CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review the facility failed to ensure 1 of 6 residents (Resident #54) reviewed were...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review the facility failed to ensure 1 of 6 residents (Resident #54) reviewed were free from neglect.
1.
On 11/17/24 at 7:03:01 p.m. Resident #54 left the building unnoticed by staff, despite the wander guard alarm alarming at the exit door.
Facility failed to implement immediate action to prevent neglect due to lack of supervision of 6 cognitively impaired individuals with known elopement risk which could result in falls, injuries, dehydration, and death.
An Immediate Jeopardy (IJ) was identified on 12/6/24. The IJ template was provided to the facility on [DATE] at 2:45 pm. While the IJ was removed on 12/7/24, the facility remained out of compliance at a level of potential for more than minimal harm and a scope of isolation, because all staff had not been trained on door codes, what to in case of door alarms, and procedure for a resident elopement.
These failures could affect residents who were identified as elopement risks and place them at risk of serious bodily harm, physical impairment, or death.
The findings included:
Record review of Resident #54's, face sheet dated 12/9/24 revealed a [AGE] year-old female admitted to the facility on [DATE]. Resident #54 had diagnoses which included hypertensive heart disease, hypertension, muscle weakness, schizoaffective disorder, bipolar type, and reduced mobility. The face sheet indicated Resident #54 was discharged on 11/29/24 to another nursing facility.
Record review of Resident #54's quarterly MDS dated [DATE] revealed she had a BIMS of 00, which indicated severe cognitive impairment. Resident #54 required supervision and wore a wander guard.
During an observation of a facility video dated 11/17/24 indicated Resident #54 exited the facility by pushing on the 15 second emergency exit (alarm sounding) at 7:03:00 pm. Resident #54 was wearing a t-shirt, pajama pants, and tennis shoes. CNA A arrived at the door at 7:11:20 pm and exited the building. CNA A was viewed entering back into the building at 7:11:50 pm, indicated 30 seconds elapsed looking for Resident #54. Upon entering back into the building at 7:11:50, CNA A turned off the door alarm and did not do a head count of all residents. Afterwards the facility failed to investigate and take measures to prevent recurrence. Even after Resident #54 was returned to the facility, the facility failed to ensure that residents, who require wander guard bracelets, were monitored, and supervised appropriately to prevent further neglect.
Record review of a progress note of Resident #54 dated 11/18/24 at 12:10 am by ADON LVN . indicated, this ADON LVN received a call regarding resident at 9:46 pm asking if we had a resident by the name of Resident #54. ADON LVN enquired about how resident had come to be at apartment. ADON LVN also brought resident back to facility and facilitated safe return and delegated that agency nurse perform skin assessment and assign one on one monitoring and fill out event for elopement. CNA asked to assist resident out of wet clothes get into dry bed clothes. No injuries or wounds noted. Resident placed on 1 on 1. ADON LVN spoke to CNA A and MD to report elopement and subsequent actions. Resident denies pain or discomfort and just wishes to go to bed. No acute distress noted.
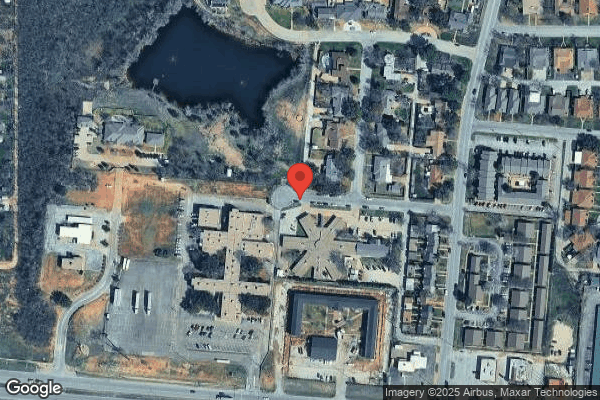
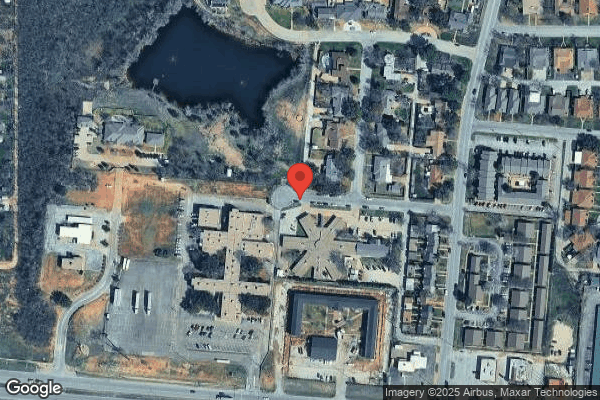
During an interview on 12/5/24 at 3:15 pm, MOTP A stated that on 11/17/24 at roughly 9:15 pm her son came inside and said there was a lady wandering out on the road and in the apartment complex. She stated, he stated she looked lost and confused because she was walking in a circle. She stated, let's go get her. She stated her son went back out in the rain and dark and finally found her and brought her back to the apartment. She stated Resident #54 seemed confused, was cold and shivering. She stated Resident #54 was only wearing a t-shirt, pajama pants, and tennis shoes. She stated she wrapped Resident #54 in a towel and did not recognize her as any of her neighbors. She stated that her son went and got MOTP B to see if she knew who Resident #54 was. She stated when MOTP B showed up they asked Resident #54 some questions and then they found the wander guard on Resident #54's leg. She stated when they found the wander guard, they realized that Resident #54 was probably from the nursing facility across the street. She stated MOTP B called the facility and ADON LVN came and picked Resident #54 up.
During an interview on 12/5/24 at 3:45 pm, MOTP B stated MOTP A's son came to her apartment and stated he saw someone in the parking lot out on the road kind of wandering and walking in a circle out there. She stated it was dark and raining. She stated her primary concerns were to not let her go to highway off the road because they have been having issues with drag racers on that road. She stated that MOTP A's son told her they found Resident #54, she was wandering and they took her inside their apartment. She stated when she got to their apartment Resident #54 was sitting on the couch and wrapped up in a towel and shivering. She stated Resident #54 was wearing a t-shirt, pajama pants, and tennis shoes. She stated she tried to ask Resident #54 her name and where she was from but Resident #54 told her another town and her name. She stated when she came back to the living room MOTP A told her she believed the woman was hurt. She asked MOTP A why and MOTP A told her she had a bandage on her leg. She stated she went to Resident #54 and asked her if she was hurt and if she could look at her leg. She stated that was when she found Resident #54 was not hurt but had a wander guard on, and stated to MOTP A, I bet she was from that facility across the street. She stated she called the facility and asked if they were missing any residents. She stated the woman who answered (ADON LVN) stated no, what were you talking about. She stated were you missing anyone by the name of Resident #54. She stated ADON LVN replied, oh shit and stated she would be right there to pick her up. She stated ADON LVN did come and picked her up immediately.
During an interview at 12/6/24 at 8:40 AM, CNA A stated she was the aid who was in the video. She stated she was helping another resident in their room. She stated when she exited their room, she heard the alarm going off down hallway B. She stated there were two nurses sitting at the nursing station not doing anything. She stated she was not sure how long the alarm had been going off. She stated most of the day, another resident with a wander guard had been setting off the alarm. She stated as she was walking down hallway B and saw the resident and assumed he was the one that set the door off. She stated she went to the door, exited the facility, looked outside, and came back in. She stated she did not see any resident. She stated upon entering back into the building she turned the alarm off. She stated because she saw the other resident, she did not do a head count of the facility for all residents. She stated the two nurses sitting at the nurse's station, stated they did not answer the alarming door because they did not know the codes. She stated that the headcount should have been done for Resident #54's safety. She stated it was lucky that Resident #54 did not get hurt.
Attempted to reach out to agency staffing company on 12/5/24 and 12/6/24, could not contact two nurses notated sitting at nurses' station.
During an interview on 12/6/24 at 10:40 am, LVN A (agency nurse) stated when she first worked for the facility the facility gave her an onboarding packet. She stated the packet did not contain any door codes for the facility. She stated the standard for any facility was if a door alarm was going off and was triggered by a wander guard, move the resident from the door. She stated if the resident that triggered the door was still by the door, move the resident away from the door. She stated if the door was activated and there was no resident near the door, you were to go search outside for the resident. She stated then return inside the building and initiate a resident head count. She stated if the head count was missing any resident, to call the admin, the DON, the charge nurse whoever you can, to inform them of an elopement. She stated at the facility, the codes for the doors were not given. She stated she did not know the codes for any of the doors to go in or out other than the breakroom door. She stated the protocol for any alarming door was to find the resident that set it off. She stated most of the time the resident that triggered the alarm was still standing near the door. She stated but if a door alarm was triggered and the door opened, she would have looked outside first. She stated after she looked outside, if she did not know the door code, she would request help from staff that did know the code. She stated not knowing the code to a door is no excuse to not check the door or on any resident in the area.
During an interview on 12/5/24 at 12:40, pm ADON LVN stated the normal protocol for possible elopement was that if an alarm was sounding at any door in the building the individual (employee) goes to the door. She stated they should go outside to look for the resident. She stated if the resident was still there setting off the alarm to remove the resident from the door and then reset the alarm. She stated that she did not know the full story and has not seen the video. She stated that was the door in which Resident #54 exited through. She stated employee CNA A went and looked outside, came back inside, reset the door alarm, and went back to work. She stated that at roughly 9:40 pm the facility received a call from someone outside the facility. She stated they asked her if they had a resident by the name of Resident #54 that stayed in the facility. She stated that they did. She stated the caller informed her that they had her at the apartment across the street. She stated she would come get Resident #54 immediately. She stated she had no idea what Resident #54 was doing or where exactly the resident went for 2 hours and 40 mins. She stated that rounding should be completed every 2 hours on all residents. She stated she was not sure if a head count was completed for the entire facility on the 17th at 7pm by employee CNA A. She stated multiple times throughout the day there was another resident activating the front door alarm with his wander guard. She stated because the alarm had gone off so many times during the day, the staff was desensitized to the alarm going off in the building. She stated that normally Resident #54 sits at the nurse's station each night after she gets done walking. She stated she believed the facility would have noticed at some point Resident #54 was missing. She stated when she received the call from MOTP B at 9:40 pm, she had the staff initiate a head count of all residents while she went and picked up Resident #54. She stated when she got back to the facility, Resident #54 was taken to her room, her wet clothing was removed, and she was put to bed. She stated to her knowledge no other residents were reviewed or rounded on because Resident #54 was safe and back in the facility. She stated she did not know there were two nurses sitting at the nurse's station did not even check the door. She stated she was lucky that Motp found Resident #54, it could have been much worse if Resident #54 got hurt.
During an interview on 12/6/24 at 11:15 am, ADON LVN stated she did not give out any of the door codes to any agency staff. She stated that there was a list of topics that were covered with the agency staff, she stated but I won't lie to you the topics to cover were done extremely fast so the agency staff can get out on the floor and start working. She stated there was a binder at the nurse's station that had all the door codes and policies/procedures for anyone to pick up and review.
During an observation on 12/6/24 at 11:20 am, there were no policies or procedures in the binder only signature sheets of staff that had completed orientation. No door codes were found in the binder.
During an interview on 12/6/24 at 11:45 am, the DON stated Resident #54 did exit the building through the fire emergency exit door on hallway B at 7:00 pm on 11/17/24. She stated the video showed CNA A go down to the door, exit the building, return inside the building, and turn off the alarm. She stated she was not sure why CNA A did not do a head count of all residents when she deactivated the alarm. She stated she was not sure why the alarm went off for that long of a time. She stated there were 2 agency nurses working that night. She stated her expectation of a door alarm going off should be acknowledged immediately. She stated if the resident was not by the door, the employee should go outside, do an observation around the facility, and look any resident, if no resident was found outside the employee should let the charge nurse and the DON know immediately. She stated that she knew Resident #54 was picked up and brought back to the facility. She stated a head count of all residents was done at 9:40 pm. She stated that Resident #54 was rounded on every 15 minutes. She stated she did not know if all other residents with wander guards were monitored after the return of Resident #54. She stated that all agency staff should have known to go and check the alarming door. She stated it did not matter if the door codes were known or not by any staff. She stated the residents are the priority and should have been checked on. She stated the ADON LVN does all the trainings for the facility. She stated this should never have happened and the head count should have been done.
Record review of facility's policy titled Abuse, Neglect, and exploitation dated 10/2023 inidcated: the facility will provideprotection for the health, welfare, and rights of each resident by developing and implementing written polices and procedures that prohibit and prevent abuse, neglect, and exploitation and misappropriation of resident property.
Record review of facility's policy titled emergency procedure-missing resident dated 10/2023 inidcated: Any staff member may implement the protocol for a missing resident immediately upon discovering that a resident cannot be located. 1. Announce code pink with the resident's room/unit number. 2. Note the time that the resident was dicovered missing. 3. Report to the nursing station to see if the resident was signed out. 4. Notify the admin, dom, and DON, if not on the premises. 5. activate recall roster if necessary.
An Immediate Jeopardy was identified on 12/6/24 at 2:45 pm. The Administrator and DON were informed, and Immediate Jeopardy Template was provided. The Administrator and DON were notified that a Plan of Removal was requested at that time.
A Plan of Removal was accepted on 12/7/24 at 6:03 PM and reflected the following:
1. Immediate Actions Taken for Those Residents Identified:
Action: Resident #54 returned to the nursing home. Resident was assessed with no injuries. Resident behaving per norm. Increased supervision implemented with Resident #54 which included resident in line of sight of an employee at all times until discharge.
Elopement assessment updated. RP & MD informed.
(Resident #54 has since been discharged on 11/29/2024 to a secured unit)
Person(s) Responsible: Charge Nurse, Assistant Director of Nursing, and/or Designee
Date: 11/18/24.
2. How the Facility Identified Other Possibly Affected Residents:
Action: Resident head count performed no additional findings.
Person(s) Responsible: Charge Nurse and/or Designee
Date: 11/17/2024
Action: All residents received an elopement assessment. Residents' current elopement assessment will reflect on their face sheet and care plan.
Person(s) Responsible: Director of Nursing, Assistant Director of Nursing, and/or Designee
Date: 11/18/2024
3. Measures Put into Place/System Changes to remove the immediacy, and what date these actions occurred:
Action: Elopement binder reviewed to ensure it matches the current residents who were deemed as elopement risks per their elopement assessments.
Person(s) Responsible: Director of Nursing and/or Designee
Date: 11/18/2024
Action: Sign on door verified for placement notifying visitors to, Please do not allow residents to follow you out.
Person(s) Responsible: Administrator
Date: 11/18/2024
Action: Sign posted by keypads stating: When alarms were sounding, and the door was disengaged perform a resident head count.
Person(s) Responsible: Director of Regulatory Compliance
Date: 11/18/2024
Action: All doors checked for functionality. No concerns noted.
Person(s) Responsible: Maintenance Director and/or Designee
Date: 11/17/2024
Action: Check for all residents with roam alerts for functionality. No concerns noted.
Person(s) Responsible: Administrator and/or Designee
Date: 11/18/2024.
Action: Elopement drill performed each shift (6a-6p and 6p-6a).
Person(s) Responsible: Administrator, Maintenance Director, and/or Designee
Date: 11/19/2024
Action: Education provided to direct care staff, to include agency staff, regarding missing resident/elopement & over the facility's abuse & neglect policy.
Direct care staff will be educated on the elopement binder, its location, and its contents (shows which residents were elopement risks/wander guard residents).
Direct care staff, including agency staff, will know when the door was alarming, to respond to the alarming door immediately. If the door was disengaged (open) and alarming the direct care staff will ensure all residents were in house by performing a head count (signs placed for reminders for staff to ensure all residents were in house when alarms were sounding, and the door was disengaged by keypads).
Direct care staff, including agency staff, will know the door codes/door code location through this education.
Direct care employees will be educated prior to working their next shift.
All new and temporary direct care staff will be educated prior to working.
Person(s) Responsible: Administrator and/or Designee
Date: 12/6/2024
Action: Residents deemed an elopement risk, that require a roam alert/wander guard will be rounded on every 2 hours to ensure facility was aware of residents' whereabouts.
Person(s) Responsible: Charge Nurse, Certified Nurse's Aides, and/or Designee
Date: 12/6/2024
4. How the Corrective Actions Will be Monitored, by whom, and for how long:
Action: All residents with exit seeking behaviors will be reviewed during clinical meeting to ensure safety. Appropriate supervision will occur until residents with exit seeking behaviors, that have a greater need than the roam alert system, were appropriately placed. No concerns noted.
Person(s) Responsible: Director of Nursing and/or Designee
Date: 11/17/2024
Action: Elopement drill performed weekly x4 weeks to ensure staff's retention of education to prevent recurrence.
Person(s) Responsible: Administrator and/or Designee
Date: 11/17/2024
QAPI-
Action: Ad hoc QAPI performed with medical director to inform them of the incident and the facility's plan to remove the immediacy. No further direction required.
Person(s) Responsible: Administrator
Date: 11/18/2024
State Surveyors monitored the facility's Plan of Removal and confirmed it was sufficient to remove the IJ through observations, interviews, and record reviews from 12/6/24 to 12/7/24 as follows:
Record review of resident assessment:
Record review of progress note of Resident #54 dated 11/18/24 at 12:10 am submitted by ADON LVN indicated, this LVN received a call regarding resident at 9:45 pm asking if we had a resident by the name of Resident #54. ADON LVN enquired about how resident had come to be at apartment. ADON LVN also brought resident back to facility and facilitated safe return and delegated that agency nurse perform skin assessment and assign one on one monitoring and fill out event for elopement. CNA asked to assist resident out of wet clothes get into dry bed clothes. No injuries or wounds noted. Resident placed on 1 on 1. ADON LVN spoke to CNA A and MD to report elopement and subsequent actions. Resident denies pain or discomfort and just wishes to go to bed. No acute distress noted.
Record review of progress notes of Resident #54 dated 11/17/24 at 10:24 pm submitted by ADON LVN indicated:
Resident Refused Skin Assessment: No
Temperature--Location, if applicable.: Warm
Color--Location, if applicable.: Expected color for ethnicity.
Moisture--Location, if applicable.: Dry
Skin Turgor: Normal
Capillary Refill: Less than 3 seconds
Was Resident at risk for developing pressure injuries? No Risk Factors: Moisture, Incontinence
Were contractures present? No
Alterations in Skin Integrity. Note location of any noted areas. Enter measurements in box provided.: None.
Notifications if Applicable: Physician Notified MD, Responsible Resident Representative Notified. Guardian
Interventions: No new or additional interventions required at this time.
