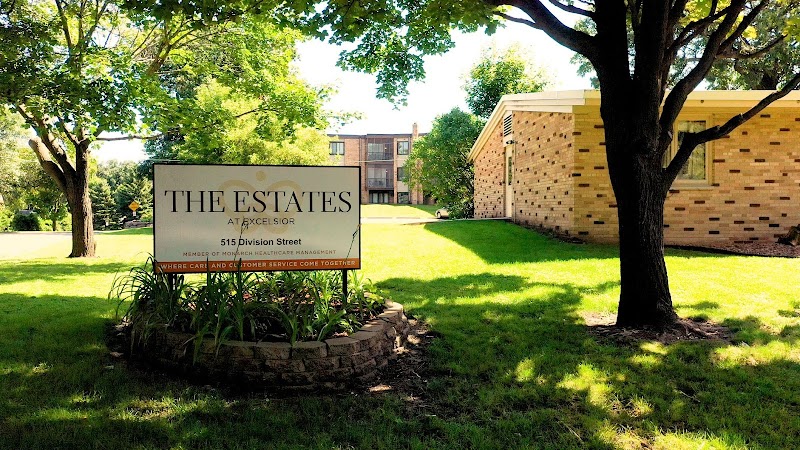
The Estates at Excelsior LLC



Inspected within the last 6 months. Data reflects current conditions.
The Estates at Excelsior LLC has received a Trust Grade of F, indicating significant concerns about the facility's overall quality and care. It ranks #328 out of 337 nursing homes in Minnesota, placing it in the bottom half of all facilities, and #52 out of 53 in Hennepin County, suggesting limited local options for better care. The facility's situation is worsening, with reported issues increasing from 7 in 2024 to 23 in 2025. Staffing is a relative strength, receiving a 4/5 star rating, but with a concerning turnover rate of 56%, which is higher than the state average. There have been no fines reported, which is a positive sign, and the facility offers more RN coverage than 94% of Minnesota facilities, ensuring critical oversight for patient care. However, recent inspections revealed some serious issues, such as residents not being offered snacks during long intervals between meals, and staff observed eating in food preparation areas, raising concerns about infection control practices. Additionally, there were lapses in the facility's quality assurance processes, with no clear action plans in place to address identified issues, which could potentially impact resident care.
- Trust Score
- F
- In Minnesota
- #328/337
- Safety Record
- Low Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 56% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Minnesota facilities.
- Skilled Nurses ✓ Good
- Each resident gets 77 minutes of Registered Nurse (RN) attention daily — more than 97% of Minnesota nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 43 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, fire safety.
The Bad
Below Minnesota average (3.2)
Significant quality concerns identified by CMS
10pts above Minnesota avg (46%)
Frequent staff changes - ask about care continuity
Part of a multi-facility chain
Ask about local staffing decisions and management
8 points above Minnesota average of 48%
The Ugly 43 deficiencies on record
Jun 2025
21 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on interview and document review the facility failed to ensure Notice of Medicare Non- Coverage (NOMNC) and Advanced Beneficiary Notice (ABN) was given to the resident's representative for signa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
R18's 4/9/25, quarterly Minimum Data Set (MDS) assessment identified R18's cognition was intact, R18 was dependent on staff for transfers and R18 attended dialysis.
R18's care plan identified R18 had...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0605
(Tag F0605)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R7
R7's 3/26/25, quarterly Minimum Data Set (MDS) identified his cognition was intact, he felt down and depressed 2-6 days weekl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on interview and document review, the facility failed to complete a 48 hour baseline care plan upon admission for 1 of 10 residents (R187) reviewed.
Findings include:
R187's 6/5/25, admission M...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
The facility failed to develop and implement a comprehensive person-centered care plan for 1 of 2 sampled residents (R5) that addressed anticoagulant (prevents and breaks down blood clots) therapy wit...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and document review, the facility failed to revise the care plan to reflect current care needs for 2 of 13 sampled residents (R2 and R18) reviewed.
Findings include:
R2's 3/27/25, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview and document review, the facility failed to identify appropriate turning and repositioning schedule based off professional standards of practice and document when staff...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review the facility failed to provide a prescribed therapeutic diet to 1 of 1 resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review, the facility failed to implement their dialysis contract and arrange for transportation ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interview and document review, the facility failed to ensure supply and administration of ordered medications for 1 of 1 resident (R24) reviewed for pharmacy services.
Findings include:
R24...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on observation, interview, and document review the facility failed to offer an alternative food item for 1 of 1 residents (R187).
