GREEN MEADOWS SKILLED NURSING AND REHAB




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Green Meadows Skilled Nursing and Rehab has a Trust Grade of C, indicating that it is average and sits in the middle of the pack among nursing homes. It ranks #473 out of 913 facilities in Ohio, placing it in the bottom half, and #18 out of 33 in Stark County, meaning there are only a few better local options. The facility is currently worsening, with issues increasing significantly from 2 in 2024 to 19 in 2025. Staffing is rated 2 out of 5 stars, which is below average, with a turnover rate of 54%, slightly above the state average, suggesting that staff may not remain long enough to build strong relationships with residents. The facility has concerning fines of $28,763, higher than 76% of facilities in Ohio, which may indicate ongoing compliance problems. Additionally, RN coverage is average, so while there is some oversight, it may not be as strong as in other facilities. Specific incidents of concern include a failure to assess a resident’s acute health changes, leading to multiple falls and a subsequent hospitalization for a urinary tract infection, and a lack of quality assurance meetings, which could affect all residents. Though there are strengths, such as the facility's quality measures rated at 5 out of 5 stars, the weaknesses highlighted by these issues warrant careful consideration from families researching care options.
- Trust Score
- C
- In Ohio
- #473/913
- Safety Record
- Moderate
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 54% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $28,763 in fines. Lower than most Ohio facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 36 minutes of Registered Nurse (RN) attention daily — about average for Ohio. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 47 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Near Ohio average (3.2)
Meets federal standards, typical of most facilities
Near Ohio avg (46%)
Higher turnover may affect care consistency
Below median ($33,413)
Moderate penalties - review what triggered them
The Ugly 47 deficiencies on record
Feb 2025
19 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the closed medical record, review of facility investigation, interview and review of the facility policy the ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of a Self Reported Incident (SRI) with the facility's investigation, policy review, medical record review, and i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the medical record and interview with the staff the facility failed to ensure a Significant Change assessment...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the medical record and interview with the staff the facility failed to ensure the comprehensive assessment ac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of Resident #71's medical record revealed diagnoses including cerebral infarction, type two diabetes mellitus, depress...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observations, interviews, record review, and facility policy review, the facility failed to ensure Resident #55's doorway was free from potential fall hazards. This affected one (#55) residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interviews, record review, manufacturer's instructions, and facility policy review, the facility failed to ensure Resident #42 received nectar thick liquids as ordered. This affe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of the medical record revealed Resident #2 was admitted to the facility on [DATE]. Diagnoses included cerebral infarct...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on record review, review of the facility's dialysis contract, and interview, the facility failed to monitor vital signs and weights before and after dialysis for Residents #52 and #239, and fail...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interviews, and facility policy review, the facility failed to ensure narcotic pain medications were pro...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations, review of the medical record and interview with staff the facility failed to ensure multi-dose insulin pens were dated as to when they were first accessed. This affected three r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0773
(Tag F0773)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, the facility failed to ensure a physician order was written prior to obtaining a l...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 02/03/25 at 1:49 P.M., Resident #71 reported she had problems with constipation and sometimes went four to six days before...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observations, interviews, record reviews, and facility policy, the facility failed to ensure the E wing (memory care unit) was homelike by having a basin on the hallway floor outside of Resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on review of employee files and staff interviews, the facility failed to consistently complete staff evaluations for two Certified Nursing Assistants (CNA). This was identified in two personnel ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected most or all residents
Based on review of Quality Assurance (QA) committee meeting attendance sheets, policy review and interview, the facility failed to ensure a QA meeting was held the first quarter of 2024. This had the ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. During the onsite survey, the following information was obtained:
a.Review of Resident #187's medical record revealed an admi...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0625
(Tag F0625)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the medical record, review of the facility bed hold notices and interview with staff the facility failed to e...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
QAPI Program
(Tag F0867)
Minor procedural issue · This affected most or all residents
Based on policy review and interview, the facility failed to establish comprehensive written policies and procedures related to the Quality Assurance (QA) process. This had the potential to affect all...
Read full inspector narrative →
Oct 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** THE FOLLOWING DEFICIENCY REPRESENTS AN INCIDENT OF PAST NONCOMPLIANCE THAT WAS SUBSEQUENTLY CORRECTED PRIOR TO THIS SURVEY.
Base...
Read full inspector narrative →
Mar 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
THE FOLLOWING DEFICIENCY REPRESENTS AN INCIDENT OF PAST NON-COMPLIANCE THAT WAS SUBSEQUENTLY CORRECTED PRIOR TO THIS SURVEY.
Based on observation, interview, record review, and facility investigation ...
Read full inspector narrative →
Dec 2023
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of resident photographs, facility fall log review, resident medical record review, facility policy review and st...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** THE FOLLOWING DEFICIENCY REPRESENTS AN INCIDENT OF PAST NON-COMPLIANCE THAT WAS SUBSEQUENTLY CORRECTED PRIOR TO THIS SURVEY.
Bas...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** THE FOLLOWING DEFICIENCY REPRESENTS AN INCIDENT OF PAST NON-COMPLIANCE THAT WAS SUBSEQUENTLY CORRECTED PRIOR TO THIS SURVEY.
Bas...
Read full inspector narrative →
Sept 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, record review, and pharmacy dispensing records the facility failed to implement a gradual dose reducti...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview the facility failed to ensure the comprehensive Minimum Data Set (MDS) 3.0 assessment...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, staff interview, and staff education, the facility failed to document why as needed pain medications wer...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure fall prevention interventions were in place as ordered for R...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to establish home health services for Resident #405 to ensure a safe a...