[Corporation] Assessment for Risk of Elopement completed 11/18/24. Indicated yes to all:
Does the resident have a diagnosis of Dementia, OBS, Alzheimer's, I/DD, Delusions, Hallucinations, Anxiety, Depression, Schizophrenia, or other Mental Illness? Yes
Does the resident ambulate independently, with or without the use of an assistive device (i.e., walker, cane, or wheelchair)? Yes
If the resident has wandering behavior, was it tied to resident's past (i.e., their prior work, takes long walks, seeking someone they cannot find)? Yes
Was the resident ambulatory (able to walk without someone assisting them) yet cognitively impaired with poor decision-making skills (i.e., intermittent confusion, cognitive deficits, appears disoriented)? Yes
Has the resident verbally expressed the desire to go home, packed belongings to go home, talked about going on a trip, or stayed near an exit door? Yes
Does the resident have a history of leaving the facility without Informing staff? Yes
Does the resident wander without a sense of purpose (i.e., confused, moves aimlessly, may enter other resident rooms, and explore their belongings)? Yes
Record review of observations initiated by the facility on 11/17/24 at 10:07 pm of Resident #54 for increased rounding indicated: times starting at 10:07 pm and every 15min interval after that with sign off sheet until 11:45 pm. Sheet dated 11/18/24 had monitoring every 15min, all day long, no time was missed, signatures provided. Sheet dated 11/19/24 had monitoring every 15min up until 12:00 pm.
Record review of facility Resident head count dated 11/17/24 at 9:40 pm indicated all residents were in the building except Resident #54. At which time ADON LVN was going to pick up Resident #54.
Record review of the facility Resident observation summary report for all residents dated 11/17/24 to 11/19/24 completed for [corporation] assessment for risk of elopement for all residents in the facility completed daily by all nurses in the facility.
Record review of door checks (door locking mechanism) log sheet dated 11/11/24 to 11/15/24 all indicated a pass. Door check log sheet dated 11/18/24 all indicated a pass.
Record review of Code Pink drill documentation form dated 12/6/24 at 5:02 pm indicated all staff acted correctly. Signature pages presented. Record review of Code Pink drill documentation form dated 11/27/24 indicated all staff acted correctly. Signature pages presented.
Record review of drill dated 11/19/24 time stamped 5:30 am indicated: The Administrator hid as an unaccompanied resident which would activate a missing resident situation. Informed staff that we were looking for an unaccounted resident. Verbally alerted staff to the Code Pink status. Staff immediately met at the Nurses Station and received direction from the charge nurse to begin looking for a missing resident. Staff searched all hallways/rooms/dining area/lobby, and closets. Within 5 minutes the Mock resident was found in the kitchen. Signed and dated by the Administrator.
Record review of drill dated 11/18/24 time stamped 5:00 pm indicated: The Maintenance Director chose an employee to hide as an unaccompanied resident which would activate a missing resident situation. Informed staff that we were looking for an unaccompanied resident. Verbally alerted staff to Code Pink status. Staff immediately met at the Nurses Station and received direction from the charge nurse to begin looking for missing resident. Staff searched all hallways/rooms/dining area/lobby, and closets. Within 3 minutes the Mock resident was found in the Beauty Shop. Signed and dated by the Maintenance Director.
Record review of Ad hoc QAPI meeting dated 12/6/24 indicated: An ad hoc QAPI meeting was performed with the MD to review the incident regarding Resident #54. The MD was agreeable with the plan of action. The MD completed a telehealth visit with Resident #54 with no concerns.
Record review on 12/8/24 of Agency orientation to the facility book and for the rest of the staff, located at nurses' station, binder contained: policy's abuse, neglect, and exploitation, wandering and elopement, comprehensive care plans, advanced directives, change in residents' condition or status, fall prevention program, and resident rights. Binder also contained: Note that stated, door codes-if they do not work, please call the admin or the DON, and then list all door codes for the entire facility for going in or out of the facility. Binder also contained completed orientations of nursing and agency staff.
Record review on 12/9/24 of In-service titled visual rotation risk of elopement, led by the Administrator indicated: go into the MAR and check residents that have wander guards. All residents with wander guards were rounded on, the even hours were rounded on by CNA's and odd hours were rounded on by Nurses. The sign off sheet would be reviewed by both the nurses and CNA's when the rounding was completed.
Record review on 12/9/24 of in-service titled Door alarm education and elopement policy, instructed by a group of people, but the Administrator did educate. The Administrator stated the education included door alarms, how to react and what to do. He stated the education included elopement, education, and abuse/neglect. He stated that if the alarm was sounding the door should be observed immediately. He stated then if the door opens even with the alarm going off, the employee should go outside, and check the area. He stated the employee should walk the entire facility and check the surrounding area. He stated if no resident was seen/found the employee was to come back inside, turn off the alarm, make sure door was locked, and then inform staff to initiate a head count for the entire facility. He stated that if the door was alarming and the door did not open to look in the surrounding area inside the building to find the possible resident that set the alarm off and redirect the resident from the door.
Record review on 12/9/24 of in-service titled abuse, neglect, and exploitation, instructed by ADON LVN completed on 11/18/24. ADON LVN stated that due to the elopement the facility did do an in-service on abuse, neglect, and exploitation. She stated during the education she did go over the whole policy, and she discussed with staff what constitutes as abuse, neglect, and exploitation. She stated she also covered what to do if abuse or neglect were to occur and/or was witnessed in the facility. She stated the process was to report any incident directly to the Administrator because he was the abuse neglect coordinator.
During an interview on 12/7/24 at 10:15 am, LVN C (day nurse) stated there were 3 in-services that she could remember but it was basically a big training yesterday while she was on shift. She stated first was elopement and what to do if a door alarm was going off. She stated if a door alarm was going off and opened upon arrival with no resident in site, she would go outside and search the surrounding area. She stated if no resident was found outside, she would return back inside, and inform staff of a possible elopement. She stated she would inform the charge nurse, the DON, or the Administrator of a possible elopement. She stated she would then start a head count of all residents in the facility. She stated there was a binder now at the nurse's station with all the policies and procedures. She stated the binder included abuse neglect, elopement, and other policies and procedures. She stated that one sheet in the book also contained the alarms and codes to all doors in the facility. She stated they also would do rounding on all residents with wander guards every two hours. She stated for abuse/neglect, if she were to witness or observe anything of that nature to separate or remove the resident from the situation, also to immediately inform the Administrator of the incident, and give report to the Administrator.
During an interview on 12/7/24 at 10:25 am, CNA B (Day shift) stated she did have to do in-services before she could come on to work today. She stated the categories of the in-services included elopement, where to find guidance, and abuse/neglect. She stated the main topic at hand was what to do if a door alarm was going off in the facility. She stated they emphasized the importance of going to the door immediately and checking for any residents at the door. She stated if a resident with a wander guard was still at the door and the door was still locked to re-direct the resident away from the door. She stated but if the door alarm was going off and the door could open, it was vital to go outside, and look for the resident. She stated if no resident was found outside, she was to inform staff to start a resident head count. She stated the second topic was where to find all the policies and procedures in the building. She stated there was a new binder at the nurse's station that contained all the policies and procedures for given situations. She stated also within the binder were all the codes for all the doors in the building.
During an interview on 12/7/24 at 10:30 am, LVN D (Night Nurse) stated before he was allowed to work last night he had to go through a few trainings. He stated he used to be an agency nurse, but now worked full time for the facility. He stated he forgot his phone at work, so he was here at this time. He stated most of the trainings were related to door alarms in the facility. He stated if an alarm was going off in the facility, he was to immediately check the door. He stated if the resident that set off the alarm was still in the area and the door was still locked then he was to re-direct the resident from the door. He stated however, if the door alarm was going off and the door opens, even if there was a resident with a wander guard standing next to the door, he was to go outside the facility and look around the building. He stated if no resident was found outside, he was to turn off the door alarm, make sure the door locks, and get with all the staff to do a resident head count. He stated he was also in-serviced on a new binder that would be at the nurse's station. He stated the new binder contained all the door codes and alarms. He stated the binder also contained all the policies and procedures given for different situation, like a quick reference guide. He stated other than that the last in-service was related to abuse/neglect. He stated it went over what to look for, how to react, and who to report to if he were to witness anything like that.
During an interview on 12/7/24 at 10:35 am, RN A (Day Nurse) she stated there were 3 total in-services. She stated there was training about elopement and risk of elopement for residents in the facility. She stated, for example if there was a door going off in the facility to immediately go and check the door. She stated if the resident who set the alarm off was still standing there, to redirect the resident. She stated however if there was no resident at the door and the alarm[TRUNCATED]
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Abuse Prevention Policies
(Tag F0607)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review the facility failed to ensure implementation of written policies and proced...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review the facility failed to ensure implementation of written policies and procedures that prohibit and prevent neglect for 1 of 6 residents (Resident #54) reviewed were free from neglect.
1. On 11/17/24 at 7:03:01 p.m. Resident #54 left the building unnoticed by staff, despite the wander guard alarm alarming at the exit door.
2. Facility failed to follow policy for emergency procedure-missing resident.
3. Facility failed to implement immediate action to prevent neglect due to lack of supervision of 6 cognitively impaired individuals with known elopement risk which could result in falls, injuries, dehydration, and death.
An Immediate Jeopardy (IJ) was identified on 12/6/24. The IJ template was provided to the facility on [DATE] at 2:45 pm. While the IJ was removed on 12/7/24, the facility remained out of compliance at a level of potential for more than minimal harm and a scope of isolation, because all staff had not been trained on door codes, what to in case of door alarms, and procedure for a resident elopement.
These failures could affect residents who were identified as elopement risks and place them at risk of serious bodily harm, physical impairment, or death.
The findings included:
Record review of Resident #54's, face sheet dated 12/9/24 revealed a [AGE] year-old female admitted to the facility on [DATE]. Resident #54 had diagnoses which included hypertensive heart disease, hypertension, muscle weakness, schizoaffective disorder, bipolar type, and reduced mobility. The face sheet indicated Resident #54 was discharged on 11/29/24 to another nursing facility.
Record review of Resident #54's quarterly MDS dated [DATE] revealed she had a BIMS of 00, which indicated severe cognitive impairment. Resident #54 required supervision and wore a wander guard.
During an observation of a facility video dated 11/17/24 indicated Resident #54 exited the facility by pushing on the 15 second emergency exit (alarm sounding) at 7:03:00 pm. Resident #54 was wearing a t-shirt, pajama pants, and tennis shoes. CNA A arrived at the door at 7:11:20 pm and exited the building. CNA A was viewed entering back into the building at 7:11:50 pm, indicated 30 seconds elapsed looking for Resident #54. Upon entering back into the building at 7:11:50, CNA A turned off the door alarm and did not do a head count of all residents. Afterwards the facility failed to investigate and take measures to prevent recurrence. Even after Resident #54 was returned to the facility, the facility failed to ensure that residents, who require wander guard bracelets, were monitored, and supervised appropriately to prevent further neglect.
Record review of a progress note of Resident #54 dated 11/18/24 at 12:10 am by ADON LVN . indicated, this ADON LVN received a call regarding resident at 9:46 pm asking if we had a resident by the name of Resident #54. ADON LVN enquired about how resident had come to be at apartment. ADON LVN also brought resident back to facility and facilitated safe return and delegated that agency nurse perform skin assessment and assign one on one monitoring and fill out event for elopement. CNA asked to assist resident out of wet clothes get into dry bed clothes. No injuries or wounds noted. Resident placed on 1 on 1. ADON LVN spoke to CNA A and MD to report elopement and subsequent actions. Resident denies pain or discomfort and just wishes to go to bed. No acute distress noted.
During an interview on 12/5/24 at 3:15 pm, MOTP A stated that on 11/17/24 at roughly 9:15 pm her son came inside and said there was a lady wandering out on the road and in the apartment complex. She stated, he stated she looked lost and confused because she was walking in a circle. She stated, let's go get her. She stated her son went back out in the rain and dark and finally found her and brought her back to the apartment. She stated Resident #54 seemed confused, was cold and shivering. She stated Resident #54 was only wearing a t-shirt, pajama pants, and tennis shoes. She stated she wrapped Resident #54 in a towel and did not recognize her as any of her neighbors. She stated that her son went and got MOTP B to see if she knew who Resident #54 was. She stated when MOTP B showed up they asked Resident #54 some questions and then they found the wander guard on Resident #54's leg. She stated when they found the wander guard, they realized that Resident #54 was probably from the nursing facility across the street. She stated MOTP B called the facility and ADON LVN came and picked Resident #54 up.
During an interview on 12/5/24 at 3:45 pm, MOTP B stated MOTP A's son came to her apartment and stated he saw someone in the parking lot out on the road kind of wandering and walking in a circle out there. She stated it was dark and raining. She stated her primary concerns were to not let her go to highway off the road because they have been having issues with drag racers on that road. She stated that MOTP A's son told her they found Resident #54, she was wandering, and they took her inside their apartment. She stated when she got to their apartment Resident #54 was sitting on the couch and wrapped up in a towel and shivering. She stated Resident #54 was wearing a t-shirt, pajama pants, and tennis shoes. She stated she tried to ask Resident #54 her name and where she was from but Resident #54 told her another town and her name. She stated when she came back to the living room MOTP A told her she believed the woman was hurt. She asked MOTP A why and MOTP A told her she had a bandage on her leg. She stated she went to Resident #54 and asked her if she was hurt and if she could look at her leg. She stated that was when she found Resident #54 was not hurt but had a wander guard on, and stated to MOTP A, I bet she was from that facility across the street. She stated she called the facility and asked if they were missing any residents. She stated the woman who answered (ADON LVN) stated no, what were you talking about. She stated were you missing anyone by the name of Resident #54. She stated ADON LVN replied, oh shit and stated she would be right there to pick her up. She stated ADON LVN did come and picked her up immediately.
During an interview at 12/6/24 at 8:40 AM, CNA A stated she was the aid who was in the video. She stated she was helping another resident in their room. She stated when she exited their room, she heard the alarm going off down hallway B. She stated there were two nurses sitting at the nursing station not doing anything. She stated she was not sure how long the alarm had been going off. She stated most of the day, another resident with a wander guard had been setting off the alarm. She stated as she was walking down hallway B and saw the resident and assumed he was the one that set the door off. She stated she went to the door, exited the facility, looked outside, and came back in. She stated she did not see any resident. She stated upon entering back into the building she turned the alarm off. She stated because she saw the other resident, she did not do a head count of the facility for all residents. She stated the two nurses sitting at the nurse's station, stated they did not answer the alarming door because they did not know the codes. She stated that the headcount should have been done for Resident #54's safety. She stated it was lucky that Resident #54 did not get hurt.
Attempted to reach out to agency staffing company on 12/5/24 and 12/6/24, could not contact two nurses notated sitting at nurses' station.
During an interview on 12/6/24 at 10:40 am, LVN A (agency nurse) stated when she first worked for the facility the facility gave her an onboarding packet. She stated the packet did not contain any door codes for the facility. She stated the standard for any facility was if a door alarm was going off and was triggered by a wander guard, move the resident from the door. She stated if the resident that triggered the door was still by the door, move the resident away from the door. She stated if the door was activated and there was no resident near the door, you were to go search outside for the resident. She stated then return inside the building and initiate a resident head count. She stated if the head count was missing any resident, to call the admin, the DON, the charge nurse whoever you can, to inform them of an elopement. She stated at the facility, the codes for the doors were not given. She stated she did not know the codes for any of the doors to go in or out other than the breakroom door. She stated the protocol for any alarming door was to find the resident that set it off. She stated most of the time the resident that triggered the alarm was still standing near the door. She stated but if a door alarm was triggered and the door opened, she would have looked outside first. She stated after she looked outside, if she did not know the door code, she would request help from staff that did know the code. She stated not knowing the code to a door is no excuse to not check the door or on any resident in the area. She stated that the policy is to check any door that was alarmed as fast as possible. She stated that was the number one rule with a door that was alarmed, find the resident than shut off the alarm.
During an interview on 12/5/24 at 12:40, pm ADON LVN stated the normal protocol for possible elopement was that if an alarm was sounding at any door in the building the individual (employee) goes to the door. She stated they should go outside to look for the resident. She stated if the resident was still there setting off the alarm to remove the resident from the door and then reset the alarm. She stated that she did not know the full story and has not seen the video. She stated that was the door in which Resident #54 exited through. She stated employee CNA A went and looked outside, came back inside, reset the door alarm, and went back to work. She stated that at roughly 9:40 pm the facility received a call from someone outside the facility. She stated they asked her if they had a resident by the name of Resident #54 that stayed in the facility. She stated that they did. She stated the caller informed her that they had her at the apartment across the street. She stated she would come get Resident #54 immediately. She stated she had no idea what Resident #54 was doing or where exactly the resident went for 2 hours and 40 mins. She stated that rounding should be completed every 2 hours on all residents. She stated she was not sure if a head count was completed for the entire facility on the 17th at 7pm by employee CNA A. She stated multiple times throughout the day there was another resident activating the front door alarm with his wander guard. She stated because the alarm had gone off so many times during the day, the staff was desensitized to the alarm going off in the building. She stated that normally Resident #54 sits at the nurse's station each night after she gets done walking. She stated she believed the facility would have noticed at some point Resident #54 was missing. She stated when she received the call from MOTP B at 9:40 pm, she had the staff initiate a head count of all residents while she went and picked up Resident #54. She stated when she got back to the facility, Resident #54 was taken to her room, her wet clothing was removed, and she was put to bed. She stated to her knowledge no other residents were reviewed or rounded on because Resident #54 was safe and back in the facility. She stated she did not know there were two nurses sitting at the nurse's station did not even check the door. She stated she was lucky that Motp found Resident #54, it could have been much worse if Resident #54 got hurt. She stated the protocol was to check the alarmed door, find the resident, and then initiate a head count. She stated this was not done. She stated the policy for missing resident was not followed. She stated the fact that CNA A went to the door and did not do a headcount was not following the policy.
During an observation on 12/6/24 at 11:20 am, there were no policies or procedures in the binder only signature sheets of staff that had completed orientation. No door codes were found in the binder.
During an interview on 12/6/24 at 11:45 am, the DON stated Resident #54 did exit the building through the fire emergency exit door on hallway B at 7:00 pm on 11/17/24. She stated the video showed CNA A go down to the door, exit the building, return inside the building, and turn off the alarm. She stated she was not sure why CNA A did not do a head count of all residents when she deactivated the alarm. She stated she was not sure why the alarm went off for that long of a time. She stated there were 2 agency nurses working that night. She stated her expectation of a door alarm going off should be acknowledged immediately. She stated if the resident was not by the door, the employee should go outside, do an observation around the facility, and look any resident, if no resident was found outside the employee should let the charge nurse and the DON know immediately. She stated that she knew Resident #54 was picked up and brought back to the facility. She stated a head count of all residents was done at 9:40 pm. She stated that Resident #54 was rounded on every 15 minutes. She stated she did not know if all other residents with wander guards were monitored after the return of Resident #54. She stated that all agency staff should have known to go and check the alarming door. She stated it did not matter if the door codes were known or not by any staff. She stated the residents are the priority and should have been checked on. She stated the ADON LVN does all the trainings for the facility. She stated this should never have happened and the head count should have been done. She stated that the CNA A should have done a head count, because this was not done, she did not follow the policy for the facility with a missing resident.
Record review of facility's policy titled Abuse, Neglect, and exploitation dated 10/2023 indicated: the facility will provide protection for the health, welfare, and rights of each resident by developing and implementing written policies and procedures that prohibit and prevent abuse, neglect, and exploitation and misappropriation of resident property.
