CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews conducted during a recertification survey the facility did not ensure that ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews conducted during a recertification survey the facility did not ensure that based on the comprehensive assessment and care plan and the preferences of each resident, an ongoing program to support residents in their choice of activities, both facility-sponsored group and individual activities and independent activities, designed to meet the interests of and support the physical, mental, and psychosocial well-being of each resident was provided. Specifically, the facility did not ensure that services were provided to a resident who required one to one (1:1) activities. This is evident for 1 of 5 residents reviewed for Activities out of the sample of 38 residents. (Resident #44)
The findings are:
Resident #44 was admitted to the facility with diagnoses that included Unspecified Dementia without behaviors disturbance, and Bipolar disorder, current episodes manic without psychotic features severe.
On 07/08/21 at 01:19 PM, Resident #44 was observed on multiple occasions in a room with no television or radio playing, the room walls were bare and there was no evidence of any stimulation being provided.
On 07/09/21 at 09:28 AM, Resident #44 was observed in bed, mumbling; at 10:29 AM in bed sleeping; at 01:02 PM, 01:50 PM, 02:45 PM, and 03:13 PM the resident was observed in a wheelchair (w/c), in front of the closet visible at the doorway. The resident repeatedly called out both while in the wheel chair when approached, and when alone.
On 07/12/21 at 10:18 AM, Resident #44 was observed in bed; at 11:09 AM the resident was observed in a wheelchair, in front of the closet visible at the doorway while Certified Nursing Assistant (CNA) positioned the wheelchair. The resident was observed yelling out again.
On 07/13/21 at 1:40 PM, resident was observed seated in the wheelchair next to their assigned bed. A television was observed mounted on the wall but was not turned on.
No television was heard playing on multiple previous observations during the survey.
The Annual Minimum Data Set (MDS) dated [DATE] documented the resident had short and long term memory problems. Based on staff assessment the resident's daily and activity preferences included listening to music and participating in religious activities or practices based on staff assessment of daily and activity preferences. The resident was totally dependent on staff for Activities of Daily Living. The MDS also documented the resident displayed verbal behavioral symptoms directed toward others for 4-6 days.
The Quarterly MDS dated [DATE] documented the resident had short and long term memory problems. The resident was totally dependent on staff for Activities of Daily Living. Based on staff assessment the resident had little interest/pleasure in doing things and feeling tired or having little energy for 12-14 days. The MDS also documented the resident displayed physical and verbal behavioral symptoms directed toward others daily and rejection of care for 4-6 days.
The Comprehensive Care Plan (CCP) titled Mood State initiated on 2/22/2018 documented a goal which included the resident will be accepting of nursing home by positive interaction with staff and peers and having improved sleep patterns. The CCP interventions included to encourage family, friends, other residents to visit, maintain regular contact and keep resident in the company of others as much as possible. An update to the CCP on 4/28/21 documented current interventions are appropriate in regards to the resident management. Resident responded therapeutically to all implemented interventions. Resident's plan of care is revised as needed with new interventions to manage change in condition. Goal met, continue POC (plan of care).
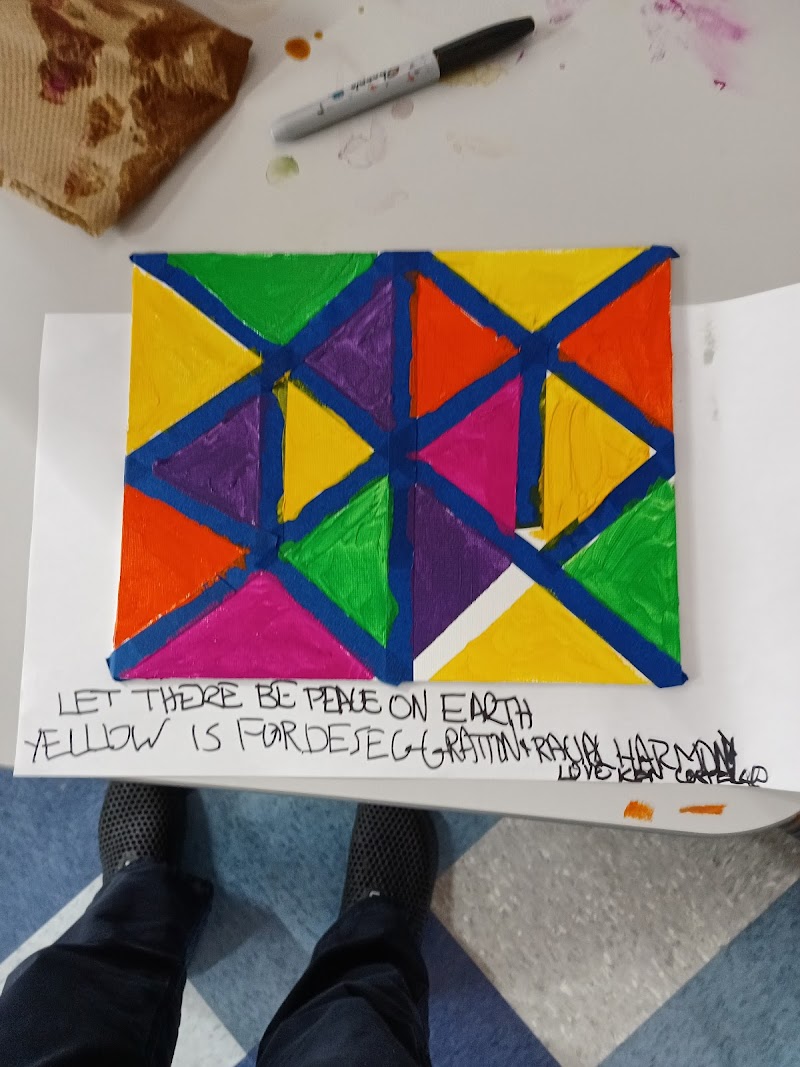
The CCP titled Activities initiated 8/29/2017 documented a goal which included the resident will attend and participate with staff assistance and verbal prompts to increase psychosocial well-being. The resident will be receptive to 1:1 staff interactions during room activities to increase psychosocial well-being, avoid social isolation, and improve mental and sensory awareness (aroma therapy visits, creative art programs - music, ball/toss, parties, religious service) as tolerated. Also, the resident will be receptive to 1:1 program (reality orientation, current events) 1-3 weekly to avoid social isolation and increase sensory stimulation. The CCP interventions included initiate conversations with resident as often as possible, provide 1:1 visits to supplement socialization, provide sensory stimulation during 1:1 interventions, provide 1:1 programs: room bound programs, strolling minstrel, aroma therapy, and holy communion. An update to the CCP on 4/28/2021 documented the resident is responsive with impaired cognition, confusion sometimes, in a happy and good mood other times, yelling and saying bad words for no reason. Enjoys listening to music during 1:1 interaction at bedside with a short attention span.
The Therapeutic Recreation assessment dated [DATE] documented the resident's mental status as confused, oriented to person, judgement impaired, and mobility with w/c. The general activities preferences included music/social; tv/radio; and talking/conversing. All resident needs continue to be anticipated and met by staff. Level of participation is a passive observer, receptive to visits, enjoys listening to music, enjoys animals, and enjoys spending time outdoors. Present activity preferences/programs attended in last 3 months were exercise/sports, music, visits, sensory stimulation, movies, radio/tv, strolling minstrel, pet visit, special events. Resident continues to receive room bound 1:1 social activity visit with therapeutic music/touch and reality orientation with current events and newspaper read during interaction. The plan of care (POC) included resident will continue to respond to during 1:1 interaction, room bound social, therapeutic music/sensory visits. Interventions documented included will continue to provide 1:1 social visits during interaction at bedside with reality orientation and verbal cues to encourage participation in social activity of choice. Resident has impaired cognition which has an impact on recreational involvement and requires constant redirection.
The Therapeutic Recreation assessment dated [DATE] included the resident has poor response during room bound 1:1 social interaction with therapeutic music/touch and reality orientation.
Nursing note dated 4/30/2021 documented the resident is responsive to verbal and tactile stimulation, oriented to name, and unable to hold a conversation. Diagnosis is Mood Disorder and Anxiety. The resident is visually impaired, and seldom watches TV. The resident screams loudly for no apparent reason when providing care, at mealtime and when medicated. The resident also uses profanity and racial remarks.
