Crestwood Care Center




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Crestwood Care Center has received a Trust Grade of F, indicating significant concerns with the quality of care provided. Ranked #856 out of 913 facilities in Ohio, this places them in the bottom half, and at #8 out of 10 in Richland County, only one local option ranks lower. While the facility's trend is improving-issues decreased from 25 in 2024 to 16 in 2025-the overall situation remains troubling, with 77 deficiencies found, including four critical incidents related to inadequate supervision and medication errors. Staffing is rated below average at 2 out of 5 stars, with a turnover rate of 52%, which is average for Ohio, but they have less RN coverage than 91% of state facilities, potentially affecting resident care. Additionally, the facility faces concerning fines totaling $232,204, indicating repeated compliance problems, and specific incidents reveal serious issues, such as a resident being pushed to the floor during an altercation due to a lack of supervision and staff failing to administer medications as ordered.
- Trust Score
- F
- In Ohio
- #856/913
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 52% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $232,204 in fines. Lower than most Ohio facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 20 minutes of Registered Nurse (RN) attention daily — below average for Ohio. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 77 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Ohio average (3.2)
Significant quality concerns identified by CMS
Near Ohio avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 77 deficiencies on record
Mar 2025
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0620
(Tag F0620)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, admission agreement review, and interview the facility failed to ensure the consent to treat was signed ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interview, and facility policy review the facility failed to ensure wound treatment orders were obtained...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interview, and policy review the facility failed to ensure pressure ulcer wound treatment orders were ob...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, review of the late administration medication report, interview, and facility policy review the facility ...
Read full inspector narrative →
Feb 2025
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff and resident interview, medical record review, and review of facility policy, the facility failed to ensure perso...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, review of facility policy, and record review, the facility failed to ensure baseline care plans were d...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of the medical record for Resident #79 revealed an admission date of 11/13/24 with diagnoses including diabetes mellit...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the medical record, observation, resident and staff interview, and policy review, the facility failed to ensu...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the medical record, observation, staff interview, and policy review, the facility failed to ensure the reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review, staff interview and review of facility policy, the facility failed to ensure oxygen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on resident and staff interviews, record review, and review of facility policy, the facility failed to monitor weights and vital signs before and after dialysis and maintain adequate communicati...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident and staff interview, medical record review, and facility policy review, the facility failed to en...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, resident and staff interview, and policy review, the facility failed to ensure that residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of the medical record for Resident #54 revealed an admission date of 09/13/23. Diagnoses included type II diabetes mel...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, review of facility policy, and staff interviews, the facility failed to ensure clean food service areas and beard restraints were worn during food preparation. This had the pote...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0730
(Tag F0730)
Minor procedural issue · This affected most or all residents
Based on record review and staff interview, the facility failed to ensure annual performance evaluations were completed as required for certified nursing assistants (CNAs). This affected three of thre...
Read full inspector narrative →
Dec 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, record reviews, and policy review, the facility failed to ensure resident's advance directives were readily...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on resident and staff interviews, record review and observation, the facility failed to ensure Resident #78's continuity of care was reviewed and implemented timely. This affected one (#78) of t...
Read full inspector narrative →
Sept 2024
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, resident and staff interviews, and policy review, the facility failed to provide effective pain ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, resident and staff interviews and policy review, the facility failed to timely inform and allow ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0742
(Tag F0742)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, staff interviews, and review of the facility policy, the facility failed to timely implement eff...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on record review and staff interview, the facility failed to ensure a Registered Nurse (RN) was on duty for eight consecutive hours each day, seven days a week. This had the potential to affect ...
Read full inspector narrative →
May 2024
6 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, staff and resident interview, record review and policy review, the facility failed to ensure timely and appropriate incontinence care was provided for a resident. This affected o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, record review, interview, and policy review, the facility failed to ensure physician-ordered treatments were applied as ordered. This affected two (Residents #45 and #50) of thre...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
Based on staff interview, record review, and policy review, the facility failed to ensure physician-ordered laboratory testing was completed timely. This affected one (Resident #100) of three resident...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected multiple residents
Based on observation, interview, record review, policy review, and self reported incident (SRI) review, the facility failed to report, investigate and document allegations of resident-to-resident abus...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on record review, staff and resident interview, policy review, and self-reported incidents (SRI) review, the facility failed to maintain accurate resident records. This affected four (Residents ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on record review and interview, the facility failed to ensure a Registered Nurse (RN) was on duty for eight consecutive hours each day, seven days a week. This had the potential to affect all re...
Read full inspector narrative →
Apr 2024
5 deficiencies
1 IJ (1 affecting multiple)
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0760
(Tag F0760)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, resident and staff interview, and review of a facility policy, the facility failed to ensure med...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on medical record review, review of a self-reported incident, staff interview, and policy review, the facility failed to ensure residents were free from improper physician restraints. This affec...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review, staff interview, and policy review, the facility failed to ensure medications were ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and resident and staff interviews, the facility failed to ensure medication administration was ac...