An Immediate Jeopardy was identified on 12/6/24 at 2:45 pm. The Administrator and DON were informed, and Immediate Jeopardy Template was provided. The Administrator and DON were notified that a Plan of Removal was requested at that time.
A Plan of Removal was accepted on 12/7/24 at 6:03 PM and reflected the following:
1. Immediate Actions Taken for Those Residents Identified:
Action: Resident #54 returned to the nursing home. Resident was assessed with no injuries. Resident behaving per norm. Increased supervision implemented with Resident #54 which included resident in line of sight of an employee at all times until discharge.
Elopement assessment updated. RP & MD informed.
(Resident #54 has since been discharged on 11/29/2024 to a secured unit)
Person(s) Responsible: Charge Nurse, Assistant Director of Nursing, and/or Designee
Date: 11/18/24.
2. How the Facility Identified Other Possibly Affected Residents:
Action: Resident head count performed no additional findings.
Person(s) Responsible: Charge Nurse and/or Designee
Date: 11/17/2024
Action: All residents received an elopement assessment. Residents' current elopement assessment will reflect on their face sheet and care plan.
Person(s) Responsible: Director of Nursing, Assistant Director of Nursing, and/or Designee
Date: 11/18/2024
3. Measures Put into Place/System Changes to remove the immediacy, and what date these actions occurred:
Action: Elopement binder reviewed to ensure it matches the current residents who were deemed as elopement risks per their elopement assessments.
Person(s) Responsible: Director of Nursing and/or Designee
Date: 11/18/2024
Action: Sign on door verified for placement notifying visitors to, Please do not allow residents to follow you out.
Person(s) Responsible: Administrator
Date: 11/18/2024
Action: Sign posted by keypads stating: When alarms were sounding, and the door was disengaged perform a resident head count.
Person(s) Responsible: Director of Regulatory Compliance
Date: 11/18/2024
Action: All doors checked for functionality. No concerns noted.
Person(s) Responsible: Maintenance Director and/or Designee
Date: 11/17/2024
Action: Check for all residents with roam alerts for functionality. No concerns noted.
Person(s) Responsible: Administrator and/or Designee
Date: 11/18/2024.
Action: Elopement drill performed each shift (6a-6p and 6p-6a).
Person(s) Responsible: Administrator, Maintenance Director, and/or Designee
Date: 11/19/2024
Action: Education provided to direct care staff, to include agency staff, regarding missing resident/elopement & over the facility's abuse & neglect policy.
Direct care staff will be educated on the elopement binder, its location, and its contents (shows which residents were elopement risks/wander guard residents).
Direct care staff, including agency staff, will know when the door was alarming, to respond to the alarming door immediately. If the door was disengaged (open) and alarming the direct care staff will ensure all residents were in house by performing a head count (signs placed for reminders for staff to ensure all residents were in house when alarms were sounding, and the door was disengaged by keypads).
Direct care staff, including agency staff, will know the door codes/door code location through this education.
Direct care employees will be educated prior to working their next shift.
All new and temporary direct care staff will be educated prior to working.
Person(s) Responsible: Administrator and/or Designee
Date: 12/6/2024
Action: Residents deemed an elopement risk, that require a roam alert/wander guard will be rounded on every 2 hours to ensure facility was aware of residents' whereabouts.
Person(s) Responsible: Charge Nurse, Certified Nurse's Aides, and/or Designee
Date: 12/6/2024
4. How the Corrective Actions Will be Monitored, by whom, and for how long:
Action: All residents with exit seeking behaviors will be reviewed during clinical meeting to ensure safety. Appropriate supervision will occur until residents with exit seeking behaviors, that have a greater need than the roam alert system, were appropriately placed. No concerns noted.
Person(s) Responsible: Director of Nursing and/or Designee
Date: 11/17/2024
Action: Elopement drill performed weekly x4 weeks to ensure staff's retention of education to prevent recurrence.
Person(s) Responsible: Administrator and/or Designee
Date: 11/17/2024
QAPI-
Action: Ad hoc QAPI performed with medical director to inform them of the incident and the facility's plan to remove the immediacy. No further direction required.
Person(s) Responsible: Administrator
Date: 11/18/2024
State Surveyors monitored the facility's Plan of Removal and confirmed it was sufficient to remove the IJ through observations, interviews, and record reviews from 12/6/24 to 12/7/24 as follows:
Record review of resident assessment:
Record review of progress note of Resident #54 dated 11/18/24 at 12:10 am submitted by ADON LVN indicated, this LVN received a call regarding resident at 9:45 pm asking if we had a resident by the name of Resident #54. ADON LVN enquired about how resident had come to be at apartment. ADON LVN also brought resident back to facility and facilitated safe return and delegated that agency nurse perform skin assessment and assign one on one monitoring and fill out event for elopement. CNA asked to assist resident out of wet clothes get into dry bed clothes. No injuries or wounds noted. Resident placed on 1 on 1. ADON LVN spoke to CNA A and MD to report elopement and subsequent actions. Resident denies pain or discomfort and just wishes to go to bed. No acute distress noted.
Record review of progress notes of Resident #54 dated 11/17/24 at 10:24 pm submitted by ADON LVN indicated:
Resident Refused Skin Assessment: No
Temperature--Location, if applicable.: Warm
Color--Location, if applicable.: Expected color for ethnicity.
Moisture--Location, if applicable.: Dry
Skin Turgor: Normal
Capillary Refill: Less than 3 seconds
Was Resident at risk for developing pressure injuries? No Risk Factors: Moisture, Incontinence
Were contractures present? No
Alterations in Skin Integrity. Note location of any noted areas. Enter measurements in box provided.: None.
Notifications if Applicable: Physician Notified MD, Responsible Resident Representative Notified. Guardian
Interventions: No new or additional interventions required at this time.
[Corporation] Assessment for Risk of Elopement completed 11/18/24. Indicated yes to all:
Does the resident have a diagnosis of Dementia, OBS, Alzheimer's, I/DD, Delusions, Hallucinations, Anxiety, Depression, Schizophrenia, or other Mental Illness? Yes
Does the resident ambulate independently, with or without the use of an assistive device (i.e., walker, cane, or wheelchair)? Yes
If the resident has wandering behavior, was it tied to resident's past (i.e., their prior work, takes long walks, seeking someone they cannot find)? Yes
Was the resident ambulatory (able to walk without someone assisting them) yet cognitively impaired with poor decision-making skills (i.e., intermittent confusion, cognitive deficits, appears disoriented)? Yes
Has the resident verbally expressed the desire to go home, packed belongings to go home, talked about going on a trip, or stayed near an exit door? Yes
Does the resident have a history of leaving the facility without Informing staff? Yes
Does the resident wander without a sense of purpose (i.e., confused, moves aimlessly, may enter other resident rooms, and explore their belongings)? Yes
Record review of observations initiated by the facility on 11/17/24 at 10:07 pm of Resident #54 for increased rounding indicated: times starting at 10:07 pm and every 15min interval after that with sign off sheet until 11:45 pm. Sheet dated 11/18/24 had monitoring every 15min, all day long, no time was missed, signatures provided. Sheet dated 11/19/24 had monitoring every 15min up until 12:00 pm.
Record review of facility Resident head count dated 11/17/24 at 9:40 pm indicated all residents were in the building except Resident #54. At which time ADON LVN was going to pick up Resident #54.
Record review of the facility Resident observation summary report for all residents dated 11/17/24 to 11/19/24 completed for [corporation] assessment for risk of elopement for all residents in the facility completed daily by all nurses in the facility.
Record review of door checks (door locking mechanism) log sheet dated 11/11/24 to 11/15/24 all indicated a pass. Door check log sheet dated 11/18/24 all indicated a pass.
Record review of Code Pink drill documentation form dated 12/6/24 at 5:02 pm indicated all staff acted correctly. Signature pages presented. Record review of Code Pink drill documentation form dated 11/27/24 indicated all staff acted correctly. Signature pages presented.
Record review of drill dated 11/19/24 time stamped 5:30 am indicated: The Administrator hid as an unaccompanied resident which would activate a missing resident situation. Informed staff that we were looking for an unaccounted resident. Verbally alerted staff to the Code Pink status. Staff immediately met at the Nurses Station and received direction from the charge nurse to begin looking for a missing resident. Staff searched all hallways/rooms/dining area/lobby, and closets. Within 5 minutes the Mock resident was found in the kitchen. Signed and dated by the Administrator.
Record review of drill dated 11/18/24 time stamped 5:00 pm indicated: The Maintenance Director chose an employee to hide as an unaccompanied resident which would activate a missing resident situation. Informed staff that we were looking for an unaccompanied resident. Verbally alerted staff to Code Pink status. Staff immediately met at the Nurses Station and received direction from the charge nurse to begin looking for missing resident. Staff searched all hallways/rooms/dining area/lobby, and closets. Within 3 minutes the Mock resident was found in the Beauty Shop. Signed and dated by the Maintenance Director.
Record review of Ad hoc QAPI meeting dated 12/6/24 indicated: An ad hoc QAPI meeting was performed with the MD to review the incident regarding Resident #54. The MD was agreeable with the plan of action. The MD completed a telehealth visit with Resident #54 with no concerns.
Record review on 12/8/24 of Agency orientation to the facility book and for the rest of the staff, located at nurses' station, binder contained: policy's abuse, neglect, and exploitation, wandering and elopement, comprehensive care plans, advanced directives, change in residents' condition or status, fall prevention program, and resident rights. Binder also contained: Note that stated, door codes-if they do not work, please call the admin or the DON, and then list all door codes for the entire facility for going in or out of the facility. Binder also contained completed orientations of nursing and agency staff.
Record review on 12/9/24 of In-service titled visual rotation risk of elopement, led by the Administrator indicated: go into the MAR and check residents that have wander guards. All residents with wander guards were rounded on, the even hours were rounded on by CNA's and odd hours were rounded on by Nurses. The sign off sheet would be reviewed by both the nurses and CNA's when the rounding was completed.
Record review on 12/9/24 of in-service titled Door alarm education and elopement policy, instructed by a group of people, but the Administrator did educate. The Administrator stated the education included door alarms, how to react and what to do. He stated the education included elopement, education, and abuse/neglect. He stated that if the alarm was sounding the door should be observed immediately. He stated then if the door opens even with the alarm going off, the employee should go outside, and check the area. He stated the employee should walk the entire facility and check the surrounding area. He stated if no resident was seen/found the employee was to come back inside, turn off the alarm, make sure door was locked, and then inform staff to initiate a head count for the entire facility. He stated that if the door was alarming and the door did not open to look in the surrounding area inside the building to find the possible resident that set the alarm off and redirect the resident from the door.
Record review on 12/9/24 of in-service titled abuse, neglect, and exploitation, instructed by ADON LVN completed on 11/18/24. ADON LVN stated that due to the elopement the facility did do an in-service on abuse, neglect, and exploitation. She stated during the education she did go over the whole policy, and she discussed with staff what constitutes as abuse, neglect, and exploitation. She stated she also covered what to do if abuse or neglect were to occur and/or was witnessed in the facility. She stated the process was to report any incident directly to the Administrator because he was the abuse neglect coordinator.
During an interview on 12/7/24 at 10:15 am, LVN C (day nurse) stated there were 3 in-services that she could remember but it was basically a big training yesterday while she was on shift. She stated first was elopement and what to do if a door alarm was going off. She stated if a door alarm was going off and opened upon arrival with no resident in site, she would go outside and search the surrounding area. She stated if no resident was found outside, she would return back inside, and inform staff of a possible elopement. She stated she would inform the charge nurse, the DON, or the Administrator of a possible elopement. She stated she would then start a head count of all residents in the facility. She stated there was a binder now at the nurse's station with all the policies and procedures. She stated the binder included abuse neglect, elopement, and other policies and procedures. She stated that one sheet in the book also contained the alarms and codes to all doors in the facility. She stated they also would do rounding on all residents with wander guards every two hours. She stated for abuse/neglect, if she were to witness or observe anything of that nature to separate or remove the resident from the situation, also to immediately inform the Administrator of the incident, and give report to the Administrator.
During an interview on 12/7/24 at 10:25 am, CNA B (Day shift) stated she did have to do in-services before she could come on to work today. She stated the categories of the in-services included elopement, where to find guidance, and abuse/neglect. She stated the main topic at hand was what to do if a door alarm was going off in the facility. She stated they emphasized the importance of going to the door immediately and checking for any residents at the door. She stated if a resident with a wander guard was still at the door and the door was still locked to re-direct the resident away from the door. She stated but if the door alarm was going off and the door could open, it was vital to go outside, and look for the resident. She stated if no resident was found outside, she was to inform staff to start a resident head count. She stated the second topic was where to find all the policies and procedures in the building. She stated there was a new binder at the nurse's station that contained all the policies and procedures for given situations. She stated also within the binder were all the codes for all the doors in the building.
During an interview on 12/7/24 at 10:30 am, LVN D (Night Nurse) stated before he was allowed to work last night he had to go through a few trainings. He stated he used to be an agency nurse, but now worked full time for the facility. He stated he forgot his phone at work, so he was here at this time. He stated most of the trainings were related to door alarms in the facility. He stated if an alarm was going off in the facility, he was to immediately check the door. He stated if the resident that set off the alarm was still in the area and the door was still locked then he was to re-direct the resident from the door. He stated however, if the door alarm was going off and the door opens, even if there was a resident with a wander guard standing next to the door, he was to go outside the facility and look around the building. He stated if no resident was found outside, he was to turn off the door alarm, make sure the door locks, and get with all the staff to do a resident head count. He stated he was also in-serviced on a new binder that would be at the nurse's station. He stated the new binder contained all the door codes and alarms. He stated the binder also contained all the policies and procedures given for different situation, like a quick reference guide. He stated other than that the last in-service was related to abuse/neglect. He stated it went over what to look for, how to react, and who to report to if he were to witness anything like that.
During an interview on 12/7/24 at 10:35 am, RN A (Day Nurse) she stated there were 3 total in-services. She stated there was training about elopement and risk of elopement for residents in the facility. She stated, for example if there was a door going off in the facility to immediately go and check the door. She stated if the resident who set the alarm off was still standing there, to redirect the resident. She stated however if there was no resident at the door and the alarm was sounding, she would exit the facility. She stated she would search the surrounding area for any possible residents. She stated she would return inside and start a head count of all residents in the facility. She stated if there was no resident found, to turn the [TRUNCATED]
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure each resident received adequate supervision ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure each resident received adequate supervision and assistive devices to prevent accidents for 2 (Resident #54, Resident #52) of 6 residents reviewed.
1.
The facility failed to provide supervision for Resident # 54, who had a history of exit seeking behaviors, to prevent her from eloping from the facility on 11/17/24.
2.
The facility failed to ensure that smoking materials (lighters, cigarettes) were not stored properly for 1 (Resident #52) of 17 residents listed as smokers.
An Immediate Jeopardy (IJ) was identified on 12/6/24. The IJ template was provided to the facility on [DATE] at 2:45 pm. While the IJ was removed on 12/7/24, the facility remained out of compliance at a level of potential for more than minimal harm and a scope of pattern, because all staff had not been trained on door codes, what to in case of door alarms, and procedure for a resident elopement.
These failures could affect residents who were identified as elopement and smoking risks and placed them at risk of serious bodily harm, physical impairment, or death.
The findings included:
Record review of Resident #54's, face sheet dated 12/9/24 revealed a [AGE] year-old female admitted to the facility on [DATE]. Resident #59 had diagnoses which included hypertensive heart disease, hypertension, muscle weakness, schizoaffective disorder, bipolar type, and reduced mobility. The face sheet indicated Resident #54 was discharged on 11/29/24 to another nursing facility.
Record review of Resident #54's quarterly MDS dated [DATE] revealed she had a BIMS of 00, which indicated severe cognitive impairment. Resident #54 required supervision and wore a wander guard.
During an observation of facility video dated 11/17/24 indicated Resident #54 exited facility by pushing on 15 second emergency exit (alarm sounding) at 7:03:00 pm. Resident #54 was wearing a t-shirt, pajama pants and tennis shoes. CNA A arrives at door at 7:11:20 pm exits the building. CNA A was viewed entering back into building at 7:11:50 pm indicated 30 seconds elapsed looking for Resident #54. Upon entering back into building at 7:11:50 CNA A turned off door alarm and does not do a head count of all residents.
Record review of progress note of Resident #54 dated 11/18/24 at 12:10 am by ADON LVN . indicated, this ADON LVN received a call regarding resident at 9:46 pm asking if we had a resident by the name of Resident #54. ADON LVN enquired about how resident had come to be at apartment. ADON LVN also brought resident back to facility and facilitated safe return and delegated that agency nurse perform skin assessment and assign one on one monitoring and fill out event for elopement. CNA asked to assist resident out of wet clothes get into dry bed clothes. No injuries or wounds noted. Resident placed on 1 on 1. ADON LVN spoke to CNA A and MD to report elopement and subsequent actions. Resident denies pain or discomfort and just wishes to go to bed. No acute distress noted.
During an interview on 12/5/4 at 3:15 pm, Motp A stated that on 11/17/24 at roughly 9:15 pm her son came inside and said there was a lady wandering out on the road and in the apartment complex. She stated, he stated she looked lost and confused because she was walking in a circle. She stated, let's go get her. She stated her son went back out in the rain and dark and finally found her and brought her back to the apartment. She stated Resident #54 seemed confused, was cold and shivering. She stated Resident #54 was only wearing a t-shirt, pajama pants and tennis shoes. She stated she wrapped Resident #54 in a towel and did not recognize her as any of her neighbors. She stated that her son went and got the apartment manager Motp B to see if she knew who Resident #54 was. She stated when Motp B showed up they asked Resident #54 some questions and then they found the wander guard on Resident #54's leg. She stated when they found the wander guard, they realized that Resident #54 was probably from the nursing facility across the street. She stated Motp B called the facility and ADON LVN came and picked Resident #54 up.
During an interview on 12/5/24 at 3:45 pm, Motp B stated Motp A's son came to her apartment and stated he saw someone in the parking lot out on the road kind of wandering and walking in a circle out there. She stated it was dark and raining. She stated her primary concerns was to not let her go to highway off the road because they have been having issues with drag racers on that road. She stated that Motp A's son told her they found Resident #54 was wandering and took her inside their apartment. She stated when she got to their apartment Resident #54 was sitting on the couch and wrapped up in a towel and shivering. She stated Resident #54 was wearing a t-shirt, pajama pants, and tennis shoes. She stated she tried to ask Resident #54 her name and where she was from but Resident #54 told her another town and her name. She stated when she came back to the living room Motp A told her she believed the woman was hurt. She asked Motp A why and Motp A told her she had a bandage on her leg. She stated she went to Resident #54 and asked her if she was hurt and if she could look at her leg. She stated that was when she found Resident #54 was not hurt but had a wander guard on, and stated to Motp A, I bet she was from that facility across the street. She stated she called the facility and asked if they were missing any residents. She stated the woman who answered (ADON LVN) stated no, what were you talking about. She stated were you missing anyone by the name of Resident #54. She stated ADON LVN replied, oh shit and stated she would be right there to pick her up. She stated ADON LVN did come and picked her up immediately.
