FORT GIBSON CARE & REHAB CENTER



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Fort Gibson Care & Rehab Center has received a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranking #160 out of 282 facilities in Oklahoma places it in the bottom half statewide, and #5 out of 10 in Muskogee County suggests only a few local options are available. The facility is reportedly improving, with the number of issues decreasing from 11 in 2023 to 8 in 2025. While staffing turnover is impressively low at 0%, indicating staff stability, the facility has incurred $52,377 in fines, which is concerning and higher than 91% of Oklahoma facilities. Specific incidents include failure to update fall prevention plans for a resident who experienced a fall and did not ensure proper restorative services for another resident, indicating potential gaps in care. Overall, while there are some strengths, significant weaknesses and compliance issues raise red flags for families considering this facility.
- Trust Score
- F
- In Oklahoma
- #160/282
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ✓ Good
- $52,377 in fines. Lower than most Oklahoma facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 17 minutes of Registered Nurse (RN) attention daily — below average for Oklahoma. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 35 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Oklahoma average (2.6)
Below average - review inspection findings carefully
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 35 deficiencies on record
Jan 2025
8 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on observation, record review, and interview, the facility failed to update and implement individualized fall interventions in the care plan for a resident who fell and sustained a head injury f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to complete a significant change assessment for a resident with a decl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure a referral was made to the LOCEU for one (#3) of three sampled residents reviewed for PASSARs.
The DON identified eight residents wi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to ensure a care plan was updated for one (#7) of thirteen resident care plans reviewed for accuracy.
The administrator identifie...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure medications were administered as ordered for one (#21) of five sampled residents reviewed for unnecessary medications.
The administ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure a resident received restorative services to ma...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure:
a. the ovens were clean;
b. foods were labeled and dated in the refrigerator; and
c. the ice scoop was maintained in ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure enhanced barrier precautions were
utilized during resident care for one (#32) of one sampled resident observed during ...
Read full inspector narrative →
Sept 2023
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure assessments were encoded and transmitted to CMS in the requi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, it was determined the facility failed to ensure a comprehensive care plan was developed fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure residents received the supervision and assista...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure the physician was notified of a significant weight loss and residents received interventions to maintain nutritional status within a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure behaviors and/or side effects were monitored for the use of psychotropic medications for two of (#20 and #25) of five sampled reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure residents were free from significant medication errors for one (#20) of five residents reviewed for unnecessary medications.
The Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure labs were obtained per physician order for one (#20) of five sampled residents reviewed for unnecessary medications.
The Resident Ce...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
Based on observation, record review,and interview, the facility failed to follow the menu and provide pureed foods listed on the menu for the puree diets from the kitchen.
The Resident Census and Con...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview the facility failed to provide food that was palatable and at an appetizing temperature for the residents.
The Resident Census and Conditions of Resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure food was stored, prepared, and served in a sanitary manner.
The Resident Census and Conditions of Residents form documented 45 reside...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to utilize their antibiotic stewardship policy to monitor antibiotic use for four (#11, 25, 32, and #36) of five residents revie...
Read full inspector narrative →
Aug 2022
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview, the facility failed to conduct a significant change assessment when the resident had an improvement in condition for one (#44) of 20 residents whose...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure completed resident assessments were transmitted to CMS within the required time frame for one (#1) of one resident reviewed for MDS ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview, the facility failed to conduct routine assessments of pressure ulcers for one (#39) of one resident reviewed for pressure ulcers.
The Resident Censu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure a PRN psychotropic medication duration order did not extend beyond 14 days and GDR of psychotropic medications were attempted for on...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview, the facility failed to ensure the residents were free of significant medication errors.
The Resident Census and Conditions of Residents form documen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure a DNR was signed by the appropriate person for two (#7 and #...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to notify the physician of blood pressure readings below normal limits for one (#5) of five residents reviewed for unnecessary medications.
Th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide letters of NOMNC to residents discharged from Medicare cove...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #5 had diagnoses which included insomnia and anxiety disorder.
