Shirley Chapman Sholom Home East
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
The Shirley Chapman Sholom Home East has a Trust Grade of C, indicating that it is average compared to other facilities. It ranks #147 out of 337 in Minnesota, placing it in the top half of nursing homes in the state, and #7 out of 27 in Ramsey County, meaning only six local options are better. The facility's performance has been stable, with a consistent number of issues (9) reported in both 2024 and 2025. Staffing is a strong point, rated 5 out of 5 stars with a turnover rate of 30%, which is significantly lower than the state average, suggesting experienced staff who know the residents well. However, there are several concerns, including a critical incident where a resident was not resuscitated according to their wishes due to conflicting information in their medical records, and failures to post required nurse staffing information, which could affect residents and their families. While the home has good staffing levels and a decent overall rating, these issues raise important questions about the quality of care and communication at the facility.
- Trust Score
- C
- In Minnesota
- #147/337
- Safety Record
- High Risk
- Inspections
- Holding Steady
- Staff Stability ✓ Good
- 30% annual turnover. Excellent stability, 18 points below Minnesota's 48% average. Staff who stay learn residents' needs.
- Penalties ○ Average
- $13,039 in fines. Higher than 50% of Minnesota facilities. Some compliance issues.
- Skilled Nurses ✓ Good
- Each resident gets 85 minutes of Registered Nurse (RN) attention daily — more than 97% of Minnesota nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 26 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Staffing Rating · Excellent nurse staffing levels
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Low Staff Turnover (30%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (30%)
18 points below Minnesota average of 48%
Facility shows strength in staffing levels, quality measures, staff retention, fire safety.
The Bad
Below median ($33,413)
Minor penalties assessed
The Ugly 26 deficiencies on record
Apr 2025
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review, the facility failed to notify the provider of the use of antibiotics concurrent with war...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review the facility failed to ensure a sanitary and homelike environment for 1 of ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and document review, the facility failed to ensure 1 of 1 residents (R61) received treatments an...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and document review, the facility failed to ensure a hand brace and palm protector was used cons...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to fully assess and follow up on weight loss and meal ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review the facility failed to ensure a feeding tube tubing and nutrition bag were ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure respiratory equipment was properly maintained fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and document review the facility failed to ensure the recommended personal protective equipment ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and document review the facility failed to ensure dietary staff was wearing beard guards/restraints when preparing food. This had the potential to affect all 93 reside...
Read full inspector narrative →
Sept 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and document review, the facility failed to review and revise the care plan with current interventions for the care of a new catheter and enhanced barrier precautions (EBP) for 1 of...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and document review, the facility failed to ensure enhanced barrier precautions (EBP) were implemented for 1 of 1 residents (R2) reviewed who had an indwelling cathete...
Read full inspector narrative →
Jun 2024
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure a self-administration of medications (SAM) a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to notify a provider for a significant weight gain for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure grooming was offered and or provided for 2 o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to provide assistance to ensure eyeglasses were availa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and document review, the facility failed to ensure breakfast was provided to a resident prior to dialysis an...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure food was properly stored, labeled, and dated...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** LINEN
During observation on 6/10/24 at 12:00 p.m., an uncovered linen cart was located midway down the [NAME] wing. A variety of...
Read full inspector narrative →
Mar 2023
8 deficiencies
1 IJ (1 affecting multiple)
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0578
(Tag F0578)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R349's admission Minimum Data Set (MDS), dated [DATE], indicated R349 was cognitively intact.
R349's provider order, dated [DAT...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure self-administration of medication (SAM) was ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R86's MDS, dated [DATE], indicated R86 had severe cognitive impairment and was diagnosed with Alzheimer's disease, dysphagia (di...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review, the facility failed to develop and implement an effective discharge planning process whi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0810
(Tag F0810)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to provide adaptive equipment to promote independence ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and document review, the facility failed to ensure current standards of practice for catheter c...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected most or all residents
Based on observation, interview, and document review, the facility failed to ensure the required nurse staff information was posted daily. This had the potential to affect all of the 94 residents resi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review the facility failed to ensure the Quality Assessment and Assurance (QAA)/Quality Assuranc...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 30% annual turnover. Excellent stability, 18 points below Minnesota's 48% average. Staff who stay learn residents' needs.
- • Multiple safety concerns identified: 1 life-threatening violation(s). Review inspection reports carefully.
- • 26 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $13,039 in fines. Above average for Minnesota. Some compliance problems on record.
- • Grade C (59/100). Below average facility with significant concerns.
About This Facility
What is Shirley Chapman Sholom Home East's CMS Rating?
CMS assigns Shirley Chapman Sholom Home East an overall rating of 4 out of 5 stars, which is considered above average nationally. Within Minnesota, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Shirley Chapman Sholom Home East Staffed?
CMS rates Shirley Chapman Sholom Home East's staffing level at 5 out of 5 stars, which is much above average compared to other nursing homes. Staff turnover is 30%, compared to the Minnesota average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Shirley Chapman Sholom Home East?
State health inspectors documented 26 deficiencies at Shirley Chapman Sholom Home East during 2023 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 25 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Shirley Chapman Sholom Home East?
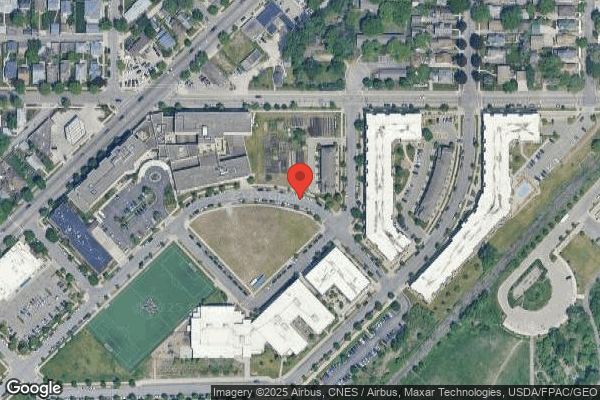
Shirley Chapman Sholom Home East is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 118 certified beds and approximately 86 residents (about 73% occupancy), it is a mid-sized facility located in SAINT PAUL, Minnesota.
How Does Shirley Chapman Sholom Home East Compare to Other Minnesota Nursing Homes?
Compared to the 100 nursing homes in Minnesota, Shirley Chapman Sholom Home East's overall rating (4 stars) is above the state average of 3.2, staff turnover (30%) is significantly lower than the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Shirley Chapman Sholom Home East?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Shirley Chapman Sholom Home East Safe?
Based on CMS inspection data, Shirley Chapman Sholom Home East has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 4-star overall rating and ranks #1 of 100 nursing homes in Minnesota. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Shirley Chapman Sholom Home East Stick Around?
Staff at Shirley Chapman Sholom Home East tend to stick around. With a turnover rate of 30%, the facility is 16 percentage points below the Minnesota average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly.
Was Shirley Chapman Sholom Home East Ever Fined?
Shirley Chapman Sholom Home East has been fined $13,039 across 1 penalty action. This is below the Minnesota average of $33,209. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Shirley Chapman Sholom Home East on Any Federal Watch List?
Shirley Chapman Sholom Home East is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.