AVAMERE REHABILITATION OF OREGON CITY




Inspected within the last 6 months. Data reflects current conditions.
Avamere Rehabilitation of Oregon City has received a Trust Grade of F, indicating significant concerns about the facility's operations and care quality. It ranks #51 out of 127 nursing homes in Oregon, placing it in the top half, but the overall score suggests there are serious issues to consider. The situation appears to be improving, with a decrease in reported problems from 31 in 2024 to 12 in 2025, but the facility still faces challenges. Staffing is rated well at 4 out of 5 stars, with a turnover rate of 38% which is lower than the state average, but there are concerning fines totaling $147,486, higher than 88% of Oregon facilities. Specific incidents include a resident sustaining a fractured arm due to improper assistance during transfers and lapses in skin care assessments for another resident, highlighting areas of both concern and the need for improvement in resident care.
- Trust Score
- F
- In Oregon
- #51/127
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 38% turnover. Near Oregon's 48% average. Typical for the industry.
- Penalties ✓ Good
- $147,486 in fines. Lower than most Oregon facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 34 minutes of Registered Nurse (RN) attention daily — about average for Oregon. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 65 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (38%)
10 points below Oregon average of 48%
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Near Oregon average (3.0)
Meets federal standards, typical of most facilities
Near Oregon avg (46%)
Typical for the industry
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 65 deficiencies on record
Aug 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on interview and record review it was determined the facility failed to provide adequate supervision and assistance to prevent a fall with injury for 1 of 2 sampled residents (#8) reviewed for f...
Read full inspector narrative →
Jun 2025
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure residents were informed of the risks and benefits of psychotropic medications for 1 of 5 sampled residents (#14) re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to provide a homelike environment for 1 of 4 sampled residents (#15) reviewed for environment. This placed resi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to thoroughly investigate allegations of mental abuse for 1 of 2 sampled residents (#2) reviewed for abuse. This placed resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure a PASARR Level II (Preadmission Screening and Resident Review for individuals with a mental disorder a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure hearing aids fit properly and worked for 1 of 1 sampled resident (#45) reviewed for communication. Thi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to offer restorative services to increase range of motion for 1 of 1 sampled resident (#4) reviewed for rehabili...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to ensure staff followed transmission-ba...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined the facility failed to ensure biologicals were stored securely for 1 of 3 sampled medication carts reviewed for medication storage. ...
Read full inspector narrative →
Jan 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed properly orientate and sufficiently prepare a residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to follow physician's orders for 1 of 3 sampled residents (#2) reviewed for diabetic medication management. This placed resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to provide palatable food for 4 of 5 sampled residents (#s 3, 9, 12 and 13) reviewed for dietary services. This ...
Read full inspector narrative →
Feb 2024
31 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 46 admitted to the facility in 10/2023 with diagnoses including chronic kidney disease.
Resident 46's 10/31/23 admi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to assess a resident's ability to self-administer medications for 1 of 1 sampled resident (#33) reviewed for se...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure residents received written information in a manner they understand for 1 of 1 sampled residents (#24) and failed to...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to maintain adequate room temperatures for 1 of 1 resident (#156) reviewed comfortable environments. This placed...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure resident drug records including narcotics were accurate for 1 of 1 sampled resident (#259) reviewed for medications...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
2. Resident 46 was admitted to the facility in 10/2023 with diagnoses including chronic kidney disease.
Resident 46's 10/31/23 admission MDS indicated the resident was moderately cognitively impaired...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to investigate an allegation of abuse and injury of unknown origin for 2 of 4 sampled residents (#s 42 and 46) reviewed for a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to provide ongoing assessments of a skin condition fo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to ensure a significant change of condit...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to accurately code MDS assessments for 2 of 3 sampled...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on interview, and record review it was determined the facility failed to develop comprehensive care plans for 2 of 3 sampled residents (#s 17, and 33) reviewed for dialysis and dental. This plac...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review it was determined the facility failed to revise care plans and conduct person...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined facility staff failed to meet professional standards for medication administration for 2 of 2 unsampled residents (#s 13 and 37) and...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
2. Resident 8 admitted to the facility in 12/2023 with diagnoses including stroke.
Resident 8's 12/10/23 admission MDS indicated the resident was cognitively intact and dependent on staff assistance ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review it was determined the facility failed to ensure treatment and services to mai...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
