YORK MANOR NURSING HOME



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
York Manor Nursing Home in Muskogee, Oklahoma, has a Trust Grade of F, indicating significant concerns and a poor overall rating. It ranks #191 out of 282 facilities in the state, placing it in the bottom half, and #7 out of 10 in the county, meaning there are only three local options with lower rankings. While the facility's trend is improving, with issues decreasing from 19 in 2023 to 7 in 2025, the high turnover rate of 63% is concerning, although they do have good RN coverage, surpassing 91% of state facilities. Families should be aware of serious incidents such as a resident being left unattended in the shower, resulting in a fall and fracture, as well as concerns regarding proper hand hygiene practices among staff during meal service. Overall, while there are strengths in RN coverage and staffing ratings, the facility's poor trust grade and specific incidents of neglect raise significant red flags for potential residents and their families.
- Trust Score
- F
- In Oklahoma
- #191/282
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 63% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $9,750 in fines. Lower than most Oklahoma facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 26 minutes of Registered Nurse (RN) attention daily — below average for Oklahoma. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 40 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Below Oklahoma average (2.6)
Below average - review inspection findings carefully
17pts above Oklahoma avg (46%)
Frequent staff changes - ask about care continuity
Below median ($33,413)
Minor penalties assessed
15 points above Oklahoma average of 48%
The Ugly 40 deficiencies on record
Sept 2025
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to include the actual and working hours of licensed and unlicensed staff on the daily posted staffing and failed to ensure disci...
Read full inspector narrative →
Jan 2025
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure a NOMNC form was provided to a resident within the mandated time frame for one (#10) of three sampled residents reviewed for benefic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure infection control practices were followed for one (#26) of two sampled residents who were reviewed for wound care.
Th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to provide written notices of transfer to residents transferred to acute care hospitals by the facility for three (#17, 27, and #45) of three ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to post nurse staffing in a prominent place accessible to residents and visitors.
The administrator identified 42 residents who resided in the ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure:
a. the deep fryer was cleaned after use; and
b. refrigerated items were labeled and dated for the residents.
The die...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure the facility medical director participated in the quality as...
Read full inspector narrative →
Oct 2023
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure residents code status was documented correctly...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to notify a representative of a discharge to the hospital for one (#96) of three residents sampled for discharges.
The Resident Census and Co...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to ensure a significant change assessment was submitted to CMS within 14 days of completion for one (#7) of 21 residents whose assessments were...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure a resident with a newly evident possible serious mental disorder was referred to OHCA for one (#12) of one sampled resident whose PA...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, it was determined the facility failed to ensure baths were performed for one (#31) of three residents sampled for ADLs.
The Resident Census and Con...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to administer oxygen according to physician orders for one (#3) of one resident reviewed for respiratory care.
The Resident Cen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure residents with a diagnosis of post traumatic stress disorder received culturally competent trauma informed care in ord...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to review the risks and benefits of side rails with the resident or resident representative and obtain an informed consent prior...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to ensure the services of an RN was available in the facility eight hours daily seven days a week and failed to ensure an RN was designated to ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure the attending physician documented they had reviewed a consultant pharmacist's recommendation or provide a rational fo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure significant medication errors did not occur for one (#23) of five residents whose medications were reviewed.
The Resi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to prepare food in a form which met the individual needs of residents for one (#10) of one resident reviewed for a mechanically altered diet.
Th...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure residents on the resident trust fund had the right to manage their own financial affairs for three (#1, 37, and #38) o...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0568
(Tag F0568)
Could have caused harm · This affected multiple residents
Based on record review and interview the facility failed to ensure quarterly statements were provided to the residents who were on the trust fund for one (#27) of three residents reviewed for trust fu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure resident assessments accurately reflected the residents' status for three (#12, 23, and #28) of 16 sampled residents whose assessmen...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure:
a. dirty linens were stored properly.
b. proper PPE was present in the laundry room.
c. a program was designed to help prevent the de...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview the facility failed to store, prepare, distribute, and serve food in accordance with professional standards for food service safety.
The Resident Census and Conditio...
Read full inspector narrative →
Mar 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview, The facility failed to follow physician orders for one (#4) of four residents reviewed for oxygen therapy.
The DON reported eleven residents who re...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on record review, observation, and interview, it was determined the facility failed to maintain an infection prevention and control program to prevent the spread of infections. The facility fail...
Read full inspector narrative →
Nov 2022
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Based on record review, observation, and interview, the facility failed to ensure residents were free from neglect for one (#1) of three residents reviewed for abuse and neglect. The facility failed t...
Read full inspector narrative →
Aug 2022
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to offer advanced directives for one (#34) of five sampled residents reviewed for advanced directives.
The Resident Census and Conditions of R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure resident assessments accurately reflected the residents' status for one (#21) of 13 whose assessments were reviewed.
The Resident C...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview , the facility failed to ensure a resident with a serious mental health diagnosis was refer...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure a discharge summary was completed for one (#43) of one sampl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure the physician was notified of a significant weight loss and/or gain for two (#17 and #34) of three sampled residents reviewed for we...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure comprehensive care plans were developed for two (#31 and #33) of 13 sampled residents reviewed for care plans.
