THE VILLAS AT THE PARK




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
The Villas at the Park has a Trust Grade of D, which indicates below-average performance and some concerning issues. They rank #206 out of 337 facilities in Minnesota, placing them in the bottom half of the state, and #32 out of 53 in Hennepin County, meaning only one local option is better. The facility is showing signs of improvement, reducing issues from 26 in 2023 to 8 in 2024. Staffing is a concern with a turnover rate of 55%, significantly higher than the state average of 42%, but they have average RN coverage. However, they face significant fines totaling $105,301, which is higher than 97% of Minnesota facilities, indicating repeated compliance problems. Specific incidents include a serious issue where medications were not administered according to physician orders for several residents, raising potential safety concerns, and a failure to maintain proper refrigeration temperatures, which could lead to foodborne illnesses. While there are some positive trends, families should be aware of the serious and concerning issues present at this facility.
- Trust Score
- D
- In Minnesota
- #206/337
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 55% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $105,301 in fines. Lower than most Minnesota facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 44 minutes of Registered Nurse (RN) attention daily — more than average for Minnesota. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 34 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Near Minnesota average (3.2)
Meets federal standards, typical of most facilities
Near Minnesota avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 34 deficiencies on record
Oct 2024
8 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The State Operations Manual (SOM) defined the various presure ulcers as follows:
A stage one pressure injury is intact skin with...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure a self administration assessment (SAM) and a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure freedom of movement was not restricted when ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R45's quarterly Minimum Data Set (MDS) dated [DATE], indicated R45 was cognitively intact and had diagnoses of chronic venous in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure an occupational therapy (OT) ordered hand sp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to implement fall interventions for 1 of 2 residents (...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure staff utilized enhanced barrier precautions ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to conduct regular inspections of hospital bed rails a...
Read full inspector narrative →
Nov 2023
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure 1 of 1 residents (R3) were comprehensively a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Findings include:
R35's Face Sheet form, printed 11/7/23, indicated R35 had diagnoses that includes metabolic encephalopathy, in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to schedule a follow-up gastrointestinal procedure for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed implement care planned fall interventions, perform a c...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview and document review, the facility failed to ensure stock medications (i.e., medication used for multiple patients) were tracked and re-ordered timely to prevent disrupt...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R4
R4's quarterly Minimum Data Set (MDS) assessment dated [DATE], indicated R4 was cognitively intact, had diagnoses of depressi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observation, interview, and document review, the facility failed to ensure a fast-acting insulin Flexpen and newly attached needle was primed and administered in accordance with manufacturer ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R3's quarterly Minimum Data Set (MDS), dated [DATE], indicated R3 was cognitively intact, was independent with toileting, occasi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R24's quarterly minimum data set (MDS) dated [DATE], identified R24 with intact cognition, a need for extensive assistance with ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0808
(Tag F0808)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure a therapeutic diet of thickened liquids was ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview and document review, the facility failed to ensure medications were administered in accordance with physician orders and manufacturer guidelines for 3 of 6 residents (R...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
HAND HYGIENE:
During continuous observation of personal cares on 11/8/23, at 7:20 a.m., nursing assistant (NA)-C and NA-D walked into R246's room. Without performing hand hygiene, NA-C and NA-D donne...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Room Equipment
(Tag F0908)
Minor procedural issue · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** During observation, interview and document review, the facility failed to assure that the kitchen dishwasher was maintained per ...
Read full inspector narrative →
May 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review, the facility failed to ensure a baseline care plan was developed within 48 hours of admi...
Read full inspector narrative →
Jan 2023
12 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to monitor blood pressures as ordered for 1 of 1 resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** During observation, interview, and document review, the facility failed to ensure repositioning was completed for 1 of 1 residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure an ordered hand brace was care planned and c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review, the facility failed to implement fall interventions to reduce the risk of falls for 1 of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on document review and interview the facility failed to identify triggers to avoid potential re-traumatization and failed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review the facility failed to ensure grab bars were assessed to determine appropri...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to review and revise behavioral health care plans and int...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review, the facility failed to ensure orders for an as needed (PRN) psychotropic medication (med...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview and document review, the facility failed to ensure medications were administered in accordance with physician orders without errors for 1 of 3 residents (R149) observed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview the facility failed to maintain a sanitary environment for 1 of 1 (R33) residents reviewed fo...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review, the facility failed to ensure pharmaceutical services were available and dispensed medic...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and document review the facility failed to maintain appropriate temperature in a refrigerator used for cold food storage to prevent potential food borne illness for al...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 harm violation(s), $105,301 in fines. Review inspection reports carefully.
