00 AM, Resident #36 reported that he had missed several dose of his Ozempic shot, but that he had never authorized anyone else to use it.
Review of the pharmacy's Consolidated Delivery Sheet dated 4/30/24, indicated that Resident #36's Ozempic was included in the delivery, and the medication was received by LPN R on 5/1/24.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to revise person centered care plans in 1 (Resident #2) of 18 reviewed for care plan revision resulting in the potential for implementation of ...
Read full inspector narrative →
Based on interview and record review the facility failed to revise person centered care plans in 1 (Resident #2) of 18 reviewed for care plan revision resulting in the potential for implementation of inaccurate care interventions.
Findings include:
Resident #2
Review of an admission Record revealed Resident #2 had pertinent diagnoses which included: acquired absence of the right leg above the knee, acquired absence of the left leg above the knee, and paraplegia.
Review of a Minimum Data Set (MDS) assessment for Resident #2, with a reference date of 6/14/2024 revealed a Brief Interview for Mental Status (BIMS) score of 13/15 which indicated Resident #2 was cognitively intact.
In an interview on 7/9/24 at 7:18 PM., Resident #2 stated .I can't go out the side door or the front door and there is a tracker on my power wheelchair .I was forced to quit (smoking) because I can't leave the property .
In an interview on 7/11/24 at 10:29 AM., Social Services Advocate (SSA) C reported that NHA A had to take away Resident #2's ability to go outside. SSA C reported that Resident #2 used to go outside often.
Review of Physician Orders for Resident #2 revealed .LOA - may take therapeutic LOA ordered 6/17/24 .May smoke independently ordered 6/24/24 .Nicotine Transdermal patch 24 hour 14mg/24 hour .apply 1 patch transdermally (on skin) one time a day for smoking cessation and remove per schedule ordered 7/2/24 .Verify wander guard placement q shift, back of electric wheelchair every shift ordered 7/2/24 .Pt is not permitted to go LOA d/t (due to) substance abuse .
Review of Care Plan for Resident #2 revealed focus .I choose to smoke independently despite the education provided to me .initiated on 6/24/24 .interventions .I smoke independently .I need to properly sign in and out as I leave the facility property .focus .I choose to quit smoking by using a nicotine patch .initiated on 7/3/24 .goal .successfully quit smoking .initiated on 7/3/24 .interventions .I may need random checks to search for smoking paraphernalia .initiated 7/3/24 .focus .I have a wander guard to the back of my motorized wheelchair r/t (related to) behavioral symptoms: short attention spans, excessive and impulsive motor activity, and TBI (traumatic brain injury) .initiated 7/2/24 . goal .my risk for elopement will be minimized .initiated 7/2/24 .interventions .elopement risk assessment on admission, quarterly, and PRN (as needed) .I need direct supervision while outside the facility .place information in the elopement book per policy .initiated 7/2/24.
Review of Safe Smoking Assessment dated for 6/23/24 at 10:11 AM., revealed .resident may smoke independently .smoking cessation material declined .
No other safe smoking assessment for Resident #2 was noted in his record.
Review of Elopement Risk for Resident #2 dated 6/15/24 revealed .is the resident at risk for elopement? 2. No .
No other elopement risk assessment for Resident #2 was noted in his record.
Review of Elopement book on 7/16/24 at 2:23 PM., revealed that Resident #2 was not included in the elopement book at the front main entrance to the facility.
Review of Elopement book on 7/16/24 at 2:25 PM., revealed that Resident #2 was not included in the elopement book at the employee entrance/A side nursing station.
Review of Elopement book on 7/16/24 at 2:30 PM., revealed that Resident #2 was not included in the elopement book at the B Side nursing station.
In an interview on 7/16/24 at 2:34 PM., Licensed Practical Nurse/Agency LPN/A LL reported that Resident #2 should be in the elopement book. LPN/A LL reported that Resident #2 no longer had privileges to go outside.
In an interview on 7/16/24 at 2:39 PM., Unit Manager (UM) G reported that Resident #2 was not an elopement risk and did not need to be in the elopement books. UM G reported that Resident #2's care plan revealed that he had a wander guard. UM G reported that if a resident has a wander guard, they were an elopement risk. UM G reported that Resident #2 could not go outside independently. UM G reported that Resident #2 no longer smoked. UM G reported that Resident #2's care plan needed to be updated as it contained conflicting information.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident was consistently provided with showers/bathing fo...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident was consistently provided with showers/bathing for 2 of 7 residents (Resident #27 and Resident #406) reviewed for activities of daily living, resulting in unmet personal hygiene needs with the potential for isolation, psychosocial harm, skin breakdown, harboring infection, and decreased self-esteem.
Findings include:
According to [NAME], [NAME] A.; [NAME], [NAME] Griffin; Stockert, [NAME]; Hall, [NAME]. Fundamentals of Nursing - E-Book (Kindle Locations 50742-50744). Elsevier Health Sciences. Kindle Edition.Personal hygiene affects patient's comfort, safety, and well-being. Hygiene care included cleaning and grooming activities that maintain personal body cleanliness and appearance. Personal hygiene activities which as taking a bath or shower and brushing and flossing the teeth also promote comfort and relaxation foster a positive self-image, promote healthy skin, and help prevent infection and disease .
Resident #27:
Review of an admission Record revealed Resident #27 was a male with pertinent diagnoses which included dementia, abnormal posture, pain in right hip, pain in right hip, stroke, polyneuropathy (damage/disease affecting peripheral nerves on both sides of the body featuring weakness, numbness, and burning pain), dysphagia (damage to the brain responsible for production and comprehension of speech), dorsalgia (back pain), muscle weakness, unsteadiness on feet, lack of coordination, paralysis, cognitive communication deficit (progressive degenerative brain disorder resulting in difficulty with thinking and how someone uses language) and fracture of right hip.
Review of current Care Plan for Resident #27, revised on 6/9/23, revealed the focus, .I have an ADL self care performance deficit r/t (related to) chronic pain, weakness, neuropathy, CVA (stroke), osteoarthritis (flexible tissue at the ends (cartilage) of bones wears down) . with the intervention .Bathing preference: shower in the morning .Shower-Wednesday and Saturday 1st shift .
During an observation on 07/10/24 at 10:58 AM, Resident #27 appeared disheveled with his hair uncombed and mustache/beard needed trimmed and combed. He needed to be shaved on the side of his face and neck area. Resident #27's face appeared very greasy looking and when asked if anyone had washed his face, he was able to shake his head, No.
During an observation on 07/16/24 at 09:34 AM, Resident #27 was observed lying in his bed with food on his face in his mustache and his beard all around his mouth area. His facial hair was not groomed and over grown. He did not have his neck shaved nor the side of his face.
Resident #406:
Review of an admission Record revealed Resident #406 was a female with pertinent diagnoses which included spinal stenosis (space inside the bones of the spine get too small), wedge compression fracture of fifth lumbar vertebra (spinal compression fracture that occurs when the front of a vertebra collapses, but the back does not), wedge compression fracture of first lumbar vertebra, fusion of spine (surgical procedure that permanently joins two or more vertebra together so there is no movement between them), muscle weakness, difficulty in walking, unsteadiness on feet, and lack of coordination.
Review of current Care Plan for Resident #406, revised on 7/10/2018, revealed the focus, .I have an ADL self care performance deficit r/t lumbar surgery and fusion, fatigue, limited mobility, limited rom (range of motion), musculoskeletal impairment recent fall and history of falls, BLE (bilateral lower extremity) weakness, pain . with the intervention .Praise all efforts for self care .Shower 2 assist Wednesday and Saturday 7-3 .
Review of a Minimum Data Set (MDS) assessment for Resident #406, with a reference date of 5/31/24 revealed a Brief Interview for Mental Status (BIMS) score of 13 out of 15 which indicated Resident #406 was cognitively intact.
In an interview on 07/10/24 at 09:50 AM, Resident #406 reported she has not had a shower and not offered a shower or bed bath.
Review of Minimum Data Set (MDS dated 5/31/24, revealed, .Section F: How important is it to you to choose between a tub bath, shower, bed bath, or sponge bath? .Very important .
Review of a Minimum Data Set (MDS) assessment for Resident #406, with a reference date of 5/31/24 revealed, .Section GG: E. Shower/bathe self: The ability to bathe self, including washing, rinsing, and drying self (excludes wahing of back and hair) .2. Substantial/maximal assistance .A. roll left and right: the ability to roll from lying on back to left and right side, and return to lying on back on the bed .01. Dependent .B. Sit to lying: The ability to move from sitting on side of bed to lying flat on the bed .01. Dependent .C. Lying to sitting on side of bed: The ability to move from lying on the back to sitting on the side of the bed and with no back support .01. Dependent .
In an interview on 07/09/24 at 08:35 PM, Resident #406 reported she was unable to get up by herself and she had not been out of bed yet. Resident #406 reported she was unable to stand and had numbness in her feet. Resident #406 reported she had not received a shower, not a full bed bath since she had been at the facility. During an observation, Resident #406's hair was in an unkempt, knotted bun on the top of her head.
In an interview on 07/12/24 at 10:39 AM, Resident #406 reported it had been approximately 4-6 weeks since her hair has been washed and she had not received a bath or a shower. Resident #406 reported when she was sent to the hospital they did not wash her hair while she was there as well. Resident #406 reported the staff could have taken her to the sink to wash her hair or laid her on the shower gurney to wash her up.
In an interview on 07/12/24 at 03:15 PM, Resident #406 reported no staff had offered to provide her with a shower or bath and the most any had done was a quick wash with a wash cloth on her upper stomach area and down the tops of her arms. Resident #406 reported she had not been asked or provided a shower/bath since her initial admission a few months ago.
In an interview on 07/10/24 at 10:53 AM, Certified Nursing Assistant (CNA) N reported she had 15 residents assigned to her on hallway II. There were three persons for Hoyer transfers. CNA N reported she tried to get the showers done for the residents on the hallway, depends on the day and what was happening on the hallway. CNA N reported the showers were documented in the medical record and on a skin monitoring form. She reported she tried to get everything done for the resident and still try to get out on time. CNA N reported most days there were 3 CNAs scheduled for the building. She reported she was by herself this week on the hallway.
In an interview on 07/16/24 at 10:38 AM, Hospice Aide SS reported if the resident refused she would document in the medical record. When she completed a shower, she would inform the regular staff at the facility and the hospice RN case manager. When she does oral care, nail care she documents that in the medical record as well. She reported she also documented in the hospice system as well. If any changes to the resident, she would let the staff know and the RN case manager for hospice.
In an interview on 07/16/24 at 11:12 AM, CNA FFF reported when a resident would refuse a shower/bath we would encourage them by asking again, offer a different time, approached by a different staff member. if the resident continued to refuse, we have to let the nurse know they refused. The skin monitoring sheets were placed in the kiosk and the shower/bath or refusal was documented in the medical record.
In an interview on 07/16/24 at 11:37 AM, UM W reported the skin monitoring sheets were for her QA purpose, she reviews, makes sure the weekly skin sweep was in the medical record and then she shreds the document.
In an interview on 07/16/24 11:42 AM DON reported the skin monitoring was not their process, the shower or bath was to be documented in the task section of the electronic medical record. If a resident refused, it was documented in the medical record as well as approached by the nurse to encourage the resident.
Review of policy, Activities of Daily Living implemented 2/25/24, revealed, .Care and services will be provided for the following activities of daily living .1. Bathing, dressing, grooming, and oral care .3. A resident who is unable to carry out activities of daily living will receive the necessary services to maintain good nutrition, grooming, and personal and oral hygiene .
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake #MI00142938.
Based on observation, interview and record review, the facility failed to provide ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake #MI00142938.
Based on observation, interview and record review, the facility failed to provide care to prevent the development, consistent with professional standards of practice in 1 of 3 residents (Resident #405) reviewed for pressure injuries, resulting in the development of pressure ulcers on bilateral heels, and the potential for infection and overall deterioration in health status for all residents at risk for deterioration in skin integrity.
Findings include:
Resident #405
Review of an admission Record revealed Resident #405 was originally admitted to the facility on [DATE], with pertinent diagnoses which included: weakness, difficulty walking and prediabetes (higher than normal blood sugar levels).
Review of a Minimum Data Set (MDS) assessment for Resident #405, with a reference date of 2/8/24 revealed that the resident was at risk for pressure ulcers, and had zero unhealed ulcers.
Review of Resident #405's Hospital Records indicated that the resident had admitted on [DATE] for sepsis, and was found to have pressure wounds present both heels. Wound images reviewed revealed a large black blister covering the left heel and a smaller reddish/purple blister on the right heel.
Review of Resident #405's Practitioner Note dated 2/21/24 revealed, .seen today by provider to evaluate reported heel pain. Rehab director reported that patient has been doing well with therapy, walking, and standing up until yesterday. She complained of pain to bilateral heels that interfered with her ability to stand and take steps. Pain was reported in bilateral heels. Pain reported on 2/20/24 was supposedly 10/10 and reported pain during therapy today is 6/10. Upon assessment She reports pain to both heels and reports that nothing makes it better. She states this as increasing over the last few days. Upon examination, there is blood blister present to left heel and excessive dryness to bilateral feet. There is no evidence of pressure injury to right heel .New diagnoses: Pressure induced deep tissue damage .
Review of Resident #405's Physical Therapy Treatment Notes revealed a decline in participation related to complaints of bilateral foot pain.
In an interview on 07/17/24 at 11:17 AM, Licensed Practical Nurse (LPN) Q reported that Resident #405 did not move herself when in bed or in her chair, but that she could stand with assistance. LPN Q reported that the resident frequently complained of being wet and soiled.
In an interview on 07/17/24 at 11:55 AM, Director of Nursing (DON) B reported that Resident #405 did not have any wounds upon admission, per the skin assessment. DON B reported that a pressure wound on the left heel was first noted in the practitioners visit note on 2/21/24. DON B reported that the residents care plan included only general pressure interventions, and was not updated to reflect the resident's individual status. DON B reviewed the resident's order for unna boots (a compression dressing specifically to manage lower leg venous wounds, and not indicated for pressure wounds on the heels), and reported that it did not make sense for pressure ulcer treatment.
Review of Resident #405's admission Skin Assessment dated 2/3/24 at 4:21 AM, indicated that all skin was intact, and there were no specific body locations listed in the assessment.
Review of Resident #405's Weekly Skin Sweep dated 2/10/24 indicated no skin conditions, and intact skin.
Review of Resident #405's Weekly Skin Sweep dated 2/19/24 indicated an open stage 2 pressure ulcer on the left buttock, measuring 2.6 cm x 2.1 cm. There was no documentation related to heels.
Review of Resident #405's most recent Braden Assessment (risk level for pressure injuries) dated 2/10/24 indicated that the resident was at low risk for developing pressure injuries.
Review of Resident #405's Care Plan revealed, .at risk for impaired skin integrity .dated initiated 2/3/34, revision on 2/9/24 .Interventions: .Assist me to moisturize my skin as needed, Assist me to position body with pillows/support devices, protect bony prominences .Assist me to turn &/or reposition .Assist/encourage me to elevate my heels off the bed . There was no documentation related to the identified pressure wounds.
Review of Resident #405's Physician Orders/Treatment Administration Record revealed, Float heels off surfaces at all times every shift-Start Date 02/02/2024. There were 8 of 42 opportunities missed to document this treatment was in place.
Review of Resident #405's Physician Orders/Treatment Administration Record revealed, Sacrum (tailbone): Cleanse with NS (normal saline), skin prep (protectant) all around. Apply foam dressing. every night shift every 3 day(s) -Start Date 02/02/2024 This wound was not documented on an assessment until 2/19/24.
Review of Resident #405's Physician Orders/Treatment Administration Record revealed,skin prep to bilateral heals every day every night shift for pressure injury -Start Date 02/22/2024 .patient to where (sic) unna boots while in bed. every shift for pressure injury-Start Date 02/21/2024.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to maintain sufficient urine incontinence care in 1 resident (Resident...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to maintain sufficient urine incontinence care in 1 resident (Resident #304) of 1 resident reviewed for incontinence care resulting in the potential for skin breakdown.
