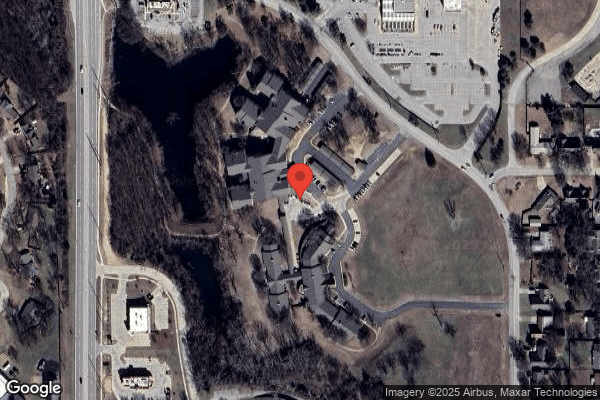
HERITAGE VILLA CARE & REHAB CENTER
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Heritage Villa Care & Rehab Center has a Trust Grade of D, indicating that it is below average with some concerning issues. It ranks #168 out of 282 facilities in Oklahoma, placing it in the bottom half statewide, and #4 out of 5 in Washington County, meaning only one nearby option is better. The facility is improving, as it reduced its issues from 14 in 2023 to 10 in 2025. Staffing is rated average with a turnover rate of 48%, which is better than the state average of 55%, but the overall star rating is only 2 out of 5, suggesting several areas for improvement. There have been some serious concerns, including a recent incident where a resident who required a two-person lift was transferred by a single staff member, increasing the risk of falls. Additionally, there was a finding regarding the cleanliness of the ice machine, which had not been properly maintained, posing a potential health risk. Despite these weaknesses, the facility shows some strengths in staffing retention and has no critical life-threatening issues reported.
- Trust Score
- D
- In Oklahoma
- #168/282
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 48% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $8,278 in fines. Lower than most Oklahoma facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 14 minutes of Registered Nurse (RN) attention daily — below average for Oklahoma. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 50 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Oklahoma average (2.6)
Below average - review inspection findings carefully
Near Oklahoma avg (46%)
Higher turnover may affect care consistency
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 50 deficiencies on record
Aug 2025
5 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure staff announced their presence in a resident's room while the resident was using the bathroom for 1 (#2) of 3 sampled residents revi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure a thorough investigation was completed following the discovery of an injury of unknown origin for 1 (#3) of 3 sampled residents revi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure a resident received a head-to-toe physical assessment after being found to have an injury of unknown origin for 1 (#3) of 3 sampled ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure a resident received medications as prescribed by a nurse practitioner for 1 (#1) of 3 sampled residents reviewed for unnecessary med...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0628
(Tag F0628)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure residents and their representatives were provided with a wri...
Read full inspector narrative →
Jan 2025
5 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure a certified nurse aide did not attempt to transfer a residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure a discharge MDS assessment was transmitted in the required t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure physician orders were followed for insulin administration for one (#31) of one sampled resident reviewed for insulin a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure a resident was provided education on the use of bed rails and given the option to consent or decline the use of bed ra...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure involuntary movement assessments were completed for a resident receiving an antipsychotic medication for one (#31) of five sampled r...
Read full inspector narrative →
Sept 2023
14 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility to ensure residents were assisted with dining in a dignified manner for one (#43) of four sampled residents reviewed for ADLs.
The Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure privacy was provided while performing a finger stick for blood sugar reading and while administering insulin to one (#...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure a resident was not involuntarily discharged while an appeal order was pending for one (#219) of one sampled residents reviewed for i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure a discharge summary was completed after a discharge for one (#169) of three sampled resident reviewed for discharge.
The Resident C...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
2. Resident #169 had diagnoses which included hypertension, diabetes mellitus, hyperlipidemia, and dementia.
An admission Resident Assessment, dated 07/17/22, documented Resident #169 required correct...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure a resident did not experience a significant medication error when a long acting insulin was administered instead of th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to ensure resident records were accurate for one (#43) of one sampled resident reviewed for nutrition.
The Resident Census and Co...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to ensure used linens were not placed on the floor during incontinent care for one (#12) of three sampled residents observed for ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to maintain comfortable air temperatures in resident rooms for two (#3 and #8) of 24 sampled residents reviewed for air temperat...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to:
a. monitor the amount of meals a resident who experienced weight loss consumed for one (#43); and
b. provide a physician ordered health sh...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure an accurate account of controlled medications was maintained for three (#62, 175, and #176) of three sampled residents...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
2. Resident #3 had diagnoses which included anxiety disorder, restlessness, and agitation.
A Physician's order, dated 06/21/23, documented lorazepam oral concentrate 2 mg/ml, give 0.25 ml by mouth eve...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
5. Resident #19 had diagnoses which included neurogenic bladder, diabetes mellitus, Alzheimer's, and dementia.
A Quarterly Resident Assessment, dated 08/30/23, documented Resident #19's cognition was...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
2. On 09/18/23 at 11:32 a.m., during meal service observation, with blue gloves on, [NAME] #2 rested their hands on their waist. The back of their hands touched their purple scrubs.
On 09/18/23 at 11...