Findings include:
Observation on 6/11/25 at 8:02 a.m., of nursi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on interview and document review, the facility failed to complete a comprehensive assessment for continued use of antibiotics for 2 of 3 (R24 and R238) sampled residents reviewed for antibiotic ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review, the facility failed to ensure 1 of 5 (R5) were offered and/or provided updated vaccinati...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on observation, interview, and document review, the facility failed to act promptly and provide resolution for resident concerns related to the dietary department failure to post upcoming menus....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0628
(Tag F0628)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R27's 4/24/25, 14-day admission assessment, MDS identified her cognition was intact, and she required supervision to moderate as...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
Based on observation, interview, and document review, the facility failed to provide for Activities of Daily Living (ADL) related to assisting with toileting, turning and repositioning, queuing for fo...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected most or all residents
Based on observation, interview, and document review, the facility failed to offer a snack to residents on a routine basis when meals were greater than 14 hours apart. This had the potential to affect...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to ensure infection control practices were maintained in the kitchen when 1 of 1 staff were observed eating in the facility food preparation are...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
Based on interview and document review, the facility failed to ensure data submitted to the Quality Assurance and Performance Improvement (QAPI) committee was analyzed and documented to ensure areas i...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on interview and document review, the facility failed to have evidence of a goal, an action plan, and analysis of data brought forth for the identified Performance Improvement Projects (PIP). Th...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on interview and document review, the facility failed to ensure employee illnesses were tracked to identify when employee would be able to return to work after an illness, dependent upon their s...
Read full inspector narrative →
Jan 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review, the facility failed to implement the use of an air pressure redistribution mattress to a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and document review, the facility failed to implement appropriate personal protective equipment (PPE) to prevent the spread of infection for 1 of 1 residents (R2) obse...
Read full inspector narrative →
Nov 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review, the facility failed to provide timely notification for change in condition to the physic...
Read full inspector narrative →
May 2024
5 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide a written notification/copy of a bed hold for 2 of 2 (R1, R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review, the facility failed to ensure 1 of 5 resident (R5) were offered or received pneumococcal...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and document review, the facility failed to ensure insulin pens were appropriately labeled according to manufacturer's guidelines with an opened date in 1 of 2 medicat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R15's face sheet dated 5/16/24, identified diagnoses including diabetes mellitus (DM), lymphedema (swelling of the legs related ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on interview and document review, the facility failed to ensure the Quality Assurance Process Improvement (QAPI) committee was effective in maintaining appropriate action plans to correct a qual...
Read full inspector narrative →
Apr 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review, the facility failed to ensure an allegation of staff to resident abuse was reported imme...
Read full inspector narrative →
Aug 2023
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, observation and document review, the facility failed to ensure timely resolution of missing personal propert...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0553
(Tag F0553)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and documents review, the facility did not ensure participation in care planning for 1 of 5 residents (R1) w...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, observation and document review, the facility failed to ensure resident call device was within reach and res...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review the facility failed to administer dietary supplements recommenced for 1 of 1 (R1) who was...
Read full inspector narrative →
Jun 2023
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to assess and determine safety for self-administration...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure food preferences of the resident were honore...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review the facility failed to ensure resident floors and equipment were clean for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R184's nursing progress notes dated 5/22/23 indicated R184 was admitted and alert and oriented.
R184's Medical Diagnosis form in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interview, and document review, the facility failed to provide a therapeutic diet as prescribed for 1 of 2 residents (R184) reviewed who had an altered diet.
Findings include:
R...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and document review, the facility failed to ensure hand hygiene was completed during nursing car...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0826
(Tag F0826)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R183
R183's hospital discharge orders dated 4/13/23, indicated R183 had a fall while standing. The orders identified physical th...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
Based on interview and document review, the facility failed to conduct ongoing quality assurance and performance improvement (QAPI) activities and develop and implement action plans to correct quality...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0801
(Tag F0801)
Minor procedural issue · This affected most or all residents
Based on observation, interview, and document review, the facility failed to designate a qualified person to serve as the director of food and nutrition services in the absence of a full-time dietitia...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • No fines on record. Clean compliance history, better than most Minnesota facilities.
- • 43 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • Grade F (35/100). Below average facility with significant concerns.
- • 56% turnover. Above average. Higher turnover means staff may not know residents' routines.
About This Facility
What is The Estates At Excelsior Llc's CMS Rating?
CMS assigns The Estates at Excelsior LLC an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Minnesota, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is The Estates At Excelsior Llc Staffed?
CMS rates The Estates at Excelsior LLC's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 56%, which is 10 percentage points above the Minnesota average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at The Estates At Excelsior Llc?
State health inspectors documented 43 deficiencies at The Estates at Excelsior LLC during 2023 to 2025. These included: 42 with potential for harm and 1 minor or isolated issues.
Who Owns and Operates The Estates At Excelsior Llc?
The Estates at Excelsior LLC is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by MONARCH HEALTHCARE MANAGEMENT, a chain that manages multiple nursing homes. With 45 certified beds and approximately 31 residents (about 69% occupancy), it is a smaller facility located in EXCELSIOR, Minnesota.
How Does The Estates At Excelsior Llc Compare to Other Minnesota Nursing Homes?
Compared to the 100 nursing homes in Minnesota, The Estates at Excelsior LLC's overall rating (1 stars) is below the state average of 3.2, staff turnover (56%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting The Estates At Excelsior Llc?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's high staff turnover rate.
Is The Estates At Excelsior Llc Safe?
Based on CMS inspection data, The Estates at Excelsior LLC has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Minnesota. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at The Estates At Excelsior Llc Stick Around?
Staff turnover at The Estates at Excelsior LLC is high. At 56%, the facility is 10 percentage points above the Minnesota average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was The Estates At Excelsior Llc Ever Fined?
The Estates at Excelsior LLC has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is The Estates At Excelsior Llc on Any Federal Watch List?
The Estates at Excelsior LLC is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.