Findings include:
Resident #304 (R304)
Review of the Face Sheet and Minimum Data Set (MDS) dated [DATE] revealed R304 admitted to the facility on [DATE] with diagnoses of anxiety, depression, and dementia. Brief Interview for Mental Status (BIMS) reflected a score of 14 out of 15 which indicated R304 was cognitively intact (13 to 15 cognitively intact).
During an interview on 7/09/2024 at 8:17 PM, R304 stated that she was left in urine for about an hour that day. She was teary eyed while talking about it and said it didn't make her feel good. R304 said that she asked to get up several times and it took them about an hour to get to her up. R304 stated that she knows lying in urine isn't good for her skin and she was worried about developing pressure ulcers on her bottom.
Review of the admission Assessment Section F dated 6/26/2024 revealed R304 had MASD (moisture associated skin damage) to her left and right buttocks and a red groin area upon admission.
Review of the weekly skin sweep dated 6/30/2024 revealed R304 had an open area to her right buttocks.
Review of the weekly skin sweep dated 7/5/2024 revealed R304's skin was intact.
Review of the weekly skin sweep dated 7/10/2024 revealed R304 had a rash/excoriation to her coccyx and groin area.
Review of the admission Assessment, Section K dated 6/26/2024 revealed R304 was incontinent of bladder during the day and night, once or more per shift, and toileting wasn't scheduled.
Review of the task bladder incontinence look back since admission showed R304 was incontinent of care each day and time except for 2 times.
Review of R304's MDS dated [DATE] Section H Bowel and Bladder revealed that resident wasn't on a urinary toileting program and was frequently incontinent. Section M Skin Conditions revealed Moisture Associated Skin Damage (MASD) (e.g., incontinence-associated dermatitis (IAD), perspiration, drainage).
Review of R304's care plan shows that she was at risk for impaired skin integrity due to urinary incontinence and inspect skin daily with care-report any concerns to nurse. R304's care plan didn't address what was being done for incontinence care related to a toileting program and/or bladder training to help with urinary incontinence.
During an interview on 7/10/2024 at 3:33 PM, Unit Manager (UM) G stated that R304 didn't have any skin issues when she arrived and didn't have any areas when she checked the previous week. UM G said she wasn't aware of the weekly skin sweep done on 6/30/2024 that indicated R304 had an open area.
During an interview on 7/10/2024 at 3:40 PM, Licensed Practical Nurse (LPN) LL stated that she completed the skin sweep on 6/30/2024 and that it was open that day and she thought it was a Stage II. LPN LL said that she can't remember if she put a treatment in place or if there was already a treatment in place or if she notified anyone about it.
During an interview on 7/10/2024 at 3:31 PM, Certified Nursing Assistant (CNA) I stated that she has known R304 to have a red bottom most of the time.
During an interview on 7/11/2024 at 9:29 AM, UM G stated that R304's skin was checked and she has maceration and they will be starting triad cream. Order for Triad Hydrophilic Wound Dress External Paste (Wound Dressings) Apply to Buttocks/sacrum topically every shift for Incontinence AND Apply to buttocks/sacrum topically as needed for Incontinence care was started on 7/11/2024.
Review of the nursing progress note completed by UM G dated 7/11/2024 revealed, .Observed with MASD to buttocks and sacrum. Verbal order to initiate Triad wound paste BID (twice a day) and PRN (as needed). Notified daughter of new orders and update in plan of care. Daughter agreed with interventions. Requested if resident could possibly have a urology or gynecology appointment to address the urine dribbling. Informed daughter that this writer will communicate with in-house physician. Resident also updated on new plan of care with her stating oh good.
During an interview on 7/16/2024 09:48 AM UM G stated that R304 didn't have a treatment in place due her incontinence prior to 7/11/2024 besides the standard barrier cream. UM G said R304 didn't have any areas on her bottom from the skin sweep done by her and it could have been an issue with the nurse since she didn't find anything. UM G stated that they normally put a treatment in place if a resident was admitted with MASD. UM G looked at R304's admission skin assessment and noted she was admitted with MASD and no treatment was ordered.
During an interview on 7/16/2024 at 2:38 PM, Therapy Director (TD) PP was asked if therapy assisted with R304's bladder incontinence and/or training for staff and he said that they did not.
Review of the Incontinence Policy with an Implementation Date of 12/2005 and a Review/ Revision Date of 6/2023 revealed, Based on the resident's comprehensive assessment, all residents that are incontinent will receive appropriate treatment and services.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain a BiPAP after resident use for infection control for 1 (Resident #13) of 1 resident, resulting in the potential for ...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to maintain a BiPAP after resident use for infection control for 1 (Resident #13) of 1 resident, resulting in the potential for cross-contamination of respiratory equipment, transmission of disease, and growth of infectious microorganisms.
Findings include:
Review of an admission Record revealed Resident #13 was a female with pertinent diagnoses which included heart failure, pulmonary hypertension, insomnia, obstructive sleep apnea, and asthma.
Review of current Care Plan for Resident #13 revised on 2/29/24, revealed, the focus, .I have a sleep disturbance r/t (related to) obstructive sleep apnea that requires me to use CPAP Unit. Please remind me that I am to wear this at night and during naps with the intervention .Clean CPAP equipment, tubing, filters, bags and masks per facility protocol .Clean or replace filters per Manufacture recommendations once a week .
Review of Orders dated 3/21/24, revealed, .CPAP Mask: Wash with mild soap and warm water. Rinse thoroughly and let air dry .every day shift .Do not use any products containing bleach or alcohol .
Review of Orders dated 3/20/24, revealed, .CPAP/BiPAP: Remove filter and replace for disposable filters. For non-disposable: Remove and wash with soap and water. Rinse and let dry and replace in machine. Complete Monthly .
In an interview on 07/09/24 at 09:29 PM, Resident #13 was observed in lying in her bed looking at her tablet. Resident #13 reported the staff do not clean her CPAP/BiPAP mask after removal and they had not replaced the mask. Resident #13 reported she had to ask staff to fill her tank for the distilled water.
In an interview on 07/10/24 at 12:23 PM, Resident #13 reported the staff did not clean her CPap/BiPAP mask when she got up in the morning.
During an observation on 07/11/24 at 01:09 PM, Resident #13 was observed up in her wheelchair, and her CPap/BiPAP mask was lying on the top of the night stand next to her bed, it was not on a barrier or in a bag. No plastic bag or basin was noted near the CPap/BiPAP mask and machine on her night stand.
In an interview on 07/11/24 at 01:49 PM, Resident #13 reported the nurse had not cleaned her CPap/Bipap mask this morning.
During an observation on 07/12/24 11:24 AM Resident #13 CPap/BiPap mask was observed on the night stand next to her bed, there was not barrier under it, or not placed in a bag.
During an observation on 07/12/24 at 11:24 AM, Resident #13's CPap/BiPap mask was observed on lying on the top of the night stand next to her bed, there was not barrier under it or not placed in a bag.
In an interview on 07/16/24 at 09:58 AM, Resident #13 reported the facility did not clean her CPap/Bipap mask at all this past weekend, she asked for the CNAs to add water to her machine, and she reported she changed out the CPap/BiPAP tubing not the facility, she reported he sister helped her do so.
In an interview on 07/16/24 at 01:58 PM, Unit Manager (UM) W reported the nurse was responsible rinse the CPap/BiPap mask and place it in a bag. UM W reported the mask was supposed to be cleaned at least once per day. UM W reported the CPap/Bipap tubing was supposed to be removed and cleaned on every day shift, every Tuesday. UM W reported the nurses were supposed to the the staff member who filled the resevior for her CPap/BiPap machine and the night nurse should be check it to make sure the resevior was full.
Review of policy, BiPAP-CPAP reviewed/revised on 6/23, revealed, .PROCEDURE: Licensed Nursing, respiratory therapy, or other trained personnel will; Obtain physician order .Assemble equipment .Fill humidifier to appropriate level (if using) .Oxygen flow should be set according to sleep study results or most recent settings from the referring facility .Store mask or nasal pillows in mesh bag or other approved storage container approved by the facility when not in use 5. CLEANING: Mask or nasal pillows shall be wiped with an approved disinfecting solution daily per manufacturers guidelines .Mask or nasal pillows stored in Mesh bag or other approved container per facility protocol .BIPAP/CPAP unit wiped weekly with approved anti-microbial agent per manufacturers guidelines .Humidifier reservoir emptied daily and allowed to air dry before refilling (if using) .Replace Mesh bag (or other approved storage device) monthly .Filters cleaned weekly per manufacturers recommendation .Tubing replaced every 3 months or sooner if soiled or damaged .Replace mask or nasal pillows every three months or sooner if visibly soiled or damaged .
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to identify post traumatic stress disorder (PTSD) trigger...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to identify post traumatic stress disorder (PTSD) triggers and develop individualized care plan interventions to mitigate triggers for 1 (Resident #65) of 24 residents reviewed for trauma informed care, resulting in the potential of re-traumatization due to staff not being informed and knowledgeable of the resident's past trauma.
Findings include:
Review of an admission Record revealed Resident #406 was a female with pertinent diagnoses which included spinal stenosis (space inside the bones of the spine get too small), wedge compression fracture of fifth lumbar vertebra (spinal compression fracture that occurs when the front of a vertebra collpases, but the back does not), wedge compression fracture of first lumbar vertebra, fusion of spine (surgical procedure that permanently joins two or more vertebra together so there is no movement between them), muscle weakness, difficulty in walking, unsteadiness on feet, and lack of coordination.
In an interview on 07/09/24 at 08:35 PM, Resident #406 reported she was sent to a hospital in another state. Resident #406 reported she was very fearful while staying there as the male resident in the next room was trying to climb out the window and staff were always coming to intervene with him and his behaviors. She reported she could hear all kinds of commotion happening next door and she was very afraid he was having a psychotic episode and would come over and hurt her. She reported she asked the staff to close her door all the way, but they always left it open some and she didn't sleep well because she was so worried he was going to come into her room and harm her or kill her.
This emotional distress had the potential to continue well past the unwarranted psychiatric hospitalization based any reasonable person would have endured psychosocial harm from being sent to another state for psychiatric hospitalization when they were cognitively intact with a BIMS (Brief Interview for Mental Status) of 13, dated 5/31/24.
Review of (Local Hospital) History & Physical dated 5/16/24, revealed, .HISTORY OF PRESENT ILLNESS: She states for the last 6 months she has ongoing lower back pain. She states that it has gotten progressively worse over the last 3 weeks since she has been off work. She believes this is because she has no longer on her feet walking around all day, but has been in bed more. Over the last 3 weeks she has also had some bilateral leg weakness. About 3 days ago her legs gave out from underneath her and she did fall, she was unable to get off the ground by herself and did need assistance from her landlord. Since then she is basically remained in bed the entire time, stating if she fell she did not know how she would get back up and felt so weak that she was sure she would fall. Psychiatric: Mood and Affect: Mood normal .Behavior: Behavior normal .Subjective: States she has intermittent paraesthesias to her fingers and toes, but states that this started around the time she began Keflex last week for a urinary tract infection; no frank numbness. Reports gait instability secondary to RLE (right lower extremity) perceived weakness, and pain. Pain is made worse with strenuous movement and is improved with lying still. Pt states she has experienced reduced daily function secondary to pain. Patient has attempted ibuprofen to help with back pain .ASSESSMENT AND PLAN: Spinal stenosis at L4-L5 level .Patient has had back pain off and on for the last 6 months. States especially worsening over the last 3 weeks as she has been off work. Over the last 3 weeks has progressive leg weakness bilaterally. She was walking to the bathroom [ROOM NUMBER] days ago and her legs gave out, since then she has not been able to leave her bed .Also endorses some numbness and tingling in her hands and feet bilaterally .
In an interview on 07/12/24 at 09:27 AM, Social Service Director (SSD) C reported she did not complete a trauma assessment for Resident #406 prior to her psychiatric hospitalization or when she was re-admitted to the facility. SSD C reported a referral to (mental health services provider) for the long term care residents that have any psychiatric diagnosis or medications, she reported she would meet with them and discuss mental health services and referral to the contracted (mental health services provider). If the resident was here for subacute rehab and the time does not fall in line to when the provider will be here, she reported she would provide supportive visits, get the activities department involved, and our physician. If there were acute concerns and (mental health services provider) was not coming, the resident would get sent out. SSD C reported before the resident was sent out to the emergency room, she would go and meet with the resident, gather information, do a risk assessment to determine the risk of self harm and then petitioning depends on the situation like if the resident was actively suicidal and had a plan, self-neglect which is considered self-harm, would petition the resident as sending them to the ER they would be sent right back. SSD C reported the ex-husband reported she had a history of trauma as he father had abruptly passed away and this sent the resident into a mental breakdown.
In an interview on 07/11/24 at 09:38 AM, Unit Manager (UM) W reported she had lumbar surgery and she was refusing cares. She doesn't like to offload pressure, or to turn, she liked to be on her back. UM W reported her back hurt, the back brace hurts her and that was why she was not up in her chair. UM W reported a lot of what was happening was due to fear, she reported she can't feel her feet, and she was fearful of falling. UM W reported Resident #406 was very smart, answered questions appropriately. UM W reported told Resident #406 she was so sorry, whatever happened over there was over there, she was on a new unit, new room and felt like she was willing to work with me. She had been putting on her light, allowed staff to provide cares and now I feel she has a lot less fear than before, before her back really hurt her.
In an interview on 07/11/24 at 02:18 PM, Therapy Director (TD) PP reported Resident #406 was very resistive, she was not trying to get up, roll side and side, she was very scared and smacked at us, not to hurt us but like she was terrified. We tried a few times to get her up into her wheelchair, and it took 3 people to do it, she was resistant due to the numbness in her hands and feet. TD PP reported he discussed with her the need to work the upper body otherwise she would lose her abilities and not be able to get out of bed.
In an interview on 07/12/24 at 09:48 AM, Director of Nursing (DON) B reported during Resident #406's time with us, she was declining cares and was unmotivated when working with therapy. Resident #406 was choosing not to allow the staff to complete incontinence care and just basic hygiene care as a result her surgical wound began to open, and she had developed an open area on her bottom. Her roommate reported she was the same at home by declining to perform self-hygiene and had incontinent episodes in her bed. Her ex-husband had shared she had a history of tragedy in her life which was not dealt with and her behaviors he believed to be underlying causes to those behaviors. DON B reported the resident's actions were not matching her words as she had indicated she wanted to discharge. When queried whether the resident was septic or on an IV antibiotic, DON B reported she was not. DON B reported the intention was to help the resident, but the facility did not work to provide alternative lesser restrictive services prior to petitioning her and sending her to a psychiatric hospital for declining cares. When asked if other residents in the facility declined care, the DON reported there were. DON B reported she had worked at other facilities and those social workers provided push back and advocated for their residents. DON B reported she depended on her staff to provide her with a different perspective and to complete the necessary steps to move to that point for what was best for the resident.
According to, National Alliance on Mental Illness (NAMI) Post-traumatic stress disorder (PTSD) is an anxiety disorder that can occur after someone experiences a traumatic event that caused intense fear, helplessness, or horror. PTSD can result from personally experienced traumas (e.g., rape, war, natural disasters, abuse, serious accidents, and captivity) or from the witnessing or learning of a violent or tragic event .While it is common to experience a brief state of anxiety or depression after such occurrences, people with PTSD continually re-experience the traumatic event; avoid individuals, thoughts, or situations associated with the event; and have symptoms of excessive emotions. People with this disorder have these symptoms for longer than one month and cannot function as well as they did before the traumatic event. PTSD symptoms usually appear within three months of the traumatic experience; however, they sometimes occur months or even years later . https://namimi.org/mental-illness/ptsd
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure the nursing staff was evaluated for appropriate competencies and skill sets resulting in the potential for residents of the facility ...
Read full inspector narrative →
Based on interview and record review the facility failed to ensure the nursing staff was evaluated for appropriate competencies and skill sets resulting in the potential for residents of the facility to be unable to maintain the highest practicable physical, mental, and psychosocial well-being and the potential for decreased resident safety for all residents who resided in the facility.
Findings include:
In an interview on 7/12/24 at 10:41 AM., Director of Nursing (DON) B reported that she had provided a competency fair for nursing employees last month and that it was poorly attended. DON B reported that she did not make the competency fair attendance mandatory. DON B reported that a staff development role did not exist, and the responsibilities of that role fell to the director of nursing.