The resident's April 2022 MAR documented temazepam (...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Res #27 was admitted into the facility on [DATE] with diagnoses anxiety disorder, depression (other than bipolar), psychotic ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Based on record review, observation, and interview, the facility failed to develop and revise care plans for two, (#3 and #44) of 13 residents whose care plans were reviewed. The facility failed to:
a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on record review, observation, and interview, the facility failed to ensure residents received monitoring, interventions, and supervision to prevent falls for two, (#3 and #44) of two residents ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to designate an RN to serve as DON for the previous eight months.
The...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
The facility failed to ensure medications were administered as ordered by the physician for one (#5) of five residents sampled for medication review.
The Resident Census and Condition of Resident's d...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure drug regimen reviews were acted upon for two (#5 and #20) of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on record review, observation, and interview, the facility failed to ensure the medication error rate was not five percent or greater.
The Resident Census and Conditions of Residents documented...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 harm violation(s), $52,377 in fines, Payment denial on record. Review inspection reports carefully.
- • 35 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $52,377 in fines. Extremely high, among the most fined facilities in Oklahoma. Major compliance failures.
- • Grade F (35/100). Below average facility with significant concerns.
About This Facility
What is Fort Gibson Care & Rehab Center's CMS Rating?
CMS assigns FORT GIBSON CARE & REHAB CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Oklahoma, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Fort Gibson Care & Rehab Center Staffed?
CMS rates FORT GIBSON CARE & REHAB CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes.
What Have Inspectors Found at Fort Gibson Care & Rehab Center?
State health inspectors documented 35 deficiencies at FORT GIBSON CARE & REHAB CENTER during 2022 to 2025. These included: 1 that caused actual resident harm and 34 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Fort Gibson Care & Rehab Center?
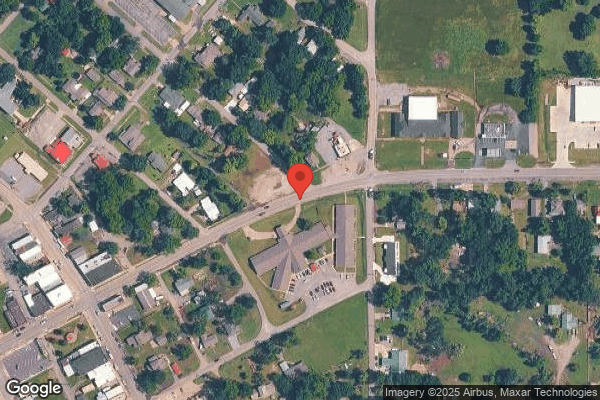
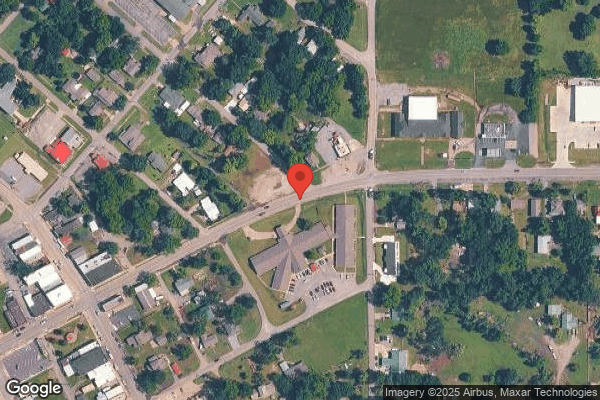
FORT GIBSON CARE & REHAB CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by MGM HEALTHCARE, a chain that manages multiple nursing homes. With 66 certified beds and approximately 52 residents (about 79% occupancy), it is a smaller facility located in FORT GIBSON, Oklahoma.
How Does Fort Gibson Care & Rehab Center Compare to Other Oklahoma Nursing Homes?
Compared to the 100 nursing homes in Oklahoma, FORT GIBSON CARE & REHAB CENTER's overall rating (2 stars) is below the state average of 2.6 and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Fort Gibson Care & Rehab Center?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Fort Gibson Care & Rehab Center Safe?
Based on CMS inspection data, FORT GIBSON CARE & REHAB CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Oklahoma. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Fort Gibson Care & Rehab Center Stick Around?
FORT GIBSON CARE & REHAB CENTER has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Fort Gibson Care & Rehab Center Ever Fined?
FORT GIBSON CARE & REHAB CENTER has been fined $52,377 across 1 penalty action. This is above the Oklahoma average of $33,603. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Fort Gibson Care & Rehab Center on Any Federal Watch List?
FORT GIBSON CARE & REHAB CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.