Nursing behavior note dated 5/04/2021, 5/27/2021, 6/7/2021, 6/27/2021 documented Resident #44 have no interest in doing things, oriented to name, unable to make his needs known, confused, noisy and resistive during care nearly every day. Resident #44 has trouble concentrating on things, such as reading newspaper/watching tv almost daily. Resident was noted with disruptive sounds and yelling for no apparent reasons daily.
There was no recent documented evidence of recreational activities that had been provided to the resident.
On 07/13/21 at 09:21 AM, an interview was conducted with Certified Nursing Aide (CNA) #4. CNA #4 stated the resident is very aggressive, fights, screams, calls negative names, will spit out food in the aide's face, kicks, pushes aide away during meals and ADL care. CNA #4 also stated the resident is not really involved in activities, as they would not comply and make a lot of noise during the activities. CNA #4 further stated they were not sure if one to one basis activities were provided to the resident. CNA #4 stated the resident will pull and throw anything within reach including table, television, radio, sheets, and pillow.
On 07/13/21 at 09:35 AM, an interview was conducted with Licensed Practical Nurse (LPN)#3. LPN #3 stated the resident screams and yells racial slurs as you step in the room and tells the nurse to leave the room. LPN #3 also stated the resident may try to grab/scratch the CNA and is a little resistive during care. LPN #3 further stated the resident is provided one to one activities and he does not interact with other residents. LPN #3 stated recreation is provided three times a week for the resident. The LPN #3 stated the yelling disturbs the other residents during group activities.
On 07/13/21 at 10:13 AM, an interview was conducted with a Senior Recreational Aide (SRA) who stated the resident receives therapy 2-3 times a week for 10-15 minutes. The SRA also stated that currently they are also providing coverage on units 2-6 based on the activity for the day. The SRA stated therapeutic music, tv, sensory stimulation, reading of the newspaper to the resident, reality orientation by recalling the resident's days in [NAME] Island, and therapeutic touch are provided during 1:1 activities. The SRA also stated Resident #44 has a short attention span, has to be redirected frequently, and curses and yells a lot. The SRA stated they were not able to provide 1:1 recreational activity including aroma therapy during the survey as they were covering additional floors due to a staff's vacation and had additional required duties. During a follow-up interview, the SRA stated the resident was greeted and spoken to for about 10 minutes on 7/7/21, however 1:1 recreational activities were not conducted during this time.
On 07/13/21 at 10:35 AM, the Art Therapist (AT) was interviewed. The AT stated their job duties had changed due to COVID and they have not been able to perform art therapy to residents as current role includes group/individual sessions, supervising smoking, and facilitating calls between family members and residents. The AT also stated staff had taken Resident #44 out for air in the back yard on one occasion last week. The AT also stated the resident listens to music but would often refuse to engage and be easily agitated. Resident #44 would be seen every week, and asked about preferred activities but would get aggressive, curse, shout, and demand that staff get out of the room. The AT stated the Resident #44 was last visited and offered a coloring activity in early June 2021 and responded by telling therapist to get out of their room.
On 07/13/21 at 10:53 AM, an interview was conducted with the Recreation Director (RD) who stated Resident #44 requires sensory stimulation. The resident has a history of profane outbursts. Activities provided to Resident #44 include music, products (touch tactile), redirection, visits to the park/backyard when weather permitting and if the resident allows. The RD also stated this past week (possibly Tuesday) the resident was taken to the back yard by the Home Health Attendant (HHA). The RD further stated the resident should be receiving sensory stimulation 2-3 times a week but could not specify what activities had been provided specifically for Resident #44. The RD further stated that prior to COVID monthly accountability records were maintained of activities being provided on the floor. The RD also stated that they are involved in conducting activities and makes observations of staff once a day during recreational activities.
On 07/13/21 at 02:01 PM, the Administrator was interviewed. The Administrator stated whatever resources/supplies the Recreation Director requests is provided. The Administrator also stated if the resident's care plan calls for one to one activities then that is what should be provided. The Administrator further stated an Art therapist was recently hired and scheduled to start in August.
415.5 (f)(1)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, record review and staff interview conducted during the recertification survey, the facility did not ensure timely identification and removal of expired medications from current m...
Read full inspector narrative →
Based on observation, record review and staff interview conducted during the recertification survey, the facility did not ensure timely identification and removal of expired medications from current medication supply. Specifically, expired medications were observed in the medication storage room. This was evident during the Medication Storage Task (Medication Storage Room/Nursing Office)
The findings are:
The facility policy and procedure titled Medication Storage last revised on 3/12/2021 documented medication will be stored in a manner that maintains the integrity of the product, ensures the safety of the residents and is accordance with New York State Department of Health guidelines .Expired, discontinued and or/contaminated medications will be removed from the medication storage areas and disposed accordingly.
On 07/07/21 at 02:46 PM, an observation of the medication storage room on the 1st floor in the Nursing Office was conducted with the Director of Nursing (DON). The following expired medications were observed in the current medication supply: -
1 Piperacillin and Tazobactam injection 2.25 gram per vial - expired 06/2021
Nitroglycerin tabs full bottle - expired 06/2021
Ketorolac Tromethamine 30mg per ml vial - expired 06/2021
Heparin 5,000 unit per ml vial - expired 06/2021
On 07/07/2021 at 02:55 PM, the DON was interviewed and stated that the medication storage is audited by the Pharmacy Consultant every month and any expired medication observed during audits is removed and replaced. The DON also stated that the last date that the Consultant audited the storage was on May 5, 2021. DON further stated that the supervisors always check for the expiration date of the medication before dispensing it to the unit for residents' use and ensure that the expired medication are not used on the resident. The DON stated that the facility is waiting for the Pharmacy to refill expired medication.
On 07/12/2021 at 11:30 AM, a telephone interview was conducted with the Pharmacy Consultant. The Consultant stated that the facility's carts on all the units except unit 5 were last reviewed and audited on July 6, 2021, while the medication storage on the 1st floor Nursing office was reviewed and audited at a separate date on June 8, 2021. The Consultant stated that the medication review/auditing is done once a month for both medication carts and the storage room at a different date, which does not have to be exact 30 days interval but is dependent on the priority. The Consultant further stated that some Calcium Oyster and IV solution mixture of dextrose and sodium chloride (quantity not sure) were found with expiration date of 5/21 and were pull off from medication storage room during the last audit of June 8, 2021. The consultant stated that any medication that has expiration date of 6/21 expires at the end of June and would not have been removed during the last audit date in June 8, 2021. The Consultant stated that if any medication expires in between the visit dates, the nurse is expected to check and remove the items from the storage before the next audit date.
415.18(a)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations and staff interviews conducted during a recertification survey, the facility did not ensure that all medications and biologicals were stored and labeled properly. Specifically, m...
Read full inspector narrative →
Based on observations and staff interviews conducted during a recertification survey, the facility did not ensure that all medications and biologicals were stored and labeled properly. Specifically, medications were not labelled properly. This was evident during observations conducted for the Medication Storage Task. (3rd floor)
The findings are:
The facility policy and procedure titled Medication Storage revised on 3/12/21, documented that medication will be stored in a manner that maintains the integrity of the product ensures the safety of the residents and is accordance with the New York Department of Health Guidelines.
On 07/12/21 at 04:58 PM, an observation was conducted of the medication cart on the 3rd floor. One plastic bag was observed with a vial of Novolin N in it. There was no open/discard date on the vial. The bag which contained the vial was dated 7/9/21.
One plastic bag was observed with a Levemir insulin pen. The bag was dated 7/6/21. There was no open/discard date on the device.
One bag was observed with a Basaglar insulin pen. The bag was dated 7/5/21. There was no open/discard date on the device.
A bottle of Aspirin 81 mg was also observed in the cart. The manufacturer's expiration date on the label had been smudged and was not visible.
An Anoro delivery system was observed in the packaging box. There was no label identifying the resident that the medication was prescribed for attached to the device.