Read full inspector narrative →
Apr 2021
26 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, it was determined the facility failed to accurately complete an annual assessment for one (#57) of 24 sampled residents whose assessments were revie...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined the facility failed to address a resident's elopement risk in the baseline care plan for one (#114) of one newly admitted resident who was at ri...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, it was determined the facility failed to review/revise resident care plans for two (#11 an...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, it was determined the facility failed to ensure an activity program that met residents preferences and/or needs for two (#20, and #29) of five sampl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, it was determined the facility failed to ensure a resident with an indwelling urinary catheter received appropriate care and services for one (#11) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined the facility failed to ensure pharmacy consultations/recommendations were addressed by the physician for one (#1) of five sampled residents who ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined the facility failed to ensure laboratory monitoring for a medication was completed for one (#1) of five sampled residents who were reviewed for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined the facility failed to ensure antianxiety medications were not ordered for more than 14 days for one (#1) of five sampled residents who were rev...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0776
(Tag F0776)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined the facility failed to ensure a resident was provided radiology services as ordered by the physician for one (#11) of three sampled residents wh...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0577
(Tag F0577)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, it was determined the facility failed to ensure survey results were accessible to residents/visitors. This had the potential to affect all 65 reside...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, it was determined the facility failed to provide facility failed to provide liability and ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** On 04/27/21 at 5:30 p.m., the MDS nurse was asked by phone interview if he was responsible for completing the assessments. He st...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Resident #35 had diagnoses which included muscle weakness, pain, and osteoporosis.
The resident's clinical record contained a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident #23 had a diagnosis of traumatic brain injury.
An admission assessment, dated 03/30/20, documented listening to musi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0680
(Tag F0680)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, it was determined the facility failed to have a qualified activities director. This had the potential to affect all 65 residents who resided in the ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, it was determined the facility failed to ensure residents with limited ROM received treatment and services to prevent further decrease or maintain R...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected multiple residents
Based on interview and record review, it was determined the facility failed to ensure pre and post dialysis assessments and physician's orders for dialysis were completed for one (#16) of one sampled ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected multiple residents
Based on interview and record review, it was determined the facility failed to ensure the DON did not work as a charge nurse when the resident census was 60 or greater. This had the potential to affec...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure CNAs had received performance/competency reviews yearly for five (CNA #2, #3, #4, #6, and CNA #7) of five employee ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
5. Resident #57 had diagnoses which included paraplegia, delusional disorders, and dementia with behavioral disturbance.
Review of the social services notes in the EMR from 01/01/20 to 04/19/21 contai...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected multiple residents
Based on interview and record review, it was determined the facility failed to ensure the QAA committee developed and implemented appropriate plans of action to correct quality deficiencies. The facil...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Resident #55 had diagnoses which included MS, chronic kidney disease, UTI, and neurogenic bladder.
A care plan, dated 01/18/...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, it was determined the facility failed to ensure the ice machine and scoop bucket were maintained in a sanitary manner. The dietary manager identifie...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
Based on interview and record review, it was determined the facility failed to ensure the QAPI program made good faith attempts to identify and correct quality deficiencies. The facility identified 65...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected most or all residents
Based on interview and record review, it was determined the facility failed to have complete documentation of the seasonal influenza vaccine and the pneumococcal vaccine, for three (#11, #1, and #59) ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected most or all residents
Based on interview and record review, it was determined the facility failed to:
~ ensure all staff were routinely tested for COVID-19; and
~ ensure outbreak testing was conducted until 14 days of no n...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • 50 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade D (43/100). Below average facility with significant concerns.
About This Facility
What is Heritage Villa Care & Rehab Center's CMS Rating?
CMS assigns HERITAGE VILLA CARE & REHAB CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Oklahoma, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Heritage Villa Care & Rehab Center Staffed?
CMS rates HERITAGE VILLA CARE & REHAB CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 48%, compared to the Oklahoma average of 46%.
What Have Inspectors Found at Heritage Villa Care & Rehab Center?
State health inspectors documented 50 deficiencies at HERITAGE VILLA CARE & REHAB CENTER during 2021 to 2025. These included: 1 that caused actual resident harm and 49 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Heritage Villa Care & Rehab Center?
HERITAGE VILLA CARE & REHAB CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by MGM HEALTHCARE, a chain that manages multiple nursing homes. With 100 certified beds and approximately 79 residents (about 79% occupancy), it is a mid-sized facility located in BARTLESVILLE, Oklahoma.
How Does Heritage Villa Care & Rehab Center Compare to Other Oklahoma Nursing Homes?
Compared to the 100 nursing homes in Oklahoma, HERITAGE VILLA CARE & REHAB CENTER's overall rating (2 stars) is below the state average of 2.6, staff turnover (48%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Heritage Villa Care & Rehab Center?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Heritage Villa Care & Rehab Center Safe?
Based on CMS inspection data, HERITAGE VILLA CARE & REHAB CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Oklahoma. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Heritage Villa Care & Rehab Center Stick Around?
HERITAGE VILLA CARE & REHAB CENTER has a staff turnover rate of 48%, which is about average for Oklahoma nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Heritage Villa Care & Rehab Center Ever Fined?
HERITAGE VILLA CARE & REHAB CENTER has been fined $8,278 across 1 penalty action. This is below the Oklahoma average of $33,162. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Heritage Villa Care & Rehab Center on Any Federal Watch List?
HERITAGE VILLA CARE & REHAB CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.