2. Resident 19 admitted to the facility in 4/2023 with diagnoses including congestive heart failure.
On 2/5/24 at 11:11 AM Resident 19 was observed in bed with a long darkened colored right toenail. R...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to provide a restorative program to prevent further decline in range of motion as ordered for 1 of 1 sampled re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure staff followed the care plan related to fall safety for 1 of 2 sampled residents (#46) reviewed for ac...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to follow physician orders related to oxygen and BiPAP (breathing support through a face mask) administration fo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to provide appropriate and timely pain m...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure ongoing communication with the dialysis center for 1 of 1 sampled resident (#17) reviewed for dialysis. This placed res...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to maintain a medication error rate of less than 5%. There were 3 errors in 26 opportunities resulting in an 11...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to provide timely dental services to meet resident needs for 1 of 1 sampled resident (#33) reviewed for dental. This placed r...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0810
(Tag F0810)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure residents received adaptive utensils for 1 of 7 sampled resident (#16) reviewed for ADLs. This placed ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 49 admitted to the facility on [DATE] with diagnoses including subdural hemorrhage (bleeding inside the skull).
Res...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
3. Resident 259 was admitted to the facility on 1/2024 with diagnoses including lumbar radiculopathy (inflammation of a nerve root in the lower back).
A 1/25/24 admission MDS indicated Resident 259 h...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide sufficient nursing staff to ensure residents a...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure CNAs received annual performance reviews for 4 of 5 randomly selected CNA staff (#s 19, 21, 22 and 23) reviewed for...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review it was determined the facility failed to ensure the Direct Care Daily Staff Reports (DCSDR) were accurate for 79 of 188 days reviewed for staffing. T...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to have a system in place to ensure CNA staff received 12 hours of in-service training annually for 3 of 5 randomly selected ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on interview and record review it was determined the facility's quality assessment and assurance committee (QAA) failed to implement and oversee appropriate plans of action to correct identified...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to provide sufficient staffing to ensure...
Read full inspector narrative →
Jan 2023
21 deficiencies
3 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Based on interview and record review it was determined the facility failed to protect the residents right to be free from physical abuse by staff for 1 of 1 sampled resident (#25) reviewed for abuse. ...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Investigate Abuse
(Tag F0610)
A resident was harmed · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a thorough investigation was completed related to an allegation of physical abuse for 1 of 1 sampled resident (#25)...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
b. Resident 45 admitted to the facility in 12/2022 with diagnoses including a stroke and aphasia (communication disorder).
The 12/20/22 admission MDS indicated the resident was cognitively intact but...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure a resident received a recliner chair for 1 of 2 sampled residents (#26) reviewed for accommodation of ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on observation and interview the facility failed to assist a resident with transportation to a medical appointment for 1 of 1 sampled residents (#98) reviewed for medical transportation. This pl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to update the care plan for feeding assistance for 1 of 5 sampled residents (#25) reviewed for food. This placed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to consistently document behaviors and u...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on observation and interview it was determined the facility failed to not administer a blood pressure medication according to physician ordered parameters for 1 of 5 sampled residents (#15) revi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure a medication error rate of less than five percent for 1 of 4 sampled residents (#15) reviewed for medi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to accommodate resident food preferences for 1 of 5 sampled residents (#25) reviewed for food. This placed resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a resident's medical record reflected the care and services provided across all disciplines to ensure information i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure resident council requests or grievances were followed up on for 1 of 1 Resident Council reviewed for grievances. Th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident 16 admitted to the facility in 2015 with diagnoses including dementia.
The 11/5/22 Annual MDS indicated Resident 16...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0680
(Tag F0680)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to provide a qualified professional to direct the activities program for the facility. This placed residents at risk for unme...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined the facility failed to ensure the daily staff posting was accurate for 18 out of 31 days reviewed for staffing. This placed resident...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined the facility failed to develop a policy that identified staff responsible for monitoring the use and storage of food in resident per...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review it was determined the facility failed to provide sufficient nursing staff to attain and maintain the highest practicable wellbeing for 3 of 3 halls (1...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected most or all residents
Based on observation and interview it was determined the facility failed to provide sufficient support personnel to effectively carry out the functions of the food and nutrition service for 1 of 1 kit...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected most or all residents
3. Resident 25 admitted to the facility in 2018 with diagnoses including Alzheimer's disease.
The 11/30/22 Quarterly MDS indicated Resident 25 was rarely/never understood and required extensive assis...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review it was determined the facility failed to ensure kitchen equipment was clean, food was stored and labeled according to appropriate food handling guidel...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on interview and record review it was determined the facility's quality assessment and assurance committee (QAA) failed to implement and oversee appropriate plans of action to correct identified...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 38% turnover. Below Oregon's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 5 harm violation(s), $147,486 in fines. Review inspection reports carefully.
