FRIENDSHIP HEALTH CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Friendship Health Center in Portland, Oregon, has received a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranking #114 of 127 facilities in the state places it in the bottom half, and #31 of 33 in Multnomah County suggests there are very few local options that perform better. Although the facility is showing an improving trend, going from 31 issues in 2024 to just 1 in 2025, the high turnover rate of 70% is alarming, especially compared to the Oregon average of 49%. Staffing is rated as average with a 3/5 score, but the RN coverage is below that of 80% of state facilities, which is concerning because registered nurses play a crucial role in catching potential problems. Notably, there were serious incidents reported, including a resident not receiving timely rehabilitative services, leading to a decline in their physical health, and others being discharged without adequate wound care instructions, resulting in complications that required re-hospitalization. While there are some strengths in staffing, the overall trust grade and serious findings highlight significant weaknesses that families should carefully consider.
- Trust Score
- F
- In Oregon
- #114/127
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 70% turnover. Very high, 22 points above average. Constant new faces learning your loved one's needs.
- Penalties ✓ Good
- $103,564 in fines. Lower than most Oregon facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 33 minutes of Registered Nurse (RN) attention daily — about average for Oregon. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 58 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Oregon average (3.0)
Significant quality concerns identified by CMS
24pts above Oregon avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Significant penalties indicating serious issues
22 points above Oregon average of 48%
The Ugly 58 deficiencies on record
Feb 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, it was determined the facility failed to assess and conduct weekly wound evaluations for pressure ulcer care for 1 of 3 sampled residents (#3) review...
Read full inspector narrative →
Oct 2024
27 deficiencies
1 IJ
CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Quality of Care
(Tag F0684)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 38 was admitted to the facility in 7/2021 with diagnoses including hypertension (a condition where the pressure of b...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0825
(Tag F0825)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to ensure residents received timely spec...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
2. Resident 77 was admitted to the facility in 3/2024 with diagnoses including anemia and major depressive disorder.
Resident 77's 3/22/24 Physician Order indicated the resident was prescribed Celexa ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to honor a resident's preference for room layout for 1 of 2 sampled residents (#16) reviewed for choices. This ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure residents had an advance directive for 2 of 4 sampled residents (#s 1 and 16) reviewed for advance directives. This...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a resident's emergency contact was notified of a resident's hospitalization for 1 of 2 sampled residents (#16) revi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to ensure NOMNC (Notice of Medicare Non-Coverage) not...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a system was in place to resolve resident grievances promptly for 1 of 1 resident (#57) reviewed for abuse. This pl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to accurately assess residents for communication, dental, and transfers for 3 of 9 sampled residents (#s 1, 14 a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to provide appropriate treatment and services in the area of communication for 1 of 4 sampled residents (#53) re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to provide the necessary care and servic...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
3. Resident 50 was admitted to the facility in 11/2021 with diagnoses including dementia.
Resident 50's 7/13/24 Fall Risk Assessment indicated the resident was considered at moderate risk to fall.
R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0742
(Tag F0742)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to provide treatment and services to correct ongoing signs of depressive behavior for 1 of 1 sampled resident (#...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
2. Resident 49 was admitted to the facility in 5/2024 with diagnoses including hyperlipidemia (high cholesterol) and kidney failure.
A 5/31/24 BIMS indicated Resident 49 had normal cognitive function....
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure a resident was monitored for side effects of antidepressants for 1 of 5 sampled residents (#1) reviewed for unneces...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to ensure a follow-up dental exam was scheduled for 1 of 4 sampled residents (#16) reviewed for dental. This pl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined the facility failed to ensure dignified language was used to address residents and their equipment for 1 of 1 facility and 1 of 2 sa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Observations of the facility's general environment and residents' rooms from 10/7/24 through 10/15/24 identified the following i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
2. Resident 33 was admitted to the facility in 12/2021 with diagnoses including chronic respiratory failure with hypoxia (a condition in which the body does not have enough oxygen in the blood).
A re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Resident 7 was admitted to the facility in 11/2019 with diagnoses including multiple sclerosis and depression.
Resident 7's health record revealed she/he had contractures to the left shoulder, hips, a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident 38 was admitted to the facility in 7/2021 with diagnoses including dementia.
