COLUMBUS ALZHEIMER'S CARE CTR




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Columbus Alzheimer's Care Center has a Trust Grade of F, indicating significant concerns about the facility's overall care and management. It ranks #638 out of 913 nursing homes in Ohio, placing it in the bottom half of facilities in the state. The facility is reportedly improving, with the number of issues decreasing from 18 in 2024 to 5 in 2025. Staffing is a relative strength, with a turnover rate of 42% that is below the state average. However, the facility has received concerning fines totaling $26,685, higher than 76% of Ohio facilities, which suggests ongoing compliance problems. Specific incidents raise serious concerns. For example, a resident suffered a femur fracture after being pushed by another resident, indicating a failure to prevent resident-to-resident abuse. Additionally, another incident involved inadequate staffing, where a resident received care from a single aide instead of the required number of staff, resulting in a serious injury. While the facility has areas of strength, such as quality measures, these troubling incidents highlight significant weaknesses that families should consider.
- Trust Score
- F
- In Ohio
- #638/913
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 42% turnover. Near Ohio's 48% average. Typical for the industry.
- Penalties ✓ Good
- $26,685 in fines. Lower than most Ohio facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 33 minutes of Registered Nurse (RN) attention daily — about average for Ohio. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 35 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (42%)
6 points below Ohio average of 48%
Facility shows strength in quality measures, fire safety.
The Bad
Below Ohio average (3.2)
Below average - review inspection findings carefully
Near Ohio avg (46%)
Typical for the industry
Below median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 35 deficiencies on record
Mar 2025
2 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, review of the facility Self-Reported Incidents (SRI), review of the facility investigation, review of fa...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, review of a facility submitted Self-Reported Incident (SRI), hospital record review, interviews ...
Read full inspector narrative →
Jan 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, resident interview, family interview, review of the self-reported misappropriation incident investigat...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and staff interviews the facility failed to ensure call lights were in reach and accessible for resident u...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interviews, review of self-reported incident investigations (SRI) and policy review, the facility failed to ensur...
Read full inspector narrative →
Aug 2024
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, family interview, staff interviews, and policy review the facility failed to make a life insurance polic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on medical record review, staff interview, and review of the facility policy, the failed to ensure staff notified resident physicians of abnormal lab results in a timely manner. This affected on...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, staff interview, policy review, and review of the facility assessment, the facility failed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Record review for Resident #45 revealed an admission date of 07/29/21. Diagnoses included dementia, other specified disorders...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, the facility failed to follow physicians orders in obtaining daily weights. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, record review, resident and staff interview, the facility failed to assist Resident #78 with applying his corrective lenses. This affected one (Resident #78) of two residents rev...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of Resident #01's medical record revealed an admission date of 08/13/21. Medical diagnoses included Alzheimer's diseas...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on medical record review, observation, and staff interview, the facility failed to ensure tube feedings were administered at the rate ordered by the physician. This affected one (Resident #26) o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on medical record review, observation, staff interview, and policy review, the facility failed to ensure residents were free from significant medication errors related to insulin administration....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interviews, and record review, the facility failed to maintain a clean and homelike environment for seven (#18, #26, #35, #44, #78, #90, and #92) residents, all residents were sc...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on medical record review, observation, staff interview, policy review, and review of manufacturer's guidelines, the facility failed to ensure the medication error rate did not exceed five percen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
4. Review of the medical record for Resident #49 revealed an admission date of 05/22/23 with diagnoses including type two diabetes.
Review of the Minimum Data Set (MDS) assessment for Resident #49 da...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0680
(Tag F0680)
Could have caused harm · This affected most or all residents
Based on personnel file review, staff interview and review of a job description, the facility failed to ensure a qualified Activity Director (AD) was in place to oversee the facility's overall activit...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
Based on observation, staff interview, medical record review, policy review, and review of manufacturer's guidelines, the facility failed to ensure medications were labeled and stored appropriately pe...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, staff interview, and review of the facility policy, the facility failed to prevent clean equipment and utensils from contamination, failed to maintain kitchen equipment in operat...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility document review and staff interview, the facility failed to ensure the facility assessment contained all requi...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0843
(Tag F0843)
Minor procedural issue · This affected most or all residents
Based on review of facility documents and staff interview, the facility failed to ensure transfer agreements were in place. This had the potential to affect all residents who reside in the facility. T...
Read full inspector narrative →
Mar 2024
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0729
(Tag F0729)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** THE FOLLOWING DEFICIENCY REPRESENTS AN INCIDENT OF PAST NON-COMPLIANCE THAT WAS SUBSEQUENTLY CORRECTED PRIOR TO THIS SURVEY.
Bas...
Read full inspector narrative →
Feb 2022
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observations, and staff and resident interviews, the facility failed to ensure resident rooms and facili...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review, resident and staff interview, review of the resident council minutes, and policy re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and staff interview, the facility failed to ensure call lights in the bathrooms were functioning properly f...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, staff interview, policy review, and review of the Centers for Disease Control (CDC) guidance and COVID-19 Data Tracker, the facility failed to ensure staff wore personal protecti...