Licensed Practical Nurse (LPN) #6 working the evening shift, was immediately interviewed. LPN #6 stated that nurses are supposed to label the vials once opened and are responsible for checking the insulin vials each shift. LPN #6 also stated that the labels are supposed to be on each medication and that Anoro box was labelled with the resident's name, so they thought that was good enough.
On 7/12/21 at 05:44 PM, Registered Nurse (RN) #4 was interviewed. RN #4 stated they work as the Evening shift supervisor. RN #4 also stated that insulins are supposed to labeled for either 28 or 30 days depending on manufacturers recommendation and the label should be affixed to the vial or pen and not just on the bag. RN #4 also stated the label should be on the actual container, and not just on the box, as the box can also be discarded. RN #4 further stated that the charge nurse should be the one to label the medication when its open and the supervisor is responsible for checking to ensure that the labelling is done.
On 7/13/21 at 1:38 PM, the Director of Nursing (DON) was interviewed. The DON stated that when a vial is opened, it is supposed to be dated when opened. Labels should not block the instructions and should be placed on a clear area on the bottle. The DON stated that the Pharmacy Consultant audits of the medication carts on a monthly basis and nursing supervisors do weekly audits. The DON further stated that stickers with the opened date should be on the pen and not the bag.
415.18 (d)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review conducted during the recertification survey, the facility did not ensure each resident rece...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review conducted during the recertification survey, the facility did not ensure each resident received food that accommodated resident allergies, intolerance, and preferences. Specifically, residents' food preferences were not honored. This was evident for 2 of 7 residents reviewed for Food out of a sample of 38 residents. (Resident # 22 and Resident # 144)
The findings include:
The policy titled Food Preferences dated 03/10/2021 documented the facility to provide food preferences to resident while allowing residents to make point of service choices that reflect individualized, day to meal preferences as able. The policy also documented that food preferences are communicated to the Food Service Manager and/or Dietitian. Food Service Manager will provide food preferences as possible with the limitations of the facility and withing the dietary restrictions of the resident. Residents can change their food preferences as desired based on verbal and non-verbal cures of food acceptance and preferences as updated in food service systems.
1). Resident # 22 was admitted to the facility with diagnoses that included Type 2 Diabetes Mellitus without complications, Vitamin deficiency unspecified, and Hyperlipidemia.
The Annual Minimum Data Set (MDS) assessment dated [DATE] documented the resident had intact cognition, required supervision and set up help with eating.
The Nutrition Quarterly Review dated 06/30/2021 documented nourishment yogurt at breakfast.
The Nutrition Full assessment dated [DATE] documented new food preferences no eggs hardboiled or scrambled in morning.
The Comprehensive Care Plan (CCP) titled Nutrition Status (At Risk for Nutritional Decline) dated 03/24/2020 documented interventions that included monitor diet preferences and offer substitutes of preferred foods.
The Physician's Order documented the resident as on No Concentrated Sweets/No Added salt diet.
On 07/12/2021 at 08:52 AM, Resident #22 was observed with their breakfast tray that included eggs, oatmeal, milk, 4 oz orange juice, 1 slice of French toast (original menu item was waffle). The resident tray ticket documented No Concentrated Sweets (NCS)/ No Added Salt and (NAS).
On 07/12/2021 at 09:35 AM, Certified Nursing Assistant # 5 was interviewed. CNA#5 stated that resident did not have any food complaints and the resident normally request yogurt and gets daily and if the residents requests something different, the CNA calls the kitchen.
On 07/12/2021 at 11:01 AM, Registered Dietitian (RD #2) was interviewed. RD #2 stated that the resident has food preferences and was spoke with recently regarding their dislike of eggs. RD #2 also stated that a few months ago the food service team, dietary and nursing staff were made aware during a meeting. Resident has a food preference for yogurt as protein source instead of eggs. RD #2 also stated that the comments on the tray ticket should specify no eggs. RD #2 stated that they observe meal rounds one time every week once every two weeks and primary focus on resident with food preferences or dietary needs to make sure they are getting the right thing.
On 07/12/2021 at 12:59 PM, the Food Service Manager (FSM) was interviewed. The FSM stated that they would communicate with the nurse on the unit if there are any menu changes. They stated that they would communicate with the RD when a menu change is made. Food preferences would be noted on tray ticket and we are able to access the system to see them and the dietitians make changes to the resident's menu.
2). Resident #166 had diagnoses which included Hyperlipidemia, Folic acid anemia unspecified, and Thiamine deficiency unspecified.
The admission MDS dated [DATE] documented resident required limited assistance of 1 staff with eating.
The Quarterly MDS dated [DATE] documented was cognitively intact and needed supervision and set up help with eating.
The tray ticket for the resident dated documented resident had a food preference for no red meat and preference was for chicken.
The Nutrition note dated 06/09/2021 documented resident consumes upwards of 75% of meals, snacks, fluids, self feeds, missing some teeth and no known food allergies.
The New admission Nutrition Assessment note dated 12/07/2020 documented food preferences that included pasta, fish, and cold cereal.
The Nursing progress notes dated 01/21/2021 to 05/07/2021 were reviewed and documented resident was observed hoarding foods, feeds self and consumes more food 85-95% of most meals and had no difficulty chewing/swallowing.
The Comprehensive Care Plan (CCP) titled Nutrition Status (At Risk for Nutritional Decline) dated 12/20/2020 documented interventions that included regular consistency diet and determine food preferences and provide within dietary limitations.
On 07/08/2021 at 05:29 PM, an observation was made of the dinner meal for Resident #166. Resident's tray was observed with a ham and cheese sandwic. The resident was observed eating the cheese and bread only and had was not eaten the ham which had been placed to the side of the plate.
On 07/07/2021 at 11:25 AM, an interview was conducted on with Resident #166 who stated that they have discussed food likes and dislikes and don't eat meat except for chicken and don't eat any other kind of meat.
On 07/12/2021 at 10:23 AM, an interview was conducted with RD #1. RD #1 stated that the resident does not like beef too much and would eat chicken, eggs, and other sources of protein. RD #1 stated that they discuss diet changes with Food Service Manager. RD #1 further stated they have had no food complaints from the resident and the resident likes having sandwiches as a snack.
415.14(d)(4)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected multiple residents
Based on observations, records review and staff interviews during the Recertification Survey, the facility did not ensure residents' personal medical information was kept confidential. Specifically, a...
Read full inspector narrative →
Based on observations, records review and staff interviews during the Recertification Survey, the facility did not ensure residents' personal medical information was kept confidential. Specifically, a notice which documented room numbers, type of precaution, and type of infection was observed posted throughout the facility. This was evident for 4 of 4 residents who were on Transmission Based Precautions. (Residents # 390, #133, #690, & 391)
The findings are:
The facility's policy and procedure titled Confidentiality of Information and Personal Privacy dated 03/10/2021 documented that the facility will protect and safeguard resident confidentiality and personal privacy. The policy further documented that posting the resident isolation status or Transmission Based Precaution in the interest of public health is permissible as long as the type of infection remains confidential.
The facility's HIPPA Policy dated 3/10/21 documented that the facility must reasonably protect health information from any intentional or unintentional use or disclosure.
On 07/09/2021 at 1:25 PM, a notice titled Daily Infection Control Update July 9, 2021 which documented room numbers for four residents along with the type of precaution and type of infection was observed posted on a board that contained other notices in the facility lobby adjacent to the elevator. The additional information on the board included the facility's banking hours, smoking hours, visitation, Resident Council meeting notice, monthly happenings, summer notices, and BBQ schedule for each unit.
On 07/09/2021 at 1:25 PM, upon entering the elevator, the notice was observed posted at eye level, fully visible to anyone entering the elevator.
On 07/09/21, from 1:26 PM to 1:30 PM, observation of Unit 2 to Unit 6 was conducted. A copy of the notice was observed taped to the wall next to the door to enter the unit.
On 07/09/2021 at 1:40 PM, multiple staff persons, including family members at the facility for a visit were observed in the lobby in the vicinity of the notice board.
On 07/09/2021 at 2:48 PM, each unit was revisited. The notice was observed taped to the top of the desk of each nursing station, fully visible to anyone walking by.
On 07/09/2021, staff members from different departments were observed entering the units where the infection control updates were visibly posted.