Resident 38's 6/30/24 Annual MDS reveal...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected multiple residents
4. Resident 7 was admitted to the facility in 11/2019 with diagnoses including multiple sclerosis and depression.
A 3/17/24 annual MDS revealed Resident 7 had impaired mobility of the upper and lower ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was it was determined the facility failed to ensure a medication error rate of less than 5%. The facility administration error rate was 19.23% with...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
3. On 10/8/24 at 3:53 PM a treatment cart was observed to be unlocked on 2C. The nurse was not in view of the cart.
On 10/8/24 at 4:09 PM Staff 6 (LPN) confirmed the cart was unlocked.
4. On 10/10/24...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined the facility failed to ensure foods were labeled and stored to ensure proper food storage practices were followed in 1 of 1 kitchen ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0847
(Tag F0847)
Could have caused harm · This affected most or all residents
Based on interview and record review it was determined the facility failed to ensure residents were fully informed and understood the binding arbitration agreement for 1 of 1 facility reviewed for bin...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
3. On 10/10/24 at 12:16 PM Staff 22 (Laundry Services) was observed to deliver clean resident clothing throughout wings B and C on the 2nd floor. A small sheet was draped over a portion of the cart bu...
Read full inspector narrative →
Jul 2024
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0661
(Tag F0661)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete a discharge summary with required information for wound ca...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to follow physician orders and provide correct oxygen administration for 1 of 3 sampled residents (#12) reviewed for physicia...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure licensed nursing staff possessed the competencies and skill sets necessary related to oxygen administration for 1 o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure wheelchairs were clean and sanitary for 1 of 3 sampled residents (#13) reviewed for equipment. This pl...
Read full inspector narrative →
Sept 2023
7 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to ensure Staff 9 (Agency CNA) met professional stand...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to follow physician's orders for 1 of 3 sampled resid...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to ensure residents were free from negle...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to ensure residents were free from misappropriation o...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to provide ADL care to 4 of 4 sampled residents (#s 2...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to ensure sufficient staffing to meet re...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to implement a Quality Assessment and Performance Improvement (QAPI) program which identified quality deficiencies, developed and implemented a...
Read full inspector narrative →
Jun 2023
12 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure residents were assessed for self-administration of medications and a physician order was in place for ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to ensure a call light was readily acces...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident 18 was admitted to the facility in 2022 with diagnoses including major depressive disorder.
Review of the 5/2023 MAR...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to implement the care plan related to po...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
2. Resident 8 was admitted to the facility in 2019 with diagnoses including multiple sclerosis and depression.
An 11/12/19 Care Plan included Resident 8 required assistance with personal hygiene and g...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to provide support for a resident's choi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to consistently perform pressure ulcer assessments and wound care for 1 of 4 sampled residents (# 56) reviewed for pressure u...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to follow physician orders for oxygen therapy for 1 of 1 sampled resident (#25) reviewed for oxygen. This placed...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0712
(Tag F0712)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure physician visits occurred as required for 1 of 5 sampled residents (#40) reviewed for unnecessary medications. This...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure a medication pass error rate of less than 5%. There were three errors in 28 opportunities resulting in...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
2. Resident 56 was admitted to the facility in 2021 with diagnoses including paraplegia.
A 9/14/21 Weekly Skin Evaluation determined Resident 56 acquired an unstageable left ischeal tuberosity (boney...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation and interview it was determined the facility failed to maintain comfortable sound levels for 1 of 1 facility observed for environment. This placed residents at risk for an uncomfo...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Based on interviews and record review it was determined the facility failed to ensure residents were free from misappropriation of financial resources for 1 of 7 sampled residents (#100) reviewed for ...