Review of untitled spreadsheet document on 7/17/24 provided by DON B revealed columns that included employee names, position, department date, hire date, initial competency, annual competency 2023 and annual competency 2024. The untiled document included a total of 50 employee names, all from the nursing department. The final column that was titled annual competency 2024 had recorded 12 of 50 competencies completed on 6/5/2024. The final column that was titled annual competency 2024 had recorded overdue, due on a date prior to review date, or was blank for 38 of 50 employees.
In an interview on 7/16/24 at 1:57 PM., this surveyor asked DON B if the untitled spreadsheet she provide for staff competencies was interpreted that the blank boxes in the annual competency 2024 column indicated that the competency evaluations were incomplete and DON B reported that the interpretation of the blank boxes in the annual competency 2024 column did indicate that the competencies were not complete.
In an interview on 7/17/24 at 9:26 AM., Nursing Home Administrator (NHA) A reported that competencies and performance reviews were to be completed annually. NHA A reported that human resources individual provided a list to department head via email with expected completion dates and the expectation was that department heads completed the performance evaluations and annual competency reviews. NHA A reported that nursing staff competency evaluations were noted to be overdue, missing, and incomplete.
In an interview on 7/17/24 at 9:23 AM., NHA A reported that the new hire competency evaluations were to be completed on day 2 of new hire orientation. NHA A reported that new hire orientation day 2 was to be done in person at the facility. NHA A reported that day 2 orientation was not being completed as expected by the facility staff and new hire competency evaluations were not being completed.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0742
(Tag F0742)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to facilitate appropriate mental health treatment and services for 1 (...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to facilitate appropriate mental health treatment and services for 1 (Resident #406) of 1 resident reviewed for mental health services, resulting Resident #406 being sent to a psychiatric hospital for hospitalization causing psychosocial distress and fear.
Findings include:
According to, National Alliance on Mental Illness (NAMI) Post-traumatic stress disorder (PTSD) is an anxiety disorder that can occur after someone experiences a traumatic event that caused intense fear, helplessness, or horror. PTSD can result from personally experienced traumas (e.g., rape, war, natural disasters, abuse, serious accidents, and captivity) or from the witnessing or learning of a violent or tragic event .While it is common to experience a brief state of anxiety or depression after such occurrences, people with PTSD continually re-experience the traumatic event; avoid individuals, thoughts, or situations associated with the event; and have symptoms of excessive emotions. People with this disorder have these symptoms for longer than one month and cannot function as well as they did before the traumatic event. PTSD symptoms usually appear within three months of the traumatic experience; however, they sometimes occur months or even years later . https://namimi.org/mental-illness/ptsd
Resident #406:
Review of an admission Record revealed Resident #406 was a female with pertinent diagnoses which included spinal stenosis (space inside the bones of the spine get too small), wedge compression fracture of fifth lumbar vertebra (spinal compression fracture that occurs when the front of a vertebra collapses, but the back does not), wedge compression fracture of first lumbar vertebra, fusion of spine (surgical procedure that permanently joins two or more vertebra together so there is no movement between them), muscle weakness, difficulty in walking, unsteadiness on feet, and lack of coordination. Note: No mental health diagnoses currently in the electronic medical record.
Review of (Local Hospital) History & Physical dated 5/16/24, revealed, .HISTORY OF PRESENT ILLNESS: She states for the last 6 months she has ongoing lower back pain. She states that it has gotten progressively worse over the last 3 weeks since she has been off work. She believes this is because she has no longer on her feet walking around all day, but has been in bed more. Over the last 3 weeks she has also had some bilateral leg weakness. About 3 days ago her legs gave out from underneath her and she did fall, she was unable to get off the ground by herself and did need assistance from her landlord. Since then she is basically remained in bed the entire time, stating if she fell she did not know how she would get back up and felt so weak that she was sure she would fall. Psychiatric: Mood and Affect: Mood normal .Behavior: Behavior normal .Subjective: States she has intermittent paraesthesias to her fingers and toes, but states that this started around the time she began Keflex last week for a urinary tract infection; no frank numbness. Reports gait instability secondary to RLE (right lower extremity) perceived weakness, and pain. Pain is made worse with strenuous movement and is improved with lying still. Pt states she has experienced reduced daily function secondary to pain. Patient has attempted ibuprofen to help with back pain .ASSESSMENT AND PLAN: Spinal stenosis at L4-L5 level .Patient has had back pain off and on for the last 6 months. States especially worsening over the last 3 weeks as she has been off work. Over the last 3 weeks has progressive leg weakness bilaterally. She was walking to the bathroom [ROOM NUMBER] days ago and her legs gave out, since then she has not been able to leave her bed .Also endorses some numbness and tingling in her hands and feet bilaterally .
Review of current Care Plan revised on 6/7/24 revealed the focus, .I have acute pain r/t (related to) Lumbar surgery, recent small bowel obstruction, and a colvaginal fistula. I do not like to turn as I am fearful of falling. I reported to the SNF CENA that I fell at the hospital. I will not turn or reposition although I report that I am doing it. I continually ask for an increase in pain medications . with the intervention .My pain is aggravated by: movement and repositioning .Revision on: 05/28/2024.
Review of Kardex dated 7/10/24, revealed, .Resident Care: I have spinal precautions: No bending or twisting at the waist, no lifting greater than 10 pounds, up in chair as tolerated with my lumbosacral orthotic on .
Review of Preadmission Screening (PAS)/Annual Resident Review (ARR) (PASARR) Level I Screening dated 5/21/24 revealed, no mental illness or dementia diagnosis.
Review of Minimum Data Set (MDS) dated [DATE] revealed, .Section D: Mood revealed, .Resident Mood Interview: PHQ-2-9 revealed, .A. Little interest or pleasure in doing things .1. Symptom presence: 0. No .B. Feeling down, depressed, or hopeless .1. Symptom Presence: 0. No . The remainder of the assessment was disabled due to no concerns with resident mood.
Review of Minimum Data Set (MDS) dated [DATE] revealed, .Section E: Rejection of Care- Presence & Frequency: 0. Behavior not exhibited .
Review of Task: Behaviors for the previous 30 days, revealed no entries for any behaviors.
Review of Care Conference Summary dated 5/28/2024 at 2:59 PM, revealed, .Summary of Discussion: Initial care conference held to discuss admission, goals, and discharge planning. Resident admits into subacute rehabilitation post hospitalization at (Local Hospital) r/t spinal stenosis (L4-5) and compression fracture of L5. Resident is s/p orthopedic surgery and TOC states to follow up with OAM in 2 weeks. Resident reports she is still in a lot of pain, but the pain medications make it tolerable. Resident resides in a home in the community with a friend, where she reports, she is planning to discharge back to post SAR (subacute rehab). Resident reports she was hoping to be home by now and did not expect her healing to take this long. Resident reports she has never had HHC (home health care) before and does not have a preference on an agency. Does not currently have any DME (durable medical equipment). Resident has several stairs to enter her home, which is a barrier to discharge. Resident admits with PRN hydroxyzine for anxiety, however no dx of anxiety listed on TOC. Per resident she had some situation anxiousness during the hospital and did not know they sent her with the medication. She denies a hx of anxiety
In an interview on 07/09/24 at 08:35 PM, Resident #406 reported she was sent to a psychiatric hospital in another state by the facility. Resident #406 reported she was very fearful while staying there as the male resident in the next room was trying to climb out the window and staff were always coming to intervene with him and his behaviors. She reported she could hear all kinds of commotion happening next door and she was very afraid he was having a psychotic episode and would come over and hurt her or even kill her. She reported she asked the staff to close her door all the way, but they always left it open some and she didn't sleep well because she was so worried he was going to come into her room and harm her or kill her.
Review of Social Service Progress Note dated 6/10/2024 at 12:21 PM, revealed, .Resident discussed this morning with IDT. Continues to defy facility policy of no smoking on the grounds. Resident has smoked a vape pen and cigarettes in her room several times now, despite paraphernalia being removed and education. This is a risk to herself, other residents, and staff as oxygen is being used throughout the facility. Resident continues to neglect her basic needs, soiling herself and then declining to be changed. This has caused an infection to her surgical wound. At this time, IDT is in agreement that resident is a risk to herself and others. Inpatient psychiatric treatment has been agreed as the most appropriate treatment plan to prevent further harm to herself . Note: Other than the discharge planning meeting note for Resident #406 completed by SW Intern DDD on 5/28/24, this was the first note entered in the medical record by the Social Services Director (SSD) C .
Review of Social Service Progress Note dated 6/10/2024 at 2:45PM, revealed, .Call received from (Admissions staff at Psychiatric Hospital) .Transportation is arranged via ambulance for 10:30pm pick up. IDT notified .
Review of petition for hospitalization dated 6/10/24, revealed, .3. I believe the individual has mental illness and a. as a result of that mental illness, the individual can reasonably be expected within the near future to intentionally or unintentionally seriously physically injure self of other, and has engaged in an act or act or made significant threats that are substantially supportive of this expectation .c. the individual's judgment is so impaired that mental illness, and who lack of understanding of the need for treatment has caused him or her to demonstrate an unwillingness to voluntarily participate in or adhere to treatment that is necessary, on the basis of competent clinical opinion, to prevent a relapse or harmful deterioration of his or her condition, and presents a substantial risk of significant physical or mental harm to the individual or others .
Review of Complete Evaluation/Initial Psychological evaluation Psychology dated 6/15/24, revealed.HISTORY: (Resident #406) is a [AGE] year-old woman. Her chief complaint is, I honestly don't know why I am here. Patient spoke of false accusations. From anger nurses at a sub-acute rehab facility about her refusing treatment and ADLs. She says these things were false. She was there for rehab for her back injury .She was sent here due to concerns about her safety .EXAM: Examination of Ms. [NAME] reveals her to have no apparent serious mental status abnormalities. She is normal in appearance with age appropriate dress and grooming and she appears to be her stated age. Neither depression nor mood elevation Is evident. Her speech is normal in rate, volume, and articulation and her language skills are intact. She convincingly denies suicidal and self-injurious ideas or intentions. Homicidal or assaultive ideas or intentions are also denied. Hallucinations and delusions are denied, and her behavior is generally appropriate. Associations are intact, thinking is basically logical and thought content Is appropriate. There are no signs of cognitive difficulty, based on vocabulary and fund of knowledge. Memory is intact for recent and remote events and the patient is oriented to time, place, and person. There are no apparent signs of anxiety. A normal attention span is in evidence, and she exhibits no signs of hyperactivity. Insight and judgment appear intact .
Review of psychiatric hospital records had her diagnosed as having Chronic pain syndrome, status post back surgery with history of wedge compression fracture of the first lumbar vertebra. The patient is on gabapentin, acetaminophen, and oxycodone .6/15 we will add Motrin 800 mg TID PRN for pain .
In an interview on 07/11/24 at 02:18 PM, Therapy Director (TD) PP reported Resident #406 was very resistive, she was not trying to get up, roll side and side, she was very scared and smacked at us, not to hurt us but like she was terrified. We tried a few times to get her up into her wheelchair, and it took 3 people to do it, she was resistant due to the numbness in her hands and feet. TD PP reported he discussed with her the need to work the upper body otherwise she would lose her abilities and not be able to get out of bed.
Review of Physical Therapy PT Evaluation & Plan of Treatment dated 5/29/24, revealed, .Clinical Impressions: PT eval complete and POC established, patient in a lot of pain, states she has none of her pain meds since admission, therapy informing nursing. Patient seen via telehealth with her approval, not able to tolerate sitting up at this time or work on rolling as she felt like she was going to throw up at this time. Able to complete assessment for ROM and strength though very limited. States goal is to return home but unsure if attainable at this time, will continues to assess as patient progresses with skilled therapies .
Review of Occupational Therapy Evaluation & Plan of Treatment dated 5/27/24, revealed, .Clinical Impressions: Pt. requires 24 hour supervision and assistance w/ all aspects of living at this time at this time. Pt. presents with w/ declines in strength, endurance and balance at this time. Pt. is a high fall risk at this time due to residual symptoms from L5, L1 compression fractures, recent fall, s/p decompression surgery. Pt. needs to reach maximum level in order to safely return home and reduce caregiver burden .Reason for Therapy: Pt. is a fall risk at this time, due to intense fear of falling .
Review of Occupational Therapy Treatment Encounter Note dated 5/27/24, revealed, .Therapist educated staff on pt. (patient) present level, transfers status and strategies to promote safety and reduce fall risk. Pt. was pleasant and oriented. However, pt. was very fearful of falling. Pt. was unable to identify spinal precautions. Therapist demonstrated and educated pt. on spinal precautions. Therapist provided therapeutic encouragement and explained process of getting pt. to EOB (end of bed). Pt. reports no feeling in hands and feet Therapist goal was to build confidence and promote participation, pt. continued to show increased anxiety and refused to transition to EOB due to intense fear of falling as observed by pt. becoming emotional. Therapist stressed importance and purpose of therapy and engaged pt. in visualizing goals in order to promote hope. These factors greatly impacted the duration of evaluation .
Review of Weekly Wound Note dated 5/28/2024 at 10:59 AM, revealed, .Location/Type/Stage if applicable : Lumbar back surgical incision: 30 staples present .Wound Measurements: Length x Width x Depth: 14.5, edges approximated .Wound Base: %Epithelial/Granulation/Slough/Eschar/other: N/A .Drainage: Type/color/amount/odor: No drainage, no odor, skin in neutral in color with no redness noted .Tunneling/Undermining: Y/N then enter _to_o'clock &cm deep: None .Wound Edges: Attached/Unattached/Rolled/Macerated/Calloused: Approximated .Surrounding skin: Normal/Edematous/Non-blancable/Dry/Macerated/Discolored/Excoriated: Normal skin tone, no s/s of infection noted .Wound Progression: Improved/No change/Stable/Declined: Stable .Pain associated with wound: Y/N: Tender r/t surgery .
Review of Occupational Therapy Treatment Encounter Note dated 6/1/24, revealed, .97530: Pt approached for treatment with pt agreeing to sit EOB during tx (treatment) session. Pt moves from supine to EOB with max A (therapist performs approximately 75% of the work in a mobility task) with pt reporting she is unable to move her legs. Pt sits EOB and completes LE (lower extremity) exercises of kicks and ankle pumps and UE (upper extremity) AROM (active range of motion) exercises mirroring the movements of this COTA. Pt returns to supine and is TD (total dependence) to boost in bed .
Review of Physical Therapy Treatment Note dated 6/4/24, revealed, .97530: Pt engaged in bed mobility rolling U/R X max assist of 2. Pt completed supine >< EoB x max x2. Pt completed sit X stand x max of 3 with bracing of BLE (bilateral lower extremities) from WC (wheelchair) >< 2WW (wheeled walker). Positioning in supine completed x max of 2 for comfort, donning/doffing or (sic) LSO (lumbar-sacral orthotic -brace) x max x 2 .
Review of Nursing Progress Note dated 6/3/24 at 4:54 PM, Unit Manager VV been down to the gym. Patient then states Roommate then talked about her well-being getting help for her depression. Patient stated I am not depressed, and I am not crazy, both roommate and this writer sympathized with patient and said getting help through our (Mental Health provider) services does not mean you're crazy or that it would be long term. Explained that sometimes it helps to talk to someone after having multiple health issues and they could give her ways to help cope. Patient then stated to her roommate that her house is chaos .
In an interview on 07/12/24 at 10:39 AM, Resident # 406 reported she was not approached by staff to speak to someone for any grief or depression. She reported she was feeling bummed as she would have hoped that she would have been out of here by now but was happy that she was starting therapy and can see the light at the end of the tunnel and hoping to get out of here soon.