On 07/09/2021 at 2:44 PM, an interview was conducted with Licensed Practical Nurse (LPN) #1. LPN #1 stated that a daily infection control update is posted at the nursing station for everyone to see. It is updated when there is new admission and when the residents are off contact precautions.
On 07/09/2021 at 2:56 PM, an interview was conducted with LPN #2. LPN #2 stated that the daily infection control updates are printed and posted at the nurse's station and is changed every day by the night supervisor.
On 07/09/2021 at 3:27 PM, the Registered Nurse (RN) #3 who was assigned to unit 3 and 4 was interviewed. RN #3 stated that the Infection Control Nurse creates the list every day and gives to the staff who then post it in the building. RN #3 also stated that no one is on contact precaution on our unit right now. RN #3 further stated the notice tells us what type of infection the resident has on each floor, so staff know what type of precautions are needed for the resident. RN #3 stated that for privacy reasons we should only have the type of precaution that the resident is on.
On 07/09/2021 at 3:30 PM, the Senior Recreation Aide (SRA) was interviewed. The SRA stated that the notice is posted to inform the staff of the resident's condition so the staff will know which residents require the use of gowns before they enter the room. The SRA also stated that they observe the notices on all the floors, all of the time.
During an interview on 07/09/2021 at 3:30 PM, the Director of Nursing (DON) stated that the DON is responsible for the daily infection control updates notice. The infection control notice is renewed every day and as needed and posted in the elevator and on all the units daily. The DON also stated that the notice is posted daily to protect residents, staff, visitors, and consultants as this is the way for all staff to know the residents on isolation and the PPE applicable to that room so they can comply with the PPE requirement. The DON further stated that since the resident's name is not listed on the posting they did not think that it violated the resident's right to privacy or confidentiality although a room number and bed number were noted on the posting.
On 07/09/2021 at 3:37 PM, the Administrator was interviewed. The Administrator stated that the Nursing department posts the infection control updates to inform staff of which residents are on precaution and the type of PPE to use. The Administrator also stated that according to the facility's Confidentiality of Information and Personal Privacy policy, posting residents isolation status is not a violation as long the isolation status remains confidential. As per the policy, the reason for the isolation should not be included. The Administrator further stated that the residents' isolation status should not be posted.
413.3(d)(1)(ii)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews, and interviews conducted during the recertification survey, the facility did not ensure t...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews, and interviews conducted during the recertification survey, the facility did not ensure that necessary housekeeping services were provided to maintain a safe, clean, comfortable, and homelike environment. Specifically, a corroded radiator cover, unpainted areas, mis-matched paint and water damage on the walls were observed in residents' rooms. This was evident in multiple rooms on 3 of 6 units. (Units 1, 2 & 3)
The findings are:
The facility policy and procedure for Environmental Services revised on 3/11/2021 documented it is the policy of [NAME] Nursing Home, to provide clean, contamination-free surroundings for residents, visitors, and personnel. A clean environment is essential in preventing transmission of infection in the facility .Needed repairs, leaky faucets, light bulbs, are to be reported to the Maintenance Supervisor for attention and repair.
On 07/07/21 at 10:45 AM, mismatched paint was observed on the walls next to two beds in room [ROOM NUMBER].
On 07/07/21 at 11:47 AM, bed linen saturated with urine was observed in room [ROOM NUMBER]A. Mismatched paint was also observed on the wall behind the residents' closet.
On 07/07/21 at 11:58 AM, panels for a heating radiator installed in room [ROOM NUMBER]D were observed to be corroded, and peeling painting was observed on the radiator cover exposing blackish colored metal corrosion on the top and side of the radiator.
On 07/07/21 at 03:31 PM, Resident #120 was observed in room [ROOM NUMBER]A during an interview and stated the bulb has been out since I've been here. One bulb from a fluorescent light fixture was observed to be out during multiple observations during the survey. Unpainted patches were observed on the wall on the side of the bed and other areas of the wall. Multiple bags were observed on the floor at the foot of the resident's bed.
On 07/08/21 at 10:25 AM, walls with unpainted areas and other areas with mis-matched paint were in room [ROOM NUMBER]C. Water damage was also observed on the wall.
The above findings were noted throughout the survey period.
The Maintenance logbooks on floors 1, 2, and 3 were reviewed. None of the above concerns were documented in any of the log books.
On 07/12/21 at 08:55 AM, an interview was conducted with the Certified Nursing Assistant (CNA) #1 assigned to Unit 1. CNA #1 stated that if anything is noted to need repair or to be fixed in the resident's room or area, the charge nurse is notified. CNA #1 also stated that the staff in charge of the housekeeping/maintenance are also notified of the problem when they come around on the floor. CNA #1 further stated that the housekeeping staff has already been made aware of the peeling paint in room [ROOM NUMBER] and believe that they are trying to fix it.
On 07/12/21 at 09:07 AM, and interview was conducted with the Charge Nurse, Licensed Practical Nurse, LPN #1 assigned to Unit 1. LPN #1 stated that if anything needed to be repaired on the unit, the Maintenance Supervisor is notified on phone. LPN stated that there is a logbook to report other critical issues for the maintenance to fix, but most of the repairs needed on the unit is communicated via phone to the maintenance department.
On 07/12/21 at 09:31 AM, an interview was conducted with the RN Supervisor, RN #1 who provides coverage for Unit 1 and 2. RN #1 stated that if they notice anything that needed to be fixed while making rounds on the unit, it is discussed at the morning report, and the supervisor in charge of maintenance will address the problem. RN #1 also stated that the peeling paint on walls in room [ROOM NUMBER] had been discussed at the morning report about 2 weeks ago and believes that the maintenance is working on it.
On 07/12/2021 at 09:55 AM, Maintenance Staff (MS) #5 who does the painting at the facility was interviewed. MS#5 stated that they are informed by the supervisor of needed work and sometimes they make rounds or a coworker will notify them that work needs to be done. MS #5 also stated that they were informed of the painting work in room [ROOM NUMBER] about a week ago but has also been assigned to other places to work on and has not been able to get it done yet.
On 07/12/21 at 10:26 AM, the Director of Housekeeping/Maintenance (DHM) was interviewed and stated that there is a maintenance log book on the units. Staff makes rounds daily to check the book and check for any concerns. The DHM also stated that the department is aware of the peeling paint on the unit, the area has been plastered, and just waiting for the painting. The director stated that they were about to paint it when the surveyors arrived.
On 07/13/21 at 09:16 AM, an interview was conducted with the Registered Nurse (RN #2), covering unit 2. RN #2 stated that there is a maintenance book on the unit to report any issue or concerns on the unit or the resident's room for Maintenance staff to check and repair. The RN stated that staff may also call the maintenance staff on phone or make verbal report of any issue or concern to be repaired. The RN stated that the corroded radiator panel in resident #127's room is an oversight that has not been noted or reported for repair.
On 07/13/21 at 09:20 AM, the Nursing Supervisor, RN #1 was interviewed and stated that rounds are made on the unit and on the residents daily. Anything that is noted in the resident's area or rooms to be fixed is reported to the maintenance. RN #1 further stated that the corroded radiator cover in the resident room was not noted and had not been reported.
On 7/13/21 01:03 PM, a follow-up interview was conducted with the DHM. The DHM stated they are usually informed of issues on the unit by word of mouth as the log books on the unit are not really being utilized. The DHM also stated they make daily rounds on the units and observe for cleanliness and needed repairs. The DHM also stated that some of these issues, such as the light bulb that needed to be replaced, should have been brought to his attention by housekeeping staff.
On 07/13/21 at 01:21 PM, the Administrator was interviewed. The Administrator stated they occasionally make rounds through the building. The Administrator also stated that while making rounds they would go into resident's rooms and see if there are any issues. The Administrator further stated that the DHM should be going into all areas of the building and ensuring that needed repairs are being made as necessary.
415.5(h)(2)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected multiple residents
Based on record review, interviews and observations conducted during the recertification survey, the facility did not ensure that resident is free from physical restraints imposed for discipline or st...