During an interview at 12/6/24 at 8:40 AM, CNA A stated she was the aid who was in the video. She stated she was helping another resident in their room. She stated when she exited their room, she heard the alarm going off down hallway B. She stated there were two nurses sitting at the nursing station not doing anything. She stated she was not sure how long the alarm had been going off. She stated most of the day, another resident with a wander guard had been setting off the alarm. She stated as she was walking down hallway B and saw the resident and assumed he was the one that set the door off. She stated she went to the door, exited the facility, looked outside, and came back in. She stated she did not see any resident. She stated upon entering back into the building she turned the alarm off. She stated because she saw the other resident, she did not do a head count of the facility for all residents. She stated the two nurses sitting at the nurse's station, stated they did not answer the alarming door because they did not know the codes. She stated that the headcount should have been done for Resident #54's safety. She stated it was lucky that Resident #54 did not get hurt.
During an interview on 12/5/24 at 12:40, pm ADON LVN stated the normal protocol for possible elopement was that if an alarm was sounding at any door in the building the individual (employee) goes to the door. She stated they should go outside to look for the resident. She stated if the resident was still there setting off the alarm to remove the resident from the door and then reset the alarm. She stated that she did not know the full story and has not seen the video. She stated that was the door in which Resident #54 exited through. She stated employee CNA A went and looked outside, came back inside, reset the door alarm, and went back to work. She stated that at roughly 9:40 pm the facility received a call from someone outside the facility. She stated they asked her if they had a resident by the name of Resident #54 that stayed in the facility. She stated that they did. She stated the caller informed her that they had her at the apartment across the street. She stated she would come get Resident #54 immediately. She stated she had no idea what Resident #54 was doing or where exactly the resident went for 2 hours and 40 mins. She stated that rounding should be completed every 2 hours on all residents. She stated she was not sure if a head count was completed for the entire facility on the 17th at 7pm by employee CNA A. She stated multiple times throughout the day there was another resident activating the front door alarm with his wander guard. She stated because the alarm had gone off so many times during the day, the staff was desensitized to the alarm going off in the building. She stated that normally Resident #54 sits at the nurse's station each night after she gets done walking. She stated she believed the facility would have noticed at some point Resident #54 was missing. She stated when she received the call from MOTP B at 9:40 pm, she had the staff initiate a head count of all residents while she went and picked up Resident #54. She stated when she got back to the facility, Resident #54 was taken to her room, her wet clothing was removed, and she was put to bed. She stated to her knowledge no other residents were reviewed or rounded on because Resident #54 was safe and back in the facility. She stated she did not know there were two nurses sitting at the nurse's station did not even check the door. She stated she was lucky that Motp found Resident #54, it could have been much worse if Resident #54 got hurt.
During an interview on 12/6/24 at 11:15 am, ADON LVN stated there was a binder at the nurse's station that has all the door codes and policies/procedures for anyone to pick up and review.
During an observation on 12/6/24 at 11:20 am, there were no policies or procedures in the binder only signature sheets of staff that had completed orientation. No door codes were found in the binder.
During an interview on 12/6/24 at 11:45 am, the DON stated Resident #54 did exit the building through the fire emergency exit door on hallway B at 7:00 pm on 11/17/24. She stated the video showed CNA A go down to the door, exit the building, return inside the building, and turn off the alarm. She stated she was not sure why CNA A did not do a head count of all residents when she deactivated the alarm. She stated she was not sure why the alarm went off for that long of a time. She stated there were 2 agency nurses working that night. She stated her expectation of a door alarm going off should be acknowledged immediately. She stated if the resident was not by the door, the employee should go outside, do an observation around the facility, and look any resident, if no resident was found outside the employee should let the charge nurse and the DON know immediately. She stated that she knew Resident #54 was picked up and brought back to the facility. She stated a head count of all residents was done at 9:40 pm. She stated that Resident #54 was rounded on every 15 minutes. She stated she did not know if all other residents with wander guards were monitored after the return of Resident #54. She stated that all agency staff should have known to go and check the alarming door. She stated it did not matter if the door codes were known or not by any staff. She stated the residents are the priority and should have been checked on. She stated the ADON LVN does all the trainings for the facility. She stated this should never have happened and the head count should have been done.
An Immediate Jeopardy was identified on 12/6/24 at 2:45 pm. The Administrator and DON were informed, and Immediate Jeopardy Template was provided. The Administrator and DON were notified that a Plan of Removal was requested at that time.
A Plan of Removal was accepted on 12/7/24 at 6:03 PM and reflected the following:
1. Immediate Actions Taken for Those Residents Identified:
Action: Resident #54 returned to the nursing home. Resident was assessed with no injuries. Resident behaving per norm. Increased supervision implemented with Resident #54 which included resident in line of sight of an employee at all times until discharge.
Elopement assessment updated. RP & MD informed.
(Resident #54 has since been discharged on 11/29/2024 to a secured unit)
Person(s) Responsible: Charge Nurse, Assistant Director of Nursing, and/or Designee
Date: 11/18/24.
2. How the Facility Identified Other Possibly Affected Residents:
Action: Resident head count performed no additional findings.
Person(s) Responsible: Charge Nurse and/or Designee
Date: 11/17/2024
Action: All residents received an elopement assessment. Residents' current elopement assessment will reflect on their face sheet and care plan.
Person(s) Responsible: Director of Nursing, Assistant Director of Nursing, and/or Designee
Date: 11/18/2024
3. Measures Put into Place/System Changes to remove the immediacy, and what date these actions occurred:
Action: Elopement binder reviewed to ensure it matches the current residents who were deemed as elopement risks per their elopement assessments.
Person(s) Responsible: Director of Nursing and/or Designee
Date: 11/18/2024
Action: Sign on door verified for placement notifying visitors to, Please do not allow residents to follow you out.
Person(s) Responsible: Administrator
Date: 11/18/2024
Action: Sign posted by keypads stating: When alarms were sounding, and the door was disengaged perform a resident head count.
Person(s) Responsible: Director of Regulatory Compliance
Date: 11/18/2024
Action: All doors checked for functionality. No concerns noted.
Person(s) Responsible: Maintenance Director and/or Designee
Date: 11/17/2024
Action: Check for all residents with roam alerts for functionality. No concerns noted.
Person(s) Responsible: Administrator and/or Designee
Date: 11/18/2024.
Action: Elopement drill performed each shift (6a-6p and 6p-6a).
Person(s) Responsible: Administrator, Maintenance Director, and/or Designee
Date: 11/19/2024
Action: Education provided to direct care staff, to include agency staff, regarding missing resident/elopement & over the facility's abuse & neglect policy.
Direct care staff will be educated on the elopement binder, its location, and its contents (shows which residents were elopement risks/wander guard residents).
Direct care staff, including agency staff, will know when the door was alarming, to respond to the alarming door immediately. If the door was disengaged (open) and alarming the direct care staff will ensure all residents were in house by performing a head count (signs placed for reminders for staff to ensure all residents were in house when alarms were sounding, and the door was disengaged by keypads).
Direct care staff, including agency staff, will know the door codes/door code location through this education.
Direct care employees will be educated prior to working their next shift.
All new and temporary direct care staff will be educated prior to working.
Person(s) Responsible: Administrator and/or Designee
Date: 12/6/2024
Action: Residents deemed an elopement risk, that require a roam alert/wander guard will be rounded on every 2 hours to ensure facility was aware of residents' whereabouts.
Person(s) Responsible: Charge Nurse, Certified Nurse's Aides, and/or Designee
Date: 12/6/2024
4. How the Corrective Actions Will be Monitored, by whom, and for how long:
Action: All residents with exit seeking behaviors will be reviewed during clinical meeting to ensure safety. Appropriate supervision will occur until residents with exit seeking behaviors, that have a greater need than the roam alert system, were appropriately placed. No concerns noted.
Person(s) Responsible: Director of Nursing and/or Designee
Date: 11/17/2024
Action: Elopement drill performed weekly x4 weeks to ensure staff's retention of education to prevent recurrence.
Person(s) Responsible: Administrator and/or Designee
Date: 11/17/2024
QAPI-
Action: Ad hoc QAPI performed with medical director to inform them of the incident and the facility's plan to remove the immediacy. No further direction required.
Person(s) Responsible: Administrator
Date: 11/18/2024
State Surveyors monitored the facility's Plan of Removal and confirmed it was sufficient to remove the IJ through observations, interviews, and record reviews from 12/6/24 to 12/7/24 as follows:
Record review of resident assessment:
Record review of progress note of Resident #54 dated 11/18/24 at 12:10 am submitted by ADON LVN indicated, this LVN received a call regarding resident at 9:45 pm asking if we had a resident by the name of Resident #54. ADON LVN enquired about how resident had come to be at apartment. ADON LVN also brought resident back to facility and facilitated safe return and delegated that agency nurse perform skin assessment and assign one on one monitoring and fill out event for elopement. CNA asked to assist resident out of wet clothes get into dry bed clothes. No injuries or wounds noted. Resident placed on 1 on 1. ADON LVN spoke to CNA A and MD to report elopement and subsequent actions. Resident denies pain or discomfort and just wishes to go to bed. No acute distress noted.
Record review of progress notes of Resident #54 dated 11/17/24 at 10:24 pm submitted by ADON LVN indicated:
Resident Refused Skin Assessment: No
Temperature--Location, if applicable.: Warm
Color--Location, if applicable.: Expected color for ethnicity.
Moisture--Location, if applicable.: Dry
Skin Turgor: Normal
Capillary Refill: Less than 3 seconds
Was Resident at risk for developing pressure injuries? No Risk Factors: Moisture, Incontinence
Were contractures present? No
Alterations in Skin Integrity. Note location of any noted areas. Enter measurements in box provided.: None.
Notifications if Applicable: Physician Notified MD, Responsible Resident Representative Notified. Guardian
Interventions: No new or additional interventions required at this time.
[Corporation] Assessment for Risk of Elopement completed 11/18/24. Indicated yes to all:
Does the resident have a diagnosis of Dementia, OBS, Alzheimer's, I/DD, Delusions, Hallucinations, Anxiety, Depression, Schizophrenia, or other Mental Illness? Yes
Does the resident ambulate independently, with or without the use of an assistive device (i.e., walker, cane, or wheelchair)? Yes
If the resident has wandering behavior, was it tied to resident's past (i.e., their prior work, takes long walks, seeking someone they cannot find)? Yes
Was the resident ambulatory (able to walk without someone assisting them) yet cognitively impaired with poor decision-making skills (i.e., intermittent confusion, cognitive deficits, appears disoriented)? Yes
Has the resident verbally expressed the desire to go home, packed belongings to go home, talked about going on a trip, or stayed near an exit door? Yes
Does the resident have a history of leaving the facility without Informing staff? Yes
Does the resident wander without a sense of purpose (i.e., confused, moves aimlessly, may enter other resident rooms, and explore their belongings)? Yes
Record review of observations initiated by the facility on 11/17/24 at 10:07 pm of Resident #54 for increased rounding indicated: times starting at 10:07 pm and every 15min interval after that with sign off sheet until 11:45 pm. Sheet dated 11/18/24 had monitoring every 15min, all day long, no time was missed, signatures provided. Sheet dated 11/19/24 had monitoring every 15min up until 12:00 pm.
Record review of facility Resident head count dated 11/17/24 at 9:40 pm indicated all residents were in the building except Resident #54. At which time ADON LVN was going to pick up Resident #54.
Record review of the facility Resident observation summary report for all residents dated 11/17/24 to 11/19/24 completed for [corporation] assessment for risk of elopement for all residents in the facility completed daily by all nurses in the facility.
Record review of door checks (door locking mechanism) log sheet dated 11/11/24 to 11/15/24 all indicated a pass. Door check log sheet dated 11/18/24 all indicated a pass.
Record review of Code Pink drill documentation form dated 12/6/24 at 5:02 pm indicated all staff acted correctly. Signature pages presented. Record review of Code Pink drill documentation form dated 11/27/24 indicated all staff acted correctly. Signature pages presented.
Record review of drill dated 11/19/24 time stamped 5:30 am indicated: The Administrator hid as an unaccompanied resident which would activate a missing resident situation. Informed staff that we were looking for an unaccounted resident. Verbally alerted staff to the Code Pink status. Staff immediately met at the Nurses Station and received direction from the charge nurse to begin looking for a missing resident. Staff searched all hallways/rooms/dining area/lobby, and closets. Within 5 minutes the Mock resident was found in the kitchen. Signed and dated by the Administrator.
Record review of drill dated 11/18/24 time stamped 5:00 pm indicated: The Maintenance Director chose an employee to hide as an unaccompanied resident which would activate a missing resident situation. Informed staff that we were looking for an unaccompanied resident. Verbally alerted staff to Code Pink status. Staff immediately met at the Nurses Station and received direction from the charge nurse to begin looking for missing resident. Staff searched all hallways/rooms/dining area/lobby, and closets. Within 3 minutes the Mock resident was found in the Beauty Shop. Signed and dated by the Maintenance Director.
Record review of Ad hoc QAPI meeting dated 12/6/24 indicated: An ad hoc QAPI meeting was performed with the MD to review the incident regarding Resident #54. The MD was agreeable with the plan of action. The MD completed a telehealth visit with Resident #54 with no concerns.
Record review on 12/8/24 of Agency orientation to the facility book and for the rest of the staff, located at nurses' station, binder contained: policy's abuse, neglect, and exploitation, wandering and elopement, comprehensive care plans, advanced directives, change in residents' condition or status, fall prevention program, and resident rights. Binder also contained: Note that stated, door codes-if they do not work, please call the admin or the DON, and then list all door codes for the entire facility for going in or out of the facility. Binder also contained completed orientations of nursing and agency staff.
Record review on 12/9/24 of In-service titled visual rotation risk of elopement, led by the Administrator indicated: go into the MAR and check residents that have wander guards. All residents with wander guards were rounded on, the even hours were rounded on by CNA's and odd hours were rounded on by Nurses. The sign off sheet would be reviewed by both the nurses and CNA's when the rounding was completed.
Record review on 12/9/24 of in-service titled Door alarm education and elopement policy, instructed by a group of people, but the Administrator did educate. The Administrator stated the education included door alarms, how to react and what to do. He stated the education included elopement, education, and abuse/neglect. He stated that if the alarm was sounding the door should be observed immediately. He stated then if the door opens even with the alarm going off, the employee should go outside, and check the area. He stated the employee should walk the entire facility and check the surrounding area. He stated if no resident was seen/found the employee was to come back inside, turn off the alarm, make sure door was locked, and then inform staff to initiate a head count for the entire facility. He stated that if the door was alarming and the door did not open to look in the surrounding area inside the building to find the possible resident that set the alarm off and redirect the resident from the door.
Record review on 12/9/24 of in-service titled abuse, neglect, and exploitation, instructed by ADON LVN completed on 11/18/24. ADON LVN stated that due to the elopement the facility did do an in-service on abuse, neglect, and exploitation. She stated during the education she did go over the whole policy, and she discussed with staff what constitutes as abuse, neglect, and exploitation. She stated she also covered what to do if abuse or neglect were to occur and/or was witnessed in the facility. She stated the process was to report any incident directly to the Administrator because he was the abuse neglect coordinator.
During an interview on 12/7/24 at 10:15 am, LVN C (day nurse) stated there were 3 in-services that she could remember but it was basically a big training yesterday while she was on shift. She stated first was elopement and what to do if a door alarm was going off. She stated if a door alarm was going off and opened upon arrival with no resident in site, she would go outside and search the surrounding area. She stated if no resident was found outside, she would return back inside, and inform staff of a possible elopement. She stated she would inform the charge nurse, the DON, or the Administrator of a possible elopement. She stated she would then start a head count of all residents in the facility. She stated there was a binder now at the nurse's station with all the policies and procedures. She stated the binder included abuse neglect, elopement, and other policies and procedures. She stated that one sheet in the book also contained the alarms and codes to all doors in the facility. She stated they also would do rounding on all residents with wander guards every two hours. She stated for abuse/neglect, if she were to witness or observe anything of that nature to separate or remove the resident from the situation, also to immediately inform the Administrator of the incident, and give report to the Administrator.
During an interview on 12/7/24 at 10:25 am, CNA B (Day shift) stated she did have to do in-services before she could come on to work today. She stated the categories of the in-services included elopement, where to find guidance, and abuse/neglect. She stated the main topic at hand was what to do if a door alarm was going off in the facility. She stated they emphasized the importance of going to the door immediately and checking for any residents at the door. She stated if a resident with a wander guard was still at the door and the door was still locked to re-direct the resident away from the door. She stated but if the door alarm was going off and the door could open, it was vital to go outside, and look for the resident. She stated if no resident was found outside, she was to inform staff to start a resident head count. She stated the second topic was where to find all the policies and procedures in the building. She stated there was a new binder at the nurse's station that contained all the policies and procedures for given situations. She stated also within the binder were all the codes for all the doors in the building.
During an interview on 12/7/24 at 10:30 am, LVN D (Night Nurse) stated before he was allowed to work last night he had to go through a few trainings. He stated he used to be an agency nurse, but now worked full time for the facility. He stated he forgot his phone at work, so he was here at this time. He stated most of the trainings were related to door alarms in the facility. He stated if an alarm was going off in the facility, he was to immediately check the door. He stated if the resident that set off the alarm was still in the area and the door was still locked then he was to re-direct the resident from the door. He stated however, if the door alarm was going off and the door opens, even if there was a resident with a wander guard standing next to the door, he was to go outside the facility and look around the building. He stated if no resident was found outside, he was to turn off the door alarm, make sure the door locks, and get with all the staff to do a resident head count. He stated he was also in-serviced on a new binder that would be at the nurse's station. He stated the new binder contained all the door codes and alarms. He stated the binder also contained all the policies and procedures given for different situation, like a quick reference guide. He stated other than that the last in-service was related to abuse/neglect. He stated it went over what to look for, how to react, and who to report to if he were to witness anything like that.
During an interview on 12/7/24 at 10:35 am, RN A (Day Nurse) she stated there were 3 total in-services. She stated there was training about elopement and risk of elopement for residents in the facility. She stated, for example if there was a door going off in the facility to immediately go and check the door. She stated if the resident who set the alarm off was still standing there, to redirect the resident. She stated however if there was no resident at the door and the alarm was sounding, she would exit the facility. She stated she would search the surrounding area for any possible residents. She stated she would return inside and start a head count of all residents in the facility. She stated if there was no resident found, to turn the alarm off upon entering the facility, make sure the door locks, and then do a head count of the entire facility of all residents. She stated another in-service covered the new binder at the nurse's station. She stated the new binder had all the policies and procedures for quick referencing. She stated there were also a sheet that had all the codes for all the doors in the facility. She stated another part of the training included rounding on all elopement risk residents in the facility every 2 hours.