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on observation, staff interview, and policy review, the facility failed to maintain daily posted nurse staffing data as required. This had the potential to affect all 104 residents residing in t...
Read full inspector narrative →
Mar 2024
6 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff, resident, and family interviews, record review, policy review, and review of a local police report,...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0712
(Tag F0712)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff and resident interviews, record review, and policy review, the facility failed to ensure physician visits were co...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected most or all residents
Based on record review, staff interview, and review of facility policy, the facility failed to ensure implementation of their abuse policy and obtain an employee background check was completed for Cul...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected most or all residents
Based on interview, observation, and policy review, the facility failed to serve foods at the appropriate temperatures. The had the potential to affect all residents that resided in the facility as th...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0942
(Tag F0942)
Could have caused harm · This affected most or all residents
Based on record review, review of personnel records, and staff interview the facility failed to provide training on the rights of the residents to the staff. This affected three (Licensed Practical Nu...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected most or all residents
Based on record review, review of personnel records, and staff interviews, the facility failed to provide abuse, neglect, exploitation and misappropriation of resident property training for staff. Thi...
Read full inspector narrative →
Jan 2024
2 deficiencies
2 IJ (1 facility-wide)
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, review of open and closed medical records, hospital record review, review of self-reported incidents (SRI)...
Read full inspector narrative →
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
Based on observation, record review, job description review, staff interviews and policy review, the facility failed ensure it was administered in a manner that enabled it to use its resources effecti...
Read full inspector narrative →
Nov 2023
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on medication storage observation, medical record review, staff interview, and review of a facility policy, the facility failed to ensure controlled substances and narcotic medication were dispo...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected most or all residents
Based on resident interview, staff interview, medical record review, review of food committee minutes, and policy review, the facility failed to ensure snacks were available in the evening and at bed ...
Read full inspector narrative →
Oct 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident interview, facility staff interview, the facility failed to provide a clean and sanitary environm...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, resident interview, staff interview, and policy review, the facility failed to maintain the...
Read full inspector narrative →
Apr 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, staff interview, and policy review, the facility failed to administer medications to reside...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, staff interview, and policy review, the facility failed to maintain proper infection control practices during medication administration to Resident #15 and failed to cleanse the ...
Read full inspector narrative →
Feb 2023
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, staff interview, review of the fall evaluation, and review of the staff schedules, ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, the facility failed to ensure accuracy of the minimum data set (MDS) assessm...
Read full inspector narrative →
Jan 2023
9 deficiencies
1 IJ (1 affecting multiple)
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, review of medical records, Self-Reported Incidents (SRI) review, witness statement review, staff schedule...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and records review, the facility failed to maintain a safe and comfortable temperature. This ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on Self-Reported Incident (SRI) review, witness statement review, police call report review, policy review and interview, the facility failed to accurately notify the local law enforcement agenc...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, Self-Reported Incident (SRI) review, policy review and interviews, the facility failed to comple...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to timely acquire a prescribed medication for one residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure appropriate infection control precautions during the provision of personal care. This affected one (Resident #50) of four residents re...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on observation, medical record review, staff schedule review and interview, the facility failed to ensure sufficient staff for an ordered one-to-one staff monitoring of Residents #81 and #98. Th...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to properly secure the medication storage room on Unit One. This had the potential to affect nine (Residents #2, #3, #12, #14, #19, #26, #27, #3...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected most or all residents
Based on observations, review of medical records, Self-Reported Incidents (SRI) review, witness statement review, staff schedule review, police call report review, review of the Centers for Medicare a...
Read full inspector narrative →
Nov 2022
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the facility's Self-Reported Incidents (SRI) and corresponding investigation, staff interview, medical record...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, the facility failed to ensure cognition and mood were assessed on the compre...
Read full inspector narrative →
Sept 2022
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, review of the facility policy, and family and staff interviews, the facility failed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interviews, the facility failed to provide written notification to a resident and/or re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of medical record for Resident #56 revealed an admission date of 07/19/17. Diagnoses included acute gastroenteropathy,...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of the medical record for Resident #38 revealed an admission date of 11/06/20. Diagnoses included hemiplegia and hemip...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, resident and staff interview, review of the facility policy, and record review, the facility failed to en...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident and staff interview and record review, the facility failed to ensure residents received timely treatment and c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on medical record review, review of facility anti-psychotic dose reduction/elimination records, and staff interviews, the facility failed to ensure a resident was not receiving an anti-psychotic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0773
(Tag F0773)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, observation, and record review, the facility failed to ensure a resident's urine sample for a urine an...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, the facility failed to ensure a resident was free from unnecessary antibiotic use. This affected one (Resident #5) of six residents reviewed for unn...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected most or all residents
Based on observation, review of the facility policy, and resident and staff interviews, the facility failed to serve food at a safe and palatable temperature. This had the potential to affect all 101 ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, staff interview, and policy review, the facility failed to store dishware appropriately for food service safety and follow the facility's warewashing procedures. This had the pot...