Read full inspector narrative →
Based on record review, interviews and observations conducted during the recertification survey, the facility did not ensure that resident is free from physical restraints imposed for discipline or staff convenience and not required to treat the resident's medical symptoms. This was evident for 3 of 3 residents reviewed for Physical Restraints out of total sample of 38 residents (Residents #157, #35, and #110)
The findings are:
The facility's policy & procedure titled Physical Restraints revised on 3/12/2021 documented Oxford Nursing Home considers restraints to be a temporary care modality that is used to treat a particular Resident's medical symptom. The decision to restrain a Resident or discontinue the use of restraints is an on-going process, closely monitored and evaluated by Nursing staff, the Comprehensive care Plan (CCP) Team and the Physician. Prior to any decision to retrain a Resident, alternative measures will be used.
1. Resident #157 was admitted to facility with diagnoses which included Hypertension, Diabetes Mellitus, Non-Alzheimer's Dementia, Depression, and Pressure ulcer of left heel, unstageable.
On 7/7/21 at 10:48 AM and 7/09/21 at 08:45 AM, Resident #157 was observed lying in bed with wedge pilows placed under the fitted sheet on the mattress causing the edge of the bed to be raised and create a concave appearance to the bed.
The bed was not placed in the lowest position and the other side of the bed was placed up against the wall.
Review of the medical record revealed no Comprehensive Care Plan or Physician's Order for a Physical Restraint.
On 07/13/21 at 09:45 AM, Certified Nursing Assistant (CNA) #3 assigned to Resident #157 was interviewed. CNA #3 stated resident needs extensive assistance with 2 people for Activities of Daily Living (ADL'S) and is totally dependent on staff for eating. CNA #3 stated resident sometimes comes to the side of the bed and they tuck the wedge pillow inside of the fitted sheets to prevent the resident from coming out of the bed. 2. Resident #35 was admitted to the facility with diagnoses that included Non-Alzheimer's Dementia, Anxiety Disorder, Depression, and Unspecified Dementia with behavioral disturbance.
On 07/07/21 at 10:11 AM, 07/08/21 at 09:18 AM and 12:31 PM, 07/09/21 at 09:08 AM, 07/12/21 at 09:08 AM, and 07/13/21 at 09:25 AM, Resident #35 was observed lying in bed with the wedges placed under right side of mattress causing the edge of the bed to be raised. The resident's left side of bed was placed up against the wall. The bed was not in the lowest position.
The Care Plan for Physical Restraint/Enablers/Devices created on 6/19/2020 and revised on 6/23/2021 documented goal is have the least restrictive form of restraint to treat medical symptoms/condition. Interventions included evaluate need for continued use of restraint/device and evaluate use of alternatives. The problem statement documented as evidenced by other devices (Mittens). Evaluation note dated 6/23/2021 documented resident remained free from physical restraint and goal was met.
Physician order revised on 6/18/2021 documented mitten restraint. There was no order for any other physical restraint.
There was no observation of the resident wearing mittens at any time.
3. Resident #110 was admitted to the facility with diagnoses that included Non-Alzheimer's Dementia, CVA, Hemiplegia or Hemiparesis, and Depression.
On 07/07/21 at 10:26 AM, 07/08/21 at 09:13 AM, 07/09/21 at 09:06 AM, 07/12/21 at 09:05 AM, and 07/13/21 at 09:17 AM, Resident #110 was observed lying in bed with wedge pillows placed under right side of mattress causing the edge of the bed to be raised and create a concave appearance to the bed. The left side of the bed was placed against the wall. The bed was not at the lowest position.
Review of the medical record revealed no Comprehensive Care Plan or Physician's Order for a Physical Restraint.
On 07/13/21 at 09:49 AM, CNA #2 assigned to Resident #110 was interviewed. CNA #2 stated the resident is able to make needs known. The resident needs assistance of 2 staff for most ADLs. CNA #2 also stated resident is taken out of bed after 11 AM or after lunch and has not had any falls in the facility. CNA #2 further stated the resident has wedge pillows placed on the right side of the bed to assist with positioning and to keep the resident from getting out of bed. The wedges have been put to assist the resident with safety and are always placed when the resident is in bed and is not being directly watched.
On 07/13/21 at 09:58 AM, CNA #2 who was also assigned to Residents #35 was interviewed. CNA #2 stated the resident comes out of room around 10 AM or 11 AM. Evening shift will take the resident out also because the resident has to be observed. CNA #2 also stated the resident has wedge pillows placed on the right side of the bed to assist with positioning the resident's legs and to keep the resident from getting out of the bed. CNA #2 further stated the wedges have been put to assist the resident with safety and are always placed when the resident is in bed and is not being directly watched.
On 07/13/21 at 11:07 AM, the Physical Therapist (PT) was interviewed. The PT stated therapists are involved in devices like wedge pillows but if a device is used to prevent the resident from falling that would be the nursing department decision. The PT also stated the nursing department can refer to us if the resident would need a device. For fall prevention, the bed is put at the lowest position and because a resident may roll or slide, devices may be put also for safety and positioning. The PT further stated that no referrals have been received for an evaluation for devices for any of these residents.
On 07/13/21 at 11:32 AM, Registered Nurse (RN) #3 was interviewed. RN #3 stated the wedge pillows are used to prevent the resident from sliding from the bed and were provided by the Rehab Department. RN #3 also stated that the bed is in the highest position and placed up against the wall. Resident #110 cannot get out of the bed because of their physical condition. Resident #110 was sliding out of the bed and rehab was asked to provide wedge pillows. RN #3 stated they did not know why wedge pillows were being used with Resident #35 and will have to go to the computer to see who provided it. RN #3 also stated that Resident #157 exhibited agitated behavior and they could not speak to why this resident had wedge pillows.
On 07/13/21 at 11:49 AM, the Director of Nursing (DON) was interviewed. The DON stated wedge pillows are used if there is a need or concern for positioning. The resident is referred to OT or PT and they determine the appropriateness of the device. Nursing may have a recommendation but OT or PT may not agree. The DON also stated wedge pillows should not be used to keep residents in the bed as that would be considered a restrictive device. The DON further stated the bed for resident # 110 should not be up against the wall and they did not know why the wedge pillows were being used. There would need to an interdisciplinary for the resident and involvement of the resident and family is devices were needed. The DON stated that Resident #35 does have behavior but the same process would apply and family is very involved in care of this resident. For Resident #157, they were not aware of any need for wedge pillows used in this way for the resident. The DON further stated they do make general rounds on the unit.
On 7/13/21 at 2:02 PM, the Medical Director (MD) was interviewed. The MD stated they are at facility twice weekly. The MD also stated that wedge pillows are usually used to position residents, to provide stability, and to provide maneuverability post-surgery after joint replacement. Wedge pillows should not be utilized to prevent residents from coming out of bed. If the physician feels there is a medical need for it, it may be ordered. Then the physician would refer the resident to OT/PT for evaluation. The MD further stated that the least restrictive measures are always utilized if resident is at risk of fall or harm and the use is done in communication with family. The MD stated that none of the attending physicians had brought this to their attention and often when the physicians are doing evaluation of the residents, they are focused on the medical issue and may not be paying attention to other things like that.
415.4 (a)(2-7)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. On 07/07/2021 at 3:12 PM, Resident #22 was interviewed and stated that they had not been invited to participate in care plann...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. On 07/07/2021 at 3:12 PM, Resident #22 was interviewed and stated that they had not been invited to participate in care planning meetings.
The Annual Minimum Data Set (MDS) dated [DATE] documented that resident was cognitively intact and documented resident participated in the assessment and no family/significant other participated in assessment.
The Quarterly Minimum Data Set (MDS) dated [DATE] documented resident is cognitively intact and resident has no guardian or legally authorized representative.
The document titled MDS and Comprehensive Care Plan Schedule documented CCP meetings were held on 3/31/20, 7/1/2020, 9/30/2020, 12/30/2020 and 3/31/2021.
Social Services notes dated 03/25/2020 to 07/09/2021 contained no documented evidence that resident had been notified of or attended any of the care planning meetings.
Nursing Progress notes from admission to present were reviewed and there was no documented evidence that the resident had been notified or invited to participate in care planning meetings.
