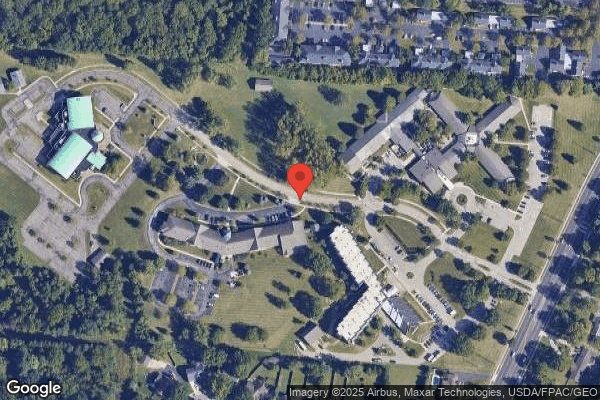
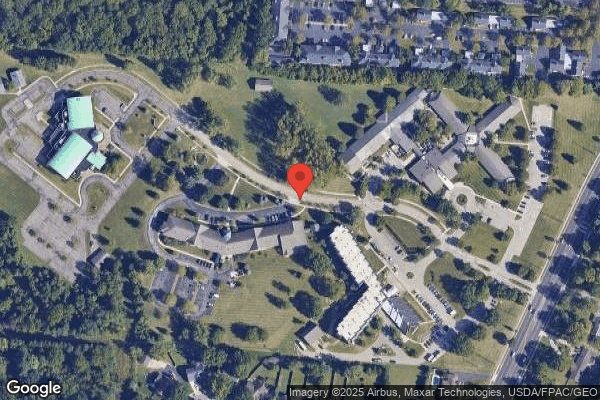
Inniswood Health and Rehabilitation




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Inniswood Health and Rehabilitation in Westerville, Ohio has received a Trust Grade of F, indicating significant concerns about the facility. Ranked #705 out of 913 in Ohio, they are in the bottom half of nursing homes in the state, and #33 out of 56 in Franklin County, meaning only a few local options are better. Although the facility's trend is improving, with issues decreasing from 19 in 2024 to just 2 in 2025, the high fines of $169,562, which are greater than 94% of Ohio facilities, raise red flags regarding compliance problems. Staffing is a weak point, with only 1 out of 5 stars and no turnover, but they do have more RN coverage than 78% of Ohio facilities, which is a positive aspect since RNs can catch issues that other staff might miss. Specific incidents, such as a resident losing significant weight without timely re-assessment and another resident developing a serious pressure ulcer due to inadequate care, highlight critical areas of concern despite some strengths in staffing stability.
- Trust Score
- F
- In Ohio
- #705/913
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ✓ Good
- $169,562 in fines. Lower than most Ohio facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 41 minutes of Registered Nurse (RN) attention daily — about average for Ohio. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 55 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Ohio average (3.2)
Below average - review inspection findings carefully
Well above median ($33,413)
Significant penalties indicating serious issues
The Ugly 55 deficiencies on record
Jan 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, review of facility self-reported incidents (SRI's), medical record review and review of facility polic...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, review of facility self-reported incidents (SRI's), medical record review, and review of facility poli...
Read full inspector narrative →
Aug 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, medication administration observation, staff interviews, and medication administration policy re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medication administration observation, staff interview and facility policy review, this facility failed to ensure infec...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observations, staff interview, and facility policy review, this facility failed to ensure medication carts were locked at all times unless in use and under direct observation of the medicatio...
Read full inspector narrative →
Feb 2024
16 deficiencies
1 IJ
CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0692
(Tag F0692)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #49 was admitted to the facility on [DATE] with diagnoses including displaced intertrochanteric fracture of right fe...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review, interviews and facility policy review, the facility failed to implement adequate sk...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, staff interview, hospital records review, Hoyer Lift user manual review and facility policy review, the ...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interviews and facility policy review, the facility failed to provide adequate pain management for Resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on medical record review and staff interview the facility failed to ensure Minimum Data Set (MDS) assessments were accura...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, the facility failed to ensure Pre-admission Screening and Resident Review (PASARR) w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, the facility failed to ensure the preadmission screening and record review (...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0646
(Tag F0646)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, the facility failed to notify the state mental health agency of significant ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview the facility failed to ensure a self-releasing wheelchair seatbelt was only us...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to follow a physician ordered fluid restriction for Resident #55, who r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure medication monitoring was completed for the use of antipsych...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interviews and facility policy review, the facility failed to ensure one resident's (#32) physician orde...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation and staff interviews, the facility failed to ensure residents were not served food past the use-by date. This had the potential to affect 82 of 82 residents who receive food from ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, the facility failed to maintain hospice documentation on-site for resident c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide evidence of education and administration of pneumonia immun...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected most or all residents
Based on observation, record review and staff interview the facility failed to maintain effective pest management. This had the potential to affect all 83 residents.
Findings include:
Observation on 0...
Read full inspector narrative →
Jan 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0712
(Tag F0712)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, the facility failed to ensure physician visits were alternated with the nurse practitioner every 60 days as required. This affected three of three s...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected most or all residents
Based on review of employee personnel files, policy review, and staff interview, the facility failed to implement the abuse policy related to screening of new employees. This occurred with nine of nin...
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Deficiency F0843
(Tag F0843)
Minor procedural issue · This affected most or all residents
Based on review of transfer agreements and staff interview, the facility failed to have a written transfer agreement with a hospital approved for participation under the Medicare and Medicaid program....