In an interview on 07/12/24 at 09:27 AM, Social Service Director (SSD) C reported she did not complete a trauma assessment for Resident #406. SSD C reported a referral to contracted (mental health services provider) for the long term care residents that have any psychiatric diagnosis or medications, she reported she would meet with them and discuss mental health services and referral to the (mental health services provider). If the resident was here for subacute rehab and the time does not fall in line to when the provider will be here, she reported she would provide supportive visits, get the activities department involved, and our physician. If there were acute concerns and (mental health services provider) was not coming, the resident would get sent out. SSD C reported before the resident was sent out to the emergency room, she would go and meet with the resident, gather information, do a risk assessment to determine the risk of self harm and then petitioning depends on the situation like if the resident was actively suicidal and had a plan, self-neglect which is considered self-harm, would petition the resident as sending them to the ER they would be sent right back. For Resident #406, she came to the facility initially for subacute rehab, she had little motivation, initially she was in a lot of pain which was self-limiting, her friend came in and gave some background indicated this was kind of her baseline at home. When queried if the resident had her back pain at the time the roommate was referencing, SSD C reported she was unsure. SSD C reported the ex-husband reported she had a history of trauma as he father had abruptldy passes away and this sent the resident into a mental breakdown. Note: Resident's father passed away in 2012 per SSD C. SSD C reported the resident had transitioned to long term care prior to her psychiatric hospitalization. SSD C reported her case as discussed at IDT team meeting and the resident's surgical site had began to open and she as placed on oral antibiotics, she had developed a wound on her bottom, it was determined she was self-harming due to her self neglect, we felt it was appropriate to petition for mental health treatment. SSD C reported she felt she needed more immediate attention and she did not refer her to the outside (mental health service provider) as the provider was not coming to the facility due to vacation. SSD C did report the social worker for the outside mental health provider would be coming to the facility. They came on the opposite week of the provider. When queried if she had contacted the outside mental health provider service to come and evaluate the resident she reported she had not contacted them.
In an interview on 07/11/24 at 09:38 AM, Unit Manager (UM) W reported she had lumbar surgery and she was refusing cares. She doesn't like to offload pressure, or to turn, she liked to be on her back. UM W reported her back hurt, the back brace hurts her and that was why she was not up in her chair. UM W reported a lot of what was happening was due to fear, she reported she can't feel her feet, and she was fearful of falling. UM W reported Resident #406 was very smart, answered questions appropriately.
In an interview on 07/12/24 at 09:48 AM, Director of Nursing (DON) B reported during Resident #406's time with us, she was declining cares and was unmotivated when working with therapy. Resident #406 was choosing not to allow the staff to complete incontinence care and just basic hygiene care as a result her surgical wound began to open, and she had developed an open area on her bottom. Her roommate reported she was the same at home by declining to perform self-hygiene and had incontinent episodes in her bed. Her ex-husband had shared she had a history of tragedy in her life which was not dealt with and her behaviors he believed to be underlying causes to those behaviors. DON B reported the resident's actions were not matching her words as she had indicated she wanted to discharge. When queried whether the resident was septic or on an IV antibiotic, DON B reported she was not. DON B reported the intention was to help the resident, but the facility did not work to provide alternative lesser restrictive services prior to petitioning her and sending her to a psychiatric hospital for declining cares. When asked if other residents in the facility declined care, the DON reported there were. DON B reported she had worked at other facilities and those social workers provided push back and advocated for their residents. DON B reported she depended on her staff to provide her with a different perspective and to complete the necessary steps to move to that point for what was best for the resident.
According to the facility's policy titled, Behavior Management Program. revised 6/2023: .Upon admission of a new resident the interdisciplinary team reviews the plan of care, and then should develop a behavior plan for the resident as needed . Behaviors shall be identified through the RAI (Resident Assessment Instrument) process and through staff interaction .Further assessments to identify and manage behaviors may be conducted . Identified behaviors should be evaluated for frequency, duration, intensity and pattern . Behaviors should be identified and approaches for modification or redirection should be included in the plan of care .3. The facility will ensure that necessary behavioral health care services are person-centered and reflect the resident's goal for care, while maximizing the resident's dignity, autonomy, privacy, socialization, independence, choice, and safety .5. Behavioral health care and services shall be provided in an environment that is conducive to mental and psychosocial well-being .7. C. Monitor the resident closely for expressions or indications of distress .d. Evaluate whether the resident's distress was attributable to their clinical condition and demonstrate that the change in behavior was unavoidable .h. Accurately document the changes, including the frequency of occurrence and potential triggers to the resident's record .i. Ensure appropriate follow up assessment .k. Evaluate resident and care plan routinely to ensure the approaches are meeting the needs of the resident .8.B. Interpersonal communication (communication between two or more people) that promotes mental and psychosocial well-being .
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that follow up with pharmacy recommendations occurred for 1 ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that follow up with pharmacy recommendations occurred for 1 resident (Resident #22) of 5 residents reviewed for medications resulting in the potential for medication side effects and/or unnecessary medications for residents.
Findings include:
Resident #22 (R22)
Review of the Face Sheet and Minimum Data Set (MDS) dated [DATE] revealed R22 admitted to the facility on [DATE] with diagnoses of type 2 diabetes, bipolar disorder, anxiety and depression. Brief Interview for Mental Status (BIMS) reflected a score of 15 out of 15 which indicated R22 was cognitively intact (13 to 15 cognitively intact).
Review of the Pharmacy to Physician Monthly Medication Regimen Review communication dated 1/29/2024 revealed the following recommendation: D/C (discontinue) the following PRN (as needed) orders. Meclizine 25 mg (milligrams) q8hr (every 8 hours) prn for dizziness and dicyclomine 20 mg q8hr prn for cramping {both have high antichol loads (anticholinergic, inhibits nerve impulses responsible for involuntary muscle movements and various bodily functions) -Beer's List medications (database of medicines that informs healthcare providers about medicines that may be inappropriate for older people)}. Resident does have a hx of GI pain and GI referral was recommended (? Colonoscopy may be needed). Evaluate if these could be d/c'd (discontinued) due to non use. The physician agreed with the recommendation and signed it.
Review of R22's current physician orders as of 7/17/2024 revealed that R22 had the following orders: meclizine HCl (hydrogen chloride) oral tablet 25 mg-give 1 tablet by mouth every 8 hours as needed for dizziness and dicyclomine HCl oral tablet 20 mg-give 1 tablet by mouth every 8 hours as needed for cramping as prn orders.
In an email received from Nursing Home Administrator (NHA) A on 7/16/2024 at 2:57 PM, NHA A stated, Yes, the d/c of the meds were missed. However, this has been addressed and an order was received from the NP (Nurse Practitioner) to d/c (discontinue).
During an interview on 7/16/2024 at 3:11 PM, Director of Nursing (DON) B stated the medications were just discontinued that day.
Review of the Medication Regimen Review Policy with an Implementation Date of 1/5/2021 and a Reviewed/ Revised date of 1/2024 revealed, Policy Explanation and Compliance Guidelines: 7e. Facility staff shall act upon all recommendations according to procedures for addressing medication regimen review irregularities.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to label, date, and store medications in 1 out of 2 medications rooms and 2 of 2 medication carts, resulting in the potential fo...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to label, date, and store medications in 1 out of 2 medications rooms and 2 of 2 medication carts, resulting in the potential for decreased efficacy of medications and the potential for the compromise of medications and/or the misappropriation of medication.
Findings include:
In an interview on 07/17/24 at 10:01 AM, Unit Manager (UM) W reported that the medication refrigerator temperatures are supposed to be monitored and recorded every shift, at approximately 4:00 AM and 4:00 PM.
During a Medication Storage observation and interview on 07/17/24 at 10:21 AM, UM G reported that the night shift nurse is responsible for monitoring the refrigerator temperatures. Review of the the B hall medication room revealed a refrigerator with multiple resident medications and vaccinations. Subsequent review of the refrigerator temperature log for the B hall revealed, multiple missing temperature records for day time monitoring and almost no monitoring at night. UM G reported that she recently moved the binder with the refrigerator logs in them to the nurses station, due to them not being checked regularly.
In an interview on 07/17/24 at 10:51 AM, Licensed Practical Nurse (LPN) Q reported that monitoring of the refrigerator is the responsibility of the night shift nurse, and not the day shift nurse.
During a Medication Storage observation on 07/17/24 at 10:32 AM along with LPN Q of the B hall medication cart, 3 bottles of stock OTC (over the counter) medications were identified with the expiration dates worn off the bottle, a used Anoro Ellipta inhaler without an open date, and an additional inhaler without a resident name, drug name, label or open date on it.
During a Medication Storage observation on 07/17/24 at 10:53 AM of A hall medication cart, along with LPN R, a loose round yellow pill was found in the cart. LPN R reported that she did not know what medication it was and/or which resident the medication belonged to.
In an interview on 07/16/24 at 10:32 AM, LPN CCC reported that when she arrived for her shift on 5/1/24 around 7:00 AM, the door for the B hall medication room was propped open and remained propped open with a trash can until approximately noon that day, when maintenance staff delivered a new key.
In an interview on 07/16/24 at 11:03 AM, Director of Nursing (DON) B reported that she was in the facility on 5/1/24 and was not made aware of any concerns with the B hall medication room being propped open, and/or a missing key. DON B reported that 5/1/24 was the day that Resident #36 had medication come up missing.
In an interview on 07/16/24 at 01:03 PM, Environmental Service Manager (ESM) L reported that a couple of months ago he had to get extra keys made for the B hall medication room, because the previous unit manager had not turned her keys in.
Review of a facility retail receipt dated 5/1/24 at 10:33 AM, indicated Keys for Nursing.
Review of the facility policy Medication Storage dated June 2019 revealed, .F. The refridgerator or freezer in which vaccines are stored should be checked at least twice a day per CDC Guidelines .Expiration Dating: .B. Medications dispensed in the manufacturer's original container will be labeled with the manufacturer's expiration date .
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents who were eligible for recommended vaccines were of...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents who were eligible for recommended vaccines were offered vaccinations in a timely manner for 2 residents (Resident #6 & #27) out of 5 residents reviewed for immunizations resulting in the potential for developing vaccine preventable disease.
Findings include:
In an interview on 07/09/24 at 08:44 PM, Nursing Home Administrator (NHA) A reported that Regional Clinical Director/Infection Preventionist (IP) KK is currently the only person that holds the Infection Preventionist Certification, and she oversees Director of Nursing (DON) B's implementation of the program.
In an interview on 07/10/24 at 03:22 PM, ICP KK reported that she had not yet familiarized herself with how the previous Infection Preventionist tracked resident vaccinations.
Resident #6
Review of an admission Record revealed Resident #6 was originally admitted to the facility on [DATE].
Review of Resident #6's Immunizations Record revealed, Influenza doses were received annually in October in 2020, 2021, 2022, and 2023. Also a Pneumovax dose on 1/1/2000 and Prevnar 13 (type of pneumococcal vaccine) on 7/17/2016.
In an interview on 07/11/24 at 10:10 AM, DON B reported that Resident #6 had consented to all vaccines on 12/2/22, but had not been offered the additonal pneumococcal vaccines that she was eligible for. DON B reported that she audited all residents' records yesterday for pneumococcal vaccination status, and had calls out to guardians for required consents.
Resident #27
Review of an admission Record revealed Resident #27 was originally admitted to the facility on [DATE].
Review of Resident #27's Immunizations Record revealed, Refused influenza, PCV13 (type of pneumococcal vaccine) and PPV23 (type of pneumococcal vaccine) immunizations, but there was no date recorded. Also included that the resident had consented and received PCV20 (type of pneumococcal vaccine) on 6/25/24.
Review of Resident #27's Vaccine Consent Form dated 12/7/23 indicated that he wanted to receive Influenza, and Pneumonia vaccines.
In an interview on 07/11/24 at 10:10 AM, DON B reported that she was unable to explain why Resident #27's record indicated refused Influenza, and that there was no documentation of declination. DON B was not able to explain why the pneumococcal vaccine was delayed until 6/25/24, after Resident #27 consented on 12/7/2023.
Review of the facility policy Pneumococcal Vaccine dated 1/2024 revealed, .2. Each resident will be offered a pneumococcal immunization unless it is medically contraindicated or the resident has already been immunized .
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure they consistently educated, offered and administered COVID-1...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure they consistently educated, offered and administered COVID-19 vaccines or maintain valid declination in the medical record for 1 resident (Resident #27) of 5 residents reviewed for vaccinations, and failed to educate, offer and track COVID-19 vaccine status staff for facility staff, resulting in the lack of vaccine tracking, the residents right to choose and receive vaccine treatment options, and the right to an informed consent.
Findings include:
In an interview on 07/09/24 at 08:44 PM, Nursing Home Administrator (NHA) A reported that Regional Clinical Director/Infection Preventionist (ICP) KK is currently the only person that holds the Infection Preventionist Certification, and she oversees Director of Nursing (DON) B implementation of the program.
In an interview on 07/10/24 at 03:22 PM, ICP KK reported that she had not yet familiarized herself with how the previous Infection Preventionist tracked resident vaccinations.
Resident #27
Review of an admission Record revealed Resident #27 was originally admitted to the facility on [DATE].
Review of Resident #27's Immunizations Record revealed, Refused COVID-19 vaccine, but there was no date recorded.
Review of Resident #27's Vaccine Consent Form dated 12/7/23 indicated that he wanted to receive COVID-19 vaccination.
In an interview on 07/11/24 at 10:10 AM, DON B reported that she was unable to explain why Resident #27's record indicated refused COVID-19, and there was no documentation of declination.
Staff:
In an interview on 07/11/24 at 10:10 AM, DON B reported that she was not sure if staff were being educated and/or offered the COVID-19 vaccination, that she did not have any documentation of tracking immunization status, but that she would look into it.
In an interview on 07/11/24 at 11:19 AM, IP KK reported that the facility was no longer offering staff the COVID-19 vaccination and therefore was not familiar with the process for tracking COVID-19 vaccination status for staff.
In a subsequent interview on 07/12/24 at 08:03 AM, DON reported that facility staff are not being educated about or offered the COVID-19 vaccination upon hire, and vaccination status is not being tracked by the facility.
Review of a facility policy Employee Vaccination dated 10/2023 revealed, .1. Vaccination Offerings: (facility) will provide or facilitate the influenza vaccination annually for employees, and, where recommended, pneumococcal and COVID-19 vaccinations .2. Recommended Vaccinations: .COVID-19: All HCP (healthcare personel) will be offered the COVID-19 vaccine per CDC guidelines .4. Documentation and Recordkeeping: Routine vaccinations declined by employees will be noted in their HR (human resource) file for reference.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to make sure residents had an operable call light within...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to make sure residents had an operable call light within reach in 1 of 18 residents (Resident #5) reviewed for call lights, resulting in the potential for delayed emergency response and negative resident outcomes.
Findings include:
Resident #5 (R5)
Review of the Face Sheet and Minimum Data Set (MDS) dated [DATE] revealed R5 admitted to the facility on [DATE] with diagnoses of vascular dementia and dysphagia. Brief Interview for Mental Status (BIMS) reflected a score of 00 out of 15 which indicated R5 was severely cognitively impaired (00 to 07 is severe cognitive impairment). She was under Hospice care.
During an interview on [DATE] at 8:53 PM, R5 was observed to be lying in bed and had emesis on her right arm, on her bed, on the floor and on her fall mat. R5 was pleasantly confused and surveyor asked her to press her call light. R5 pressed call light and it wasn't working. Then, surveyor pressed call light too and observed it wasn't working.
During an interview on [DATE] at 9:00 PM, Unit Manager (UM) G stated that she didn't know R5 had emesis and that her call light wasn't working. UM G said she wasn't sure when the call light stopped working. UM G verified that the call light wasn't working and gave R5 another call light which was verified to be working.
On [DATE] at 03:00 PM, it was observed that R5 was sitting in her Geri chair away from her bed and her call light was under her bed.
On [DATE] at 10:27 AM, it was observed that R5 was lying in bed and her call light was at the foot of her bed.
During an interview on [DATE] at 3:13 PM, Environmental Services Manager (ESM) L stated that he does call light inspections every month on every resident and he should receive work orders in between if a call light isn't working but he doesn't usually get them. ESM L said they will call him if there is a problem with a call light.
During another interview on [DATE] at 10:29 AM, UM G stated that ESM L does monthly call light checks for each resident and in between managers were checking call lights and doing audits but she couldn't remember the last time one was done. UM G also said that call light placement should be done every time a staff member walks into the room and they need to make sure the call light is by the resident.
Review of the Call Lights System Policy with an Implementation Date of [DATE] and a Review/ Revision date of 6/2023 revealed, Policy Explanation and Compliance Guidelines: 5. With each interaction in the resident's room or bathroom, staff will ensure the call light is within reach of resident and secured, as needed. 6. Staff will report problems with a call light or the call system immediately to the supervisor and/or maintenance director and will provide immediate or alternative solutions until the problem can be remedied. (Examples include: replace call light, provide a bell or whistle, increase frequency of rounding, etc.)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to develop person centered care plans in 3 (Resident #34, Resident #49,...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to develop person centered care plans in 3 (Resident #34, Resident #49, and Resident #6) of 18 residents reviewed for person centered care plans resulting in staff not monitoring for side effects of an anticoagulant medication and not monitoring a known skin condition.