During an interview on 12/7/24 at 10: CNA C (night shift) stated before she could start working for the day she was in-serviced on a few different topics. She stated the first topic was elopement. She stated the primary key in this in-service was when a door was alarming, was the door still locked or could the door be opened. She stated if the door was still locked, she was to re-direct the resident that set off the alarm away from the door. She stated but if the door could be opened, she would inform the nurse or charge nurse and then go outside the facility to do a walk around. She stated if she was to return to the facility without seeing any residents, she would inform the charge nurse or nurse and a resident head count would be initiated. She stated the other new thing, which she felt was a great idea, was a new binder at the nurse's station. She stated in the binder was the policies and procedures for different events that could occur in the facility and what to do if they were to occur. She stated that also in the binder were all the codes to all the doors in the facility. She stated lastly there was an in-service on abuse/neglect. She stated it covered what to look for in given situations, who to report to, and what to do.
The Administrator were informed the Immediate Jeopardy was removed on 12/07/2024 at 1:33pm. The facility remained out of compliance at a severity level of at potential for more than minimal harm that was not immediate and a scope of a pattern due to the facility's need to evaluate the effectiveness of their corrective actions that were put into place.
Record review of Resident #52's electronic face sheet revealed a [AGE] year-old male admitted [DATE]. Diagnoses included liver cell carcinoma (liver cancer), personal history of other mental and behavioral disorders, bipolar (episodes of mood swings ranging from depressive lows to manic highs), nicotine dependence, anxiety disorder, and chronic pain.
During an observation on 11/18/2024 at 11:05 AM Eight residents were exiting a door in the dining room to the designated smoking area with the MD supervising and handing out cigarettes to each resident and lighting the cigarettes for each resident. Resident #52 was observed lighting his own cigarette with a cigarette and lighter in his possession. The MD did not prov[TRUNCATED]
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure before a resident was transferred or discharged that the fa...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure before a resident was transferred or discharged that the facility notified the resident's guardian of the transfer or discharge and the reasons for the move in writing and in a language and manner they understood and the facility must send a copy of the notice to a representative of the Office of the State Long-Term Care Ombudsman for 1 of 3 residents (Resident #54) reviewed for transfer or discharge.
The facility failed to provide Resident #54 ' s guardian written notice of the resident ' s transfer before Resident #54 was transferred to Facility B on 11/29/2024.
The facility failure could affect residents who were discharged from the facility and could place them at risk of having their discharge rights violated.
The findings included:
Record review of Resident #54's, face sheet dated 12/9/24 revealed a [AGE] year-old female admitted to the facility on [DATE]. Resident #59 had diagnoses which included hypertensive heart disease, hypertension, muscle weakness, schizoaffective disorder, bipolar type, and reduced mobility. The face sheet indicated Resident #54 was discharged on 11/29/24 to another nursing facility.
Record review of Resident #54's quarterly MDS dated [DATE] revealed she had a BIMS of 00, which indicated severe cognitive impairment. Resident #54 required supervision and wore a wander guard.
Record review of Resident #54's Discharge summary dated [DATE] indicated: Resident #54 was discharged [DATE] to Facility B because Resident #54 was an elopement risk and Facility B had a locked unit. Discharge summary did not indicated that anyone at Facility A contacted Resident #54's PoA A upon being transferred out of Facility A. Completed by ADON LVN.
Record review of a progress note dated 11/29/24 at 4:50 pm indicated: Resident discharged with belongings and medications to Facility B's secure unit due to elopement risk. Residents wander guard removed. Discharge summary printed with other paperwork. Facility B's driver arrived at 4:15 pm left with the resident at 4:35 pm. Completed by ADON LVN.
Record review of electronic notification dated 11/30/24 at 8:07 am from SW to ombudsman stated: The following are discharges that took place in Noveber. Residet #54.
During an interview on 12/6/24 at 9:55 am, POA A stated that his concern was that as of yesterday 12/5/24, it was the first time he was informed that Resident #54 was moved to another facility on 11/29/24. He stated the facility must inform them of the move and get their approval of the move before they move Resident #54 to another facility. He stated this did not occur. He stated he never recieved anything that Resident #54 was discharged from the facility, no written documents or phone calls from Facility A. He stated without knowing where Resident #54 was moved, it could have caused her emotional distress because she could have gotten hurt and no one would have been there for her.
During a phone interview on 12/7/24 at 2:05 pm, the SW stated she did remember Resident #54. She stated Resident #54 recently had an incident where she eloped out of the facility. She stated that it was discussed with the facility staff at her facility that it would be better for Resident #54 to be moved to a facility that had a locked unit. She stated she did start the paperwork and did reach out to the guardian of Resident #54 to let her know. She stated that the resident was not accepted at Facility A, so she was working on finding another facility for Resident #54. She stated that on 11/29/24, Resident #54 was accepted at Facility B and was moved to that facility. She stated she should have called the guardian. She stated but she dropped the ball on this. She stated that the guardian called her on 12/7/24 and it was explained to the guardian that she should have contacted the guardian about the transfer but did not and that was on her. She stated the guardian understood. She stated Resident #54 being transferred to another facility without the PoA knowing could have caused Resident #54 sadness due to not having visitors to see her.
During a phone interview on 12/7/24 at 1:00 pm, ADON LVN stated that the normal process for discharge was to fill out the discharge summary documentation. She stated to also get the medications for the resident so they could be transferred with the resident and make sure the resident was good to go with everything they needed to go to the new facility. She stated she did do the discharge summary for Resident #54 and got everything together for the transfer/discharge. She stated she did not contact the guardian or the POA for Resident #54 because she believed that should have been done by the SW.
Record review of facilities policy dated July 2024, titled Transfer and Discharge (including AMA) indicated: Supporting documentation shall include evidence of the resident's or resident's representative's verbal or written notice of intent to leave the facility, a discharge plan, and documented discussions with the resident and/or resident representative.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on interviews and record review the facility failed to promptly resolve grievances for 12 of 12 confidential residents reviewed for grievances.
The facility did not ensure grievance concerns vo...
Read full inspector narrative →
Based on interviews and record review the facility failed to promptly resolve grievances for 12 of 12 confidential residents reviewed for grievances.
The facility did not ensure grievance concerns voiced in a Resident Council meeting were addressed or that a resolution had been communicated back to 12 of 12 confidential residents.
This deficient practice could place the residents at risk of unresolved grievances and a decreased quality of life.
The findings included:
During a confidential interview on 11/19/2024 at 10:00 a.m., 12 of 12 confidential residents stated they did know how to file a grievance. They stated the AD wrote down grievances voiced in the Resident Council meetings, but the Resident Council members did not get told the facility's responses to their grievances. They stated they felt that management of the facility did address some of their concerns but not all of them. 1 of 12 confidential residents stated they no longer came to Resident Council meetings because they felt it did not do any good and nothing changed in the facility.
Record review of Resident Council meeting minutes dated 11/6/2024 revealed Nursing .4-day ago, no aide and nurse came in the room to check on her for about 4-5 hours. The resident had to call the facility phone to see if someone would answer and someone did and stated, they are shorthanded, I will send someone in a bit. Bottom of the resident council minutes stated that Old Business - Review of Previous Meeting, Outstanding Issues, and Resident Council Departmental Response Forms Reviewed and approved by council meeting.
Record review of Resident Council meeting minutes dated 10/09/2024 revealed Nursing .2. Not enough aides at night 6pm-6am, 2 aides not going to work .10. Call lights take too long, time 45 minutes to an hour .Dietary .1. Tray tickets do not match with what is on tray .Administration Money issues are not getting like they are supposed to. Their answer is that corporations manage their money. They want to know an answer to where their money is and why it is taking too long for them to get it. Bottom of council minutes stated that Old Business - Review of Previous Meeting, Outstanding Issues, and Resident Council Departmental Response Forms Reviewed and approved by council meeting.
Record review of Resident Council meeting minutes dated 9/12/2024 revealed 1. Nursing running out of blue pads for the beds .4. Aides going in and turning the call light off and not asking who needed help and walk out .5. Not Enough training for staff. They need more training. Bottom of council minutes stated that Old Business - Review of Previous Meeting, Outstanding Issues, and Resident Council Departmental Response Forms Reviewed and approved by council meeting.
Record review of Resident Council meeting minutes dated 8/7/2024 revealed 8/7/2024: 4. Resident call lights are not being answered in a timely manner and the residents are having to leave their room to go look for help. 5. F hall residents are concerned that they do not have an aide at times, and no one tends to them they have to find out if anyone is working on their hall. 6. Staff go into residents rooms, turn the light off and does not even ask what help is needed and walk off .7. Staff leaving residents on bed pan, commode, and potty chair too long. Could they not come back 10-15 minutes later and check on them not an hour .8. Communication with the aides and nurses. Nurses do not know where the aide on the hall is or can't find them and there is no one to check on them. Bottom of council minutes stated that Old Business - Review of Previous Meeting, Outstanding Issues, and Resident Council Departmental Response Forms Reviewed and approved by council meeting.
Record review of Grievance logs dated June 2024 - November 2024 revealed no evidence of grievances voiced in Resident Council meetings.
During an interview on 11/20/2024 at 10:50 a.m., the SW stated grievances were to be written by the person that directly received the grievance. She stated the grievance would then come to her. The SW stated she would hand the grievance to the department manager the grievance pertained to. She stated after the department manager finished their part in the grievance investigation, the form would be handed back to her. She stated she filed the form in the grievance binder once the process had been completed. The SW stated the AD brought grievances made during the Resident Council meeting to her attention during the morning staff meeting. The SW stated she had been working in the facility for the last 3 months. She stated there was a grievance from August 30th, 2024, written by the AD about call lights taking too long to be answered. She stated there was no documentation that the resident who made the grievance was notified of the findings after the grievance had gone through investigation process. She stated the facility should notify residents of what was discovered about the grievance after the residents' representatives were notified. She stated there was no place on the form for resident notification but there was a place for resident representative notification. She stated that was not filled in on August 30th, 2024, grievance. She stated everything that required attention should be documented on the grievance form. She stated she felt communication and the AD not being used to having the SW in the building may have led to the failure of grievance forms not being filled out. She stated she believed that the AD had taken care of the grievances. The SW stated the effect that not communicating responses back to residents could lead to them being frustrated and could cause feelings of not being heard.
During an interview on 11/20/2024 at 11:26 a.m., the DON stated if the Resident Council had a grievance that was nursing related, she was to follow up on those grievances. She stated she thought the AD had come to her about 2 months ago with concerns from the Resident Council meeting. She stated she had gone back to the Resident Council President with some of those resolutions but stated she had not gone back to the all the resident council members. She stated she felt all the Resident Council members should be notified during a follow-up resident council meeting of the grievance findings and she did not know why that had not been done. She stated she continued to learn the processes of the facility. She stated the result of not following up with the Resident Council could cause them to lose faith in Resident Council meetings. She stated members could feel their needs were not being addressed or that they were not important. The DON stated she did not know who was responsible for the grievance process in relation to the Resident Council meetings. She stated that she would file a grievance if the resident spoke to her about a concern. She stated that after a grievance had been made, the SW would follow up with residents about findings.
During an interview on 11/20/2024 at 11:51 a.m., the AD stated she took down minutes from the Resident Council meetings and then transferred information onto a form titled Resident Council Response Form. She stated on 11/6/2024 she had not filled out the form for nursing. The AD stated on 11/6/2024 the members of the confidential meeting had asked the DON to join the meeting, and the DON had joined that meeting. The AD stated there was nothing documented about actions that were discussed at the meeting on 11/6/2024. She stated on 9/12/2024 she did fill out a form for nursing. She stated she handed that form to the DON and did not receive the form back from the DON. She stated the last form she had received back from the DON was back on 6/5/2024 and that was a different DON that had filled the form out. The AD stated each department head monitored that she received the response forms back. She stated the DON had been having to work on the floor and that may have caused her to delay giving the response form back to the AD. The AD stated she had been instructed to document anything brought up in the Resident Council meetings as that was important to the residents. She stated she could only report back to the Resident Council what was verbally told to her, and she did remember that management told her staff were being educated on the Resident Council's concerns. She stated she did feel that Resident Council needed a response about their concerns. She stated some departments were good at reporting the findings back to her so that she could relay information to the Resident Council.
During an interview on 11/20/2024 at 12:51 p.m., the ADMN stated the facility was in the process of changing over the process for handling grievances voiced in the Resident Council meetings. He stated his expectation would be for the grievance to be brought to the department manager's attention. He stated the facility had 72 hours to resolve the issue and then the resolution should be communicated to the individual or council if an actual grievance was filed. He stated some of the concerns brought up in the Resident Council meetings should be grievances and documented as grievances. The ADMN stated if there were multiple people bringing up the same issue then a resolution should be communicated back to the group. He stated the AD was responsible for communicating resolution of grievances to the Resident Council or depending on the situation the department manager was responsible. He stated that the AD was who monitored that grievance resolutions were communicated back to the Resident Council. He stated the AD could ask the department manager to attend the Resident Council meeting and verbalize resolution based on the members' request. He stated not communicating resolutions could cause for the Resident Council members to be frustrated.
Record review of the policy titled Grievances, Recording, and Investigating revised on 01/12/2023, revealed The Administrator or designee will record and maintain all grievances in the Grievance Log. The Resident Grievance Form will be filed with the Administrator or designee and the resolution will be identified within three (3) working days of the concern. The resident, or person acting on behalf of the resident, will be informed of the findings of the investigation, as well as any corrective actions recommended, within 3 working days of the filing of the grievance.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to develop and implement a comprehensive person-centered care plan b...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to develop and implement a comprehensive person-centered care plan based on assessed needs with measurable objectives that have the ability to be evaluated or quantified to attain or maintain the resident's highest practicable physical, mental, and psychosocial well-being for 4 (Resident #6, Resident #30, Resident #68, and Resident #43) of 18 residents reviewed for comprehensive person-centered care plans.
The facility failed to develop care plans based on the assessed needs with measurable objectives and timeframes in area of nebulized breathing treatments for Resident #6.
The facility failed to develop care plans based on the assessed needs with measurable objectives and timeframes in area of oxygen therapy for Resident #30.
The facility failed to develop a comprehensive care plan based on the assessed needs with measurable objectives and timeframes in area of care needs with a resident who required trach maintenance and care for Resident #68.
The facility failed to develop care plans based on the assessed needs with measurable objectives and timeframes in area of resident's preference to sleep in her recliner for Resident #43.
This failure could place the residents at risk for decreased quality of life and not having their needs met.
Findings included:
Resident #6
Review of Resident #6's electronic face sheet revealed a [AGE] year-old female admitted to the facility on [DATE] with diagnoses to include: lung disease, heart failure, and urinary tract infection.
Review of Resident #6's quarterly MDS, dated [DATE], revealed a BIMS score of 00 which indicated severe cognitive impairment. Further review of the quarterly MDS, Section O revealed oxygen therapy.
Review of Resident #6's comprehensive care plan, last revised 11/19/2024, revealed: Problem: Continuous use of Oxygen. Goal: Oxygen levels will maintain above 90%. Approach: Apply oxygen as per Medical Director orders. Further review of comprehensive care plan revealed no evidence of the use of nebulized breathing treatments.
Review of Resident #6's electronic physicians' order revealed: ipratropium-albuterol solution for nebulization four times a day. Further review of electronic physicians' orders revealed no evidence of an order for oxygen, start date 09/29/2024.
During an observation on 11/18/24 at 11:06 AM, Resident #6 was resting in bed in low position. Resident #6's nebulizer was lying in the nightstand drawer not in a plastic bag.
Resident #30
Review of Resident #30's electronic face sheet revealed a [AGE] year-old male admitted to the facility on [DATE] with diagnoses to include: respiratory disorders, respiratory infection, and anxiety.
Review of Resident #30's quarterly MDS, dated [DATE], revealed a BIMS score of 09 which indicated moderate cognitive impairment. Further review of the quarterly MDS, Section O revealed no evidence of oxygen therapy.
Review of Resident #30's comprehensive care plan, last revised 09/24/2024, revealed: Problem: Resident is at risk for respiratory complications. Goal: Resident will be free form respiratory complications. Approach: Administer meds as ordered (Albuterol). Further review of comprehensive care plan revealed no evidence of the use of oxygen therapy.
Review of Resident #30's electronic physicians' order revealed: albuterol sulfate for nebulization every 6 hours PRN, start date 04/12/2024 and Nasal Cannula continuous oxygen at 2-3 LPM, start date 11/07/2024.
During an observation and interview on 11/19/24 at 04:30 PM, Resident 30 was resting in bed. Resident #30's oxygen nasal cannula was lying on the floor beside his bed. Resident #30's nebulizer was lying on the nightstand not in a bag. He stated his nebulizer had never been put in a bag. He stated he finished his breathing treatment and then laid it down.
During an observation on 11/20/24 at 10:35 AM, Resident #30 was resting in bed. Resident #30's oxygen nasal cannula was lying on the floor beside his bed. Resident #30's nebulizer was lying on the nightstand not in a bag.
Resident #68
Review of Resident #68's electronic face sheet revealed a [AGE] year-old female admitted to the facility on [DATE] with diagnoses to include: tracheostomy, brain injury, and brain bleed.
Review of Resident #68's admission MDS, dated [DATE], revealed the resident was admitted on [DATE].
Review of Resident #68's comprehensive care plan revealed no evidence of a comprehensive care plan until after entrance on 11/18/2024.
During an observation on 11/18/24 at 02:28 PM, Resident #68 was resting in bed with oxygen connected to her trach.
Resident #43
Review of Resident #43's quarterly MDS, dated [DATE], revealed a [AGE] year-old female admitted to the facility on [DATE] with diagnoses to include: diabetes, and traumatic brain injury. Further review of the quarterly MDS revealed a BIMS score of 15 which indicated no cognitive impairment.
Review of Resident #43's comprehensive care plan, last revised 09/08/2024, revealed no evidence of the resident sleeping in her recliner.
During an observation and interview on 11/18/24 at 02:17 PM, Resident #43 was up in her wheelchair. She stated she can't lay on her right side because she falls out of bed and that she slept in her recliner every night.
During an interview on 11/20/24 at 12:12 PM, CNA A stated he only received verbal communication regarding residents' care needs. He stated he did not know where to find the care plan. He stated if he had questions regarding resident care, he just asked the nurses.
During an interview on 11/20/24 at 01:41 PM, LVN K stated she knew how to find the care plan. She stated trach care, oxygen therapy, and a resident sleeping in a recliner were all things that should have been care planned. She stated the DON and the ADON were responsible for updating the care plans. She stated not having an updated care plan confused the nurses about what care they needed to provide.
During an interview on 11/20/24 at 02:06 PM, the MDS coordinator stated she was responsible for comprehensive care plans. She stated a trach and trach care needed to be care planned as did a resident sleeping in a recliner. The MDS Coordinator stated oxygen should have been care planned. She stated the care plans were usually updated by the DON because she was more involved with the clinical care. She stated that care plans were signed off by an RN. She stated this was usually the DON and the DON was to monitor and ensure care plans were updated within the correct time frames. She stated the negative effects to the residents were staff not knowing what care they needed to provide.
