PARK PLACE TRANSITIONAL CARE AND REHABILITATION



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Park Place Transitional Care and Rehabilitation has a Trust Grade of F, indicating significant concerns and a poor reputation among nursing homes. It ranks #33 out of 59 facilities in Montana, placing it in the bottom half, but is #2 out of 4 in Cascade County, meaning only one local option is better. The facility is showing an improving trend, with the number of issues decreasing from 11 in 2024 to 8 in 2025. Staffing is a relative strength, receiving a rating of 4 out of 5 stars with a turnover rate of 32%, which is well below the state average. However, the facility has incurred $208,117 in fines, which is higher than 78% of facilities in Montana, indicating ongoing compliance issues. While there are some strengths, there are also serious weaknesses. For example, residents have developed serious pressure ulcers due to inadequate monitoring and care. One resident who was admitted without any pressure ulcers developed a Stage IV ulcer, showing a failure to identify and address the issue promptly. Additionally, there was a failure to catch a significant weight loss in another resident, which could lead to serious health complications. Families should weigh these strengths and weaknesses carefully when considering this facility.
- Trust Score
- F
- In Montana
- #33/59
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 32% turnover. Near Montana's 48% average. Typical for the industry.
- Penalties ✓ Good
- $208,117 in fines. Lower than most Montana facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 47 minutes of Registered Nurse (RN) attention daily — more than average for Montana. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 41 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (32%)
16 points below Montana average of 48%
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Near Montana average (3.0)
Meets federal standards, typical of most facilities
13pts below Montana avg (46%)
Typical for the industry
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 41 deficiencies on record
Apr 2025
8 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a resident admitted without a pressure ulcer did not develop a pressure ulcer for 1 (#10) of 2 sampled residents with ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to assist a resident with obtaining clothing that fit, and change the clothing she had regularly, are attempt to obtain clothes ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure residents received proper treatment, services, and assistive devices to maintain optimal visual abilities for 1 (#42) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to address an indwelling catheter upon admission for dis...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide behavioral health services for 1 (#391) of 1 ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation and interviews, the facility failed to provide a home like setting and correct and control odors emanating on the 400B hallway, for 2 (#s 114 and 130) of 39 sampled residents. Thi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure safe and effective blood-draw practices were u...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to properly store, label, date, and discard food items by the use by date, in the backroom cooler in the kitchen; and failed to ...
Read full inspector narrative →
Nov 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to identify a resident's elopement risk and update the care plan with interventions to prevent elopement for 1 (#16) of 4 residents sampled fo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to identify a resident's elopement risk, implement effective interventions to prevent elopement, and failed to follow facility policy, for 2 (...
Read full inspector narrative →
Apr 2024
4 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to identify a discrepancy in weight recordings which wou...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to continuously assess and document on a penile ulcer that was progres...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident was free from a medication error ommission, for 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility staff failed to use standard precautions while doing laundry, resulting in the potential for cross contamination, which could negativel...
Read full inspector narrative →
Mar 2024
5 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide dignity and respect to 1 (#1) of 4 sampled residents. This deficient practice caused the resident to feel embarrassed...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to complete a thorough investigation to include root cause analysis for a fall with injury for 1(#9) of 3 sampled residents. Thi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to complete an accurate MDS assessment in the area of bowel and bladder in accordance with the RAI requirements for 1 (#1) of 4 ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement a baseline care plan, outlining pertinent information needed to care for a new resident within 48 hours of admissio...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to complete a comprehensive, person-centered care plan for 1 (#1) of 4 sampled residents. This deficient practice did not addres...
Read full inspector narrative →
Dec 2023
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, facility staff neglected to assess and monitor a new admission, and ensure antibiotic medi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to report an incident of neglect of care for 1 (#2) of 1 sampled resident. This neglect increased the risk for the resident to deteriorate wit...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0635
(Tag F0635)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to have a system in place to ensure new admissions had complete and accurate transcription of physician admission orders for 1 (#2) of 1 sampl...
Read full inspector narrative →
Oct 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to identify signs and symptoms of infection which led to septic shock ...
Read full inspector narrative →
Apr 2023
18 deficiencies
2 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Notification of Changes
(Tag F0580)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to identify, follow up, and notify the physician when 1 (#195) admitte...