On 07/12/2021 at 10:10 AM, an interview was conducted with the Licensed Practical Nurse (LPN #5). LPN #5 stated that there had been care planning meetings on the unit and they participated in care planning meetings for the Resident #22 but the resident was not present at the meeting. LPN#5 stated the interdisciplinary team met without residents during the pandemic.
4. On 07/07/2021 at 4:46 PM, Resident #143 was interviewed and stated that they had not been invited to any care planning meeting.
The Annual Minimum Data Set (MDS) dated [DATE] documented that resident was cognitively intact and documented resident participated in the assessment and no family/significant other participated in assessment.
The Quarterly Minimum Data Set (MDS) dated [DATE] documented resident is cognitively intact, and resident has no guardian or legally authorized representative.
There was no documented evidence in the medical record that the resident was informed of, invited to, or participated in any care planning meetings after 12/14/2020.
On 07/12/2021 at 10:10 AM, an interview was conducted with the Licensed Practical Nurse (LPN #5). LPN #5 stated that there had been care planning meetings on the unit and they participated in care planning meetings for the Resident #143 but the resident was not present at the meeting. LPN#5 stated the interdisciplinary team met without residents during the pandemic.
On 07/13/2021 at 09:30 AM, an interview was conducted with the Director of Social Work (DSW). The DSW stated care planning meeting are held with family and resident. During the pandemic they reached out to family via phone. The DSW also stated that residents with intact cognition would be invited to the meetings but during the pandemic meetings were held without the resident and they were given updates by staff after the meeting.
415.11(c)(2) (i-iii)
2. Resident #67 was admitted to the facility with diagnoses that included Anemia, Hypertension, and Seizure Disorder.
On 07/08/21 at 08:49 AM, Resident #67 was interviewed. Resident # 67 stated they did not recall being informed of or invited to any care plan meeting since being in the facility.
The admission MDS dated [DATE] and Quarterly Minimum Data Set (MDS) dated [DATE] documented the resident had intact cognitive status.
The Comprehensive Care Plan (CCP) for Cognitive Loss/Dementia dated 10/25/2019 documented that resident has no impairment in memory or recall ability; independent in decision making. Interventions included monitor for changes; provide opportunities for social changes.
The Comprehensive Care Plan (CCP) for Communication dated 10/25/2019 documented that resident hears adequately, with adequate communication ability. Interventions included: address resident needs in a timely manner; encourage resident to verbalize feelings and concerns.
The facility record of attendance for CCP meetings documented that care planning meetings were held for the resident after admission on [DATE], and a quarterly meeting was held on 04/28/2021.
There was no documented evidence that Resident #67 or their representative was invited to or attended any of the meetings.
Progress Notes dated 01/19/2021 to 7/13/2021 contained no documented evidence that resident or representative was invited to participate in care planning meetings.
On 07/12/21 at 01:01 PM, an interview was conducted with the Social Worker (SW). The SW stated that residents are invited to care plan meeting quarterly and based on resident's needs. The SW also stated that Social Services has been communicating regularly with Resident #67 and the family members since resident was re-admitted to the facility. SW was unable to explain why there was no documented evidence that resident and/or the family member had been notified of or invited to participate in any scheduled CCP meeting.
On 07/13/21 at 09:42 AM, an interview was conducted with the Registered Nurse (RN) #2. RN #2 stated that residents' care plan meeting is held quarterly, or if there is a significant change in resident's status. RN #2 also stated that the MDS department schedules the meeting, and the Social Worker will notify the resident and the family member to attend the meeting. RN #2 further stated that there is a sign-in sheet for each of the resident's care meeting which is kept by nursing. On this sheet the interdisciplinary team members and the resident/family members sign documenting attendance at the meeting. RN #2 was unable to explain why the resident and/or resident's representative were not invited to the meeting as per the record of attendance produced.
On 07/13/21 at 10:51 AM, an interview was conducted with the Director of Social Work (DSW). The DSW stated that when Resident #67 was admitted , resident was assessed to be moderately cognitively impaired with a BIMS score of 11 and was unable to comprehend information given, which might be why the resident was not invited. The DSW also stated that resident or the family member was not notified before the CCP meeting, but the family member was updated about the initial CCP meeting after the meeting was held. DSW was unable to explain why the resident or resident's representative was not invited to the Quarterly meeting held on 4/28/2021.Based on record review and interviews conducted during the Recertification Survey, the facility did not ensure that each resident and resident representative was involved in developing the care plan and making decisions about their care. Specifically, the facility did not ensure that residents and resident representatives were afforded the opportunity to participate in the Comprehensive Care Plan (CCP) meeting. This was evident for 4 out of 6 residents reviewed for Participation in Care Planning. (Resident #52, #67, #22 and #143).
The findings include:
The facility policy and procedure titled Comprehensive Care Plan Meeting dated 03/03/2021 documented it is the facility's policy to encourage residents and families to participate in forming a plan of care. The policy also documented that the facility values the input of residents, family members, and community patterners to assure and achieve a good continuum of care best solution outcome and promote high-quality care. The policy further documented that during the MDS (Minimum Data Set) & Comprehensive care plan schedule (admission, quarterly, a significant annual change, or as requested), residents and families will be contacted by the Social Services to have the opportunity to obtain input from all involved disciplines.
1. Resident #52 was admitted to the facility with diagnoses that included Type 2 Diabetes, Mood Disorder and Hypertension. The (MDS) dated [DATE] documented resident had intact cognition.
During an interview on 07/07/2021 at 12:01 PM, Resident #52 stated that he had not been invited to attend the care planning meeting.
Social Service Progress Note dated 06/03/2021 documented that Resident #52's representative was updated on the resident and the plan of care.
There was no documented evidence that either that Resident #52's or their representative had been invited to participate in the quarterly care plan meeting.
Review of the CCP Meeting sign-in sheet dated 6/3/21 contained no evidence that Resident #52 or their representative was not notified of or attended the CCP Meeting.
During an interview on 07/13/2021 at 11:53 AM, the Licensed Practical Nurse (LPN) #7 stated that he attended the care plan meeting that was held on 6/3/21 for Resident #52. Neither Resident #52 nor their representative was at the meeting. LPN #7 also stated that at times the family member will be included by phone and they were not sure if Resident #52's representative was called during the meeting.
During an interview on 07/13/2021 at 12:23 PM, the Director of Social Work (DSW) stated that on 06/03/2021, Resident #52's representative was updated with the plan of care after the care plan meeting was held. Resident #52 was also updated with the plan of care but was not invited to the care plan meeting. The DSW also stated Resident #52 was alert and oriented and should have been invited to attend the care plan meeting.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and staff interviews conducted during the recertification survey, the facility did not ensure that food was stored and prepared in accordance with professional standards for food ...
Read full inspector narrative →
Based on observation and staff interviews conducted during the recertification survey, the facility did not ensure that food was stored and prepared in accordance with professional standards for food service safety. Specifically, potentially hazardous cold foods were not maintained at the proper temperature (at or below 41 degrees Fahrenheit). This was observed during the Kitchen Observation facility task.
The findings are:
The facility's policy and procedure titled Food Temperatures, revised on 03/10/2021, documented cold foods stay below 40 degrees Fahrenheit during the portioning, transportation, and service process until received by the resident. Normally cold food items will be well below 45 degrees when removed from cooling and must be kept below 40 degrees until served.
The facility policy and procedure titled Handling Cold Foods For Trayline revised on 03/10/2021 documented at the time of service cold food items will be taken from the refrigerator one tray at a time to be used at the meal service (unless a reach-in refrigerator is available on meal service) and cold temperatures will be taken and recorded prior to service to assure foods are at or below 40 degrees Fahrenheit.
The undated facility policy and procedure titled Potentially Hazardous Foods documented this facility to identify potentially hazardous foods to prevent any foodborne illness. Although almost any food can be contaminated, certain foods are considered potentially hazardous foods (PHF) or Time/Temperature Controlled for Safety (TCS) food. TCS Foods include milk and dairy and meat.
A tray line observation was done on 07/08/2021 at 04:37 PM with the Cook. The internal temperature of a ham and cheese sandwich was 73.9 degrees Fahrenheit (F). The State Agent (SA) and [NAME] checked the temperature of an additional sandwich being prepared at room temperature in the prep area and the temperature was noted to be 73.7 F.