During an interview on 11/20/24 at 02:00 PM, the DON stated her and the ADON were responsible for baseline care plans and the MDS Coordinator was responsible for comprehensive care plans. She stated she was responsible for signing off on the accuracy and ensuring that care plans were completed accurately and in a timely manner. She stated trach care, oxygen therapy, and sleeping in a recliner were all things that should have been care planned. She stated this failure could result in residents not receiving the care they needed. She stated staff would be unable to provide appropriate care if the care plan was not updated and accurate.
Review of facility's policy Care Plans, Comprehensive Person-Centered revised December 2020 revealed: The comprehensive, person-centered care plan will: A. include measurable objectives and time frames; B. describe the services that are to be furnished to attain or maintain the resident's highest practicable physical, mental, and psychosocial well-being; C. Describe services that would otherwise be provided for the above, but are not provided due to the resident exercising his or her rights, including the right to refuse treatment; . E. Include the resident's stated goals upon admission and desired outcomes G. Incorporate identified problem areas; H. Incorporate risk factors associated with identified problems . Reflect treatment goals, timetables and objective in measurable outcomes; L. Identify the professional services that are responsible for each element of care; M. Aid in preventing or reducing decline in the residents functional status and or functional ; N. Enhance the optimal functioning of the resident by focusing on a rehabilitative program, and O. Reflect current recognized standards of practice for problem areas and conditions . Care plan interventions are chosen only after careful data gathering, proper sequence of events, careful consideration of the relationship between the resident's problem areas and their causes, and relevant clinical decision making.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record review the facility failed to ensure that residents received treatment and care in accordance with professional standards of practice, and residents' choi...
Read full inspector narrative →
Based on observations, interviews, and record review the facility failed to ensure that residents received treatment and care in accordance with professional standards of practice, and residents' choices during a confidential meeting for 12 of 12 residents reviewed for quality of care.
The facility failed to ensure that licensed staff were not withheld resident wipes, which led to the staff having to use paper towels and toilet paper for resident care.
This failure could put residents at risk of being unclean and skin sheer during direct resident care.
Findings included:
During an observation on 11/18/2024 at 10:00 AM, cases of resident wipes were being stored in the DON's office. The supply closets on Hall C and E were observed to have no wipes available.
During an interview on 11/18/2024 at 10:00 AM, CNA-C stated the wipes were kept in the DON's office with only a few kept on one or two hall carts. She stated the DON locked them in her office storage closet.
During an observation on 11/18/2024 at 10:09 PM there were no wipes on the linen carts of Halls D, E, F with only half of one package of wipes on Hall C.
During a confidential meeting on 11/19/2024 at 9:59 AM, 12 of 12 residents had issues with staff not having enough wipes/briefs. 1 stated that she had to go to the ADON or the DON and ask for wipes herself due to staff not being able to get them. Another resident stated peri care had been performed on night shift with paper towels due to wipes shortage.
During an interview on 11/18/2024 at 9:50 AM, LVN-G stated the wipes were kept in the DON's office. She stated she felt they should have been easily accessible on the floor. LVN-G stated if she ran out of wipes, she, other staff, and residents had to ask for them with the residents having to show them an empty package if they wanted more. She stated it was inconvenient when having to provide resident care. She stated, staff had to get permission from the DON before more was to be provided. LVN-G stated she felt it slowed down resident care in the wipes not being provided.
During an interview on 11/18/2024 at 10:00 AM, CNA-H stated, the wipes were kept in the DON's office. She stated the DON had started doing this to save on wipes and was told staff were using too many.
During an interview on 11/18/2024 at 10:20 PM, CNA-E stated she had worked at this facility since May 2024 with continued shortage of wipes. CNA-E stated she had cleaned residents with wet towels when running out of wipes due to the wipes being locked in the DON's off at night. She stated the towels were not as soft as the wipes and it was hard on resident's skin. CNA-E stated that the staff were only allowed so many packages per shift and if they ran out, they were to call the DON, but having been at night she would not answer. She stated they only received a certain number of packages of wipes per shift.
During an interview on 11/18/2024 at 10:35 PM with LVN-F and LVN-J they both stated there was a shortage of wipes. LVN-F stated if she ran out of wipes on the night shift, she was to call the DON for her to come up and unlock her office, but she stated most of the time, they did not answer the phone. LVN-F and LVN-J stated she felt the facility should have provided more wipes.
During an interview on 11/20/2024 at 9:30 AM the DON stated there was a shortage of wipes. She stated the residents who needed and wanted them had to go get them from her. The DON stated she did the ordering of supplies and forgot to order them in time. The DON stated she did not like to leave wipes out because they disappeared.
She had currently ordered 26 cases a week, with prior orders been 10 a week and had not been sufficient. The DON stated she has failed at times and had not always been organized. She stated she would have liked for the ADON to take over the supplies but felt she was not ready. She stated she would provide documentation of the orders but those were not provided prior to exit. The DON stated that her expectations were to have plenty of wipes for residents so their needs would be accommodated. She stated she monitored, and the failure was staff having not communicated with her.
During an interview on 11/20/2024 at10:00 AM, the ADON stated the wipes disappeared when not locked up in the DON's office. She stated that staff had also brought their own wipes for resident care. The ADON stated she helped monitor them and she stated she planned to take the position of ordering because the DON could not fulfill the requirement. The ADON stated the negative impact to residents in not using wipes and paper towels instead for resident care could be skin breakdown and infection. She stated her expectations were for all resident care be always done with wipes.
Record review on 11/20/2024 of facility Center admission Agreement, dated 2/22/2022 revealed on pg. 19 revealed:
Primary covered charges-Routine services such as .nursing care and supplies
Record review of facility policy titled Perineal Care dated 1/20/2023 revealed:
Policy Statement
Perineal Care is providing cleanliness and comfort to the resident, to prevent infections, skin irritation, and to observe the resident's skin condition.
Equipment and Supplies
The following equipment and supplies needed include, but are not limited to the following:
1. Disposable cleansing wipes; .
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review, the facility failed to have sufficient nursing staff to provide nursing and...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review, the facility failed to have sufficient nursing staff to provide nursing and related services to assure resident safety and attain or maintain the highest practicable physical, mental, and psychosocial well-being of each resident and determined by considering the number, acuity, and diagnoses of the facility's resident population with accordance with 3 of 18 residents (Resident #30, Resident #37, and Resident #54) reviewed for sufficient staffing
The facility failed to ensure the facility had sufficient staffing based off facility assessment.
This failure could place the residents at risk of resident's needs, safety and psychosocial well-being not being met.
The findings include:
Record review of Resident #30's electronic face sheet dated 11/20/2024 revealed Resident #30 was a [AGE] year-old female admitted into facility on 10/18/2022 with diagnoses to include: fracture of left patella (left knee fracture), schizoaffective disorder bipolar type (a mental health condition with a combination of symptoms including hallucinations, delusions, mania, and depression), and dementia.
Record review of Resident #30s quarterly MDS dated [DATE] revealed BIMS score of 04 which indicated severe cognitive impairment. Further review of the MDS indicated Resident #30 needed extensive assistance with bed mobility, transfers, and toilet use.
Record review of Resident #30's care plan dated 11/19/2024 revealed Resident #30 had self-care deficits d/t impaired cognition and impaired mobility start date 11/28/2022 with approach supervision 1 assist with bathing/hygiene. Further review of care plan revealed Resident #30 preferred to take her bath/shower on M/W/F between 6am and 6pm. There was no evidence that she refused showers / baths in the care plan.
Record review of Resident #30's POC documentation for the month of November 2024 revealed no evidence that Resident #30 had bath / shower on her preferred shower days Monday, Wednesday or Friday for 11/1/2024, 11/8/2024, 11/11/2024, 11/13/2024, and 11/18/2024. Further review of documentation revealed that CNA A performed bath / shower on 11/15/2024.
Record review of Resident #37's electronic face sheet dated 11/20/2024 revealed Resident #37 was a [AGE] year-old female admitted into facility on 08/31/2020 and most recently 09/19/2024 with diagnoses to include: polyneuropathy (condition in which a person's peripheral nerves are damaged), limitation of activities due to disability, and history of falling.
Record review of Resident #37's quarterly MDS dated [DATE] revealed BIMS score of 15 which indicated no cognitive impairment. Further review of the MDS indicated Resident #37 was dependent on staff in toileting hygiene, shower/bathe self, upper body dressing, lower body dressing, and putting on/taking off footwear.
Record review of Resident #37's care plan dated 11/20/2024 revealed Resident #37 had problem required assistance with ADL's start date 11/15/2024 with approach Bathing/Hygiene amount of assist: Requires extensive to total assistance of staff. May require 2 staff at times. Further review of the care plan revealed Resident #37 preferred to take her bath/shower on M/W/F between 6am and 6pm. There was no evidence that she refused showers / baths in care plan.
Record review of Resident #37's POC documentation for the month of November 2024 revealed no evidence that Resident #37 had bath / shower on her preferred shower days Monday, Wednesday or Friday for 11/2/2024, 11/8/2024, and 11/13/2024.
Record Review of Resident #54's electronic face sheet dated 11/20/2024 revealed Resident #54 was a [AGE] year-old female admitted into facility on 01/31/2023 with diagnoses to include: schizoaffective disorder bipolar type (a mental health condition with a combination of symptoms including hallucinations, delusions, mania, and depression), and dementia.
Record Review of Resident #54's quarterly MDS dated [DATE] revealed BIMS score of 00 which indicated severe cognitive impairment.
Record Review of Resident #54's care plan created on 04/17/2024 revealed approach If res is observed wandering or exit seeking, assist/offer to alternate task to divert attention .Res utilizes a wander guard to promote safety .Quarterly elopement risk assessment.
Record review of timesheets dated 09/25/2024 revealed 135.99 hours worked by direct care staff. Per facility assessment and census, 196.65 direct care staff hours were needed.
Record review of timesheets dated 11/02/2024 revealed 193.65 hours worked by direct care staff. Per facility assessment and census, 196.65 direct care staff hours were needed.
Record review of timesheets dated 11/16/2024 revealed 172.14 hours worked by direct care staff. Per facility assessment and census, 188.1 direct care staff hours were needed.
Record review of timesheets dated 11/17/2024 revealed 134.23 hours worked by direct care staff. Per facility assessment and census, 190.95 direct care staff hours were needed.
Record review of Resident Council meeting minutes dated 11/6/2024 revealed Nursing .4-day ago, no aide and nurse came in the room to check on her for about 4-5 hours. The resident had to call the facility phone to see if someone would answer and someone did and stated, they are shorthanded, I will send someone in a bit. Bottom of the resident council minutes stated that Old Business - Review of Previous Meeting, Outstanding Issues, and Resident Council Departmental Response Forms Reviewed and approved by council meeting.
Record review of Resident Council meeting minutes dated 10/09/2024 revealed Nursing .2. Not enough aides at night 6pm-6am, 2 aides not going to work .10. Call lights take too long, time 45 minutes to an hour .Dietary .1. Tray tickets do not match with what is on tray .Administration Money issues are not getting like they are supposed to. Their answer is that corporations manage their money. They want to know an answer to where their money is and why it is taking too long for them to get it. Bottom of council minutes stated that Old Business - Review of Previous Meeting, Outstanding Issues, and Resident Council Departmental Response Forms Reviewed and approved by council meeting.
Record review of Resident Council meeting minutes dated 9/12/2024 revealed 1. Nursing running out of blue pads for the beds .4. Aides going in and turning the call light off and not asking who needed help and walk out .5. Not Enough training for staff. They need more training. Bottom of council minutes stated that Old Business - Review of Previous Meeting, Outstanding Issues, and Resident Council Departmental Response Forms Reviewed and approved by council meeting.
Record review of Resident Council meeting minutes dated 8/7/2024 revealed 8/7/2024: 4. Resident call lights are not being answered in a timely manner and the residents are having to leave their room to go look for help. 5. F hall residents are concerned that they do not have an aide at times, and no one tends to them they have to find out if anyone is working on their hall. 6. Staff go into residents rooms, turn the light off and does not even ask what help is needed and walk off .7. Staff leaving residents on bed pan, commode, and potty chair too long. Could they not come back 10-15 minutes later and check on them not an hour .8. Communication with the aides and nurses. Nurses do not know where the aide on the hall is or can't find them and there is no one to check on them. Bottom of council minutes stated that Old Business - Review of Previous Meeting, Outstanding Issues, and Resident Council Departmental Response Forms Reviewed and approved by council meeting.
During an observation and interview on 11/18/2024 at 11:04 a.m., revealed Resident #37 was lying in her bed and stated that she had issues with not receiving showers three times a week and felt it was due to lack of staffing. She stated she did refuse shower on 11/13/2024 but had not been offered another shower since then. She stated she had skin issues and wanted showers, but she had a headache on 11/13/2024 and did not want shower on that day. She stated she had concerns about Resident #30, her roommate, not getting a bath or shower in the last 3 weeks.
During an observation and interview on 11/18/2024 at 11:11 a.m., revealed Resident #30 was not able to verbalize answers to questions about care in facility. She was lying in bed and fidgeting. She had a leg brace on her left leg. She kept attempting to move around in the bed.
During an observation on 11/18/2024 at 10:08 p.m., revealed a call light in room [ROOM NUMBER] was on when arriving at the facility. At 10:21 p.m., the light call was answered by staff.
During a confidential group meeting on 11/19/2024 at 9:59 a.m., 12 of 12 residents stated they had to wait approximately 30 to 45 minutes before call lights were answered. 1 of 12 residents stated she had urine incontinence due to having to wait and was embarrassed by that. 1 of 12 residents stated that she felt recurrent UTIs (Urinary Tract Infections) were because of not being changed after incontinent episode timely.
During an observation on 11/19/2024 at 10:45 a.m., revealed a recorded video viewed of Resident #54 exiting the building through door at the end of B-hall on 11/17/2024 at 7:11 p.m. One CNA was seen going to door at the end of B-hall and stepped outside. One minute later, the same CNA returned to the building without Resident #54. Resident #54 was seen returning to the building with the ADON on 11/17/2024 at 10:04 p.m.
During a telephone interview on 11/19/2024 at 9:22 a.m., a city police officer reported he had been dispatched to an apartment building on 11/17/2024 because the manager of apartment complex reported a woman wandering around the apartment complex. He stated the city police dispatch contacted the nursing facility to ask if they were missing a resident. He stated by the time he arrived at the apartment complex, Resident #30 had been loaded up and was being taken back to the facility.
During an attempted telephone interview on 11/19/2024 at 10:30 a.m., CNAs that worked on 11/17/2024 night shift were unavailable via telephone.
During an interview on 11/20/2024 at 9:27 a.m., the ADON stated she had worked at the facility for approximately 1 month. She stated that all showers and baths were documented in the EMR section for POC. She stated that Resident #30 did not get a bath on 11/19/2024 because the CNA was new but that it was discussed in morning meeting and she would be receiving a bed bath today. She stated that it was not appropriate for Resident #30 to get a shower because of her immobilizer brace.
During an interview on 11/20/2024 at 11:30 a.m., the DON stated she determined staffing levels based off HPPD (Hours Per Patient Day) that corporate had determined. She stated the HPPD was what had been budgeted for her to reach to staff the facility. She did not know how often the corporation reviewed the numbers but stated she felt that number was standard, and staffing was determined off the census. She stated she looked at the acuity needs of residents and she distributed the nursing staff to halls based off workload needed to care for residents. She stated she had difficulty with staffing weekends when there was an adjustment in staffing schedules. She stated both she and her ADON did work the floor when needed including weekends. She stated she had only had 1 day off since she had started working at the facility. She stated she attempted to fill in staffing shortages by posting opening with agencies the facility used. She stated they would call existing staff members and ask them to cover open shifts also. She stated staff had brought workload concerns to her and that she will rotate the CNAs to different halls so that they do not get overloaded. She stated she expected staff to come to her for help and that her door was always open. She stated she expected nurses to help the CNAs with their workload, but it had been reported to her that nurses did not help the CNAs. She stated she did not conduct exit conferences with staff on paper but did interview them. She stated most staff stated they resigned because of pay and not because of workload. She stated she did report those findings to her corporate staff members and the facility's ADMN.
During an interview on 11/20/2024 at 12:08 p.m., CNA B stated he did not perform showers or baths for Resident #30 because she preferred no male aides. He stated he did not bath Resident #30 on 11/15/2024 and did not know how his name was documented in EMR that he had performed. He stated he may have forgotten to log off documentation system and another CNA did not realize they were documenting under him.
During a confidential interview the confidential interview stated there were approximately 60 to 80 residents in the building that they were responsible for. The confidential interview stated they did not have issues completing their assignments when the facility was fully staffed but 3 CNAs were not enough. The confidential interview stated during the weekend of 11/16/2024 and 11/17/2024 the facility was not fully staffed. The confidential interview stated that only 3 CNAs worked during the day shift because an agency CNA called in and on 11/15/2024 a CNA walked out of the facility that the facility could not find coverage for. The confidential interview stated the management at the facility were aware of staffing situation but they had not been asked their opinion on staffing levels required to take care of current resident needs.
During an interview on 11/20/2024 at 1:16 p.m., the DORC provided the following information about the census:
09/25/2024 census was 69;
10/06/2024 census was 72;
11/02/2024 census was 69;
11/16/2024 census was 66;
11/17/2024 census was 67.
During an interview on 11/20/24 05:20 p.m., the ADMN stated he had heard comments from residents of not having enough staff. The ADMN stated the facility had residents with higher acuity than other residents and some of those residents would get impatient when their call light had not been answered quickly. The ADMN stated he did not have a system to address concerns. The ADMN stated he checked with the ADON who did scheduling. The ADMN stated HR conducted exit interviews with staff that would talk to them. The ADMN stated he had only been at the facility for 3 months and had not addressed staffing in QAPI meetings. The ADMN stated if the facility HPPD was 2.85 his goal was to meet that number. The ADMN stated it is difficult with no call no shows. The ADMN stated he was not aware of any days that the HPPD was not met. The ADMN stated that some of the agency staff did not always complete their documentation, and he had called that agency to report. The ADMN stated his expectation would be that staff would do their job and complete documentation. The ADMN stated he was not aware of any staff member documenting on another staff's log in. The ADMN stated blanks on documentation came down to staff having poor time management. The ADMN stated nursing management would monitor nursing documentation. The ADMN stated staffing would affect the residents in not getting what they need.
Record review of PBJ Staffing Data Report ran on 11/13/2024 revealed One Star Staffing Rating Triggered in FY Quarter 3 2024 and Excessively Low Weekend Staffing Triggered in FY Quarter 3 2024.
Record review of facility document titled Facility Assessment Tool last updated on 09/19/2024 revealed: The purpose of the assessment is to determine what resources are necessary to care for residents competently during both day-to-day operations and emergencies. Use this assessment to make decisions about your direct care staff needs, as well as your capabilities to provide services to the residents in your facility, at least annually, per the above requirement. Using a competency-based approach focuses on ensuring that each resident is provided care that allows the resident to maintain or attain their highest practicable physical, mental, and psychosocial well-being .Assistance with Activities of Daily Living .Bathing: Independent = 2; Assist of 1-2 Staff = 46; Dependent = 21 .Services and care we offer based on our Residents' Needs .Activities of daily living .Direct Care Staff plan 24 hour nursing, to include licensed staff, med aides when available, CNA staffing based off of care needs with an Average HPPD 2.85 .Staffing assignments are based off of acuity and needs, resident physical and psychological needs which are part of the admission assessments. Assessments are not only completed on admission, quarterly and prn with sig changes and as requested.
