DIXON HEALTHCARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Dixon Healthcare Center in Wintersville, Ohio, has received a Trust Grade of F, indicating significant concerns about its care quality. It ranks #662 out of 913 in Ohio, placing it in the bottom half of nursing facilities, and #3 out of 6 in Jefferson County, meaning only two local options are worse. The facility is trending toward improvement, having reduced issues from 30 in 2024 to 20 in 2025, but it still faces serious challenges. Staffing is rated 2 out of 5 stars, with a turnover rate of 51%, which is average but suggests instability. Notably, the facility has incurred $144,718 in fines, which is higher than 94% of Ohio facilities, indicating ongoing compliance issues. There have been critical incidents leading to resident deaths due to neglect, such as a failure to provide timely care and necessary medical interventions. For example, one resident did not receive prescribed medications and lab tests after returning from the hospital, while another experienced a decline in health without adequate assessment or communication to medical staff. On a positive note, the facility has good RN coverage, being better than 89% of similar facilities, which helps address potential problems. However, families should weigh these strengths against the serious weaknesses highlighted by the recent inspector findings.
- Trust Score
- F
- In Ohio
- #662/913
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 51% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $144,718 in fines. Lower than most Ohio facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 48 minutes of Registered Nurse (RN) attention daily — more than average for Ohio. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 85 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Ohio average (3.2)
Below average - review inspection findings carefully
Near Ohio avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 85 deficiencies on record
Jul 2025
8 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on closed medical record review, review of hospital records, review of Medscape medical reference information, policy revi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, review of self-reported incidents (SRI), interviews, and policy review, the facility failed to p...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, interview, and facility policy review, the facility failed to timely investigate an...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, and interviews, the facility failed to ensure that adequate care and treatment was ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, interview, and policy review the facility failed to ensure residents received effective pain man...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, interview, and policy review the facility failed to ensure narcotic medication (pain patches) we...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected multiple residents
Based on observation, interview, review of funds list, and policy review, the facility failed to ensure residents had access to personal funds after business hours and on weekends. This affected four ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected most or all residents
Based on review of pest invoices, review of concerns submitted to the state survey agency complaint intake unit, interviews, observation, and review of facility policy revealed the facility failed to ...
Read full inspector narrative →
Jun 2025
8 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Quality of Care
(Tag F0684)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on closed medical record review, facility policy and procedure review, and interview, the facility failed to provide timel...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review, interview and policy review, the facility failed to notify a family and physician of a resident fall. This affected one resident (#64) of three residents reviewed for falls.
Fi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, hospice communication review, and interview, the facility failed to ensure a resident who was dependent ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, Sheriff report review, interview, and policy review, the facility failed to ensure resident needs were m...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0712
(Tag F0712)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interview, and policy review the facility failed to provide evidence the physician conducted in-person e...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review, and staff interview, the facility failed to maintain accurate resident medical records. T...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review, and interview, the facility failed to ensure contact isolation precautions were implement...
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Deficiency F0565
(Tag F0565)
Minor procedural issue · This affected most or all residents
Based on review of Resident Council minutes, policy review, staff interview, and resident interview the facility failed to ensure Resident Council concerns were addressed in a timely manner. This had ...
Read full inspector narrative →
Mar 2025
4 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on closed medical record review, review of hospital records, review of an emergency medical service (EMS) report and EMS s...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the medical record, review of facility Self Reported Incidents, review of facility investigation, interview w...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the medical record, interview with staff, and review of facility policy and procedure, the facility failed to...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, review of the medical record, interview with staff, and review of manufacture guidelines, the facility fa...
Read full inspector narrative →
Dec 2024
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of the medical record revealed Resident #45 was admitted to the facility on [DATE]. Diagnoses included hypokalemia, bu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review revealed Resident #34 was admitted to the facility on [DATE] with diagnoses including chronic kidney disease, a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on closed record review and interview the facility failed to ensure a discharge summary (recapitulation of stay, final sum...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, medical record review, and policy review, the facility failed to ensure Resident #73 received timely and app...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on closed record review, interview, and policy review the facility failed to ensure pressure ulcer treatments were complet...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff and resident interview, record review, and policy review, the facility failed to ensure restorative ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, policy review, and interview the facility failed to maintain hot water temperatures in a safe manner to prevent potential accident/resident burns. This affected two (Residents #1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, and interview the facility failed to ensure residents were adequately assessed and ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on closed medical record review, and interview the facility failed to ensure residents were provided a comprehensive and i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
Based on Ombudsman interview, resident interview, medical record review and staff interview, the facility failed to provide timely assistance to Resident #56 to obtain state photo identification. This...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, the facility failed to Resident #73 was free from significant medication err...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the medical record and interview with staff, the facility failed to ensure a pneumonia vaccine was given to R...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and policy review the facility failed to maintain water temperatures in a manner to ensure resi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of the medical record for Resident #37 revealed an admission date of 9/17/19. Diagnoses include acute respiratory fail...