The Resident Census a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to update care plans for three (#21, 28, and #38) of 13 sampled reside...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0678
(Tag F0678)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 1. Resident #6 had diagnoses which included depression and psychotic disorder.
On [DATE] at 2:12 p.m., Resident #6's chart was r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
On 08/02/22 at 3:19 p.m., the pharmacist was asked where staff documented side effects for psychotropic medications. They stated, It is on the treatment sheets. They were asked what was the policy for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on record review, observation, and interview, the facility failed to ensure a medication administration error rate of less than 5% for two (#34 and #37) of four sampled residents who were observ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
2. Resident #11 had diagnoses which included, COPD, and other nonspecific abnormal finding of lung field.
A physician's order summary, dated August 2022, read in part, .Ipratropium-Albuterol Solution...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to offer pneumococcal immunizations to two (#1 and #25) of five sampled residents reviewed for immunizations.
The Resident Census and Conditi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on record review and interview, the facility failed to designate a RN to serve as the DON on a full-time basis.
The Resident Census and Conditions of Residents report, dated 08/02/22, documente...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • 40 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade F (38/100). Below average facility with significant concerns.
- • 63% turnover. Above average. Higher turnover means staff may not know residents' routines.
About This Facility
What is York Manor's CMS Rating?
CMS assigns YORK MANOR NURSING HOME an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Oklahoma, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is York Manor Staffed?
CMS rates YORK MANOR NURSING HOME's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 63%, which is 17 percentage points above the Oklahoma average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at York Manor?
State health inspectors documented 40 deficiencies at YORK MANOR NURSING HOME during 2022 to 2025. These included: 1 that caused actual resident harm and 39 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
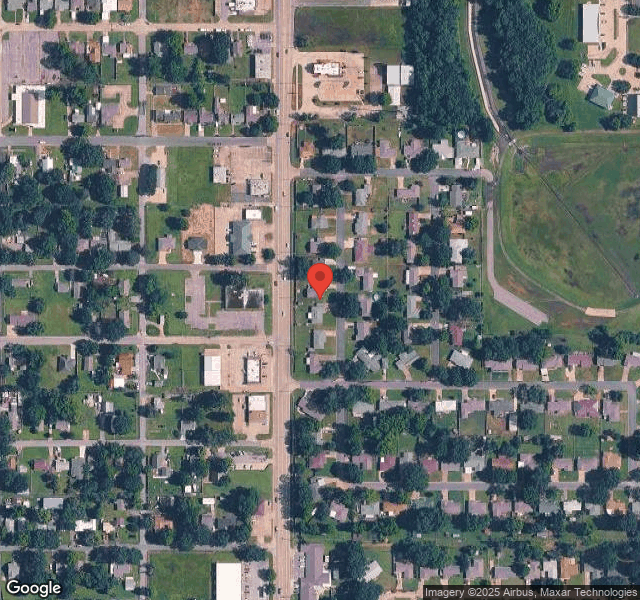
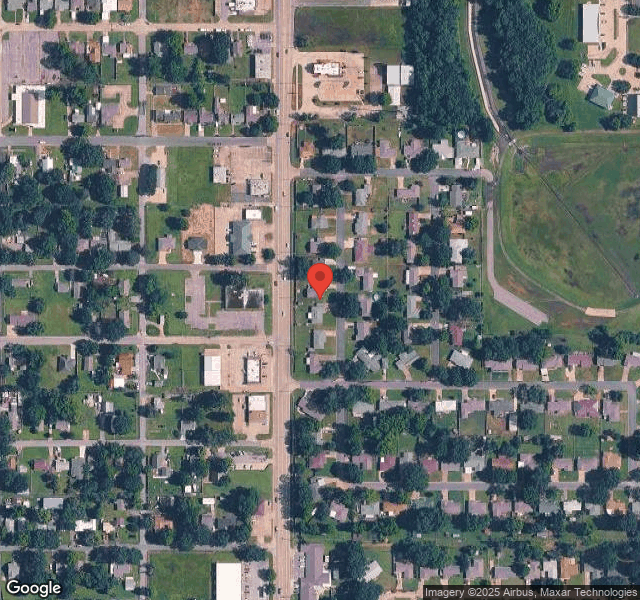
Who Owns and Operates York Manor?
YORK MANOR NURSING HOME is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 60 certified beds and approximately 41 residents (about 68% occupancy), it is a smaller facility located in MUSKOGEE, Oklahoma.
How Does York Manor Compare to Other Oklahoma Nursing Homes?
Compared to the 100 nursing homes in Oklahoma, YORK MANOR NURSING HOME's overall rating (2 stars) is below the state average of 2.6, staff turnover (63%) is significantly higher than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting York Manor?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's high staff turnover rate.
Is York Manor Safe?
Based on CMS inspection data, YORK MANOR NURSING HOME has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Oklahoma. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at York Manor Stick Around?
Staff turnover at YORK MANOR NURSING HOME is high. At 63%, the facility is 17 percentage points above the Oklahoma average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was York Manor Ever Fined?
YORK MANOR NURSING HOME has been fined $9,750 across 1 penalty action. This is below the Oklahoma average of $33,176. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is York Manor on Any Federal Watch List?
YORK MANOR NURSING HOME is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.