Record review of facility policy titled Resident Rights dated February 2021 revealed: 1. Federal and state laws guarantee certain basic rights to all residents of this facility. These rights include the resident's right to: a. a dignified existence; b. be treated with respect, kindness, and dignity.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure drug regimen of each resident was reviewed at least once a ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure drug regimen of each resident was reviewed at least once a month by a licensed pharmacist and failed to act upon the recommendations of the pharmacist report of irregularities for 1 of 5 residents (Resident #30) reviewed for (DRR) Drug Regimen Review.
The facility failed to have record of Resident #30's medication regimen review for anti-psychotic medication since last survey on 10/19/2023.
This failure could place resident as risk of not having their medications reviewed by pharmacy consultants for appropriate doses or pharmacy recommendations implemented.
The findings included:
Record review of Resident #30's electronic face sheet dated 11/20/2024 revealed Resident #30 was a [AGE] year-old female admitted into facility on 10/18/2022 with diagnoses to include: fracture of left patella (left knee fracture), schizoaffective disorder bipolar type (a mental health condition with a combination of symptoms including hallucinations, delusions, mania, and depression), and dementia.
Record review of Resident #30s quarterly MDS dated [DATE] revealed BIMS score of 04 which indicated severe cognitive impairment.
Record review of Resident #30's physician's orders dated 07/20/2023 revealed Anti-psychotic medication use of Abilify (aripiprazole). - Observe resident closely for significant side effects every shift.
Record review of Resident #30's physician's orders dated 08/02/2023 revealed Abilify (aripiprazole) 10mg give 1 tablet by mouth at bedtime.
Record review of the binder for Medication Regimen Review revealed no evidence of pharmacy recommendations or a physician's review of recommendation for Resident #30's Abilify. The binder was incomplete and did not have all Medication Regimen Reviews since last survey on 10/19/2023.
Record review of document titled Study of Psychoactive Utilization by Resident for records updated 7/5/2024 revealed Resident #30 used the antipsychotic aripiprazole 10mg tablet with order date of 08/02/2023 and instructions to give 1 tablet by mouth at bedtime. Further review of the document revealed comments GDR (Gradual Dose Reduction) requested in March of 2024.
During an interview on 11/20/2024 at 4:10 p.m., the ADON stated that the MRR binders from before July 2024 were not able to be located. She stated she would continue to look for documentation.
During an interview on 11/20/2024 at 4:39 p.m., the DON stated she was able to produce a psychiatric progress note that had a medication review and no recommendations for GDR. She stated she was unable to find a lot of documentation from prior to her being DON. She stated she was hired in June of 2024.
During a follow up interview on 11/20/2024 at 4:48 p.m., the DON stated she had called the psychiatric contracted service to see if they could produce any MRR paperwork. She stated the psychiatric service stated their physician did not receive paperwork about GDR recommendations. She stated she felt the Medical Director may have received that document and could not produce proof that he had been notified or that he either agreed or disagreed with GDR recommendation. She stated she was responsible for monitoring MRRs sent to the physician for review. She stated no negative outcome had occurred due to resident psychiatric need and psychiatric services documentation that the resident needed that medication.
Record review of facility policy titled Psychoactive Medications dated July 2024 revealed The attending physician and/or psychiatric provider will assume leadership in medication management by developing, monitoring and modifying the medication regimen in collaboration with residents, their families or representative, the interdisciplinary team and other professionals .Residents who use psychotropic drugs shall be evaluated for gradual dose reductions unless clinically contraindicated, in an effort to discontinue these drugs.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure that the menu was followed for the lunch meal on 11/18/24 and the supper menu on 11/19/24 for 2 of 2 meals (the lunch ...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to ensure that the menu was followed for the lunch meal on 11/18/24 and the supper menu on 11/19/24 for 2 of 2 meals (the lunch service on 11/18/24 and the supper service on 11/19/24) reviewed for nutritional adequacy.
The facility did not serve the lunch menu posted for Monday 11/18/24, but instead served the lunch menu posted for Tuesday 11/19/24 and did not inform the residents that the menu would be switched.
The facility did not follow the supper menu for Tuesday 11/19/24 and did not inform the residents that a substitute would be served.
These failures could affect all residents who ate food from the kitchen by placing them at risk of not receiving adequate nutritive food value needed to promote/maintain health.
Findings included:
Review of the weekly menu week 4 Monday lunch revealed roast pork, black-eyed peas, stewed okra and tomatoes, cornbread, and peanut butter pie. Further review of the weekly menu week 4 Tuesday lunch revealed Swiss steak, mashed potatoes, green peas, a garlic cheese biscuit, and chocolate frosted yellow cake.
Review of the weekly menu week 4 Tuesday supper revealed grilled ham, cinnamon swirl French toast, fried potatoes, and hot spiced apples.
During an observation of meal preparation and service on 11/18/24 from 11:15 AM to 12:20 PM, revealed the meal served was Salisbury steak, scalloped potatoes, mixed vegetables, a roll, and lemon cake.
During observation of meal service on 11/19/24 at 5:30 PM, revealed the meal served was hamburgers, hot dogs, potato chips, baked beans, potato salad, salad, and ice cream.
During an interview on 11/18/24 at 11:00 AM, the DM stated the facility was using Tuesday's menu today because a few residents requested no pork. She stated she spoke to a few residents, and they told her what they wanted to eat and that was why the menu was not followed today. She stated they did not inform all the other residents that the menu was being substituted. She stated she did not see any harm in changing the menu .
During a confidential meeting on 11/19/24 at 09:59 AM, 12 of 12 residents stated that the menu was rarely followed, and they did not like that it was not followed. They stated that sometimes they made decisions about meals based on the menu and were upset that the menu was not followed. They stated they could have made different arrangements for mealtimes if they had known. The resident stated they were not notified that the lunch menu on 11/17 was changed.
During an interview on 11/20/24 at 04:16 PM, the ADMN stated he was not aware that menus were not being followed or where being changed. He stated that should not happen because menus were made and provided to ensure proper nutrition was being offered. He stated that could possibly upset residents by them not knowing what they were going to eat that day and that it also impacted ordering the food and having the right amounts of foods available to prepare.
Review of facility policy titled, Menu Planning, dated 2018, revealed: Policy: The facility believes that nutrition is an important part of maintaining the wellbeing and health of its residents and is committed to providing a menu that is well-balanced, nutritious and meets the preferences of the resident population. A standardized menu which meets the nutritional recommendations of the residents in accordance with the recommended dietary allowances of the Food and Nutrition Board of the National Research Council, National Academy of Sciences will be used. Modifications for resident population and preferences may be made as appropriate. Procedure: 1. Menus will be prepared by each facility by [company] using the Menu Matrix program. Menus are updated twice each year with Spring-Summer and Fall-Winter cycles and are updated intermittently based on resident preferences. The menus will be for a five-week cycle and will include a week-at-a-glance menu, alternates, diet extensions for all diets offered for each day, nutritional analysis, standardized recipes, a production guide and an order guide. Menus are available in paper form and web-based. 2. Alternates may include a comparable entrée, vegetable and starch. An always available menu may also be offered. The alternative menu should be individualized by each facility based on their resident population and preferences. The alternate menu must also include diet extensions for each diet offered. 3. The menus are reviewed and approved by the Consultant Dietitian. Intermittent changes must also be reviewed and approved by the Consultant Dietitian. 4. The menu will be signed and dated by the Consultant Dietitian. An approved, signed copy of the menus will be kept on file in the Nutrition & Foodservice Manager 5. Dated current menus will be posted in all dining areas.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to store, prepare, distribute and serve food in accordance with professional standard or food service safety for 1 of 1 kitchen r...
Read full inspector narrative →
Based on observation, interview, and record review the facility failed to store, prepare, distribute and serve food in accordance with professional standard or food service safety for 1 of 1 kitchen reviewed for food service safety in that:
The facility failed to ensure all food items were labeled and dated.
The facility failed to ensure dietary staff used proper hand hygiene during meal preparation.
The failures could place residents who received meals and/or snacks from the kitchen at risk for food borne illness.
The findings included:
During an observation of the freezer on 11/18/24 at 09:40 AM, revealed what the DM identified as 6 pork loins, 8 loafs of bread, 1 turkey pot roast, and 4 bags of tatter tots out of original boxes with no labels and no open dates.
During an interview on 11/18/24 at 09:45 AM, the DM stated all food should have been labeled with what they were, when they expired, and when they were received. She stated not having food labeled could lead to serving expired food which could cause illness.
During an observation of meal preparation on 11/18/24 from 11:15 AM to12:20 PM, revealed the [NAME] exited the back door of the kitchen with boxes and returned to the kitchen without washing her hands. She then stocked food and supplies in the dry pantry. The [NAME] picked up trash off the floor in the kitchen and opened the trash can with her bare hands. She did not wash her hands and began filling boxes with packets of sugar. The [NAME] then exited the kitchen into the dining room and then entered the kitchen without washing her hands. She prepared coffee and dumped a coffee filter into the trash can using her hands to open the lid. The [NAME] did not wash her hands and placed a coffee filter in the coffee maker and touched the filter with her hands. The [NAME] rinsed her hands for less than 5 seconds with no soap then turned off the faucet and dried her hands. She then donned gloves and began making sandwiches. The [NAME] touched bread, meat, and cheese with gloved hands. She then went to the freezer to pour a glass of milk with the same gloves on and then went back to sandwich making.
During an interview on 11/18/24 on12:45 PM, the [NAME] stated she did wash her hands and she used gloves. She stated she did not feel that she did anything wrong.
During an interview on 11/18/24 at 02:00 PM, the DM stated her expectation was for her employees to wash their hands every time they entered the kitchen, anytime they entered the back of the kitchen in the dish area because it was dirty, any-time they go from on task to another. She stated gloves should be changed with each task and does not count as handwashing. She stated she did observe the cook not washing her hands as necessary during meal service today. She stated not using proper hand hygiene could lead to cross contamination and the spread of infection. She stated her staff was in-serviced last week regarding hand hygiene.
During an interview on 11/20/24 at 04:16 PM, the ADMN stated all food should be labeled and dated. He stated it was the DM's responsibility to ensure that policies and procedures were followed. He stated he did monitor and performed rounds in the kitchen to ensure that was being done. He stated a possible negative outcome could be serving expired food, but it was unlikely because they used the food quickly.
Review of facility policy titled, Food Storage, dated 2018, revealed in part: Policy: To ensure that all food served by the facility is of good quality and safe for consumption, all food will be stored according to the state, federal and US Food Codes and HACCP guidelines. Procedure: .3. Freezers .e. Store frozen foods in a moisture-proof wrap or containers that are labeled and dated .
Review of facility policy titled, Hand Washing, dated 2018, revealed in part: Policy: The facility recognized that food-borne illness has the potential to harm elderly and frail residents. All Nutrition & Foodservice employees will practice good hand washing practices in order to minimize the risk of infection and food borne illness. Procedure .2. Hands should be washed after the following occurrences .h. Taking out garbage i. Clearing tables j. Touching clothing or aprons k. Touching un-sanitized equipment, work surfaces, or wash cloths l. Assisting residents 3. Hand-washing steps a. wet hands and exposed arms with hot water at least 100 degrees. B. Apply soap. C. Scrub hands, exposed arms, and fingernails for a minimum of 20 seconds being sure to apply vigorous friction. D. Rinse hands and exposed arms thoroughly under hot running water. E. Dry hands and arms with a paper towel. F. Turn off the faucet with the paper towel to avoid contaminating hands and discard towel.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record reviews, the facility failed to maintain an infection prevention and control progra...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record reviews, the facility failed to maintain an infection prevention and control program designed to provide a safe, sanitary, and comfortable environment and to help prevent the development and transmission of communicable diseases and infections for 3 of 3 (CNA-B, CNA-C and CNA-D) staff observed during incontinent care.
The facility failed to ensure CNA B, CNA C, and CNA D performed proper peri-care (incontinent care) and proper hand hygiene during peri-care for Resident #23 and Resident #12.
These failures placed residents of the facility at risk of infections from improper incontinent care and hand hygiene while performing incontinent care.
Findings included:
Resident #23
Record Review of the Resident #23's Face Sheet dated 11/19/2024, revealed he was a [AGE] year-old male. His original admission to the facility was on 2/08/2022 with his most recent admission on [DATE]. Resident #23 had a diagnosis of Cerebral Infarction (stroke), and non-pressure chronic ulcer of buttock limited to breakdown of skin.
Record review of Resident #23's MDS assessment Section C, Cognitive Patterns dated 05/12/2023, revealed a BIMS score of 07 (severe impairment).
Record review of Resident #23's Care Plan dated 10/1/2024 Category: ADLs Functional
Status/Rehabilitation Potential revealed: Problem: Resident #23 has self-care deficits R/T impaired cognition, impaired mobility, Multiple Sclerosis, incontinence, and impaired balance. Goal: Resident will achieve maximum functional mobility.
During an observation on 11/18/2024 at 10:00 AM, revealed CNA-B and CNA-C both performed peri-care for Resident #23. CNA-B had started peri care from the back to front with continuous wiping back and forth with each wipe used. CNA-C was helping and observing CNA-B failed to correct CNA-B. Observation also revealed CNA-A and CNA-B had not used hand sanitizer, nor did they wash their hands in between changing gloves during per care.
During an interview on 11/18/2024 at 11:56 AM, CNA-B stated she knew she had not used hand sanitizer, nor did she wash her hands in between changing her gloves during peri care. She stated she should have done so but was nervous. She stated she should have started cleaning the resident from front to back and she was not to supposed to use one wipe several times over before discarding. She stated in doing so could have caused possible UTIs and cross contamination.
During an interview 11/18/2024 at 11:56 AM, CNA-C stated the peri care she had provided had not been done correctly with Resident #32 as CNA-B observed and helped. She stated it was supposed to have been from front to back, using only one wipe per swipe. She stated CNA-B was also not to wipe back and forth with one wipe. She stated in doing so could have caused infections and E.coli, (Escherichia coli), a form of bacteria, as well as skin breakdown.
Resident #12
Record review of the resident #12's Face Sheet dated 11/19/2024, revealed she was a 59 yr. old female. Her admission date to the facility was on 2/26/2024. Resident #12 had a diagnosis of irritant contact dermatitis due to friction or contact with body fluids, diarrhea, and lack of coordination.
Record review of Resident #12's MDS assessment Section C, Cognitive Patterns dated 9/26/2024, revealed a BIMS score of 09 (moderately impaired).
Record review of Resident #12''s Care Plan dated 10/10/2024 Category: ADLs Functional Status/Rehabilitation Potential revealed: Problem: Resident had self-care deficits R/T impaired mobility, impaired decision making, and impaired safety awareness. Goal: Residents care needs will be met daily and PRN
and res will maintain optimal level of functioning. Approach: Bathing/hygiene amount of assist: 1-2 Assist.
During an observation on 11/18/2024 at 11:14 AM, CNA-B and CNA-D both performed peri-care for Resident #12. Neither CNA-B and CNA-D performed hand washing nor used hand sanitizer throughout peri-care. CNA-D was also observed folding each wipe 2-3 times, wiped the resident s several times with one wipe before discarding. CNA-D also had not removed her dirty gloves prior to touching residents call light and bed control after performing peri care.
During an interview on 11/18/2024 at 11:48 AM CNA D stated she had not washed her hands between changing her gloves as well as not changing her gloves after changing the resident during peri care. She stated she had not taken enough gloves into the resident's room prior to peri-care and that was why she did not change them when she was supposed to have.
During interview on 11/20/2024 at 9:18 AM the DON stated staff were to change gloves and sanitize their hand in between the changing of gloves. She stated staff should not have touched the residents bed control without taking the dirty gloves off and having used proper hand hygiene. She stated the negative impact to residents was the possibility of cross contamination which could lead to death, and/or become septic and spread infection. The DON stated her expectations were for staff to be proficient before going to work on the floor. She stated it was herself as the facility DON who should have monitored. The DON stated the failure occurred with not having implemented a standard training procedure prior to placing the aids on the floor for resident care.
Record review of facility policy titled Handwashing/Hand Hygiene dated 1/20/2023 revealed:
Policy Statement
This facility considers hand hygiene the primary means to prevent the spread of infections.
Policy Interpretation and Implementation
1. All personnel shall follow the handwashing/hand hygiene procedures to help prevent the spread of infections to other personnel, residents, and visitors.
2. Residents, family members and/or visitors will be encouraged to practice hand hygiene throughout the facility.
3. Wash hands with soap and water, when hands are visibly soiled and after contact with resident with an infectious diagnosis.
4. Use an alcohol-based hand rub containing at least 60% to 95% ethanol alcohol or isopropyl alcohol.
5. Hand hygiene must be performed prior to donning and after doffing gloves.
6. Hand hygiene is the final step after removing and disposing of personal protective equipment
Procedure
Washing Hands
1. Wet hands first with water, then apply soap.
2. Lather your hands by rubbing them together with the soap. Lather the back of your hands between your fingers and under the nails.
3. Scrub your hands for at least 20 seconds.
4. Rinse your hands well under clean, running water.
5. Dry your hands using a clean towel and use a towel to turn off the faucet.
Using Alcohol-Based Hand Rubs
1. Apply generous amount of product to palm of hand and rub hands together.
2. Cover all surfaces of hands and fingers until hands are dry.
Record review of facility policy titled Perineal Care dated 1/20/2023 revealed:
Policy Statement
Perineal Care is providing cleanliness and comfort to the resident, to prevent infections, skin irritation, and to observe the resident's skin condition.
Equipment and Supplies
The following equipment and supplies needed include, but are not limited to the following:
1. Disposable cleansing wipes;
2. Linens; and
3. Personal protective equipment (e.g., gowns, gloves, mask, etc., as needed).
Steps in the Procedure
1. Introduce self to resident and explain care that will be provided.
2. Provide privacy. i.e., pull curtain, close door.
3. Perform hand hygiene and don gloves.
4. Arrange the supplies so they can be easily reached.
5. Adjust bedding to resident's comfort and provide dignity during care.
6. Remove clothing enough to perform peri-care. Avoid unnecessary exposure of the resident's body.
7. Remove the soiled clothing, linens, and brief. Place items in the proper receptacle.
8. Encourage the resident to participate in care as able.
A. For a Female Resident:
(1) Using the cleansing wipe, clean perineal area, wiping from front to back. Use a clean section of the cleansing wipe for each stroke by folding each used section inward.
(2) Separate labia and wash area downward from front to back. (Note: If the resident has an indwelling catheter, gently wash the juncture of the tubing from the urethra down the catheter about 3 inches. Gently rinse and dry the area.)
(3) Continue to clean the perineum moving from inside outward to the thighs, cleanse the perineum thoroughly in same direction, using a new cleansing wipe, as needed.
