Marvin & Betty Danto Health Care Center



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Marvin & Betty Danto Health Care Center currently has a Trust Grade of F, which indicates significant concerns about the quality of care provided. They rank #295 out of 422 nursing homes in Michigan, placing them in the bottom half of facilities in the state, and #21 out of 43 in Oakland County, meaning only a few local options are worse. The facility is showing a worsening trend, with issues increasing from 5 in 2024 to 15 in 2025, and has accumulated a concerning $145,315 in fines, which is higher than 85% of Michigan facilities. While staffing is rated as average with a 53% turnover, the RN coverage is also average, meaning there is some stability in staff, but many residents may not receive the best care. Specific incidents include a failure to monitor a resident's blood sugar and report abnormal lab results, leading to a delay in necessary care, as well as inadequate preventive measures against pressure ulcers for residents, resulting in serious health risks. Overall, while there are some strengths in staffing, the facility has significant weaknesses that should be carefully considered.
- Trust Score
- F
- In Michigan
- #295/422
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 53% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $145,315 in fines. Lower than most Michigan facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 33 minutes of Registered Nurse (RN) attention daily — about average for Michigan. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 49 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Michigan average (3.1)
Below average - review inspection findings carefully
Near Michigan avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 49 deficiencies on record
Apr 2025
5 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to Intake MI00149648.
Based on observation, interview and record review, the facility failed to obtain co...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to Intake Number(s): MI00150488.
Based on observation, interview, and record review, the facility failed ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to Intake Number(s): MI00149894.
Based on observation, interview, and record review, the facility failed ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to Intake MI00149894
Based on observation, interview and record review, the facility failed to prevent pr...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to maintain a sanitary healthcare environment amongst residential common...
Read full inspector narrative →
Jan 2025
10 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to obtain an assessment and physician's order for self-adm...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure timely and accurate advanced directives informat...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to assess a resident for alternative or augmentative com...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure an order for supplemental oxygen for one reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide appropriate interventions to prevent triggers for one Resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure a medication error rate less than five percent ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a clean, comfortable, homelike environment for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure medication were administered and documented pe...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure Hospice services were provided per plan of car...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** On 1/07/25 at approximately 10:44 a.m., a Medication Cart located next to room [ROOM NUMBER] was observed unlocked and unattende...
Read full inspector narrative →
Nov 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
This citation pertains to intake #MI00146798.
Based on observation and interview, the facility failed to provide an environment that promoted and enhanced residents' dignity for three (R805, R806 and ...
Read full inspector narrative →
Jun 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake #MI00145236
Based on observation, interview, and record review, the facility failed to ensure ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake #MI00145236
Based on observation, interview, and record review, the facility failed to ensure a...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake: MI00145092.
Based on observation, interview, and record review the facility failed to timely ...
Read full inspector narrative →
Feb 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake #MI00142694
Based on observation, interview and record review the facility failed to ensure an ...
Read full inspector narrative →
Dec 2023
20 deficiencies
3 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake #MI00134966 and MI00141309.
This citation has two deficient practices.
Deficient Practice #1
B...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake #'s MI00138332 and MI00135446.
Based on observations, interviews and record reviews the facili...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Deficient Practice #2
Based on observation, interview and record review the facility failed to ensure an environment free from h...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to consistently provide translator services in a language ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident #84
On 12/12/23 at 09:39 AM, during an interview, R84 was observed sitting up on the side of their bed. On the right si...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0576
(Tag F0576)
Could have caused harm · This affected 1 resident
This citation pertains to intake #MI00138733
Based on observation, interview, and record review, the facility failed to ensure the resident's right to private and confidential mail delivery for one re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This Deficient practice is linked to intake MI00140318.
Based on interviews and record review, the facility failed to protect th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to implement policies and procedures for ensuring an allegation of neglect/mistreatment was reported to the State Agency in accordance with se...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to complete a thorough investigation of an allegation of neglect/mistreatment for one resident (R62) of one residents reviewed for abuse/negle...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews the facility failed to administer oxygen as ordered by the physician for o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide medically related social services to ensure ac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure a medication error rate less than 5% when two medication errors were observed from a total 25 opportunities, resulting ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
This citation pertains to intake #MI00135446
Based on observation, interview and record review the facility failed to ensure Physician Ordered Occupational Therapy services were provided for one resid...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R62
On 12/12/23 at approximately 10:46 a.m., R62 was observed in their room, laying in their bed. R62 was queried if the facilit...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident #42
On 12/12/23 at 9:03 AM, during an interview with R42, when asked about how the meals were at the facility, R42 expr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to protect Protected Health Information (PHI) for four (R4...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R86
On 12/12/23 at 9:47 AM, R86 complained their screen to their window was broken and had been for quite some time. It was obse...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** On 12/12/23 at approximately 9:04 a.m., a cart containing creams/wound treatments next to room [ROOM NUMBER] was observed to be ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
On 12/12/23 at 02:35 PM, During an initial environmental tour of the facility activity room, this surveyor observed an empty, moderate sized commercial popcorn machine. The stand was noted with a red ...
