VILLAGE HEALTH CARE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Village Health Care in Gresham, Oregon, has a Trust Grade of D, indicating below-average quality and some significant concerns. It ranks #101 out of 127 facilities in Oregon, placing it in the bottom half, and #27 out of 33 in Multnomah County, meaning only a few local options are better. The facility's trend is worsening, with issues increasing from 7 in 2023 to 27 in 2025. While staffing is a strength with a turnover rate of 0%, significantly lower than the Oregon average, the facility has received $4,225 in fines, which is average but still suggests some compliance problems. Specific incidents include a serious medication error that led to a resident's hospitalization and failures in hand hygiene practices, which could put residents at risk for infections. Overall, while there are some strengths, such as staff stability, the facility has serious weaknesses that families should consider carefully.
- Trust Score
- D
- In Oregon
- #101/127
- Safety Record
- Moderate
- Inspections
- Getting Worse
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ✓ Good
- $4,225 in fines. Lower than most Oregon facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 40 minutes of Registered Nurse (RN) attention daily — about average for Oregon. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 38 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Oregon average (3.0)
Below average - review inspection findings carefully
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 38 deficiencies on record
May 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0760
(Tag F0760)
A resident was harmed · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure residents were free from significant medication errors for 1 of 3 sampled residents (#3) reviewed for medications. ...
Read full inspector narrative →
Feb 2025
26 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure residents were treated with dignity for 1 of 1 sampled resident (# 3) and 1 of 1 facility reviewed for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to inform residents and/or the residents' responsible party of the risks and benefits, and to ensure consent was obtained for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0553
(Tag F0553)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to ensure residents were included in care planning fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to determine the appropriateness for the self-administration of medication for 2 of 2 sampled residents (#s 18 a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure the call light was within reach for 1 of 1 sampled resident (#17) reviewed for call lights. This place...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to provide SNF ABN (Skilled Nursing Facility Advanced...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure accurate assessments for 2 of 5 sampled residents (#s 25 and 45) reviewed for medications. This placed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to conduct a new/accurate Level I PASARR (Pre-admission Sc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to comprehensively develop a resident-centered baseli...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to develop a plan of care to address resident centere...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review it was determined the facility failed to provide care and treatment as care p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to provide glasses repair assistance for 1 of 1 sampled resident (# 45) reviewed for vision. This placed residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to regularly provide restorative nursing...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to update pain medication instructions to include res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure dialysis services were in place including monitoring and communication with the dialysis provider for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to respond to pharmacy recommendations for limiting use of PRN antipsychotic to 14 days for 1 of 5 residents (#15) reviewed f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on Interview and record review it was determined the facility failed ensure PRN use of an antipsychotic was limited to 14 days for 1 of 5 residents (#15) for whom medications were reviewed. This...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to accurately document physician orders for 2 of 4 sampled residents (#s 220 and 269 ) reviewed for choices and ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0572
(Tag F0572)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure residents were notified their of rights both orally and in writing on an ongoing basis for 1 of 1 facility reviewed...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0576
(Tag F0576)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to have a system in place to deliver mail on Saturdays for 1 of 1 Resident Council reviewed. This placed residents at risk fo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to comprehensively assess 3 of 7 sampled residents (#...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 17 was admitted to the facility in 2021 with diagnoses including stroke and Aphasia (language disorder that affects ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to provide evidence a designated licensed nurse (LN) served as a charge nurse to provide the appropriate competencies and ski...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure an RN was available for at least eight consecutive hours per day seven days per week for 9 of 27 days reviewed for ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review it was determined the facility failed to ensure proper hand hygiene and infection control practices were followed during CBG monitoring for 1 of 1 sam...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on observation, interview, and record review, it was determined the facility failed to post accurate and complete staffing information for 1 of 1 facility reviewed for staffing. This placed resi...
Read full inspector narrative →
Sept 2023
7 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a resident's missing personal property was addressed for 1 of 1 sampled resident (#34) reviewed for personal proper...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure physician orders were followed for 1 of 5 sampled residents (#20) reviewed for unnecessary medications. This placed...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure residents were free from unnecessary bowel medications for 1 of 5 sampled residents (#20) reviewed for unnecessary ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to ensure a medication pass error rate o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to store drugs and biologicals in locked...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure a periodic review regarding advance directives was completed for 4 of 4 sampled residents (#s 1, 2, 29 and 32) revi...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure the Direct Care Staff Daily Report (DCSDR) postings were accurate for 17 of 36 days reviewed for staffing. This pla...