Findings include:
Resident #34
Review of an admission Record revealed Resident #34 had pertinent diagnoses which included: dementia, atrial fibrillation (a-fib - an irregular rate of the heart that could cause blood clots to form) and cerebral infarction due to unspecified occlusion (a blockage of an artery interrupting blood flow to the brain, stroke).
Review of a Minimum Data Set (MDS) assessment for Resident #34, with a reference date of 4/11/2024 revealed a Brief Interview for Mental Status (BIMS) score of 9/15 which indicated Resident #34 was cognitively intact.
Review of Physician Orders for Resident #34 revealed . Xarelto tablet 20 mg give 20 mg by mouth one time a day for A-fib .ordered on 3/19/24 .
Review of Physician Order for Resident #34 revealed no order to monitor for side effects of anti-coagulant- bleeding/bruising.
Review of Care Plan for Resident #34 revealed no developed person-centered care plan related to the use of anticoagulant medication.
Resident #49
Review of an admission Record revealed Resident #49 had pertinent diagnoses which included: atrial fibrillation (irregular heart rate that could cause blood clots to form), fracture of the right lower leg, and compression fracture of T11-T12 vertebra (fracture of the middle spine) .
Review of a Minimum Data Set (MDS) assessment for Resident #49, with a reference date of 6/20/2024 revealed a Brief Interview for Mental Status (BIMS) score of 15/15 which indicated Resident #9 was cognitively intact.
Review of Physician Orders for Resident #49 revealed . Apixaban oral tablet 5 mg give 1 tablet by mouth tow times a day for hx (history) of DVT (deep vein thrombosis (blood clot in the leg)), a fib . ordered on 3/19/24 .monitor for side effect of anti-coagulant (preventing the clotting of blood) i.e. bruising/bleeding . ordered on 3/19/24 .
Review of Care Plan for Resident #49 revealed no developed person-centered care plan related to the use of anticoagulant medication.
In an interview on 7/11/24 at 1:10 PM., Unit Manager/Licensed Practical Nurse (UM/LPN) W reported that Xarelto and apixaban are both anticoagulant medications. UM/LPN W reported that the expectation was to have a care plan in place for any resident that was taking an anticoagulant medication, and the care plan should include interventions to monitor for bleeding.
Resident #6
Review of an admission Record revealed Resident #6 was originally admitted to the facility on [DATE], with pertinent diagnoses which included: other specified disorders of nose and nasal sinuses.
During an observation on 07/09/24 at 08:05 PM in Resident #6's room, the resident was lying in bed and there was a large black crusted lesion noted on her nose.
Review of Resident #6's Care Plan for information related to the skin condition on her nose. There was no problems, goals, or interventions related to the lesion on her nose.
Review of Resident #6's Practitioner Progress Notes dated 6/20/2024 revealed, .Physician regulatory visit .no longer under hospice care. The lesion on her nose is chronic and sometimes bleeds. The guardian has declined treatment for this and pt has been uncooperative for treatment.
In an interview on 07/10/24 at 03:12 PM, Certified Nursing Assistant (CNA) Z reported that she did not know what the spot on Resident #6's nose was, and did not know if she was receiving any treatments for it.
In an interview on 07/12/24 at 01:31 PM, Unit Manager (UM) W reported that Resident #6 had the lesion on her nose for years. UM W reported that is was a chronic wound due to an untreated skin cancer, and does open up at times. UM W reported that Resident #6's guardian had declined further treatment.
In an interview on 07/12/24 at 03:01 PM, Licensed Practical Nurse (LPN) R reported that Resident #6 had the chronic wound on her nose for years, and at times the crust falls off or gets scratched off and starts to bleed. LPN R reported that the last time the wound bled was about a month ago, and that nursing applied an antibiotic ointment to the area until it scabs back over.
In an interview on 07/17/24 at 12:06 PM, Director of Nursing (DON) B reported that Resident #6's nose wound is a chronic skin cancer, and that there should be orders and a care plan in place. DON B reported that in addition to orders to monitor for signs and symptoms of infection, ideally there wound also be a monthly wound note indicating the wound status.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident #34
Review of an admission Record revealed Resident #34 had pertinent diagnoses which included: dementia and major depr...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident #34
Review of an admission Record revealed Resident #34 had pertinent diagnoses which included: dementia and major depressive disorder.
Review of a Minimum Data Set (MDS) assessment for Resident #34, with a reference date of 4/11/24 revealed a Brief Interview for Mental Status (BIMS) score of 9/15 which indicated Resident #34 was moderately cognitively impaired.
In an interview on 7/9/24 at 9:06 PM., Resident #34 stated .this place is a joke, as far as wanting something to do, we sit around and watch TV, they do not engage us in activities, and I never get one to one activity . Resident #34 reported that today's activities included communion, trivia, a sing a long, and bingo. Resident #34 reported that she asked to be reminded in time for bingo and when she was walking in the hallway to bingo the nurse told her bingo was over and she missed it.
In an interview on 7/10/24 at 9:11 AM., Resident #34 reported that she was not going to any activities today, the TV in her room would be her activity today.
Review of activity scheduled for 7/10/24 revealed .10:30 exercise, 1:30 pod cast, 2:30 Roku movie .
Review of activity schedule for 7/11/24 revealed .10:30 Mad Libs, 1:30 bean bag toss, and 2:30 nail salon.
In an interview on 7/11/24 at 10:16 AM., Unit Manager (UM) G reported that activities were provided by a certified nurse assistant (CNA) that was on light duty who is currently on vacation and not in the building this week. There were no other staff in the activity department. UM G reported that Resident #34 sleeps late and misses the first couple of activities scheduled in the day. UM G reported that Resident #34 spends time watching TV in her room, she likes to get her nails done, and she likes anything to do with dogs and/or one to one activity. UM G reported that the activity department was lacking with staff.
Review of Recreation Assessment dated 10/7/2022 for Resident #34 revealed .activity pursuit patterns and preferences included reading/writing, spiritual/religious, trips/shopping, helping others, intergenerational, social/parties, pet visits, family/friends, baking/cooking, walking/wheeling outdoors, TV/movies, gardening/plants, talking/conversing .
Review of care plan for Resident #34 revealed . will be invited to participate in the activity program .will participate independent leisure activities .I want pet visits . initiated 10/7/22 .I will be invited to special events . initiated 1/18/23 .I would prefer the following groups: .may be interested in playing bingo .initiated 10/7/22 with revision on 7/19/23 . going outside when the weather is nice . initiated on 10/7/22, revised on 3/29/24 .
Review of policy, Activities implemented 1/1/24, revealed, .It is the policy of this facility to provide an ongoing program to support residents in their choice of activities based on their comprehensive assessment, care plan, and preferences. Facility-sponsored group, individual, and independent activities will be designed to meet the interests of each resident, as well as support their physical, mental, and psychosocial well-being. Activities will encourage both independence and interaction within the community .2. Activities will be designed with the intent to: a. Enhance the resident ' s sense of well-being, belonging, and usefulness .b. Create opportunities for each resident to have a meaningful life .c. Promote or enhance physical activity .d. Promote or enhance cognition .e. Promote or enhance emotional health .f. Promote self-esteem, dignity, pleasure, comfort, education, creativity, success and independence .g. Reflect resident ' s interests and age .h. Reflect cultural and religious interests of the residents .i. Reflect choices of the residents .8. Activities may include individual, small and large group activities as well as: a. Indoor and Outdoor Activities .b. Activities away from the facility .c. Religious Programs .d. Exercise Programs .e. Community Activities .f. Social Activities .g. In-Room Activities .h. Individualized Activities .i. Educational Programs .
This citation pertains to intake: MI00142051
Based on observation, interview and record review, the facility failed to provide consistent, meaningful and person-centered activities for 6 of 18 residents (Resident #11, #12, #17, #40, #406, and #34) reviewed for activities provided by the facility, resulting in the potential for loss of interaction, joy, self-esteem, growth, sense of well-being, autonomy, connectedness, identity, creativity, independence, pleasure, and comfort.
Findings include:
Review of The Boredom of Solitude published 4/21/23 by Psychology Today, [NAME] Danckert Ph.D., [NAME], Ph.D, revealed .Loneliness is a complex experience, one that can heighten our sense of vulnerability .which leads to elevated stress . and just like boredom, loneliness has been associated with poor mental health, challenges to cognitive function, and even cognitive decline in the elderly .perceived lack of meaning will color things as being boring. So, to solve loneliness, like solutions to boredom, we can't simply reach for any kind of interaction. We need things that are meaningful to us.
Despite resident's cognitive status, their activity involvement was significantly related to better scores on care relationship, positive affect, restless tense behavior, social relations, and having something to do. [NAME] D, de [NAME] J, Willemse B, Twisk J, Pot AM. Activity involvement and quality of life of people at different stages of dementia in long term care facilities. Aging Ment Health. 2016;20(1):100-9. doi: 10.1080/13607863.2015.1049116. Epub 2015 Jun 2. PMID: 26032736.
Resident #11:
Review of an admission Record revealed Resident #11 was a male with pertinent diagnoses which included insomnia, dementia, major depressive disorder, stroke, and aphasia (loss of the ability to understand or express speech caused by brain damage, like with a stroke).
Review of current Care Plan for Resident #11, revised on 1/18/23, revealed the focus, .I am here for a long term stay and will be offered activities daily . with the intervention .For 1:1 visits, I would enjoy: reminiscing, socializing (I was in the Navy and Army National Guard and enjoy talking about my service time), doing small woodworking projects, painting on canvas, going outdoors when the weather is good, and going for strolls in my wheelchair .I am of Catholic religious affiliation. I prefer not to practice .I do not like being in large groups with a lot of people talking. It confuses me .I enjoy having the daily chronicle delivered Monday - Friday. Please encourage me to attend groups of potential daily. I also needed reminders of when groups are and where .I have consent to attend community outings with activities .I have indicated that the following items are important to me: taking care of my personal belongings or things, having a shower, snacking between meals, choosing my own bedtime, having book/newspapers/magazines to read, listening to the music I like, being around pets, keeping up with the news, doing things with groups of people, doing my favorite activities, participating in religious services or practices, and going outdoors when the weather is good . like being around people, but in small groups. A lot of conversation confuses me, because I don't know if they are talking to me or someone else .I need the following equipment for leisure activities: I use my walker to navigate the building and courtyard. Please do not sit me with others in groups of potential leisure that want to do everything for me, it sometimes takes me a minute to figure things out, and if I need help I will ask a staff member .I want pet visits will be invited to special events at the facility and in the community .I would like the following groups: parties, socials, special music (jazz and musical music), special events, exercise and fitness groups, arts and crafts (painting and woodworking), movies, bingo, outdoor groups, outings, nail salon, reading groups, pet visits, exercise, and men's groups .I would love the following for independent leisure: I like to walk around the facility daily for exercise independently, socializing with others, watching television, going outside when the weather is good, and resting when I am feeling tired .Things that comfort me: being in a small quiet space by myself so that I can collect my thoughts, walking, and being outside .
Review of medical record revealed the last Recreation Assessment completed for Resident #11 was 12/28/22.
During an interview on 07/10/24 at 11:21 AM, Resident #11 reported he was in the Navy and then the National Guard. He had a medal on the wall and reported it was from powerlifting. He started powerlifting to give him something to do and it benefited him physically. Resident #11 reported he stays in his room most of the time and doesn't participate in activities much. He reported he would like activities where they would do woodworking, or building model cars and/or boats. When asked if he would participate in pottery, he reported that he would try it. He reported the facility doesn't bring him any books, magazines, or any activities he could do in his room. Resident #11 reported he really doesn't watch much TV. He reported he would like some outside activities like fishing as well. No Daily devotions were observed in the resident's room.
Resident #12:
Review of an admission Record revealed Resident #12 was a female with pertinent diagnoses which included cognitive communication deficit (progressive degenerative brain disorder resulting in difficulty with thinking and how someone uses language), COPD, asthma, difficulty in walking, diabetes, and dysphagia (damage to the brain responsible for production and comprehension of speech).
Review of current Care Plan for Resident #12 revised on 3/21/24, revealed the focus, .I am here for long term care and will be invited to participate in the activity program . with the intervention .I need the following equipment for leisure activities: my wheelchair. I also need reminders of when groups are and encouragement to attend groups . o I will be invited to special events at the facility and in the community .I would like to have the daily chronicle delivered M - F . I would like to participate in community outings . I would prefer the following groups: bingo, resident council, cooking/baking groups, special events, special music, parties, socials, and card groups . Things that comfort me: being in my room, being by myself, watching tv, and joking with staff .
In an interview on 07/09/24 at 07:33 PM, Resident #12 was observed in her room lying in her bed. She reported the facility didn't have anyone for Bingo today. The residents waited and waited for someone to come and finally another resident ran the Bingo game. She reported she liked to color, play games, and play Bingo.
Observations throughout the survey, Resident #12 was hardly in her room she went around the building socializing with others or participated in therapy.
Resident #17:
Review of an admission Record revealed Resident #17 was a male with pertinent diagnoses which included polyosteoarthritis, diabetes, anemia, high blood pressure, anxiety, depression, asthma, and abnormalities of gait.
Review of current Care Plan for Resident #17, revised on 7/10/2018, revealed the focus, .I am here for long term care and will be invited to participate in the activity program . with the intervention .For 1:1 visits, I would enjoy: socializing with staff or residents, listening to country/[NAME] music, playing board games like monopoly, having my mail delivered, therapeutic animal visits, assistance with my electronic devices, assistance with my bird feeders and other outside window decors, etc .I am Christian Reformed and want to practice independently. I would like to have bedside communion and to attend communion services .I do have consent to attend community outings with activities .I do not like: reading books, paint by number, being around people who are talking loudly, loud noise, or doing jigsaw puzzles .I have indicated that the following items are important to me: choosing what clothes to wear, taking care of my personal belongings or things, choosing my bathroom routine, having snacks available between meals, choosing my own bedtime, using the phone in private, having a place to lock my things to keep them safe, having reading material available, being around animals, keeping up with the news, doing things with groups of people, doing my favorite activities, going outside to get fresh air when the weather is good, and participating in religious services/practices at the facility. These items are available to me through daily routine preferences, 1:1 visits, independent leisure, and modified group-based activities .I like to play bingo, read the daily chronicle, go on outings with co-residents, garden (I used to have a huge flower garden), play board/card games (Monopoly, Sorry!, SlapJack, Uno, etc.), listen to music, talk on the phone to friends/family, being offered snacks from the food cart, collect coins, and watch tv/movies in my own leisurely time .I need the following equipment for leisure activities: wheelchair, hearing aides, and glasses. At times I may choose to not wear my glasses .I want pet visits .I will be invited to special events at the facility and in the community and will attend as desired .I would like to have the daily chronicle delivered to me Monday - Friday .I would prefer the following groups: bingo, bingoscize, arts and crafts, games, brainteasers, special events, therapeutic animal visits, outdoor, laugh club, men's group, arts/crafts, bingo store, resident council, movies/popcorn, current events, socials, cooking group, bingo store, dining discussions, word games, Wii Bowling (as a spectator), special music, parties, and socials .My life occupation was Electronical Engineer at Kirkhof Transformer. I also used to work as a bouncer and DJ .Things that comfort me: reading the daily chronicle in the morning, playing board games (such as monopoly, sorry!), arts and crafts activities (scratch pictures, abstract art), listening to music (Country, Western, [NAME], 70s-80s music), and socializing with family or staff .
Review of medical record revealed the last Recreation Assessment completed for Resident #17 was 1/11/2021.
In an interview on 7/10/24 at 11:37 AM, Resident #17 reported there were no activities staff after 4:00 PM and they had no activities on the weekends. He reported the facility had gotten rid of the activity aides and the director had left a few months ago because she could not do it all herself. The facility cannot afford more activity staff for after hours and weekends.
Resident #40:
Review of an admission Record revealed Resident #40 was a female with pertinent diagnoses which included Alzheimer's disease, weakness, dementia, lack of coordination, muscle weakness, mild cognitive impairment, and repeated falls.