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on interview and record review the facility failed to ensure the daily nurse staff postings were updated daily and reflected the staffing at the facility potentially affecting all residents and ...
Read full inspector narrative →
Oct 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake: MI00139857.
Based on observation, interviews, and record reviews the facility failed to ensur...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0776
(Tag F0776)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake: MI00139857.
Based on interviews and record reviews the facility failed to timely complete a S...
Read full inspector narrative →
Jan 2023
7 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to Intake Number: MI00131453.
Based on interviews and record review, the facility failed to protect one (...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R355
Review of a Facility Reported Incident (FRI) dated 11/24/22 read in part, Apparently after therapy Friday afternoon until s...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to Intake Number: MI00132915.
Based on observation, interview, and record review the facility failed to m...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake #MI00131690, MI00131693, and MI00131853.
Based on interview and record review, the facility fai...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide timely occupational therapy (OT) services as o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure that residents were able to exercise their right to vote in the November 2022 midterm election resulting in feelings of frustration....
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure COVID-19 testing for both Staff and Residents was conducted f...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 5 harm violation(s), $145,315 in fines, Payment denial on record. Review inspection reports carefully.
- • 49 deficiencies on record, including 5 serious (caused harm) violations. Ask about corrective actions taken.
- • $145,315 in fines. Extremely high, among the most fined facilities in Michigan. Major compliance failures.
- • Grade F (10/100). Below average facility with significant concerns.
About This Facility
What is Marvin & Betty Danto Health Care Center's CMS Rating?
CMS assigns Marvin & Betty Danto Health Care Center an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Michigan, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Marvin & Betty Danto Health Care Center Staffed?
CMS rates Marvin & Betty Danto Health Care Center's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 53%, compared to the Michigan average of 46%.
What Have Inspectors Found at Marvin & Betty Danto Health Care Center?
State health inspectors documented 49 deficiencies at Marvin & Betty Danto Health Care Center during 2023 to 2025. These included: 5 that caused actual resident harm, 43 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Marvin & Betty Danto Health Care Center?
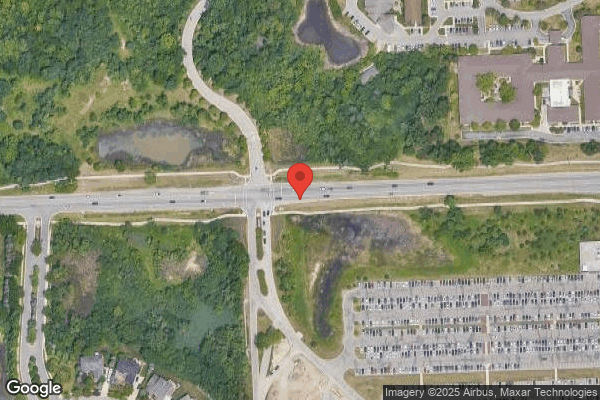
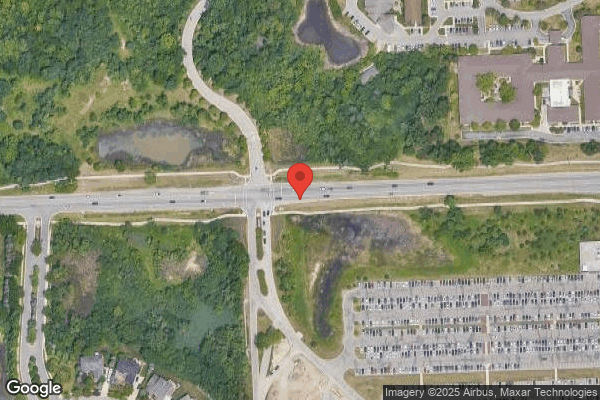
Marvin & Betty Danto Health Care Center is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PREFERRED CARE, a chain that manages multiple nursing homes. With 155 certified beds and approximately 119 residents (about 77% occupancy), it is a mid-sized facility located in West Bloomfield, Michigan.
How Does Marvin & Betty Danto Health Care Center Compare to Other Michigan Nursing Homes?
Compared to the 100 nursing homes in Michigan, Marvin & Betty Danto Health Care Center's overall rating (2 stars) is below the state average of 3.1, staff turnover (53%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Marvin & Betty Danto Health Care Center?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Marvin & Betty Danto Health Care Center Safe?
Based on CMS inspection data, Marvin & Betty Danto Health Care Center has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Michigan. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Marvin & Betty Danto Health Care Center Stick Around?
Marvin & Betty Danto Health Care Center has a staff turnover rate of 53%, which is 7 percentage points above the Michigan average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Marvin & Betty Danto Health Care Center Ever Fined?
Marvin & Betty Danto Health Care Center has been fined $145,315 across 2 penalty actions. This is 4.2x the Michigan average of $34,532. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Marvin & Betty Danto Health Care Center on Any Federal Watch List?
Marvin & Betty Danto Health Care Center is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.