Read full inspector narrative →
Oct 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, hospice provider self-reported incident review, review of a facility self-reported incident inve...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** THE FOLLOWING DEFICIENCY REPRESENTS AN INCIDENT OF PAST NON-COMPLIANCE THAT WAS SUBSEQUENTLY CORRECTED PRIOR TO THIS SURVEY.
Bas...
Read full inspector narrative →
Aug 2024
2 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** THE FOLLOWING DEFICIENCY REPRESENTS AN INCIDENT OF PAST NON-COMPLIANCE THAT WAS SUBSEQUENTLY CORRECTED PRIOR TO THIS SURVEY.
Bas...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, self-reported incident review, and staff interview the facility failed to timely report an allegation of...
Read full inspector narrative →
Jul 2024
7 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure new interventions were attempted to prevent recurring urinar...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0800
(Tag F0800)
Could have caused harm · This affected 1 resident
Based on menu review, dislike list, interviews, and photo, the facility failed to ensure a nourishing, palatable well balanced diet was served. This affected one resident (#6) of three residents revie...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, activity calendar review, and record review, the facility failed to ensure residents right to self determina...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0576
(Tag F0576)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure resident mail and packages was delivered unopened and on the weekends. This affected three residents (#2, #6 and #7).
Findings include...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected most or all residents
Based on observation, interview, and test tray, the facility failed to serve palatable chicken. This had the potential to affect all the residents in the facility except two residents (#36, #69) who d...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected most or all residents
Based on interview, observation, and invoice review, the facility failed to ensure the facility was administered in a manner to enable it to use its resources effectively to maintain the highest pract...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, policy review, and interview, the facility failed to ensure sanitary pericare technique and availability of soap in the kitchen at the handwashing sink. This affected one residen...
Read full inspector narrative →
Mar 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on medical record review, review of administration detail report, interviews, and policy review the facility failed ensure a resident received pain medication as ordered. This affected one (Resi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review, review of narcotic control sheet, review of administration detail report, interview, and policy review the facility failed to ensure medication administration was accurately do...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
Based on medical record review, observation, interview, and policy review the facility failed to ensure medications were properly stored and secured. This affected Resident #24 with the potential to a...
Read full inspector narrative →
Jan 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation and interview, the facility failed to develop and implement a comprehensive and individualiz...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and interview with the staff the facility failed to maintain a sanitary kitchen. This affected all residents but two residents ( Resident #29 and #63) who did not receive food fro...
Read full inspector narrative →
Dec 2023
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interview, and policy review, the facility failed to ensure residents were adequately protected from abu...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to initiate a recommended restorative program to promote maintenance o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview, the facility failed to ensure treatments/interventions were applied according...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observations, medical record review and interview, the facility failed to obtain a wound culture in accordance with orders. This affected one (Resident #75) of four residents reviewed for wou...
Read full inspector narrative →
Oct 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure Resident #13's oxygen tubing and humidifier bo...
Read full inspector narrative →
Aug 2023
19 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, and facility policy review, the facility failed to ensure advanced directives were accurately...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, and facility policy review, the facility failed to ensure residents were sufficiently prepare...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0646
(Tag F0646)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, and facility policy review, the facility failed to ensure a Resident's Preadmission Screening...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, review of the facility's activity calendar, observation, resident interview, staff interview, and policy...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, review of facility elopement documentation, and facility policy review, the facility failed t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and facility policy review, the facility failed to ensure confirmation of PEG (percutaneous end...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation, staff interview, and policy review, the facility failed to ensure a resident with a tracheo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review, and interview, the facility failed to provide medically related social services to ensure...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, the facility failed to ensure medications ordered on an as needed (prn) basis for hy...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, and facility policy review, the facility failed to ensure psychotropic medications were used ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and facility policy review, the facility failed to ensure they were free from a medication erro...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to insure a clean, comfortable and homelike environment. This affected ten residents (#1, #7, #12, #15, #21, #39, #56, #60, #115 ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review, and interview, the facility failed to ensure an accurate Level I Pre-admission Screening/...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of Resident #39's medical record revealed he was admitted to the facility on [DATE] with diagnoses including hypertens...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review, and interview, the facility failed to provide residents with the ability to participate i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Record review revealed Resident #55 was admitted to the facility on [DATE] with diagnoses including chronic obstructive pulmo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the facility's infection control logs, infection control surveillance criteria reports, record reviews, staff...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, record review, and facility policy review, the facility failed to ensure food appropriately stored, prepared and distributed and failed to ensure the environment was c...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on review of the facility's infection control logs, staff interview, and policy review, the facility failed to maintain an effective infection control program that adequately tracked infections ...
Read full inspector narrative →
May 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interviews, and policy review the facility failed to ensure residents were afforded the right to transfe...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, review of typed statements, review of an appointment book, and interviews the facility failed to...