Read full inspector narrative →
May 2022
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review it was determined the facility failed to investigate an allegation of abuse for 1 of 2 samp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to revise and review the plan of care after a completed assessment for 1 of 5 sampled residents (#29) reviewed for ADL care. This ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure the facility maintained a medication error rate of less than 5%. There were 6 errors in 27 opportuniti...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to follow infection control procedures for a resident on isolation precautions for 1 of 10 sampled residents (#1...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and interview it was determined the facility failed to properly store and label food for 1 of 1 kitchen reviewed for food storage. This placed residents at risk for foodborne illn...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0838
(Tag F0838)
Minor procedural issue · This affected most or all residents
Based on interview and record review the facility failed to annually update the facility assessment to include current staffing needs and resources related to COVID-19. This place residents a risk for...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s), Special Focus Facility, 2 harm violation(s), $103,564 in fines. Review inspection reports carefully.
- • 58 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $103,564 in fines. Extremely high, among the most fined facilities in Oregon. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Friendship's CMS Rating?
CMS assigns FRIENDSHIP HEALTH CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Oregon, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Friendship Staffed?
CMS rates FRIENDSHIP HEALTH CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 70%, which is 24 percentage points above the Oregon average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 60%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Friendship?
State health inspectors documented 58 deficiencies at FRIENDSHIP HEALTH CENTER during 2022 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 2 that caused actual resident harm, 54 with potential for harm, and 1 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
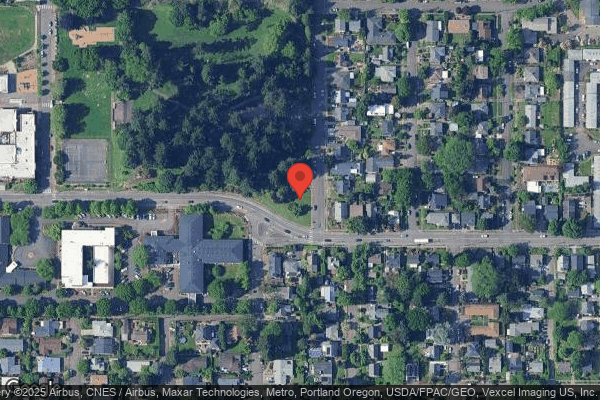
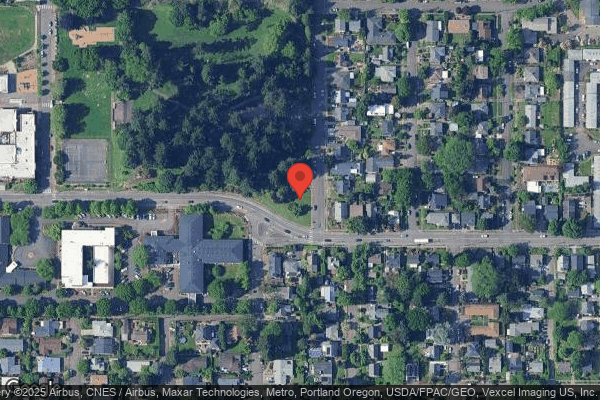
Who Owns and Operates Friendship?
FRIENDSHIP HEALTH CENTER is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 100 certified beds and approximately 65 residents (about 65% occupancy), it is a mid-sized facility located in PORTLAND, Oregon.
How Does Friendship Compare to Other Oregon Nursing Homes?
Compared to the 100 nursing homes in Oregon, FRIENDSHIP HEALTH CENTER's overall rating (1 stars) is below the state average of 3.0, staff turnover (70%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Friendship?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the facility's high staff turnover rate.
Is Friendship Safe?
Based on CMS inspection data, FRIENDSHIP HEALTH CENTER has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility is currently on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes nationwide). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Oregon. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Friendship Stick Around?
Staff turnover at FRIENDSHIP HEALTH CENTER is high. At 70%, the facility is 24 percentage points above the Oregon average of 46%. Registered Nurse turnover is particularly concerning at 60%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Friendship Ever Fined?
FRIENDSHIP HEALTH CENTER has been fined $103,564 across 2 penalty actions. This is 3.0x the Oregon average of $34,115. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Friendship on Any Federal Watch List?
FRIENDSHIP HEALTH CENTER is currently an SFF Candidate, meaning CMS has identified it as potentially qualifying for the Special Focus Facility watch list. SFF Candidates have a history of serious deficiencies but haven't yet reached the threshold for full SFF designation. The facility is being monitored more closely — if problems continue, it may be added to the official watch list. Families should ask what the facility is doing to address the issues that led to this status.