- • 34 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $105,301 in fines. Extremely high, among the most fined facilities in Minnesota. Major compliance failures.
- • Grade D (40/100). Below average facility with significant concerns.
About This Facility
What is The Villas At The Park's CMS Rating?
CMS assigns THE VILLAS AT THE PARK an overall rating of 3 out of 5 stars, which is considered average nationally. Within Minnesota, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is The Villas At The Park Staffed?
CMS rates THE VILLAS AT THE PARK's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 55%, compared to the Minnesota average of 46%.
What Have Inspectors Found at The Villas At The Park?
State health inspectors documented 34 deficiencies at THE VILLAS AT THE PARK during 2023 to 2024. These included: 1 that caused actual resident harm, 32 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
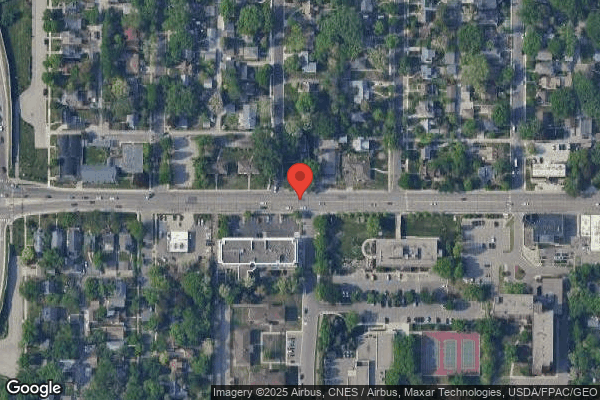
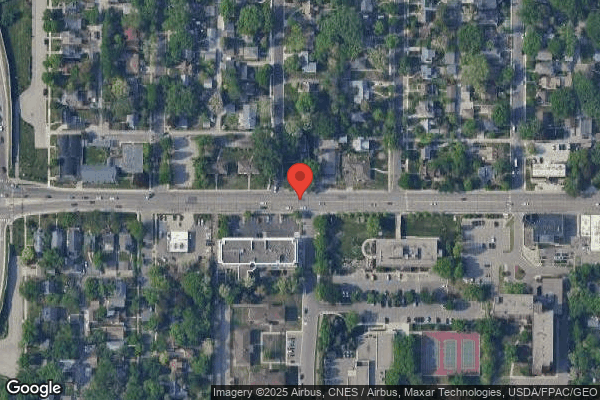
Who Owns and Operates The Villas At The Park?
THE VILLAS AT THE PARK is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by MONARCH HEALTHCARE MANAGEMENT, a chain that manages multiple nursing homes. With 52 certified beds and approximately 48 residents (about 92% occupancy), it is a smaller facility located in SAINT LOUIS PARK, Minnesota.
How Does The Villas At The Park Compare to Other Minnesota Nursing Homes?
Compared to the 100 nursing homes in Minnesota, THE VILLAS AT THE PARK's overall rating (3 stars) is below the state average of 3.2, staff turnover (55%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting The Villas At The Park?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is The Villas At The Park Safe?
Based on CMS inspection data, THE VILLAS AT THE PARK has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in Minnesota. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at The Villas At The Park Stick Around?
THE VILLAS AT THE PARK has a staff turnover rate of 55%, which is 9 percentage points above the Minnesota average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was The Villas At The Park Ever Fined?
THE VILLAS AT THE PARK has been fined $105,301 across 19 penalty actions. This is 3.1x the Minnesota average of $34,132. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is The Villas At The Park on Any Federal Watch List?
THE VILLAS AT THE PARK is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.