Read full inspector narrative →
Oct 2021
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of Resident #4 revealed a 09/17/19 admission and 07/15/20 readmission. The resident had diagnoses including insomnia, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, record review, policy and staff interview, the facility failed to ensure a resident totally dependent on staff was repositioned and his heels were floated. This affected one (Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, medical record review, and policy and procedure review, the facility failed to turn and r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on interview, medical record review, and policy review, the facility failed to ensure a physician addressed a pharmacy recommendation and ensure the pharmacist addressed the lack of response. Th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on interview, medical record review, policy review, the facility failed to ensure Resident #18 was not administered pain medications without appropriate comprehensive assessments including the l...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview, medical record review, and policy review, the facility failed to ensure as needed Xanax, antianxiety medication, did not exceed 14 days without appropriate physician assessments, b...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, and facility policy and procedure review, the facility failed to ensure proper hand washing when changing gloves. This affected two residents (Resident #2 and Re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, staff interview, record review, and policy review, the facility failed to ensure controlled drug records were in order. This affected three residents (Residents #9, #10 and #15) ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, and policy review, the facility failed to ensure all drugs and biological's were kept sto...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 4 life-threatening violation(s), Special Focus Facility, 1 harm violation(s), $144,718 in fines. Review inspection reports carefully.
- • 85 deficiencies on record, including 4 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $144,718 in fines. Extremely high, among the most fined facilities in Ohio. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Dixon Healthcare Center's CMS Rating?
CMS assigns DIXON HEALTHCARE CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Ohio, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Dixon Healthcare Center Staffed?
CMS rates DIXON HEALTHCARE CENTER's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 51%, compared to the Ohio average of 46%.
What Have Inspectors Found at Dixon Healthcare Center?
State health inspectors documented 85 deficiencies at DIXON HEALTHCARE CENTER during 2021 to 2025. These included: 4 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 1 that caused actual resident harm, 79 with potential for harm, and 1 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Dixon Healthcare Center?
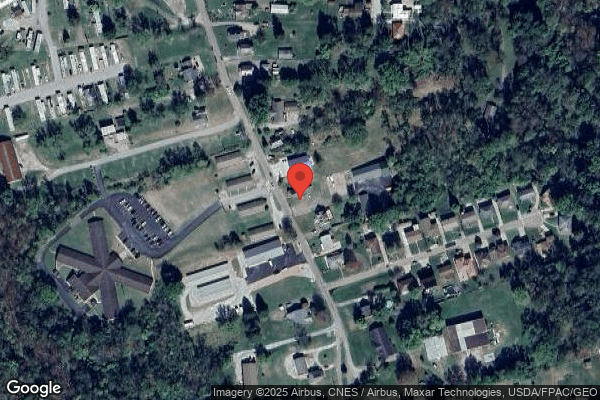
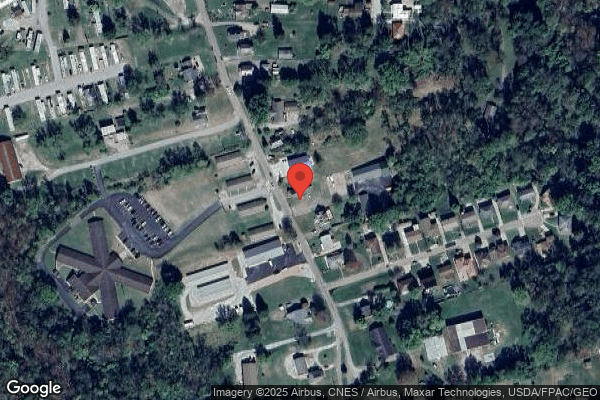
DIXON HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by COMMUNICARE HEALTH, a chain that manages multiple nursing homes. With 85 certified beds and approximately 62 residents (about 73% occupancy), it is a smaller facility located in WINTERSVILLE, Ohio.
How Does Dixon Healthcare Center Compare to Other Ohio Nursing Homes?
Compared to the 100 nursing homes in Ohio, DIXON HEALTHCARE CENTER's overall rating (2 stars) is below the state average of 3.2, staff turnover (51%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Dixon Healthcare Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the substantiated abuse finding on record, and the below-average staffing rating.
Is Dixon Healthcare Center Safe?
Based on CMS inspection data, DIXON HEALTHCARE CENTER has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). Inspectors have issued 4 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility is currently on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes nationwide). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Ohio. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Dixon Healthcare Center Stick Around?
DIXON HEALTHCARE CENTER has a staff turnover rate of 51%, which is about average for Ohio nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Dixon Healthcare Center Ever Fined?
DIXON HEALTHCARE CENTER has been fined $144,718 across 2 penalty actions. This is 4.2x the Ohio average of $34,526. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Dixon Healthcare Center on Any Federal Watch List?
DIXON HEALTHCARE CENTER is currently an SFF Candidate, meaning CMS has identified it as potentially qualifying for the Special Focus Facility watch list. SFF Candidates have a history of serious deficiencies but haven't yet reached the threshold for full SFF designation. The facility is being monitored more closely — if problems continue, it may be added to the official watch list. Families should ask what the facility is doing to address the issues that led to this status.