Read full inspector narrative →
Jan 2022
15 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
Based on observation, record review, facility policy and procedure review and interview the facility failed to implement interventions to prevent the development of a pressure ulcer for Resident #82. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, record review, facility policy and procedure review and interview the facility failed to provide Resident #35 with dignity and respect related to the use of an indwelling urinary...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, facility policy and procedure review and interview the facility failed to ensure Resident #387, who pres...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview the facility failed to ensure Resident #8, who required staff assistance from staff for personal hygiene received timely and adequate assistance with ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of Resident #387's medical record revealed the resident was discharged to the hospital on [DATE] and returned on 01/07...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of the medical record for Resident #42 revealed the resident was admitted to the facility on [DATE] with diagnoses tha...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
3. Review of the medical record for Resident #54 revealed an admission date of 08/16/21 with diagnoses including chronic obstructive pulmonary disease, depression, emphysema, osteoarthritis, foot drop...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to ensure an as needed (PRN) psychoactive medication for Resident #54 was limited to 14 days or continued only with an evaluation by the physic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, facility policy and procedure review and interview the facility failed to maintain a medica...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Review of the medical record for Resident #34 revealed an admission date of 08/02/21 with diagnoses including hemiplegia and ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on record review, staff interview, review of Food and Drug Administration (FDA)
information, review of a HealthDay News Study and facility policy and procedure review, the facility failed to pro...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 6. On 01/25/22 at 8:25 A.M. observation of room [ROOM NUMBER] revealed a dent and hole the size of a tennis ball on the wall beh...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, facility policy and procedure review and interview facility failed to properly store food items in the dry storage, refrigerator and freezer locations to prevent contamination, s...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, facility census review, review of the Centers for Disease and Prevention (CDC) guidance, facility policy and procedure review and interview the facility failed to ensure N95 mask...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Abuse Prevention Policies
(Tag F0607)
Minor procedural issue · This affected most or all residents
Based on personnel record review, facility policy and procedure review and staff interview the facility failed to develop and implement comprehensive abuse, neglect, exploitation of residents and misa...
Read full inspector narrative →
Apr 2019
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on medical record review, observation, and staff interview the facility failed to ensure all resident call lights were within reach. This affected one (Resident #82) out of one resident reviewed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to ensure there was no discrepancy regarding Resident #18's Advance Dir...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review, interview, and review of policy and procedure the facility failed to ensure Resident #82's physician was notified regarding significant weight loss. This affected one (Resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation and staff interview the facility failed to ensure resident rooms and wheel chairs were maintained in good repair. This affected one (Resident #54) of six residents reviewed for en...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview the facility failed to complete a significant change Minimum Data Set assessm...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview the facility failed to identify and address a significant decline in a reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, and staff interview the facility failed to ensure a resident received adequate supe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, policy review, and staff interview the facility failed to ensure a resident received needed serv...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interview, and review of policy and procedure the facility failed to address fluctuating weights for Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation, staff interview, and policy review the facility failed to ensure a resident's pain was adeq...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview the facility failed to ensure regular communication with the contracted dialy...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected multiple residents
Based on review of resident personal funds accounts, policy review, and staff interview the facility failed to ensure interest was applied to the accounts of residents, who were on Medicaid, with a ba...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, staff interview and policy review, the facility failed to ensure after food items were opened they were dated and paper towels were available at the hand washing sink. This had t...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation and staff interview, the facility the facility failed to dispose of trash properly. This had the potential to affect all 138 residents residing in the facility.
Findings include:
...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
Based on review of the Quality Assurance Performance Improvement (QAPI) plan and staff interview, the facility failed to develop an individualized QAPI plan for the facility. This had the potential to...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, staff interview and policy review, the facility failed to ensure staff followed proper hand hygiene and failed to ensure dust was not blowing over clean clothing. This had the po...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s), 4 harm violation(s), $169,562 in fines. Review inspection reports carefully.
- • 55 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $169,562 in fines. Extremely high, among the most fined facilities in Ohio. Major compliance failures.
- • Grade F (3/100). Below average facility with significant concerns.
About This Facility
What is Inniswood Health And Rehabilitation's CMS Rating?
CMS assigns Inniswood Health and Rehabilitation an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Ohio, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Inniswood Health And Rehabilitation Staffed?
CMS rates Inniswood Health and Rehabilitation's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes.
What Have Inspectors Found at Inniswood Health And Rehabilitation?
State health inspectors documented 55 deficiencies at Inniswood Health and Rehabilitation during 2019 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 4 that caused actual resident harm, 48 with potential for harm, and 2 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Inniswood Health And Rehabilitation?
Inniswood Health and Rehabilitation is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 99 certified beds and approximately 73 residents (about 74% occupancy), it is a smaller facility located in WESTERVILLE, Ohio.
How Does Inniswood Health And Rehabilitation Compare to Other Ohio Nursing Homes?
Compared to the 100 nursing homes in Ohio, Inniswood Health and Rehabilitation's overall rating (2 stars) is below the state average of 3.2 and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Inniswood Health And Rehabilitation?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Inniswood Health And Rehabilitation Safe?
Based on CMS inspection data, Inniswood Health and Rehabilitation has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Ohio. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Inniswood Health And Rehabilitation Stick Around?
Inniswood Health and Rehabilitation has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Inniswood Health And Rehabilitation Ever Fined?
Inniswood Health and Rehabilitation has been fined $169,562 across 1 penalty action. This is 4.9x the Ohio average of $34,774. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Inniswood Health And Rehabilitation on Any Federal Watch List?
Inniswood Health and Rehabilitation is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.