Review of current Care Plan for Resident #40, revised on 7/10/2018, revealed the focus, .I am here for long term care and will be invited to participate in the activity program . with the intervention .Encourage me to try new groups of potential leisure .For 1:1 visits, I would enjoy: socializing, reminiscing, going outside, planting or taking care of plants, coloring supplies, magazines, cards, and going of a stroll in the facility .I am of Pentecostal religious affiliation and want to participate with religious activities at the facility. I enjoy attending communion services I do not have consent to go on community outings with activities .I do not like other residents barging into my room, others coming into my room uninvited, and being cold .I have indicated that the following items are important to me: choosing my own clothes, taking care of my personal belongings, choosing between a tub bath/shower/sponge bath/bed bath, choosing my own bedtime, having snacks between meals, having family and close friends involved in discussions about my care, listening the music I like, keeping up with the news, doing things with groups of people, participating independently, going outside when the weather is good, and participating in religious service and practices .I like spending time with my family, being in my room, and attending groups of potential leisure .I need the following equipment for leisure activities: my walker and encouragement to attend .I want pet visits .I will be invited to special events at the facility and in the community .I would like the daily chronicle delivered Monday - Friday .I would love the following for independent leisure: watching television, being in my room, socializing with others, snacking, going out with my family, people watching, and resting when I am feeling tired .I would prefer the following groups: games (bingos), arts and crafts, religious groups, outdoor activities, gardening, socialization, parties, socials, pet visits, and other groups that I choose .My life occupation was Nurses Aide .Things that comfort me: being in my room, being with my family, and doing my favorite activities .
Review of medical record revealed the last Recreation Assessment completed for Resident #40 was 8/30/22.
In an interview on 07/10/24 at 11:18 AM, Resident # 40 reported no one showed up to run Bingo so another resident ended up calling the numbers. She reported the activities staff left and the facility had not replaced her yet
Resident #406:
Review of an admission Record revealed Resident #406 was a female with pertinent diagnoses which included spinal stenosis (space inside the bones of the spine get too small), wedge compression fracture of fifth lumbar vertebra (spinal compression fracture that occurs when the front of a vertebra collapses, but the back does not), wedge compression fracture of first lumbar vertebra, fusion of spine (surgical procedure that permanently joins two or more vertebra together so there is no movement between them), muscle weakness, difficulty in walking, unsteadiness on feet, and lack of coordination. Note: No mental health diagnoses currently in the electronic medical record.
Review of current Care Plan for Resident #406, revealed no care plan for activities.
Review of medical record for Resident #406 revealed no Recreation Assessment was completed by the Activities Department.
During an observation on 7/10/24 on Hallway II, there were no activities that were posted on the scheduled activities on the corkboard by the nursing station were observed from 11:30 AM to 4:00 PM. Also noted no individualized activities throughout initial tour, unit observations, sampled resident observations, as well as individual non-sampled residents in their rooms/hallways were observed throughout the day.
During an observation on 7/11/24 on Hallway II, there were no activities that were posted on the scheduled activities on the corkboard by the nursing station were observed from 10:0 AM to 2:00 PM. Also noted no individualized activities throughout initial tour, unit observations, sampled resident observations, as well as individual non-sampled residents in their rooms/hallways were observed throughout the day.
The scheduled 7/12/24 activities at 2:30 PM, Courtyard/Ice Cream Social was canceled and no other activity put in place. The weather during the survey was 7/10/24: 76 degrees, 7/11/24: 83 degrees, 7/12/24: 84 degrees, 7/16/24: 80 degrees, and 7/17/84: 81 degrees. No outside activities took place during the survey. Also noted no individualized activities throughout initial tour, unit observations, sampled resident observations, as well as individual non-sampled residents in their rooms/hallways were observed throughout the day.
Review of the activity calendars for May, June, and July 2024, revealed no outings scheduled. No activities after 4:00 PM and no scheduled activities on Saturdays.
In an interview on 07/16/24 at 10:13 AM, Certified Nursing Assistant (CNA) P reported she had been filling in, while on light duty, as an activities aide. She reported she does not have attendance sheets and any activities she does with the residents she would go into the electronic medical record and document in the appropriate task section. CNA P reported she does not have any prior experience in activities as she worked as a CNA at the facility prior to being placed on light duty.
In an interview on 07/17/24 at 10:27 AM, revealed, the facility not had an Activities Director since mid-May 2024. Administrator A reported the facility had been using a light duty certified nursing assistant (CNA) to complete activities for the residents.
During an interview on 7/9/24 at 7:45 PM, Dietary Aide (DA) F stated, I worked in Activities for a while. The facility fired all the activities aides and kept the Activity Director. The facility had to do budget cutbacks and Activities got hit the hardest. The residents do not always have activities going on. It's sad because the residents like their activities.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident #304 (R304)
Review of the Face Sheet and Minimum Data Set (MDS) dated [DATE] revealed R304 admitted to the facility on ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident #304 (R304)
Review of the Face Sheet and Minimum Data Set (MDS) dated [DATE] revealed R304 admitted to the facility on [DATE] with diagnoses of anxiety, depression, and dementia. Brief Interview for Mental Status (BIMS) reflected a score of 14 out of 15 which indicated R304 was cognitively intact (13 to 15 cognitively intact).
During an interview on 7/09/2024 at 8:17 PM, R304 stated that she was left in urine for about an hour that day. She was teary eyed while talking about it and said it didn't make her feel good. R304 said that she asked to get up several times and it took them about an hour to get to her up. R304 stated that she knows lying in urine isn't good for her skin and she was worried about developing pressure ulcers on her bottom. This citation pertains to intake MI00143238 and intake MI00142051
Based on observation, interview, and record review the facility failed to ensure sufficient staffing to meet the needs of 5 (Resident #2, Resident #15, Resident #17, Resident #304, and Resident #406) of 18 residents and 12 resident council meeting members reviewed for staffing, resulting in the potential for residents to not maintain their highest practicable physical, mental, and psychosocial well-being.
Findings include:
Resident #2
Review of an admission Record revealed Resident #2 had pertinent diagnoses which included: acquired absence of the right leg above the knee, acquired absence of the left leg above the knee, and paraplegia.
Review of a Minimum Data Set (MDS) assessment for Resident #2, with a reference date of 6/14/2024 revealed a Brief Interview for Mental Status (BIMS) score of 13/15 which indicated Resident #2 was cognitively intact.
In an interview on 7/9/24 at 7:18 PM., Resident #2 reported that it could take an hour or more for the staff to answer his call light.
In an interview on 7/16/24 at 11:32 AM., Resident #2 reported that yesterday he did not get his shower. Resident #2 reported that the CNA came to him and told him she was not going to be able to get his shower done because they were short staffed. Resident #2 reported that he did use his call light to remind the staff it was his shower day and that it took an hour or hour and a half for the staff to respond to his call light.
Resident #15
Review of an admission Record revealed Resident #15 had pertinent diagnoses which included: muscle weakness, dependence on wheelchair, morbid (severe) obesity.
Review of a Minimum Data Set (MDS) assessment for Resident #15, with a reference date of 6/8/2024 revealed a Brief Interview for Mental Status (BIMS) score of 15/15 which indicated Resident #15 was cognitively intact.
In an interview on 7/10/24 at 10:45 AM., Resident #15 reported that she had sat in a wet and soiled brief on more than one occasion for one or two hours waiting for assistance for incontinent care and to have her brief changed. Resident #15 reported that she has had to wait for over an hour for her call light to be answered. Resident #15 reported that having to wait long time for her call light to be answered makes her angry. Resident #15 reported that she has taken notes on her cell phone of specific dates that she had to wait extended time for her call light to be answered. Resident #15 reported that on March 8, 2024, and April 18, 2024, she waited for 2 hours for her call light to be answered when she needed incontinent care for a bowel movement. Resident #15 reported that would be acceptable to wait 15 minutes to have incontinence care done but an hour or two was too long to wait.
In an interview on 7/11/24 at 1:44 PM., Resident #15 reported that last night during night shift she had to wait over an hour for her call light to be answered.
During an observation on 7/12/24 at 1:40 PM., Resident #15's call light was noted to be on.
In an interview on 7/12/24 at 1:50 PM., this surveyor entered Resident #15's room after knocking and with permission and Resident #15 reported that she had turned on her call light requesting assistance with incontinence care. Resident #15 reported that her call light had been on for about 10 minutes.
During an observation on 7/12/24 at 1:54 PM., Resident #15's call light was answered, and care was provide as requested by Resident #15.
In an interview on 7/16/24 at 11:22 AM., Resident #15 reported that last night she turned on her call light requesting incontinence care for a bowel movement at 12:15 AM and she waited over an hour for her call light to be answered. Resident #15 reported that the call light was answered at 1:20 AM.
Resident #17
Review of an admission Record revealed Resident #17 had pertinent diagnoses which included: muscle weakness, lack of coordination, shortness of breath, and morbid (severe) obesity.
Review of a Minimum Data Set (MDS) assessment for Resident #17, with a reference date of 4/25/2024 revealed a Brief Interview for Mental Status (BIMS) score of 15/15 which indicated Resident #17 was cognitively intact.
During a resident council meeting on 7/11/24 at 1:30 in the main dining room with 12 residents that attended, it was reported by Resident #15 that call light wait times have been up to and over an hour before the light was answered. Resident #17 reported that call light wait times have taken up to and over an hour on the night shift for staff to respond.
Review of Resident Council Minutes dated 1/24/24 revealed .nursing staff don't always come right back on second and third shift . (call light) waits are long especially if there is a split assignment .
Review of Resident Council Minutes dated 2/28/24 revealed . call light times can be long .
Review of Resident Council Minutes dated 3/27/24 revealed . call lights . sometimes it takes a while for them to answer depending on who is working .third shift is horrible, after 11 pm you can never get someone .hit and miss depending on the shift and if there is a split .3rd shift after 11 pm is hard to get someone, they are always sitting at the desk and on their phones .Ratio of staff addressed to administration with response that administration is working on ratios, four new staff joined the team today .
Review of Resident Council Minutes dated 4/24/24 revealed . call lights not being answered . hit or miss 10-12 pm .
Review of Resident Council Minutes dated 5/22/24 revealed .call lights are getting faster .
In an interview on 7/9/24 at 7:30 PM., Certified Nurse Assistant (CNA) D CNA I and CNA O reported that typical staffing is two CNAs for the B side. CNA D reported that her normal assignment was about 14 residents for the shift and that there were maybe 27 residents on B side. CNA D reported that there was not enough staff to do what the residents need us to do for them.
In an interview on 7/12/24 at 10:41 AM., Director of Nursing (DON) B reported that nurses work 12-hour shift and CNAs work both 8 hour and 12-hour shifts. DON B reported that there are never less than 2 nurses scheduled for a shift day or night shift and that there should be 4 CNAs on day and second shift and 3 CNAs on night shift. DON B reported that she staffed as she saw needed. DON B reported that the residents on the 100 and 200 halls were long term care (LTC) residents with less acute needs than the residents on the rehab unit the 300 and 400 halls. DON B reported that the census fluctuated, and acuity levels of the residents changed, and the staffing would reflect those changes.
In an interview on 7/12/24 at 10:50 AM., Scheduler (S) J reported that yesterday 7/11/24 there was an unfilled role for CNA. S J reported that a CNA from night shift was mandated to stay over 4 hours. S J reported that she was unable to find a replacement CNA for the 11 am to 3 pm time. S J reported that there was no coverage by a CNA during that time. S J reported that nursing managers assisted with meals and resident care.
In an interview on 7/12/24 at 10:55 AM., DON B reported that she assisted with turning dependent residents on the B side unit during the time of 11 am and 3 pm on 7/11/24 because there were only 3 CNAs working at the time. DON B reported that her expectation when there was not sufficient staff on the floor was that the nurse managers would work on the floor in the roles that were needed.
Review of a word document provided by DON B that included all residents residing in the facility transfer status as of the date of 7/17/24 revealed the facility had a census of 53 residents and of those residents 28 resident required the assistance of 2 staff member to transfer.
During a resident council meeting on 7/11/24 at 1:30 PM., a resident that attended reported that mail was not being delivered on Saturdays.
During an observation a bundle of mail was noted outside of the nursing home administrator's (NHA) office.
In an interview on 7/11/24 at 3:29 PM., Regional Activity Director (RAD) BBB reported that the activity director should distribute the resident's mail and that the social services advocate should distribute mail as well.
In an interview on 7/11/24 at 3:36 PM., Social Services Advocate (SSA) C reported that the mail goes to the NHA A who then shares it with the Business Office Manager (BOM) AAA.
In an interview on 7/11/24 at 3:41 PM., BOM AAA reported that she distributed the mail to residents Monday through Friday. BOM AAA reported that during the weekend the mail was held until Monday because there was on one in the activity department that was here to distribute the mail on Saturday.
In an interview on 7/12/24 at 3:45 PM., NHA A reported that mail was distributed on Saturdays by a dietary aide that was scheduled to work in the kitchen every weekend.
During a resident council meeting on 7/11/24 at 1:30 PM., several residents that attended reported that there were no outing activities scheduled. A resident that attendance reported that there was no activity director at this time, and there was no one who could drive the bus for outings.
In an observation and interview on 7/11/24 at 3:29 PM., RAD BBB was noted to be conducting an activity in the activity room. RAD BBB' reported that she was helping until the new director started in the position. RAD BBB reported that she was here one day last week and 4 days this week. RAD BBB reported that she helped with completing recreational assessments for new admission residents if there was no one to complete them. RAD BBB reported that there were no activity aides, and there was a CNA who was on light duty that helped to provide scheduled activities. RAD BBB reported that this light duty CNA was not working this week.
Resident #406:
Review of an admission Record revealed Resident #406 was a female with pertinent diagnoses which included spinal stenosis (space inside the bones of the spine get too small), wedge compression fracture of fifth lumbar vertebra (spinal compression fracture that occurs when the front of a vertebra collpases, but the back does not), wedge compression fracture of first lumbar vertebra, fusion of spine (surgical procedure that permanently joins two or more vertebra together so there is no movement between them), muscle weakness, difficulty in walking, unsteadiness on feet, and lack of coordination.
Review of current Care Plan for Resident #406, revised on 6/4/24, revealed the focus, .I have an ADL self care performance deficit r/t (related to) lumbar surgery and fusion, fatigue, limited mobility, limited ROM (range of motion), muscoskeletal impairment, recent fall and history of falls, BLE (bilateral lower extremeties) weakness, pain . with the intervention .I have spinal precautions: No bending or twisting at the waist, no lifting greater than 10 lbs, up in chair as tolerated with my lumbrosacral orthotic on .Bed Mobility: x2 max assist, ensure that I am using my spinal precautions .Shower 2 assist Wednesday and Saturday 7-3 .
Review of Minimum Data Set (MDS dated 5/31/24, revealed, .Section F: How important is it to you to choose between a tub bath, shower, bed bath, or sponge bath? .Very Important .
Review of a Minimum Data Set (MDS) assessment for Resident #406, with a reference date of 5/31/24 revealed, .Section GG: E. Shower/bathe self: The ability to bathe self, including washing, rinsing, and dryign self (excludes wahing of back and hair) .2. Substantial/maximal assistance .A. roll left and right: the ability to roll from lying on back to left and right side, and return to lying on back on the bed .01. Dependent .B. Sit to lying: The ability to move from sitting on side of bed to lying flat on the bed .01. Dependent .C. Lying to sitting on side of bed: The ability to move from lying on the back to sitting on the side of the bed and with no back support .01. Dependent .
In an interview on 07/10/24 at 09:50 AM, Resident #406 reported she has not had a shower and not been offered a shower or bed bath.
In an interview on 07/12/24 at 10:39 AM, Resident #406 reported it had been approximately 4-6 weeks since her hair has been washed and she had not received a bath or a shower.
In an interview on 07/12/24 at 03:15 PM, Resident #406 reported no staff had offered to provide her with a shower or bath and the most any had done was a quick wash with a wash cloth on her upper stomach area and down the tops of her arms. Resident #406 reported she had not been asked or provided a shower/bath since her initial admission a few months ago.