During the tray line observation, ham and cheese sandwiches were being prepared for the dinner meal using sliced ham and cheese sandwich on white bread that was noted not to be on ice while it was being prepared.
On 07/08/2021 at 04:53 PM, the Dietary Aide (DA) was interviewed. The DA stated that after making sandwiches they put them back in the refrigerator and they normally keep the ham and cheese in the refrigerator. The DA also stated that they had food safety training when they started their job two months ago. Cold cuts should be held at 30- 40 degrees Fahrenheit. The DA further stated meats for sandwiches have to be kept cold and if held at high temperatures will spoil and become contaminated.
On 07/08/2021 at 05:05 PM, an interview was conducted with the Food Service Manager (FSM). The FSM stated that the ham and cheese sandwiches used to be prepped on ice and sent upstairs to units. The sandwiches are now being assembled in the kitchen. The FSM also stated sandwiches should be 35 degrees Fahrenheit for meal service. Temperature danger zone is over 41 degrees Fahrenheit.
On 07/08/2021 at 05:18PM, an interview was conducted with the [NAME] who stated that the sandwich temperatures should be 35 degrees Fahrenheit. The [NAME] also stated that proper temperature of cold food needs to be below 35 degrees andit is important to make sure food does not spoil and give resident any food borne illnesses. The [NAME] further stated that they had food safety in-service 1 week ago.
415.14(h)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. The facility policy and procedure Environmental Sanitation Services dated 03/11/2021 documented before entering rooms scrub h...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. The facility policy and procedure Environmental Sanitation Services dated 03/11/2021 documented before entering rooms scrub hands and arms using anti-microbial disinfectant soap for no less than 3 minutes. Dress in proper isolation attire (gloves, gown, disposable mask). A cart should be set up outside the room containing proper isolation.
On 07/08/2021 at 9:40AM, an interview was conducted with Licensed Practical Nurse (LPN) #5. LPN #5 stated the resident in room [ROOM NUMBER] was being maintained on Contact Precaution for Methicillin Resistant Staphylococcus Aureus (MRSA) infection.
On 07/08/2021 at 11:29PM, [NAME] #1 donned vinyl gloves, wore a surgical mask and entered room [ROOM NUMBER]. Signage was posted on the door which stated STOP check with nurse before entering. Please note strict hand hygiene required, wash hands with soap and water: gown, gloves and any other applicable PPE. [NAME] #1 did not don an isolation gown upon entering the resident room. [NAME] #1 was then observed collecting waste from a biohazardous can in the room. [NAME] #1 placed the biohazardous bag on top of the other biohazardous can, removed gloves and washed hands. The porter then donned another pair of gloves and took the biohazardous bag to the Porter's closet and placed the biohazardous on top of a regular garbage can. There was no biohazardous bin observed in the porter's closet. The [NAME] then proceeded to the soiled linen room and washed their hands.
On 07/08/2021 at 11:32 AM, [NAME] #1 was interviewed. [NAME] #1 stated that they normally put on a gown when entering the room. [NAME] #1 also stated that the room is on isolation and they did not know what kind of precautions were in place but they should wear a gown when removing the garbage. [NAME] #1 further stated that they have had training on Personal Protective Equipment (PPE) and PPE is located outside of the resident's door.
On 07/09/2021 at 11:05AM, the Director of Housekeeping/Maintenance (DHM) was interviewed. The DHM stated that there is a resident on the 5th Floor on isolation that they are aware of. Staff should use mask, gloves, gown every time they go into that room. They should be wearing PPE to protect themselves and residents also. The DHM also stated staff has had in-service this month on wearing of PPE. They were informed by nursing supervisors of residents who are currently on precautions.
On 07/09/2021 at 11:51 AM, the Director of Nursing Services/Infection Control Manager (DON) was interviewed. The DON stated they were unaware that there were residents on isolation on the 5th floor. The DON also stated staff should be wearing appropriate PPE when engaged in tasks involving body fluids or blood borne pathogens for a resident maintained on precautions. The DON also stated that for a resident maintained on contact precautions, staff should wear gowns and gloves when handling resident or biohazardous waste in the room. In a follow-up interview, the DON stated there was a resident on contact precaution on the 5th Floor.
415.19 (a)(1-3)
2. A undated facility policy and procedure titled Environmental Sanitation Services documented the housekeeping staff are responsible for disposing of trash in residents' rooms at least daily and gloves should be changed inn between each resident room.
On 07/08/21 at 10:59 AM, Housekeeper #1 was observed carrying a clear plastic bag 3/4 full with garbage (plates, cups, napkins, food) towards the western hallway of the unit (room [ROOM NUMBER]-208). Housekeeper #1 entered room [ROOM NUMBER] with the plastic bag in hand and picked up a garbage can that was placed next to the bed by the door. The housekeeper did not empty garbage from the small container into the bag. Housekeeper #1 left the room, went through the hallway with the large plastic garbage bag in hand, and entered the door of room [ROOM NUMBER]. In room [ROOM NUMBER], the housekeeper picked up a small garbage can, emptied it into the larger plastic bag, and then placed the large plastic bag on the floor. The housekeeper took a garbage bag from a cart in the hallway, placed it in the small garbage can, picked up the filled garbage bag and walked through the hallway back towards the dining room area. The housekeeper was then observed walking to the eastern hallway of the unit and went to the porter's closet at the end of the hallway. The plastic garbage bag was tied at the top and placed on the ground while the housekeeper opened the porter's closet. Two garbage bins with lids were observed in room. The housekeeper opened another porter closet door and revealed a large empty garbage bin with a cover.
On 07/08/21 at 11:03 AM, Housekeeper #1 was interviewed. Housekeeper #1 stated he had not been trained to carry the garbage bag around the unit without a bin. The proper procedure to remove garbage is to move from room to room with a covered garbage bin. Housekeeper #1 also stated they did not take the covered garbage bin from the porter's closet because they were trying to save time and quickly empty the full garbage cans in the resident's room. Housekeeper #1 further stated that they know they are not supposed to pick up the garbage without the covered bin.
On 07/08/21 at 03:38 PM, an interview was conducted with the Director of Housekeeping (DH). The DH stated a covered bin is supposed to be used to gather garbage from residents' rooms. The DH also stated the facility policy reflects this and no housekeeping staff should be using a clear plastic garbage bag alone to collect garbage.
On 07/08/21 at 09:46 AM, Licensed Practical Nurse (LPN #4) on Unit 4 was observed assessing blood pressure for Resident #170. LPN#4 then removed the BP cuff, placed it next to the medication cart, entered information into laptop on the medication cart then administered medication to Resident # 170. LPN #4 did not sanitize the blood pressure cuff after use.
At 9:53 AM, LPN #4 approached Resident #131, placed the BP cuff over the sleeve of the resident's shirt and took the residents blood pressure. LPN #4 then removed the BP cuff and placed it next to the cart then proceeded to administer medication to Resident #131. LPN #4 was not observed sanitizing the blood pressure cuff before or after use on Resident #131.
At 10:04 AM, LPN #4 placed the BP cuff on Resident #92. The resident removed the BP cuff when reading was complete and placed it on nursing station. At 10:07 AM, LPN #4 was observed moving the BP cuff on the top of wooden ledge next to the medication cart. LPN #4 was not observed sanitizing the blood pressure cuff before or after use on Resident #92.
On 07/08/21 at 10:23 AM, LPN #4 was interviewed. LPN #4 stated the blood pressure cuff is cleaned every morning at the beginning of the shift. LPN #4 also stated when residents wear shirts, the brown tissue (napkin) is used to cover the arms while using the BP cuff but the BP cuff was placed over the shirt of Resident #131. LPN #4 further stated the BP cuff should have been cleaned after use on each resident, especially when the BP cuff is on the skin. If the resident refuses to use the brown tissue, the BP will be cleaned with the wipes (purple top) before using the BP cuff on another resident. LPN #4 stated generally BP cuff is cleaned with the purple top wipes at the end of the shift. LPN 4 stated in-service training related cleaning of the BP cuff was received last year.