Read full inspector narrative →
Oct 2022
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on facility self reported incident review, resident interview, medical record review and staff interview. The facility failed to ensure residents were treated with dignity and respect by staff m...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Based on medical record review, electronic narcotic dispense records, policy review, schedule review and staff interview, the facility failed to ensure narcotic medications were dispensed appropriatel...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify the resident and resident's representative in writing of the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify the resident and/or the resident's representative of the fac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0646
(Tag F0646)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of the medical record revealed Resident #64 was admitted to the facility on [DATE]. Diagnoses included quadriplegia, p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on resident interview, observation, medical record review and staff interview, the facility failed to ensure residents dependent upon staff assistance with meals were provided assistance as indi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to reassess and implement interventions for Resident #8's...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, policy review, review of pharmacy delivery records, and interview, the facility failed to ensure...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, record and activity calendar review, the facility failed to provide an ongoing activities pro...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0741
(Tag F0741)
Could have caused harm · This affected multiple residents
Based on observations, interviews, review of activity calendars, review of staffing patterns and review of the facility assessment, the facility failed to have sufficient quantity of staff to provide ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, medical record review, interview, and review of product information, the facility failed to properly disinfect equipment being removed from a resident's room who had a diagnosis ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected most or all residents
Based on interview and review of personnel files, the facility failed to ensure employees did not have a finding entered into the State of Ohio Nurse Aide Registry. This had the potential to affect al...
Read full inspector narrative →
Oct 2019
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to timely implement the restorative nursing programs (RNP) for Resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review, resident interview, family interview, facility policy review and staff interview, t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, policy review, and interview, the facility failed to ensure a fall intervention was in place for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure a comprehensive and individualized bladder program was in pla...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure the antibiotic stewardship program was implemented for Reside...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, policy review, manufacturer guidelines review, and interview, the facility failed to properly sanitize a glucometer. This had the potential to affect five of five residents (Resi...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • 47 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $28,763 in fines. Higher than 94% of Ohio facilities, suggesting repeated compliance issues.
- • Grade C (50/100). Below average facility with significant concerns.
About This Facility
What is Green Meadows Skilled Nursing And Rehab's CMS Rating?
CMS assigns GREEN MEADOWS SKILLED NURSING AND REHAB an overall rating of 3 out of 5 stars, which is considered average nationally. Within Ohio, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Green Meadows Skilled Nursing And Rehab Staffed?
CMS rates GREEN MEADOWS SKILLED NURSING AND REHAB's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 54%, compared to the Ohio average of 46%.
What Have Inspectors Found at Green Meadows Skilled Nursing And Rehab?
State health inspectors documented 47 deficiencies at GREEN MEADOWS SKILLED NURSING AND REHAB during 2019 to 2025. These included: 1 that caused actual resident harm, 44 with potential for harm, and 2 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Green Meadows Skilled Nursing And Rehab?
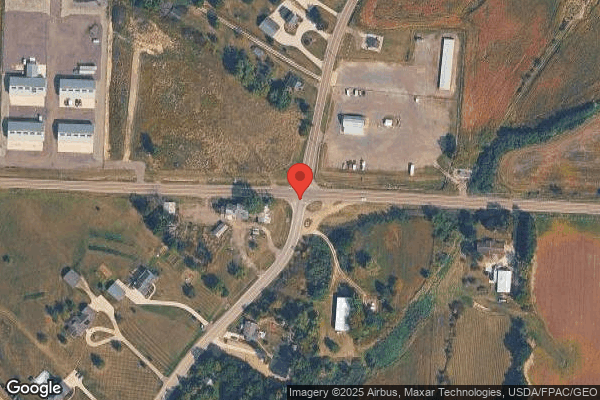
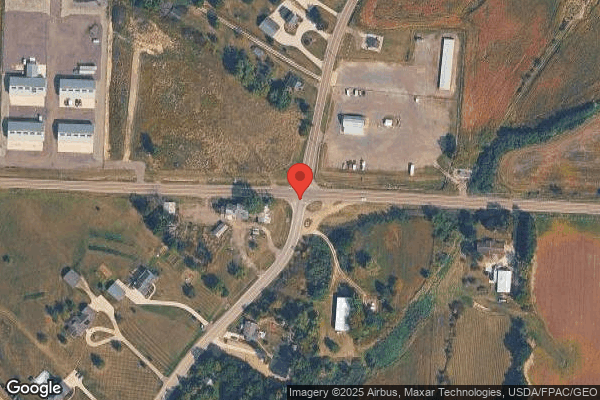
GREEN MEADOWS SKILLED NURSING AND REHAB is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 110 certified beds and approximately 89 residents (about 81% occupancy), it is a mid-sized facility located in LOUISVILLE, Ohio.
How Does Green Meadows Skilled Nursing And Rehab Compare to Other Ohio Nursing Homes?
Compared to the 100 nursing homes in Ohio, GREEN MEADOWS SKILLED NURSING AND REHAB's overall rating (3 stars) is below the state average of 3.2, staff turnover (54%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Green Meadows Skilled Nursing And Rehab?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Green Meadows Skilled Nursing And Rehab Safe?
Based on CMS inspection data, GREEN MEADOWS SKILLED NURSING AND REHAB has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in Ohio. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Green Meadows Skilled Nursing And Rehab Stick Around?
GREEN MEADOWS SKILLED NURSING AND REHAB has a staff turnover rate of 54%, which is 7 percentage points above the Ohio average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Green Meadows Skilled Nursing And Rehab Ever Fined?
GREEN MEADOWS SKILLED NURSING AND REHAB has been fined $28,763 across 1 penalty action. This is below the Ohio average of $33,366. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Green Meadows Skilled Nursing And Rehab on Any Federal Watch List?
GREEN MEADOWS SKILLED NURSING AND REHAB is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.