In an interview on 07/10/24 at 10:53 AM, Certified Nursing Assistant (CNA) N reported she had 15 residents assigned to her on hallway II. There were three persons for hoyer transfers. CNA N reported she tried to get the showers done for the residents on the hallway, depends on the day and what was happening on the hallway. CNA N reported the showers were documented in the medical record and on a skin monitoring form. She reported she tried to get everything done for the resident and still try to get out on time. CNA N reported most days there were 3 CNAs scheduled for the building. She reported she was by herself this week on the hallway.
In an interview on 07/11/24 at 01:19 PM, Cerfified Nursing Assistant (CNA) FF reported she had worked last night to help out and as nobody came in to work. CNA FF reported she had Rooms: 20-37. CNA FF reported the lunch come first to the back hallway (hallway III) and by the time that gets done, she comes over here (hallway II) for the lunch. The building was split between the three of them as the other CNA who worked last night could only stay so long over and she had to go home.
In an interview on 07/11/24 at 01:46 PM, Unit Manager (UM) W reported she had informed the staffing person first thing this morning there was only 3 aides on today. She reported she had informed the Administrator A at approximately 10:30 AM as the overnight CNA would be leaving at 11:00 AM and the floor would be left at 3 CNAs for a census of 54 residents. UM W reported the facility did not use agency staff for the CNAs only for the nurses.
In an interview on 07/11/24 at 01:51 PM, Certified Nursing Assistant (CNA) V reported she had the front half of hallway II and the whole other hallway (hallway I). Note: Rooms 1-19 single occupancy rooms.
In an interview on 07/16/24 at 02:19 PM, Unit Manager (UM) W reported the acuity on the other side (rehab and long term care) we had talked to some of the nurses about the lack of documentation in the medical records. With the amount of admissions and discharges it was hard for the nurses. UM W reported she thought the nurses want to do a good job, she thought but it was just hard to do with all that had to be done. UM W reported the agency nurses seem to just be passing medications, there was no staff development person to educate staff and it would be good to have a staff development person as it was hard to educate all the staff and to babysit staff to ensure the staff were doing what they were supposed to do. UM W reported the staffing was determined by the numbers and no on the acuity of the units.
Review of Facility Assessment dated 5/6/24, revealed, .Resident Acuity Affecting Nurse Aides: 32 residents provided assistance with dressing, 42 residents provided assistance with bathing, 11 residents provided assistance with eating, 45 residents provided assistance with toileting, and 16 residents provided assistance with mobility .
Review of Fundamentals of Nursing ([NAME] and [NAME]) 8th edition revealed: Burnout is the condition that occurs when perceived demands outweigh perceived resources ([NAME] et al., 2013a). It is a state of physical and mental exhaustion that often affects health care providers because of the nature of their work environment. Over time, giving of oneself in often intense caring environments sometimes results in emotional exhaustion, leaving a nurse feeling irritable, restless, and unable to focus and engage with patients ([NAME] et al., 2013b) .Compassion fatigue impacts the health and wellness of nurses and the quality of care provided to patients .When a nurse experiences ongoing stressful patient relationships, he or she often disengages ([NAME] et al., 2011) .It is not uncommon for nurses who are experiencing compassion fatigue to become angry or cynical and have difficulty relating with patients and co-workers (Young et al., 2011). [NAME], [NAME] A.; [NAME], [NAME] Griffin; Stockert, [NAME]; Hall, [NAME]. Fundamentals of Nursing - E-Book (Kindle Locations 1671-1672). Elsevier Health Sciences. Kindle Edition.
During an interview on 7/9/24 at 7:45 PM, Dietary Aide (DA) F stated, I worked in Activities for a while. The facility fired all the activities aides and kept the Activity Director. The facility had to do budget cutbacks and Activities got hit the hardest. The residents do not always have activities going on. It's sad because the residents like their activities.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to properly monitor and follow resident refrigerator pro...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to properly monitor and follow resident refrigerator protocol for 19 residents of 19 residents reviewed to ensure temperatures were within range, resulting in the potential for food born illness.
Findings include:
During an observation on 7/09/24 at 7:19 PM, room [ROOM NUMBER] had a personal refrigerator with no visible temperature log. Resident reported staff did not keep track of the temperature.
During an observation, interview, and record review on 7/09/24 at 7:43 PM, Dietary Aide (DA) F observed checking personal refrigerator temperatures stating, The frigs (refrigerators) are checked every day either by myself or another kitchen staff that is part-time. Reviewed with DA F, June 2024's resident's personal temperature log with multiple missing documentations. Observed copy of June 2024 resident personal refrigerator temperature log with DA F. DA F stated, I'm supposed to be done with work at 7:30 PM but since the State is here, I was told to get the temps (temperatures) and make sure everything is picked up, like trays and snacks. Usually, personal frig temps are done between lunch and dinner if staff has time. I could not find the July (2024) temperature log, so I started one on this blank page. Observed a blank sheet of paper the staff was recording temps on.
During an observation on 7/09/24 at 8:24 PM, room [ROOM NUMBER] had a personal refrigerator. The thermometer on the top shelf read 46 degrees. The freezer was filled with frost. The resident stated, Staff check it every day.
During an observation on 7/09/24 at 8:41 PM, room [ROOM NUMBER] had a personal refrigerator with no visible temperature log.
During an observation on 7/09/24 at 8:52 PM, room [ROOM NUMBER] had a small personal refrigerator. Handwritten note on door of refrigerator reported food was to be labeled and dated. No thermometer inside refrigerator noticed as lights were off in the room with resident sleeping.
During an interview on 7/17/24 at 10:00 AM, Dietary Manager (DM) CC stated, Depending on the job description of the staff of any day, it depends on which staff checks the personal refrigerators that day. The amount of staffing each day also determines on what job duties are done each day as well. Duties are prioritized to the amount of staffing the kitchen is given. As census fluctuates so do the prioritized duties. Ideally, resident personal refrigerators temps and defrosting needs would be done daily. The resident nourishment refrigerators should be checked before personal refrigerators. Staff are to let me know if I am in the building or if I am not. Staff should be calling me to let me know if the refrigerator temperatures are over 41 degrees. I will ask staff Whose frig is it? Where was the thermometer? Was the thermometer dropped? Does the freezer need to be thawed? How much food is in the frig? before I tell them to turn the thermostat down.
Review of Resident Personal Refrigerator list provided via email notification on 7/17/24 at 11:35 AM by Nursing Home Administrator (NHA)A reported there were 19 residents that had a personal refrigerator in their room.
Review of facility Resident (refrigerator) Temperatures, dated May 1-31, 2024 revealed temperature readings over 41 degrees:
- 8 resident refrigerators 14 opportunities cumulative; 2 of which had readings 50 degrees and over
-15 resident refrigerators including a nurse's station missed 15 consecutive opportunities (days) each
-An additional 4 resident refrigerators including a nurse's station missed 5 cumulative opportunities
Review of facility Resident (refrigerator) Temperatures, dated June 1-30, 2024 revealed temperature readings over 41 degrees:
-room [ROOM NUMBER] - 1 of 30 opportunities
-room [ROOM NUMBER] - 1 of 30 opportunities (over 50 degrees)
-room [ROOM NUMBER] had no reading for 1 of 30 opportunities
-room [ROOM NUMBER] - 1 of 30 opportunities
-14 resident refrigerators including the nurses' station missed 16 consecutive opportunities each
- 4 resident refrigerators including a nurse's station missed 13 consecutive opportunities each with rooms [ROOM NUMBERS] missing 6 additional opportunities each
Review of facility Resident (refrigerator) Temperatures, dated July 1-17, 2024 revealed temperature readings over 41 degrees:
-room [ROOM NUMBER] -5 of 14 opportunities
-room [ROOM NUMBER] 1- 5 of 14 opportunities with 4 of the readings consecutively 50 degrees and over
-room [ROOM NUMBER] - 3 of 14 opportunities
-room [ROOM NUMBER] - 1 of 14 opportunities
-A nurses' station missed 1 of 14 opportunities
According to the 2017 FDA Food Code section 3-501.16 Time/Temperature Control for Safety Food, Hot and Cold Holding. (A) Except during preparation, cooking, or cooling, or when time is used as the public health control as specified under §3-501.19, and except as specified under (B) and in (C ) of this section, TIME/TEMPERATURE CONTROL FOR SAFETY FOOD shall be maintained: .(2) At 5C (41F) or less.
Review of facility policy, Resident Refrigerators reviewed/revised 1/2021, revealed, .it is the policy of this facility to ensure safe and sanitary use of any resident-owned refrigerators .Dormitory-sized refrigerators are allowed in a resident's room under the following conditions .the refrigerator maintains proper temperatures .Dietary staff shall record refrigerator temperatures daily on a temperature log for the refrigerator .a thermometer shall remain in the refrigerator .temperatures will be at or below 41 degrees F (Fahrenheit) .if temperatures are out of range, dietary staff shall discard any foods that require refrigeration, and take measures to remedy the problem .
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0680
(Tag F0680)
Could have caused harm · This affected most or all residents
This citation pertains to intake: MI00142051
Based on observations, interview and record review, the facility failed to employ an Activity Director with the required qualifications resulting in the po...
Read full inspector narrative →
This citation pertains to intake: MI00142051
Based on observations, interview and record review, the facility failed to employ an Activity Director with the required qualifications resulting in the potential for unmet met psychosocial needs, feelings of boredom and a lack of person-centered activities. This citation has the potential to impact all 54 who reside in the facility.
Findings include:
In an interview on 07/16/24 at 10:13 AM, Certified Nursing Assistant (CNA) P reported she had been filling in, while on light duty, as an activities aide. She reported she does not have attendance sheets and any activities she does with the residents she would go into the electronic medical record and document in the appropriate task section. CNA P reported she does not have any prior experience in activities as she worked as a CNA at the facility prior to being placed on light duty.
In an interview on 07/17/24 at 10:27 AM, revealed, the facility not had an Activities Director since mid-May 2024. Administrator A reported the facility had been using a light duty certified nursing assistant (CNA) to complete activities for the residents.
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to ensure 12 hours of in-service education was completed in 5 reviewed certified nurse assistants (CNA) (CNA H, CNA I, CNA O, CNA P and CNA ZZ)...
Read full inspector narrative →
Based on interview and record review the facility failed to ensure 12 hours of in-service education was completed in 5 reviewed certified nurse assistants (CNA) (CNA H, CNA I, CNA O, CNA P and CNA ZZ) of 5 resulting in the potential for performance concerns and decreased resident safety for all residents who resided in the facility.
Findings include:
Review of Education Spreadsheet 2024 provided by Director of Nursing (DON) B revealed categories of education included abuse, compliance, infection control, QAPI (quality assurance, performance improvement), resident rights, and communication, total of 44 nursing department employees, the date that each education was assigned, and the completion date for each employee. The Education Spreadsheet 2024 revealed no recorded completion date for 10 employees under abuse, no recorded completion date for 15 employees under compliance, no recorded date of completion for 12 employees under infection control, no recorded completion date for 23 employees under QAPI, no recorded completion date for 18 employees under resident rights, and no recorded completion date for 13 employees under communication.
Review of Course Completion History dated 7/12/24 provided by DON B revealed 5 Certified Nurse Assistants (CNA) of 5 (CNA H, CNA I, CNA O CNA P, CNA ZZ) had not completed the assigned required training categories. CNA H had not completed any trainings as assigned. CNA I completed 4 of 6 assigned required trainings. CNA O had completed 1 of 6 assigned required trainings. CNA P completed 2 of 5 assigned required trainings. CNA ZZ had not completed any trainings as assigned.
In an interview on 7/16/24 at 1:56 PM., DON B reported that CNA 12-hour in-services that were assigned were not completed.
In an interview on 7/17/24 at 9:21 AM., DON B reported that annual training was assigned upon hire and then yearly. DON B reported that there was no staff member in the role of staff development, and no one was tracking CNA 12-hour in-service completion.
In an interview on 7/17/24 at 9:23 AM., Nursing Home Administrator (NHA) A reported that the facility assigned training was computer based and included training/topics that would count towards CNA 12-hour in-service requirements. NHA A reported that these trainings were to be completed by the facility on day 2 of new hire orientation and then assigned yearly. NHA A reported that day 2 orientation was not being completed as expected by the facility staff and the trainings were not being completed by newly hired CNAs.
In an interview on 7/17/24 at 9:30 AM., DON B reported that an email was sent to employees when a training was assigned and available to be completed. DON B reported that she had received emails notifying her that she had trainings to complete.
In an interview on 7/17/24 at 10:03 AM., CNA X reported that she has not done any required in-services that were assigned, and she was notified by email that she had courses to complete.
In an interview on 7/17/24 at 12:16 PM., CNA ZZ reported that she has not done any required trainings that were assigned, and she was notified by email that she had courses to complete.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to maintain sanitary conditions in the kitchen resulting in the potential to spread food borne illness to all residents that con...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to maintain sanitary conditions in the kitchen resulting in the potential to spread food borne illness to all residents that consume food from the kitchen.
Findings Include:
During the initial tour of the kitchen on 7/09/2024 at 7:11 PM the following was observed in the reach in refrigerator:
4 salami sandwiches on white bread on tray with parchment paper on top, not sealed, no label and date
Lettuce and tomato slices were on top of the parchment paper, not covered, no label and date
1 blue pitcher with some type of juice in it, no label and date
The following was observed in the walk-in refrigerator:
Macaroni noodles in a container, no label and date
2 aluminum pans with BBQ pork , top on but not sealed, no label and date
1 deep metal pan with small cups of sour cream, no label and date
1 tray with waffle fries spread out, open to air, no label and date
During an interview on 7/10/2024 at 2:05 PM, Dietary Manager (DM) CC stated that when they have leftover food staff is supposed to put a label and date of what it is, when it was made and the expiration date. DM CC said she has to constantly remind her staff to label and date foods.
According to the 2017 FDA Food Code revealed: 3-501.17 Ready-to-Eat, Time/Temperature Control for Safety Food, Date Marking. (A) Except when PACKAGING FOOD using a REDUCED OXYGEN PACKAGING method as specified under § 3-502.12, and except as specified in (E) and (F) of this section, refrigerated, READY-TO EAT, TIME/TEMPERATURE CONTROL FOR SAFETY FOOD prepared and held in a FOOD ESTABLISHMENT for more than 24 hours shall be clearly marked to indicate the date or day by which the FOOD shall be consumed on the PREMISES, sold, or discarded when held at a temperature of 5ºC (41ºF) or less for a maximum of 7 days. The day of preparation shall be counted as Day 1.
Review of the Food Storage Policy with an Implementation Date of 5/25/2007 and a Reviewed/Revised Date of 1/2024 revealed, Policy Explanation and Compliance Guidelines
3. Refrigerated food outside of original package shall be labeled, dated, and monitored so that it is used by the use by date, frozen, or discarded, whichever is applicable 5. Ready to eat food can be stored by expiration date, until opened, then labeled with open and use-by date if not discarded. 7. Food items that are opened shall be put into sealable container or bag, labeled and dated with open and use by-date.
During a tour of the A side pantry, at 9:31 AM on 7/10/24 it was observed that eight, individually packaged yogurts were founded with manufacture best by dates of July 4, 2024. When asked how often staff should be coming down to check and stock the pantries, RD EEE stated they should come down once a day.
During a tour of the B side Pantry, at 9:40 AM on 7/10/24, it was observed that the following items were found in the refrigeration unit: two containers of potato salad dated for 7/5, a grocery bag with an open container of bologna salami dated opened on 6/23, a grocery bag with a bbq take out plate (ribs/mac and cheese) and a steak sandwich with no dates to indicate discard, and a four pack of yogurt with a best by date of July 4, 2024. At this time, an interview with Regional Dietitian (RD) EEE found that staff are supposed to come down daily and check the units. When asked how long food from outside sources are kept, RD EEE stated that they go by manufactures expiration dates or 3 days for leftovers.
According to the 2017 FDA Food Code section 3-501.18 Ready-to-Eat, Time/Temperature Control for Safety Food, Disposition. (A) A FOOD specified in 3-501.17(A) or (B) shall be discarded if it: (1) Exceeds the temperature and time combination specified in 3-501.17(A), except time that the product is frozen; (2) Is in a container or PACKAGE that does not bear a date or day; or (3) Is inappropriately marked with a date or day that exceeds a temperature and time combination as specified in 3501.17(A) .