Read full inspector narrative →
Nov 2019
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to report injuries of unknown origin to the state agency for 1 of 3 sampled residents (#29) reviewed for abuse. This placed r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on observations, interview and record review it was determined the facility failed to accurately assess hospice, cognition and mood for 2 of 4 sampled residents (#42 and 64) who were reviewed fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to revise and update resident care plans for 2 of 3 sampled residents (#s 7, and 42) reviewed for abuse. This pl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to provide respiratory care and services in accordance with residents needs for 2 of 2 sampled residents (#s 16 ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • $4,225 in fines. Lower than most Oregon facilities. Relatively clean record.
- • 38 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade D (43/100). Below average facility with significant concerns.
About This Facility
What is Village Health Care's CMS Rating?
CMS assigns VILLAGE HEALTH CARE an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Oregon, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Village Health Care Staffed?
CMS rates VILLAGE HEALTH CARE's staffing level at 3 out of 5 stars, which is average compared to other nursing homes.
What Have Inspectors Found at Village Health Care?
State health inspectors documented 38 deficiencies at VILLAGE HEALTH CARE during 2019 to 2025. These included: 1 that caused actual resident harm, 36 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
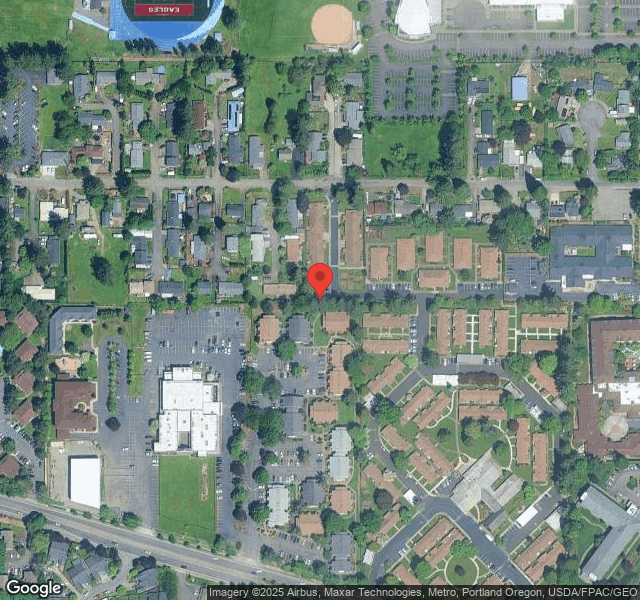
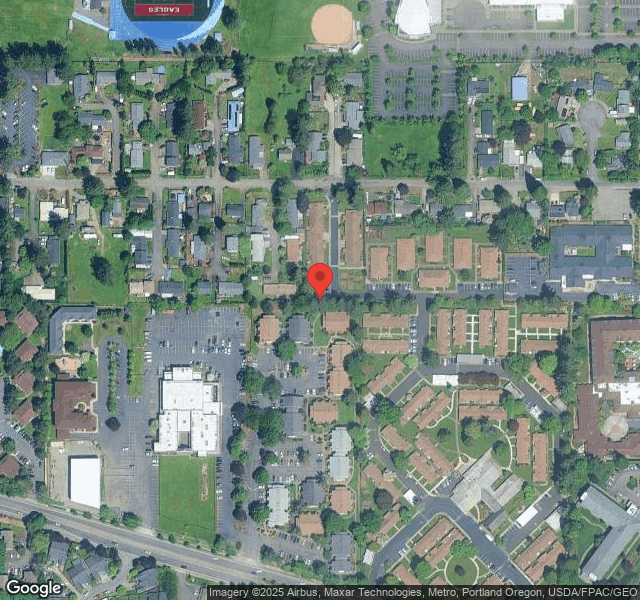
Who Owns and Operates Village Health Care?
VILLAGE HEALTH CARE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by EMPRES OPERATED BY EVERGREEN, a chain that manages multiple nursing homes. With 106 certified beds and approximately 66 residents (about 62% occupancy), it is a mid-sized facility located in GRESHAM, Oregon.
How Does Village Health Care Compare to Other Oregon Nursing Homes?
Compared to the 100 nursing homes in Oregon, VILLAGE HEALTH CARE's overall rating (2 stars) is below the state average of 3.0 and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Village Health Care?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Village Health Care Safe?
Based on CMS inspection data, VILLAGE HEALTH CARE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Oregon. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Village Health Care Stick Around?
VILLAGE HEALTH CARE has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Village Health Care Ever Fined?
VILLAGE HEALTH CARE has been fined $4,225 across 1 penalty action. This is below the Oregon average of $33,121. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Village Health Care on Any Federal Watch List?
VILLAGE HEALTH CARE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.