Read full inspector narrative →
SERIOUS
(H)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected multiple residents
2. During interviews on 4/24/23 at 2:50 p.m., resident #194 and NF6 were in resident #194's room. NF6 stated resident #194 was unable to sit in his recliner due to the pain from his buttocks. NF6 stat...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to send a reimbursement check to 1 (#185) of 1 sampled resident, within the 30-day required window. Findings include:
During an interview on 4...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide notification of Notice of Transfer for 1 (#187) of 1 sample...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide the resident or family with a written notice which specifie...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to identify pressure ulcers for 1 (#74) of 5 sampled residents upon hi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, facility staff failed to identify a significant change in a resident's of ADL status, hearing, and weight loss for 1 (#26) of 4 sampled residents. T...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to develop and implement a person-centered baseline care plan for 1 (#194) of 4 sampled residents. Findings include:
During an i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to develop and implement a comprehensive care plan for a resident who preferred to maintain and use cooking and food supplies ke...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, facility staff failed to revise a care plan for a resident with hearing deficits, for 1 (#26) of 4 sampled residents. This failure could negatively ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, facility staff failed to identify a potentially hazardous outcome related to the use of an emersion heater, and the use of multiple electrical power...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facilty failed to ensure residents who received dialysis were provided services, consistent with professional standards of practice, including p...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to provide respiratory care services, including CPAP supplies for 1 (#5)...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facilty failed to provide sufficient nursing staff with the appropriate ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, facility staff failed to ensure 3 (#s 26, 68, and 75) of 5 sampled residents were free fro...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure staff had completed the required annual training with competencies, and failed to keep records of the staff training. Findings inclu...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to provide the services of a registered nurse for at least 8 consecutive hours a day, seven days a week. This deficiency has the...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to maintain a water management program to minimize the growth and spread of waterborne pathogens. This deficient practice had the potential to...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 32% turnover. Below Montana's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 6 harm violation(s), $208,117 in fines. Review inspection reports carefully.
- • 41 deficiencies on record, including 6 serious (caused harm) violations. Ask about corrective actions taken.
- • $208,117 in fines. Extremely high, among the most fined facilities in Montana. Major compliance failures.
- • Grade F (15/100). Below average facility with significant concerns.
About This Facility
What is Park Place Transitional Care And Rehabilitation's CMS Rating?
CMS assigns PARK PLACE TRANSITIONAL CARE AND REHABILITATION an overall rating of 3 out of 5 stars, which is considered average nationally. Within Montana, this rating places the facility higher than 99% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Park Place Transitional Care And Rehabilitation Staffed?
CMS rates PARK PLACE TRANSITIONAL CARE AND REHABILITATION's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 32%, compared to the Montana average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Park Place Transitional Care And Rehabilitation?
State health inspectors documented 41 deficiencies at PARK PLACE TRANSITIONAL CARE AND REHABILITATION during 2023 to 2025. These included: 6 that caused actual resident harm and 35 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Park Place Transitional Care And Rehabilitation?
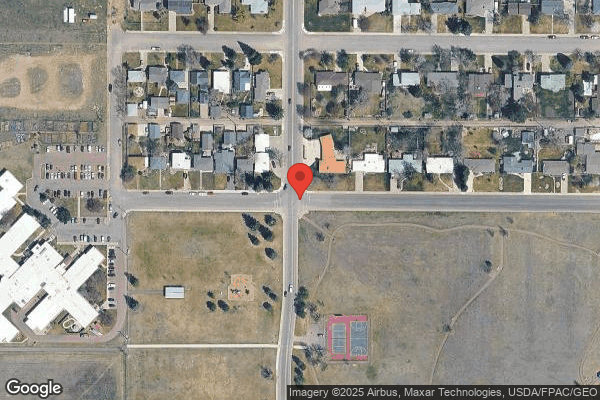
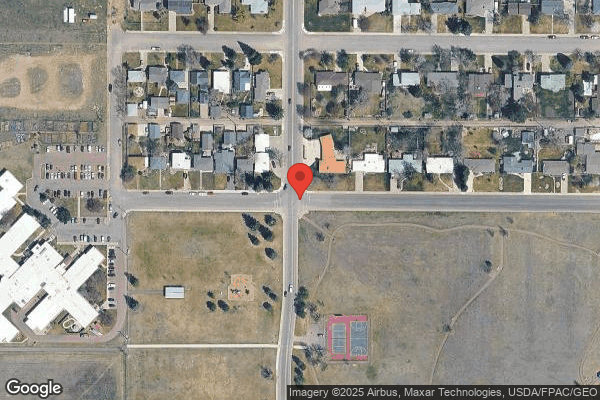
PARK PLACE TRANSITIONAL CARE AND REHABILITATION is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by SWEETWATER CARE, a chain that manages multiple nursing homes. With 189 certified beds and approximately 141 residents (about 75% occupancy), it is a mid-sized facility located in GREAT FALLS, Montana.
How Does Park Place Transitional Care And Rehabilitation Compare to Other Montana Nursing Homes?
Compared to the 100 nursing homes in Montana, PARK PLACE TRANSITIONAL CARE AND REHABILITATION's overall rating (3 stars) is above the state average of 3.0, staff turnover (32%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Park Place Transitional Care And Rehabilitation?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Park Place Transitional Care And Rehabilitation Safe?
Based on CMS inspection data, PARK PLACE TRANSITIONAL CARE AND REHABILITATION has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in Montana. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Park Place Transitional Care And Rehabilitation Stick Around?
PARK PLACE TRANSITIONAL CARE AND REHABILITATION has a staff turnover rate of 32%, which is about average for Montana nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Park Place Transitional Care And Rehabilitation Ever Fined?
PARK PLACE TRANSITIONAL CARE AND REHABILITATION has been fined $208,117 across 5 penalty actions. This is 5.9x the Montana average of $35,160. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Park Place Transitional Care And Rehabilitation on Any Federal Watch List?
PARK PLACE TRANSITIONAL CARE AND REHABILITATION is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.