Read full inspector narrative →
Oct 2019
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observations, and staff interview, the facility failed to ensure fall interventions were in plac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, and staff interview, the facility failed to ensure oxygen therapy was completed as ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, resident interview, staff interview, and review of antibiotic stewardship policy, the facility f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observations and staff interview, the facility failed to communicate a resident's behavior to ho...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, the facility failed to ensure resident care plans were updated. This affecte...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, staff interview and facility policy review, the facility failed to ensure medication carts were maintained secured. This had the potential to affect 18 residents (#10, #12, #13, ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 4 life-threatening violation(s), Special Focus Facility, 2 harm violation(s), $232,204 in fines, Payment denial on record. Review inspection reports carefully.
- • 77 deficiencies on record, including 4 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $232,204 in fines. Extremely high, among the most fined facilities in Ohio. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Crestwood Care Center's CMS Rating?
CMS assigns Crestwood Care Center an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Ohio, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Crestwood Care Center Staffed?
CMS rates Crestwood Care Center's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 52%, compared to the Ohio average of 46%. RN turnover specifically is 81%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Crestwood Care Center?
State health inspectors documented 77 deficiencies at Crestwood Care Center during 2019 to 2025. These included: 4 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 2 that caused actual resident harm, 69 with potential for harm, and 2 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Crestwood Care Center?
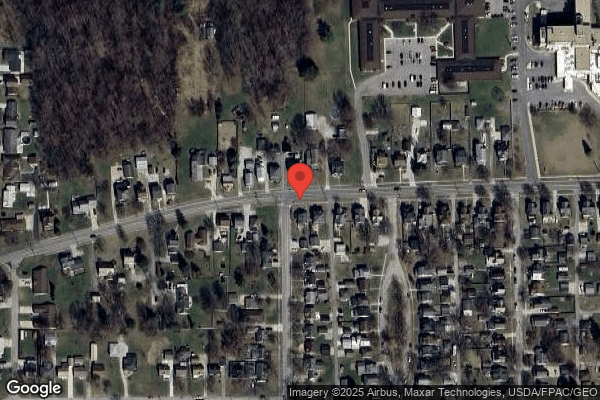
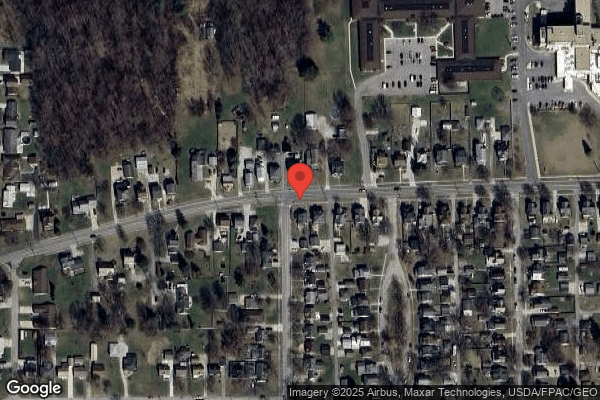
Crestwood Care Center is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by COMMUNICARE HEALTH, a chain that manages multiple nursing homes. With 130 certified beds and approximately 84 residents (about 65% occupancy), it is a mid-sized facility located in SHELBY, Ohio.
How Does Crestwood Care Center Compare to Other Ohio Nursing Homes?
Compared to the 100 nursing homes in Ohio, Crestwood Care Center's overall rating (1 stars) is below the state average of 3.2, staff turnover (52%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Crestwood Care Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Crestwood Care Center Safe?
Based on CMS inspection data, Crestwood Care Center has documented safety concerns. Inspectors have issued 4 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility is currently on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes nationwide). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Ohio. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Crestwood Care Center Stick Around?
Crestwood Care Center has a staff turnover rate of 52%, which is 5 percentage points above the Ohio average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Crestwood Care Center Ever Fined?
Crestwood Care Center has been fined $232,204 across 2 penalty actions. This is 6.6x the Ohio average of $35,401. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Crestwood Care Center on Any Federal Watch List?
Crestwood Care Center is currently an SFF Candidate, meaning CMS has identified it as potentially qualifying for the Special Focus Facility watch list. SFF Candidates have a history of serious deficiencies but haven't yet reached the threshold for full SFF designation. The facility is being monitored more closely — if problems continue, it may be added to the official watch list. Families should ask what the facility is doing to address the issues that led to this status.