GATEWAY CARE AND RETIREMENT




Inspected within the last 6 months. Data reflects current conditions.
Gateway Care and Retirement in Portland, Oregon, has a Trust Grade of C+, indicating that it is slightly above average but not particularly outstanding. It ranks #55 out of 127 facilities in Oregon, placing it in the top half, and #14 of 33 in Multnomah County, which shows that there are only a few better local options. However, the facility's trend is concerning as the number of issues reported rose significantly from 3 in 2024 to 12 in 2025. Staffing appears to be a strength with a low turnover rate of 0%, which is significantly better than the state average of 49%, but the facility has received 34 total deficiencies, mainly concerning sanitary practices and staff training, including incidents of improper food storage and inadequate staff training in dementia care. While there are no fines on record, the inspection findings suggest that while the facility has some strengths, there are important areas that require immediate attention to ensure resident safety and quality care.
- Trust Score
- C+
- In Oregon
- #55/127
- Safety Record
- Low Risk
- Inspections
- Getting Worse
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Oregon facilities.
- Skilled Nurses ○ Average
- Each resident gets 33 minutes of Registered Nurse (RN) attention daily — about average for Oregon. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 34 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Near Oregon average (3.0)
Meets federal standards, typical of most facilities
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 34 deficiencies on record
Jul 2025
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review it was determined the facility failed to properly store food and failed to maintain sanitary conditions in 1 of 1 kitchen. This placed residents at ri...
Read full inspector narrative →
May 2025
10 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to report results of abuse investigations to the State Survey Agency within the required time frame for 2 of 4 sampled reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to revise, update and implement the care...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to provide the necessary services to maintain good grooming and personal hygiene for 1 of 4 sampled resident (#...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to provide an ongoing person-centered ac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure dependent residents were provided assistance with toenail care for 2 of 4 sampled residents (#s 2 and ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure supervision and safety interventions were in place to prevent smoking related accidents for 1 of 2 sampled resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure food was
served at an appetizing temperature for 1 of 2 sampled residents (#11) reviewed for food. Th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to ensure a comfortable and homelike env...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review it was determined the facility failed to store all medications and biologicals under proper temperature controls and ensure expired medications were i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review it was determined the facility failed to ensure the call light sytem was functional for 4 of 24 sampled residents (#s 2, 29, 43 and 304) reviewed for...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review it was determined the facility failed to implement care plan interventions to prevent an elopement for 1 of 4 sampled residents (#1) reviewed for elo...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined the facility failed to ensure residents were free from abuse for 1 of 5 sampled residents (#1) reviewed for abuse. This placed residents at risk...
Read full inspector narrative →
Apr 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to ensure physician orders were followed...
Read full inspector narrative →
Apr 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure safety interventions were in place to prevent elopement for 1 of 1 sampled resident (#1) reviewed for ...
Read full inspector narrative →
Dec 2023
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
2. Resident 3 was admitted to the facility in 10/2023 with a diagnosis of cellulitis (a bacterial skin infection).
A review of Resident 3's 10/18/23 admission MDS revealed she/he was cognitively intac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure the Office of the State Long Term Care Ombudsman was notified of resident hospitalization for 1 of 1 sampled reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to comprehensively assess a resident's dental status for 1 of 1 sampled resident (#46) reviewed for dental. This...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to ensure resident call lights were answered timely for 1 of 4 sampled residents (#36) reviewed for sufficient nurse staffing...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure residents were free from a medication error rate of five percent or more for 2 of 8 sampled residents ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
2. The facility's 9/2022 Laundry and Bedding, Soiled Policy Statement indicated the following:
-Clean linen was to be stored separately, away from soiled linens, at all times.
-Clean linen was to be ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0848
(Tag F0848)
Minor procedural issue · This affected most or all residents
Based on interview and record review it was determined the facility failed to ensure arbitration would be held in a location convenient to both the resident and the facility for 1 of 1 facilities revi...
Read full inspector narrative →
Oct 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review the facility failed to ensure a call light system was adequately equipped to relay resident calls to caregivers for assistance on 2 of 2 hallways revi...