Read full inspector narrative →
Apr 2019
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on review of the medical record and staff interview, the facility failed to ensure the advanced directives were accurate according to the physician's orders and/or code status sheet signed by th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, review of the Institute of Safe Medication Practices and staff interview, the facility nurse failed to meet professional standards during routine medication administration when t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, staff interview, and facility policy review, the facility failed to ensure resident falls were t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation and staff interview, the facility failed to provide routine medications for resident when a medication was not available during medication administration. This affected one (#38) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, the facility failed to provide the appropriate diagnosis for the use of an antipsychotic medication. This affected one (Resident #51) of five reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, record review, staff interview and review of the policy and procedure for medication administration, the facility failed to ensure their medication error rate was less than 5% as...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on record review, observation, staff interviews and review of the facility's policies, the facility failed to ensure the storage of frozen and refrigerated foods in a manner to protect against s...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, staff interview, and facility policy review, the facility failed to follow infection control procedures ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 42% turnover. Below Ohio's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: Federal abuse finding, 2 harm violation(s), $26,685 in fines, Payment denial on record. Review inspection reports carefully.
- • 35 deficiencies on record, including 2 serious (caused harm) violations. Ask about corrective actions taken.
- • $26,685 in fines. Higher than 94% of Ohio facilities, suggesting repeated compliance issues.
- • Grade F (20/100). Below average facility with significant concerns.
About This Facility
What is Columbus Alzheimer'S Care Ctr's CMS Rating?
CMS assigns COLUMBUS ALZHEIMER'S CARE CTR an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Ohio, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Columbus Alzheimer'S Care Ctr Staffed?
CMS rates COLUMBUS ALZHEIMER'S CARE CTR's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 42%, compared to the Ohio average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Columbus Alzheimer'S Care Ctr?
State health inspectors documented 35 deficiencies at COLUMBUS ALZHEIMER'S CARE CTR during 2019 to 2025. These included: 2 that caused actual resident harm, 32 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
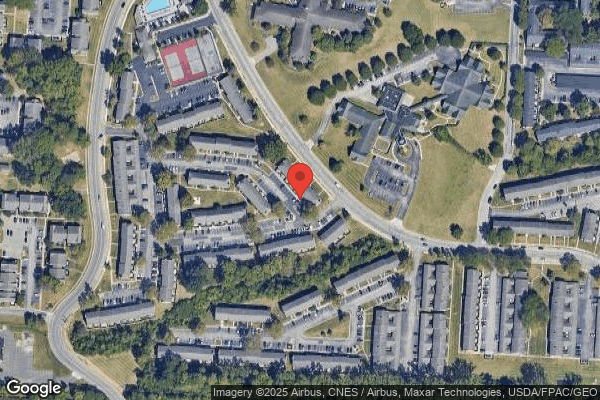
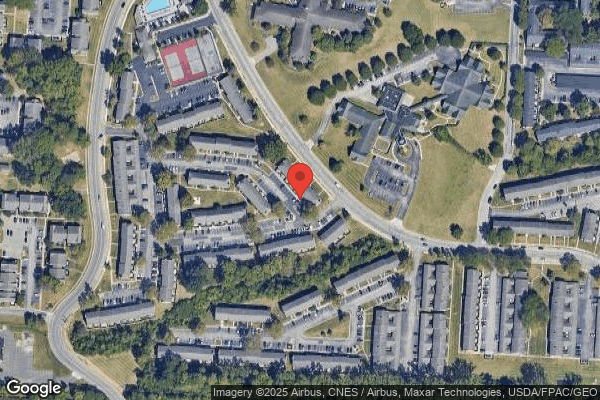
Who Owns and Operates Columbus Alzheimer'S Care Ctr?
COLUMBUS ALZHEIMER'S CARE CTR is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by LIONSTONE CARE, a chain that manages multiple nursing homes. With 99 certified beds and approximately 98 residents (about 99% occupancy), it is a smaller facility located in COLUMBUS, Ohio.
How Does Columbus Alzheimer'S Care Ctr Compare to Other Ohio Nursing Homes?
Compared to the 100 nursing homes in Ohio, COLUMBUS ALZHEIMER'S CARE CTR's overall rating (2 stars) is below the state average of 3.2, staff turnover (42%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Columbus Alzheimer'S Care Ctr?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the substantiated abuse finding on record and the below-average staffing rating.
Is Columbus Alzheimer'S Care Ctr Safe?
Based on CMS inspection data, COLUMBUS ALZHEIMER'S CARE CTR has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Ohio. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Columbus Alzheimer'S Care Ctr Stick Around?
COLUMBUS ALZHEIMER'S CARE CTR has a staff turnover rate of 42%, which is about average for Ohio nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Columbus Alzheimer'S Care Ctr Ever Fined?
COLUMBUS ALZHEIMER'S CARE CTR has been fined $26,685 across 1 penalty action. This is below the Ohio average of $33,346. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Columbus Alzheimer'S Care Ctr on Any Federal Watch List?
COLUMBUS ALZHEIMER'S CARE CTR is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.