During a tour of the kitchen, at 9:02 AM on 7/10/24, it was observed that gray chipping paint was found inside of the metal drawer of the clean utensil scoops. When asked if she could see the debris accumulation at the back of the drawer, RD EEE stated yes. After the scoops were removed from the drawer it was observed that paint chips were coming off as metal scoops slide back and forth in the drawer.
During a revisit of the kitchen, at 9:09 AM on 7/10/24, it was observed that leaking condensate was observed on the overhead ventilation system. Observation found three ventilation grates that are pushing air cold air into the kitchen food service area and slowly dripping water on the floor.
During a revisit to the kitchen, at 11:35 AM on 7/10/24, it was observed that there was cracks and open pits on the floor around and near the three-compartment sink.
During a tour of the dish machine area, at 11:40 AM on 7/10/24, it was observed that the temperature gauge on the dish machine was found with a broken lens and a shard of glass holding the dial stuck. An interview with RD EEE found that staff use a thermometer to check the temperature to make sure it works properly.
According to the 2017 FDA Food Code section 6-501.11 Repairing. PHYSICAL FACILITIES shall be maintained in good repair.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident #27:
Review of an admission Record revealed Resident #27 was a male with pertinent diagnoses which included wound on l...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident #27:
Review of an admission Record revealed Resident #27 was a male with pertinent diagnoses which included wound on left foot, dementia, altered mental status, history of foot abscess.
Review of Orders revealed no order for an external urinary catheter.
Review of current Care Plan revealed no focus for an external urinary catheter.
Review of Treatment Administration Record (TAR) revealed no monitoring of external urinary catheter.
During an observation on 07/09/24 at 07:44 PM, Resident #27 was lying in his bed and he had a catheter bag in a privacy bag on the floor under his bed frame. There was no personal protective equipment (PPE) noted in the room and there was not a sign on the door or wall at entry to indicate the resident was on enhanced barrier precautions.
During an observation on 07/10/24 at 10:58 AM, Resident #27 was observed lying in his bed and the catheter bag was in a privacy bag lying on the floor under his bed.
During an observation 07/11/24 at 01:00 PM, Resident #27 was lying in his bed and the catheter bag was on the floor in a privacy bag.
In an interview on 07/11/24 at 01:28 PM, CNA reported he had a new mattress, not put it on yet as the hospice nurse was coming to change his catheter from a condom type catheter to a foley as he had pain when the staff move him and doing that to prevent pain for him.
During an observation on 07/11/24 at 01:53 PM, Resident #27 was lying in his bed, he had his legs up over a pillows, in supine position, the catheter bag was scrunched under the bed on the floor.
In an interview on 07/16/24 at 01:48 PM, Unit Manager (UM) W reported the external catheter would not stay on and it was too distressing for when especially when he had to be turned and the pulling on it it would come off, Resident #27 would ask for it to be removed, he was miserable with it on. UM W reported the catheter bag in a privacy bag should not be on the floor as this can increase infection susceptibility. UM W reported staff should have placed a barrier under it or placed it in a basin.
Resident #23:
Review of Centers for Disease Control and Prevention (CDC) dated March 20,2024, revealed, .Enhanced Barrier Precautions (EBP) refer to an infection control intervention designed to reduce transmission of multidrug-resistant organisms that employs targeted gown and glove use during high contact resident care activities .EBP are used in conjunction with standard precautions and expand the use of PPE to donning of gown and gloves during high-contact resident care activities that provide opportunities for transfer of MDROs to staff hands and clothing .EBP are indicated for residents with any of the following: o Infection or colonization with a CDC-targeted MDRO when Contact Precautions do not otherwise apply; or o Wounds and/or indwelling medical devices even if the resident is not known to be infected or colonized with a MDRO .Effective Date: April 1, 2024 .
Review of an admission Record revealed Resident #23 was a male with pertinent diagnoses which included paralysis on left side, contracture, abnormal posture, pressure ulcer other site, contracture of left knee, and pressure ulcer of left ankle.
Review of current Care Plan for Resident #23, revised on 5/31/24, revealed the focus, .I require Enhanced barrier precautions d/t (due to) increased risk of MDRO acquisition due to my wound . with the intervention .Enhanced barrier precautions: Gown/gloves should be worn during high-contact resident care activities (Dressing, bathing, transferring, hygiene, linen changes, toileting/brief changes, device or wound care) .
During an observation on 07/09/24 at 09:44 PM, Licensed Practical Nurse (LPN) TT entered the room and she had donned gloves to assist Resident #23. She proceeded to remove the blankets and attempted to shift his right leg over a little bit, the left leg was contracted up under his right leg and was underneath his right buttock/back thigh area. Resident #23 reported he wanted the green boot of his right leg. LPN TT loosed and opened up the boot and left his right foot inside the opened boot. Observed the inside of the green boot was heavily soiled. Resident #23 had splatters of larger and smaller red marks up and down his right shin. He had a pillow under his right knee but resident reported it was not supportive enough and was causing pain for him as it was pulling his knee down and he can't straighten his right knee. LPN TT was holding Resident #23's right leg up some to prevent more pain. Resident #23 requested another pillow under his right leg and his left leg. LPN TT was asking the resident if they could leave the boot for his heel as she did not want it to be on the bed with nothing underneath it and having the heel break open. Certified Nursing Assistant (CNA) O came back to the room and she had an additional pillows for Resident #23's right and left legs. Both LPN TT and CNA O were attempting to reposition Resident #23's right leg to a comfortable position for him. CNA O placed the pillow under his left knee with no gloves or PPE on. The blue circular pad for his left foot/ankle was not preventing his foot off of the bed. CNA O took the green boot which had been on his right foot and placed it in the closet. LPN TT had not donned a gown prior to providing care to Resident #23. CNA O had not donned gloves or a gown before providing care to Resident #23.
In a interview on 07/09/24 at 09:59 PM, LPN TT reported she did not don a gown prior to providing hands on care to Resident #23. This writer and the nurse reviewed the sign on the wall outside of Resident #23's room for enhanced barrier precautions and when the PPE was required.
In an interview on 07/16/24 at 01:17 PM, Unit manager (UM) W reported Resident #23 was on enhanced barrier precautions as he had chronic wounds due to his contractures. She reported the red spots on his right shin were from scabs he had on his leg and were opened when a CNA showered him and removed the bathing blanket and the scabs came off and left those spots to heal. They were healed but red spots now left behind.
DPS 2
Based on interview and record review, the facility failed to have an active and ongoing plan for reducing the risk of Legionella and other opportunistic pathogens of premise plumbing. Findings include:
During an interview with Environmental Services Manager (ESM) L, at 2:10 PM on 7/10/24, it was found that the facility does not currently sample for Legionella or track disinfectant levels within the domestic water supply. When asked if there were ongoing control limits being maintained, ESM L stated no.
During an interview with ESM L, at 2:25 PM on 7/10/24, it was asked if he regularly meets with a team to talk about or review the water management plan, and he stated No.
A record review of the facilities Legionella Water Management Program policy, dated 11/2017, found that, a Water Management Team should be established and the considerations of team members should be followed, .Consider who among your employees, partners, and outside experts can provide these skills so that you can develop the most effective program possible. a. Those who might be part of your water management program team include: o Infection control staff who may choose to use their facility's routine surveillance for healthcare- associated Legionnaires' disease to validate their program. Important to look for healthcare-associated cases and histories for all patients with diagnosed Legionnaires' disease .Administrator, DON, Safety Committee chair, Environmental Services Manager, Employee Health, Registered Dietitian, City Water Personnel. b. Review the elements of the program at least once per year. Further review found that, .Your written program should include at least the following: a. Program team, including names, titles, contact information, and roles on the team .d. Control measures, including points in the system where critical limits can be monitored and where control can be applied .
This citation has two DPS statements
DPS 1
Based on observation, interview, and record review, the facility failed to follow infection prevention standards of practice for 1.) wound dressing change labeling and dating for 1 resident (R7), 2.) disinfecting resident-shared equipment, 3.) appropriate use of indwelling catheter cover for one resident R27, 4.) appropriated use of personal protective equipment (PPE) for EBP (enhanced barrier precautions residents for 2 residents (R7 and R23) of 18 residents reviewed for infection control, resulting in the potential of cross-contamination of blood-borne pathogens, and disease transmission to a vulnerable population.
Findings include:
R7
According to the Minimum Data Set (MDS), dated [DATE], R7 scored 13 /15 (cognitively intact) on his BIMS (Brief Interview Mental Status) with diagnoses that included a pressure injury to right elbow.
Review of R7's Order Summary dated 6/3/24, revealed, 'Right elbow .wrap with kerlix daily and PRN if soiled.
Review of R7's Care Plan dated 5/8/24, indicated the resident required enhanced barrier precautions (EBP) due to the wound on his right elbow. The goals was to use EBP to minimize the risk of MDRO transmission using interventions that included clean/disinfect reusable medical equipment after every use .gown/gloves should be worn during high-contact resident care activities .
During an observation and interview on 7/9/24 at 7:30 PM, Licensed Practical Nurse II stated, (R7) has a wound on his right elbow. Day shift does the wound dressing. I'm working 2nd shift. I do not look at it unless an aide tells me I need to.
Observed on 7//9/24 at 9:15 PM, R7 to have a dressing to his right elbow that was not labeled or dated.
During an observation and interview on 7/10/24 at 4:10 PM, observed dressing to R7's right elbow that was not labeled or dated. Resident stated, They (referring to nursing staff) never write on it.
During an observation and interview on 7/10/24 at 4:15 PM, Registered Nurse (RN) T stated, The dressing on (R7's) right elbow should be labeled and dated to other staff know when it was changed for infection control. There is no label or date on this dressing so there is no idea when it was done.
During an interview and record review on 7/17/24 at 11:22 AM, Corporate Clinical Consultant (CCC) KK stated, The facility uses the nursing resource, [NAME] and [NAME], for dressing changes, it directs that wound dressings should be labeled with dressing with date, the nurse's initials and time of dressing to provide a record to determine when to next change the dressing for infection control purposes.
Review of R7's Order Summary dated 5/15/24 revealed, I require Enhanced Barrier Precautions related to wound to my right elbow.
In an interview and observation on 7/9/24 at 07:20 PM, R7 had a bandage on his right elbow with no date on it, with an open wound under his right elbow that had a light scab on it, like a film.
During an observation and interview on 7/09/24 at 7:30, R7 had Enhanced Barrier Precautions signage on the wall next to his room's door. LPN II stated, (R7) has a wound on his right elbow. Observed with the LPN, a cupped elbow pad with dime size serosanguinous (bloody drainage) on it lying on the floor across room from resident's bed. The LPN looked at it and left the room without addressing it.
During an interview and observation on 7/10/24 at 4:15 PM, RN T entered R7's room and looked at an elbow pad on the resident's floor in the same spot as morning observation and day prior. RN stated, That should not be on the floor with blood on it. If housekeeping was in here, they should have notified nursing or CNA (certified nursing assistant) to bag it and throw it away and get the resident a new one. It is an infection control issue.
During an interview on 7/10/24 at 4:50 PM, Director of Nursing (DON) B and Infection Control Preventionist (IPC)/Regional Consultant KK stated, Any item that is soiled or has blood on it should be handled immediately and taken care of for infection control issues. (R7) does wear an elbow pad and does have a wound on his right elbow.
During an interview on 7/10/24 at 04:10 PM, CNAs X and I stated regarding R7, Housekeeping cleaned his room while he was at an appointment today. Neither one of us know anything about a bloody item on the floor. We have been in his room today.
During an observation and interview on 7/11/24 at 9:40 AM Housekeeping OO stated, If blood is found in a resident's room, housekeeping is to notified nursing or CNAs to pick it up and then housekeeping cleans it with bleach.
Review of facility policy, Cleaning and Disinfection of Resident-Care Equipment, date revised 2/22, revealed, Policy: Resident-care equipment can be a source of indirect transmission of pathogens. Reusable resident-care equipment will be cleaned and disinfected in accordance with current CDC recommendations in order to break the chain of infection . Disinfection is a process of eliminating microorganisms, except spores, from inanimate objects, usually by chemical means .Staff shall follow established infection control principles for cleaning and disinfecting reusable, noncritical equipment . Each user is responsible for routine cleaning and disinfection of multi-resident items after each use, particularly before use for another resident .
During an observation on 7/17/24 at 9:38 AM, LPN Q took a resident-shared vital sign machine from a hallway and went into a resident room to take a blood pressure prior to administering medication. The resident was in the bathroom sitting in her wheelchair, waiting to be transferred to the toilet. After the blood pressure was used on the resident, the LPN took the machine back out into the hall, did not clean it, and continued to her medication cart to prep medications for administration.
During an interview on 7/17/24 at 10:00 AM, Unit Manager (UM) G stated, Resident-shared equipment should be cleaned after use on each resident. There are disinfectant wipes all over the facility including the medication and treatment carts. The facility does not keep disinfectant wipes on equipment any longer for safety reasons.
During an observation and interview on 7/17/24 at 10:05 AM, LPN Q stated while looking in her medication cart, I do not have disinfectant wipes in this cart. Where would I put them in here? There is no room. I did not know staff had to come to the nurses at medication carts to get the disinfectant wipes. When asked if the nurse cleaned the vital sign machine after using on the resident, the nurse stared at the surveyor and did not give an answer.
During an interview on 7/17/24 at 11:22 AM, the DON (Director of Nursing/ICP) and CCC KK stated, Resident-shared equipment should be cleaned after used on each resident for infection control purposes. The disinfectant wipes should be hung in a bag on each piece of equipment.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0940
(Tag F0940)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to maintain an effective training program, which included trainings in resident rights, abuse, neglect, and exploitation, quality assurance, in...
Read full inspector narrative →
Based on interview and record review the facility failed to maintain an effective training program, which included trainings in resident rights, abuse, neglect, and exploitation, quality assurance, infection control, compliance and ethics, and communication for all new, existing, and contractual nursing department employees resulting in the potential for decreased resident safety for all residents who resided in the facility.
Findings include:
Review of Education Spreadsheet 2024 provided by Director of Nursing (DON) B revealed categories of education included abuse, compliance, infection control, QAPI (quality assurance, performance improvement), resident rights, and communication, total of 44 nursing department employees, the date that each education was assigned, and the completion date for each employee. The Education Spreadsheet 2024 revealed no recorded completion date for 10 employees under abuse, no recorded completion date for 15 employees under compliance, no recorded date of completion for 12 employees under infection control, no recorded completion date for 23 employees under QAPI, no recorded completion date for 18 employees under resident rights, and no recorded completion date for 13 employees under communication.
Review of Course Completion History dated 7/12/24 provided by DON B revealed 5 Certified Nurse Assistants (CNA) of 5 (CNA H, CNA I, CNA O CNA P, CNA ZZ) had not completed the assigned required training categories. CNA H had not completed any trainings as assigned. CNA I completed 4 of 6 assigned required trainings. CNA O had completed 1 of 6 assigned required trainings. CNA P completed 2 of 5 assigned required trainings. CNA ZZ had not completed any trainings as assigned.
In an interview on 7/16/24 at 1:56 PM., DON B reported that required annual training were not completed by nursing department staff.
In an interview on 7/17/24 at 9:21 AM., DON B reported that annual trainings were assigned upon hire and then yearly. DON B reported that there was no staff member in the role of staff development, and no one was tracking employee completion of required assigned trainings.
In an interview on 7/17/24 at 9:23 AM., Nursing Home Administrator (NHA) A reported that the training was computer based and expected to be completed by employees inside the building, while clocked in, but not while assigned to residents to provide care. NHA A reported that there was no staff member in the role of staff development. NHA A reported that required trainings should be part of the new hire orientation, specifically on day 2 during in person facility training. NHA A reported that day 2 orientation training was not being completed as expected by the facility staff.
In an interview on 7/17/24 at 9:30 AM., DON B reported that an email was sent to employees when a training was assigned and available to be completed. DON B reported that she had received emails notifying her that she had trainings to complete.
In an interview on 7/17/24 at 10:03 AM., CNA X reported that she has not done any required trainings that were assigned, and she was notified by email that she had courses to complete.
In an interview on 7/17/24 at 12:16 PM., CNA ZZ reported that she has not done any required trainings that were assigned, and she was notified by email that she had courses to complete.