Read full inspector narrative →
Sept 2022
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to obtain informed consent prior to administration of a psychotropic medication for 1 of 5 sampled residents (#17) reviewed f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
3. Resident 36 was admitted to the facility in 7/2022 with diagnoses including a left ankle fracture.
Resident 36's 7/29/22 Care Plan indicated Resident 36 required assistance from one person for bath...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure residents with limited ROM received appropriate care and services to maintain their level of functioni...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined the facility failed to ensure a medication administration error rate of less than 5%. There were two errors in 27 opportunities resu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to implement therapy orders in a timely manner for 1 of 1 sampled resident (#20) reviewed for therapy services. This placed r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to develop and implement policies and procedures regarding residents' rights to formulate advance directives for 4 of 4 sampl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected multiple residents
Based on interview and record review it was determined the facility failed to ensure RN coverage for eight consecutive hours per day for 9 of 68 days reviewed for staffing. This placed residents at ri...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review it was determined the facility failed to ensure medications and biologicals we...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review it was determined the facility failed to store food at the appropriate temperature to prevent the spread of food-borne illness and failed to provide ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected most or all residents
Based on interview and record review it was determined the facility failed to ensure staff received annual training on abuse, neglect, exploitation of resident property and dementia management for 9 o...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected most or all residents
Based on interview and record review it was determined the facility failed to have a system in place to ensure CNA staff received 12 hours of in-service training annually for 4 of 5 randomly selected ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • No fines on record. Clean compliance history, better than most Oregon facilities.
- • 34 deficiencies on record. Higher than average. Multiple issues found across inspections.
About This Facility
What is Gateway Care And Retirement's CMS Rating?
CMS assigns GATEWAY CARE AND RETIREMENT an overall rating of 3 out of 5 stars, which is considered average nationally. Within Oregon, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Gateway Care And Retirement Staffed?
CMS rates GATEWAY CARE AND RETIREMENT's staffing level at 3 out of 5 stars, which is average compared to other nursing homes.
What Have Inspectors Found at Gateway Care And Retirement?
State health inspectors documented 34 deficiencies at GATEWAY CARE AND RETIREMENT during 2022 to 2025. These included: 33 with potential for harm and 1 minor or isolated issues.
Who Owns and Operates Gateway Care And Retirement?
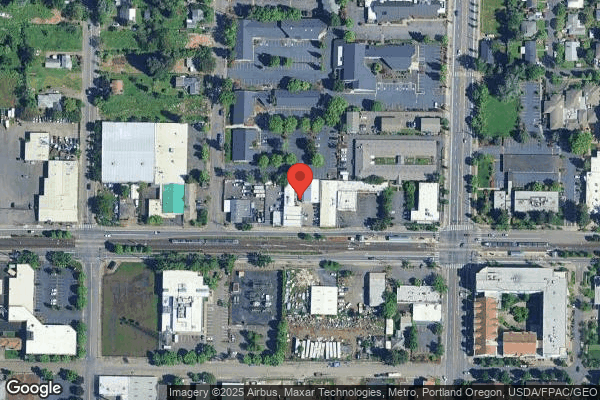
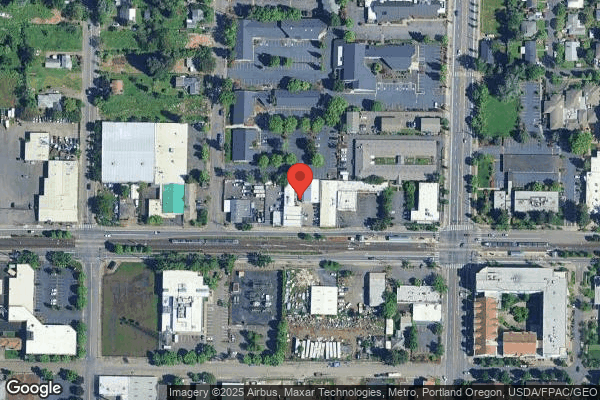
GATEWAY CARE AND RETIREMENT is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by SAPPHIRE HEALTH SERVICES, a chain that manages multiple nursing homes. With 59 certified beds and approximately 54 residents (about 92% occupancy), it is a smaller facility located in PORTLAND, Oregon.
How Does Gateway Care And Retirement Compare to Other Oregon Nursing Homes?
Compared to the 100 nursing homes in Oregon, GATEWAY CARE AND RETIREMENT's overall rating (3 stars) matches the state average and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Gateway Care And Retirement?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Gateway Care And Retirement Safe?
Based on CMS inspection data, GATEWAY CARE AND RETIREMENT has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in Oregon. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Gateway Care And Retirement Stick Around?
GATEWAY CARE AND RETIREMENT has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Gateway Care And Retirement Ever Fined?
GATEWAY CARE AND RETIREMENT has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Gateway Care And Retirement on Any Federal Watch List?
GATEWAY CARE AND RETIREMENT is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.