On 07/08/21 at 10:41 AM, an interview was conducted with Registered Nurse #3. RN #3 stated when a potential problem is observed, in-service is provided to ensure staff are performing the right steps. RN #3 also stated in-services are provided monthly and as needed to for infection protocol and medication error. RN #3 further stated BP cuffs and equipment needs to be cleaned between each resident and every nurse is aware of this.
On 07/12/21 at 03:06 PM, an interview was conducted with the Director of Nursing (DON). The DON stated in-services are conducted at a minimum on a monthly basis which included cleaning of equipment and blood-borne pathogens. The DON also stated equipment (including BP cuff and thermometer) are cleaned with Sani-wipes at the beginning and end of the shift by the nurse when used with multiple residents. The DON stated the staff does not need to clean the BP cuffs when used between residents. If there is a concern about a skin condition, an individual BP cuff would be given. The DON further stated the nurse will ensure that the resident have no skin issues from direct observation as the nurse must observe the resident's skin prior to using the BP cuff. The DON stated if there is any potential for blood borne pathogen or impaired skin integrity the equipment cannot be shared to prevent cross contamination. The DON also stated medication pass observation are performed quarterly.
Based on observations, record review, and staff interviews conducted during the recertification survey, the facility did not ensure infection control practices and procedures were maintained to provide a safe and sanitary environment to help prevent the development and transmission of communicable diseases and infections. Specifically, 1). blood pressure (BP) cuffs were not cleaned/disinfected after use between residents, 2). a housekeeping staff did not properly store and transport garbage while on the unit, and 3). a housekeeping staff did not don the required Personal Protective Equipment (PPE) upon entering a room where transmission-based precautions were in place. This was evident during the Infection Control Tasks on 4 of 6 units. (Units 3, 4, 2 & 5)
The findings are:
1.The facility policy titled Care of Equipment related to Blood Pressure Cuff revised on 03/12/2021 documented the following under the section titled procedure: 3. Deep cleaning of blood pressure cuff at beginning and end of shift should be done with Sani wipes. 4c. Prior to application of blood pressure cuff, inspect skin for rash, blister, redness, or any alteration to skin integrity. 4d. If skin in is intact, proceed with procedure of blood pressure monitoring.
On 07/08/21 between 08:56 AM and 09:09 AM, LPN #2 was observed administering medication to two residents on the 3rd floor, (Resident #12 and Resident #65). LPN #2 was observed applying blood pressure (BP) cuff on the left arm of Resident #12 without prior inspection of the resident's skin, and without sanitizing the BP cuff prior to assessing the resident's blood pressure. LPN #2 administered medication to Resident #12 and then proceeded to Resident #65. At 9:09 AM, LPN #2 was observed applying the BP to the arm of Resident #65. LPN #2 did not inspect the resident's skin or sanitize the BP cuff before placing the cuff on the resident's arm.
On 07/08/21 at 11:57 AM, an interview was conducted with LPN #2. LPN#2 stated that the blood pressure cuff is supposed to be cleaned before and after every resident. LPN #2 stated it was not cleansed in the morning in between the two residents because they were pre-occupied with other things while being observed by surveyor for medication administration.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview conducted during a recertification survey, the facility did not ensure that a safe, functiona...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview conducted during a recertification survey, the facility did not ensure that a safe, functional, sanitary, and comfortable environment is provided for staff and public. Specifically, the staff bathrooms and a resident bathroom were not maintained in good repair. This was observed on 3 of 6 resident units. (Unit 2, Unit 3 & Unit 4)
The findings are:
The facility policy & procedure titled Preventive Maintenance Program revised on 3/11/2021 documented it is the policy of [NAME] Nursing Home and the Maintenance Department to provide a hygienically clean environment by systemic inspection and preventive maintenance of all equipment, by established routines for repairs and by proper care of the entire physical structure of the institution.
On 07/12/21 at 05:18 PM, the staff bathroom on Unit 3 has observed with mismatched paint on bathroom walls over toilet, a wooden/board plate behind sink, rusted protrusion on lower left wall below the sink, peeling ceilings, dusty walls, chipped paint on wall next to sink and mismatched paint above soap dispenser.
On 07/12/21 at 05:27 PM, the staff bathroom on Unit 4 was observed with mismatched paint on the wall next to toilet, a dusty air vent, and chipped paint on a pipe. The door jamb on inner door was rusted on the lower end. The first stall of the resident male bathroom had chipped paint on a pipe and broken tiles.
On 07/12/21 at 05:33 PM, the staff bathroom on Unit 2 was observed with a towel dispenser with a rusted top, there was a leak and mismatched paint on the wall behind the toilet, chipped paint above sink, and the soap dispenser was crooked and loose.
On 7/13/21 at 01:03 PM, the Director of Housekeeping/Maintenance (DHM) was interviewed. The DHM stated the communication for maintenance is usually by word of mouth. The DHM also stated that the building is very old and they try to get to everything. The DHM further stated the rusted paper dispenser should have been removed. The DHM stated that they do make rounds in the staff bathroom areas and issues identified should have been taken care of.
On 07/13/21 at 01:21 PM, the Administrator was interviewed. The Administrator stated that he occasionally makes rounds in the building. The Administrator also stated that vents should have been cleaned in the staff bathrooms. Housekeeping staff should be going into all areas of the building and ensuring that repairs are being made as necessary. The Administrator further stated that they do make rounds in the building and may not have gone into the staff bathrooms and have looked at those conditions.
415.29
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review conducted during the Recertification survey, the facility did not ensure it m...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review conducted during the Recertification survey, the facility did not ensure it maintained an effective pest control program so that the facility is free of pests and rodents. Specifically, (1). One live rodent was noted in the dining area in the basement, and (2) one live brown colored roach about half an inch in length was noted in the nurse's station on the 5th Floor. This was evident on 1 of 6 units. (5th Floor)
The findings are:
The facility policy titled Insect and Rodent Control dated 03/11/2021 documents it is the facility policy to reduce the spread of infection and disease. The facility has in place an integrated Pest Management Program. The A & N Pest Control is contracted to assist in this program. All staff are instructed to report all roach and pest observations to the Director of Housekeeping and Nursing Supervisors. The sightings must also be entered into the maintenance log at nurse's station.
The Extermination Service Report dated 1/05/2021 to 07/06/2021 documented no infestations noted and the corrective action taken to include G/Boards Max Force Gel, IPM MaxForce Gel, G/Boards IPM.
The A& N Pest Control Report dated 07/09/2021 documented on the third floor room [ROOM NUMBER] and 307 roaches were found. On 06/09/2021 for room [ROOM NUMBER] and 508 roaches were found and treated. On 06/16/2021 for room [ROOM NUMBER] and 509 mice were found. On 06/23/2021 for the backyard rats were found and treated. On 06/29/2021 in the kitchen and outer perimeter rodents were found and treated. On 07/06/2021 for the kitchen rodent was found and treated.
1). On 07/08/2021 at 5:05PM during an interview with the Food Service Manager (FSM) in the staff dining area in the basement, near the kitchen, a [NAME] brown colored rodent was observed scurrying between the open lounge area and staff lockers.
On 07/08/2021 at 5:10PM, an interview was conducted with the Food Service Manager The (FSM) stated that due to construction nearby and when it rains rodents come inside the building. The FSM also stated when there are sightings of rodents, they notify the Housekeeping/Maintenance Director. The FSM then retrieved and placed a glue trap on the floor.
On 07/09/2021 at 11:05AM, an interview was conducted with the Director of Housekeeping/Maintenance (DHM). The DHM stated they do pest control rounds with the pest control contractor. The DHM further stated they were informed of the mouse sighting yesterday and this is why the pest control person is here today. Rounds are done once a week in the kitchen and once weekly in the basement. The DHM stated that they receive handwritten reports which are left in the kitchen and they do not see receipts of any of the pest control findings.
On 07/09/2021 at 11:24 AM, an interview was conducted with the Pest Control Contractor (PCC). The PCC stated they come to the facility once a week to set up the traps for the rodents and provides coverage for their partner on occasion. The PCC also stated that due to construction mice move. The PCC further stated that they were unaware of the facility's pest control findings as this would be provided to the facility by the company owner.
415.29(j)(5)