- • 65 deficiencies on record, including 5 serious (caused harm) violations. Ask about corrective actions taken.
- • $147,486 in fines. Extremely high, among the most fined facilities in Oregon. Major compliance failures.
- • Grade F (20/100). Below average facility with significant concerns.
About This Facility
What is Avamere Rehabilitation Of Oregon City's CMS Rating?
CMS assigns AVAMERE REHABILITATION OF OREGON CITY an overall rating of 3 out of 5 stars, which is considered average nationally. Within Oregon, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Avamere Rehabilitation Of Oregon City Staffed?
CMS rates AVAMERE REHABILITATION OF OREGON CITY's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 38%, compared to the Oregon average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Avamere Rehabilitation Of Oregon City?
State health inspectors documented 65 deficiencies at AVAMERE REHABILITATION OF OREGON CITY during 2023 to 2025. These included: 5 that caused actual resident harm and 60 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Avamere Rehabilitation Of Oregon City?
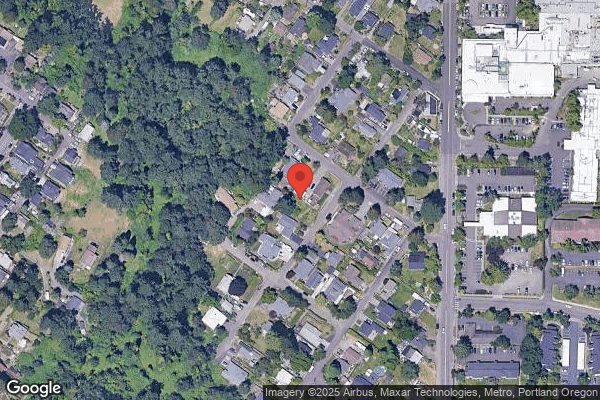
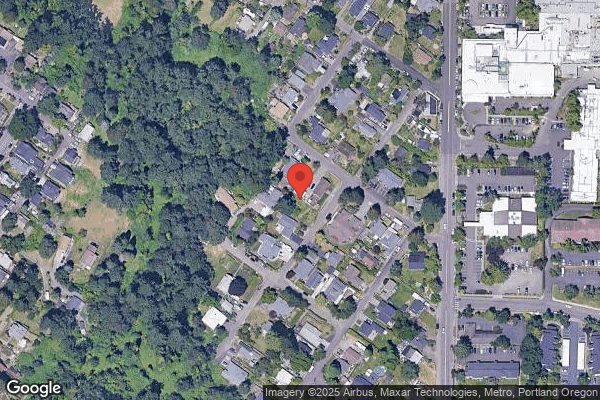
AVAMERE REHABILITATION OF OREGON CITY is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by AVAMERE, a chain that manages multiple nursing homes. With 111 certified beds and approximately 61 residents (about 55% occupancy), it is a mid-sized facility located in OREGON CITY, Oregon.
How Does Avamere Rehabilitation Of Oregon City Compare to Other Oregon Nursing Homes?
Compared to the 100 nursing homes in Oregon, AVAMERE REHABILITATION OF OREGON CITY's overall rating (3 stars) matches the state average, staff turnover (38%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Avamere Rehabilitation Of Oregon City?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Avamere Rehabilitation Of Oregon City Safe?
Based on CMS inspection data, AVAMERE REHABILITATION OF OREGON CITY has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in Oregon. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Avamere Rehabilitation Of Oregon City Stick Around?
AVAMERE REHABILITATION OF OREGON CITY has a staff turnover rate of 38%, which is about average for Oregon nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Avamere Rehabilitation Of Oregon City Ever Fined?
AVAMERE REHABILITATION OF OREGON CITY has been fined $147,486 across 2 penalty actions. This is 4.3x the Oregon average of $34,554. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Avamere Rehabilitation Of Oregon City on Any Federal Watch List?
AVAMERE REHABILITATION OF OREGON CITY is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.