(4) If the resident has an indwelling catheter, hold the catheter to one side and support the tubing against the leg to avoid traction or unnecessary movement of the catheter.
(5) Gently dry perineum.
(6) Ask the resident to turn on her side with her top leg slightly bent, if able.
(7) Using a new cleansing wipe, clean the rectal area thoroughly, wiping from the base of the labia and extending over the buttocks. Use a clean section of the cleansing wipe for each stroke by folding each used section inward. Use a new cleansing wipe, as needed.
(8) Reposition the bed covers. Make the resident comfortable.
(9) Place the call light within easy reach of the resident.
(10) Perform Hand Hygiene.
(11) Discard disposable items into designated containers.
(12) Remove gloves and discard into designated container.
(13) Perform Hand Hygiene.
B. For a Male Resident:
(1) Use a cleansing wipe.
(2) Clean perineal area starting with urethra and working outward.
(3) If the resident has an indwelling catheter, gently wash the juncture of the tubing from the urethra down the catheter about 3 inches. Gently clean and dry the area.
(4) Retract foreskin of the uncircumcised male.
(5) Clean urethral area with a cleansing wipe using a circular motion. Use a clean section of the cleansing wipe for each stroke by folding each used section inward. Use a new cleansing wipe, as needed.
(6) Continue to clean the perineal area including the penis, scrotum, inner thighs.
(7) Thoroughly clean perineal area in same order, using a new cleansing wipe as needed.
(8) If the resident has an indwelling catheter, hold the tubing to one side and support the
Revised 1/20/23 2
tubing against the leg to avoid traction or unnecessary movement of the catheter.
(9) Gently dry perineum following same sequence.
(10) Reposition foreskin of uncircumcised male.
(11) Ask the resident to turn on his side with his upper leg slightly bent, if able.
(12) Clean the rectal area thoroughly, including the area under the scrotum, the anus, and
the buttocks, change the cleansing wipe, as needed. Use a clean section of the
cleansing wipe for each stroke by folding each used section inward.
10. Dry area thoroughly.
11. Discard disposable items into designated containers.
12. Remove gloves and discard into designated container.
13. Perform Hand Hygiene.
14. Reposition the bed covers. Make the resident comfortable.
15. Place the call light within easy reach of the resident.
16. Perform Hand Hygiene.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0941
(Tag F0941)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure employees received the required training effective communications mandatory training for 4 of 16 employees (DON, CNA B, LVN F, and R...
Read full inspector narrative →
Based on interview and record review, the facility failed to ensure employees received the required training effective communications mandatory training for 4 of 16 employees (DON, CNA B, LVN F, and RN I) reviewed for training.
The facility did not ensure effective communication training was completed by the DON and CNA B during orientation.
The facility did not ensure effective communication training was completed by RN I and LVN F annually.
These failures could place residents at risk of miscommunication and social isolation due to lack of staff training.
Findings included:
Record review of the employee files revealed no evidence that the following staff had completed effective communications training during orientation:
DON hire date 6/24/2024
CNA B hire date 11/11/2024
Record reviews of the employees' files revealed no evidence the following staff had completed effective communications training annually:
RN I hire date 9/27/2022
LVN F hire date 2/22/2023
During an interview on 11/18/2024 at 11:56 a.m., CNA B stated she had filled out hiring paperwork on the orientation app but had not done orientation or had done a checkoff list prior to being placed on the floor and working. She stated the DON told her since she was already a CNA, she could work on the floor her first day.
During an interview on 11/20/2024 at 6:16 p.m., the CHRL stated the DON did not have communication training until 11/19/2024, CNA B had communication training on 11/18/2024 but there was no evidence on what time the training occurred. The CHRL stated RN I and LVN F did not complete annual communications training. She stated each department head was responsible for making sure their staff have received all the required training. She stated there was a combination team work to monitor training performed due to HR cannot perform certain educational trainings. She stated ultimately the ADMN should hold supervisors responsible for their staff training. She stated a well-trained staff member would provide the best care. She stated staff may not provide the best care without the required training. She stated there had been changes in the leadership team in the last couple of months that may have led to failure. She stated those changes have had a huge impact and the leaders needed to get back into a good routine.
During an interview on 11/20/2024 at 7:27 p.m., the ADMN stated his expectation would be for staff to receive the required annual and orientation training. He stated prior to his time at the facility, he did not know why training was not completed. The ADMN stated HR was responsible for training being completed. He stated corporate HR was responsible for monitoring that training had been done. He stated the effect on residents from training not being completed depended on how much experience an employee had prior to starting with the company. He stated he had not seen major ill effects of various degrees of training not being performed.
Record review of facility document titled Facility Assessment Tool last updated on 09/19/2024 revealed: staff training/education and competencies 3.4. Describe the staff training/education and competencies that are necessary to provide the level and types of support and care needed for your resident population. Include staff certification requirements as applicable. Potential data sources include hiring, education, training, competency instruction, and testing policies. It may be helpful to review specific references in the regulation regarding facility assessment. List (or refer to or provide a link to) all staff training and competencies needed by type of staff. Consider if it would be helpful to indicate which competencies are reviewed at the time the staff member is hired, and how often they are reviewed after that.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0942
(Tag F0942)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure employees received the required training on resident rights mandatory training for 2 of 16 employees (RN I and LVN F) reviewed for t...
Read full inspector narrative →
Based on interview and record review, the facility failed to ensure employees received the required training on resident rights mandatory training for 2 of 16 employees (RN I and LVN F) reviewed for training requirements in that:
The facility did not ensure resident rights training was completed by RN I and LVN F annually.
This failure could place residents at risk of receiving care from staff who were insufficiently trained.
The findings included:
Record reviews of the employees' files revealed no evidence the following staff had completed resident rights training annually:
o
RN I hire date 9/27/2022
o
LVN F hire date 2/22/2023
During an interview on 11/20/2024 at 6:16 p.m., the CHRL stated RN I and LVN F did not complete annual resident rights training. She stated each department head is responsible for making sure their staff have received all the required training. She stated there was a combination team work to monitor training performed due to HR cannot perform certain educational trainings. She stated Ultimately the ADMN should hold supervisors responsible for their staff training. She stated a well-trained staff member would provide the best care. She stated staff may not provide the best care without the required training. She stated there had been changes in the leadership team in the last couple of months that may have led to failure. She stated those changes have had a huge impact and the leaders needed to get back into a good routine.
During an interview on 11/20/2024 at 7:27 p.m., the ADMN stated his expectation would be for staff to receive the required annual and orientation training. He stated prior to his time at the facility, he did not know why training was not completed. The ADMN stated HR was responsible for training being completed. He stated corporate HR was responsible for monitoring that training had been done. He stated the effect on residents from training not being completed depended on how much experience an employee had prior to starting with the company. He stated he had not seen major ill effects of various degrees of training not being performed.
Record review of facility document titled Facility Assessment Tool last updated on 09/19/2024 revealed: staff training/education and competencies 3.4. Describe the staff training/education and competencies that are necessary to provide the level and types of support and care needed for your resident population. Include staff certification requirements as applicable. Potential data sources include hiring, education, training, competency instruction, and testing policies. It may be helpful to review specific references in the regulation regarding facility assessment. List (or refer to or provide a link to) all staff training and competencies needed by type of staff. Consider if it would be helpful to indicate which competencies are reviewed at the time the staff member is hired, and how often they are reviewed after that.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure employees received the required training on activities that constitute abuse, neglect, exploitation, and misappropriation of residen...
Read full inspector narrative →
Based on interview and record review, the facility failed to ensure employees received the required training on activities that constitute abuse, neglect, exploitation, and misappropriation of resident property and procedures for reporting incidents of abuse, neglect, exploitation, or the misappropriation of resident property and dementia management for 2 (RN I and LVN F) of 19 employees reviewed for staff training.
The facility did not ensure abuse, neglect, exploitation, and misappropriation of resident property and procedures for reporting training was completed by RN I and LVN F annually.
These failure could place the residents at risk of abuse, neglect, exploitation, and misappropriation.
The findings included:
Record reviews of the employees' files revealed no evidence the following staff had completed activities that constitute abuse, neglect, exploitation, and misappropriation of resident property and procedures for reporting incidents of abuse, neglect, exploitation, or the misappropriation of resident property and dementia management training annually:
o
RN I hire date 9/27/2022
o
LVN F hire date 2/22/2023
During an interview on 11/20/2024 at 6:16 p.m., the CHRL stated RN I and LVN F did not complete annual abuse, neglect, exploitation, and misappropriation of resident's property training. She stated each department head is responsible for making sure their staff have received all the required training. She stated there was a combination team work to monitor training performed due to HR cannot perform certain educational trainings. She stated Ultimately the ADMN should hold supervisors responsible for their staff training. She stated a well-trained staff member would provide the best care. She stated staff may not provide the best care without the required training. She stated there had been changes in the leadership team in the last couple of months that may have led to failure. She stated those changes have had a huge impact and the leaders needed to get back into a good routine.
During an interview on 11/20/2024 at 7:27 p.m., the ADMN stated his expectation would be for staff to receive the required annual and orientation training. He stated prior to his time at the facility, he did not know why training was not completed. The ADMN stated HR was responsible for training being completed. He stated corporate HR was responsible for monitoring that training had been done. He stated the effect on residents from training not being completed depended on how much experience an employee had prior to starting with the company. He stated he had not seen major ill effects of various degrees of training not being performed.
Record review of facility document titled Facility Assessment Tool last updated on 09/19/2024 revealed: staff training/education and competencies 3.4. Describe the staff training/education and competencies that are necessary to provide the level and types of support and care needed for your resident population. Include staff certification requirements as applicable. Potential data sources include hiring, education, training, competency instruction, and testing policies. It may be helpful to review specific references in the regulation regarding facility assessment. List (or refer to or provide a link to) all staff training and competencies needed by type of staff. Consider if it would be helpful to indicate which competencies are reviewed at the time the staff member is hired, and how often they are reviewed after that.
Record review of facility document titled Abuse, Neglect, and Exploitation dated October 2023 revealed: Existing staff will receive annual education through planned in-services and/or assigned web-based trainings and as needed.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0945
(Tag F0945)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure employees received the required training an infection prevention and control program mandatory training for 4 of 16 employees (DON, ...
Read full inspector narrative →
Based on interview and record review, the facility failed to ensure employees received the required training an infection prevention and control program mandatory training for 4 of 16 employees (DON, CNA B, LVN F, and RN I) reviewed for training.
The facility did not ensure an infection prevention and control program training was completed by the DON and CNA B during orientation.
The facility did not ensure an infection prevention and control program training was completed by RN I and LVN F annually.
These failure could affect residents and place them at risk of poor care or infections due to lack of staff training.
Findings included:
Record review of the employee files revealed no evidence that the following staff had completed an infection prevention and control program training during orientation:
DON hire date 6/24/2024
CNA B hire date 11/11/2024
Record reviews of the employees' files revealed no evidence the following staff had completed an infection prevention and control program training annually:
RN I hire date 9/27/2022
LVN F hire date 2/22/2023
During an interview on 11/18/2024 at 11:56 a.m., CNA B stated she had filled out hiring paperwork on the orientation app but had not done orientation or had done a checkoff list prior to being placed on the floor and working. She stated the DON told her since she was already a CNA, she could work on the floor her first day.
During an interview on 11/20/2024 at 6:16 p.m., the CHRL stated the DON did not have an infection prevention and control program until 11/19/2024, CNA B had an infection prevention and control program on 11/18/2024 but there was no evidence on what time the training occurred, RN I and LVN F did not complete annual infection prevention and control program training. She stated each department head is responsible for making sure their staff have received all the required training. She stated there was a combination team work to monitor training performed due to HR cannot perform certain educational trainings. She stated ultimately the ADMN should hold supervisors responsible for their staff training. She stated a well-trained staff member would provide the best care. She stated staff may not provide the best care without the required training. She stated there had been changes in the leadership team in the last couple of months that may have led to failure. She stated those changes have had a huge impact and the leaders needed to get back into a good routine.
During an interview on 11/20/2024 at 7:27 p.m., the ADMN stated his expectation would be for staff to receive the required annual and orientation training. He stated prior to his time at the facility, he did not know why training was not completed. The ADMN stated HR was responsible for training being completed. He stated corporate HR was responsible for monitoring that training had been done. He stated the effect on residents from training not being completed depended on how much experience an employee had prior to starting with the company. He stated he had not seen major ill effects of various degrees of training not being performed.
Record review of facility document titled Facility Assessment Tool last updated on 09/19/2024 revealed: staff training/education and competencies 3.4. Describe the staff training/education and competencies that are necessary to provide the level and types of support and care needed for your resident population. Include staff certification requirements as applicable. Potential data sources include hiring, education, training, competency instruction, and testing policies. It may be helpful to review specific references in the regulation regarding facility assessment. List (or refer to or provide a link to) all staff training and competencies needed by type of staff. Consider if it would be helpful to indicate which competencies are reviewed at the time the staff member is hired, and how often they are reviewed after that.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0946
(Tag F0946)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure employees received the required training on compliance and ethics mandatory training for 4 of 16 employees (DON, CNA B, LVN F, and R...
Read full inspector narrative →
Based on interview and record review, the facility failed to ensure employees received the required training on compliance and ethics mandatory training for 4 of 16 employees (DON, CNA B, LVN F, and RN I) reviewed for training.
The facility did not ensure compliance and ethics training was completed by the DON and CNA B during orientation.
The facility did not ensure compliance and ethics training was completed by RN I and LVN F annually.
These failure could affect residents and place them at risk of poor care or victimization due to lack of staff training.
Findings included:
Record review of the employee files revealed no evidence that the following staff had completed compliance and ethics training during orientation:
DON hire date 6/24/2024
CNA B hire date 11/11/2024
Record reviews of the employees' files revealed no evidence the following staff had completed compliance and ethics training annually:
RN I hire date 9/27/2022
LVN F hire date 2/22/2023
During an interview on 11/18/2024 at 11:56 a.m., CNA B stated she had filled out hiring paperwork on the orientation app but had not done orientation or had done a checkoff list prior to being placed on the floor and working. She stated the DON told her since she was already a CNA, she could work on the floor her first day.
During an interview on 11/20/2024 at 6:16 p.m., the CHRL stated the DON did not have compliance and ethics training until 11/19/2024, CNA B had compliance and ethics training on 11/18/2024 but there was no evidence on what time the training occurred, RN I and LVN F did not complete annual compliance and ethics training. She stated each department head is responsible for making sure their staff have received all the required training. She stated there was a combination team work to monitor training performed due to HR cannot perform certain educational trainings. She stated ultimately the ADMN should hold supervisors responsible for their staff training. She stated a well-trained staff member would provide the best care. She stated staff may not provide the best care without the required training. She stated there had been changes in the leadership team in the last couple of months that may have led to failure. She stated those changes have had a huge impact and the leaders needed to get back into a good routine.
During an interview on 11/20/2024 at 7:27 p.m., the ADMN stated his expectation would be for staff to receive the required annual and orientation training. He stated prior to his time at the facility, he did not know why training was not completed. The ADMN stated HR was responsible for training being completed. He stated corporate HR was responsible for monitoring that training had been done. He stated the effect on residents from training not being completed depended on how much experience an employee had prior to starting with the company. He stated he had not seen major ill effects of various degrees of training not being performed.
Record review of facility document titled Facility Assessment Tool last updated on 09/19/2024 revealed: staff training/education and competencies 3.4. Describe the staff training/education and competencies that are necessary to provide the level and types of support and care needed for your resident population. Include staff certification requirements as applicable. Potential data sources include hiring, education, training, competency instruction, and testing policies. It may be helpful to review specific references in the regulation regarding facility assessment. List (or refer to or provide a link to) all staff training and competencies needed by type of staff. Consider if it would be helpful to indicate which competencies are reviewed at the time the staff member is hired, and how often they are reviewed after that.
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on interview the facility failed to ensure the DON did not serve as a charge nurse when the facility had an average daily occupancy of 60 or more residents for 6 (11/02/24, 11/03/24, 11/09/24, 1...
Read full inspector narrative →
Based on interview the facility failed to ensure the DON did not serve as a charge nurse when the facility had an average daily occupancy of 60 or more residents for 6 (11/02/24, 11/03/24, 11/09/24, 11/15/24, 11/16/24, and 11/17/24) of 20 days reviewed for DON coverage.
The facility failed to ensure the DON did not serve as a charge nurse when the facility had an average daily occupancy of 60 or more residents on 11/02/24, 11/03/24, 11/09/24, 11/15/24, 11/16/24, and 11/17/24.
This failure left residents without the nursing administrative oversight that only the DON can provide.
Findings include :
During an interview 11/20/24 at 01:57 PM, the DON stated she had worked the floor on 11/02/24, 11/03/24, 11/09/24, 11/15/24, 11/16/24, and 11/17/24 because the facility was short staffed. She stated she worked the floor a couple days a week. She stated the negative effect was that she could not perform her DON duties. She stated she was not aware of the regulation stating that she could not work the floor. She stated corporate told her it was her responsibility to make sure the floor was covered even if it required her to work it. The DON stated she had worked 6 floor shifts in the last 20 days. She stated there was no way to prove that she worked the floor because she did not clock in.
During an interview on 11/20/24 at 04:16 PM, the ADMN stated the DON did work the floor as a charge nurse quite often. He stated if there was no nurse to work, the residents must be taken care off. He stated she had to work the floor because the facility was short staffed. The ADMN confirmed the DON worked the floor on 11/02/24, 11/03/24, 11/09/24, 11/15/24, 11/16/24, and 11/17/24. The ADMN stated he was not aware of the regulation stating the DON could not work as a charge nurse.
The policy for RN/DON coverage was requested on 11/20/2024 at 8:15 pm but was not provided.
MINOR
(B)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
MDS Data Transmission
(Tag F0640)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to ensure an encoded, accurate, and complete MDS discharge assessmen...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to ensure an encoded, accurate, and complete MDS discharge assessment was electronically transmitted to the CMS System for 1 (Resident #36) of 1 resident records reviewed for closed records. include the discharge assessment was not transmitted to CMS within 14 days of completion.
The facility did not ensure the discharge MDS assessment was completed and electronically transmitted as required for Resident #36.
This failure could place residents at risk of facility not providing complete and specific information for payment and quality of measure purposes.
Findings included:
Record review of Resident #36's electronic face sheet revealed [AGE] year-old male admitted [DATE]. Diagnoses include chronic obstructive pulmonary disease (lung disease), hypokalemia (low potassium), malignant neoplasm of colon (colon cancer), and pain. Further review of the electronic face sheet revealed the resident was discharged on 08/05/2024 to another facility.
Record review of Resident #36's discharge MDS dated [DATE] revealed, In Process and had not been electronically transmitted.
During an interview on 11/20/2024 at 02:54 PM with the MDS Coordinator, she stated she believed she had 7 or 14 days to complete and submit a discharge MDS. The MDS Coordinator stated she did not think that not submitting discharge MDS would affect the resident in any way. The MDS Coordinator stated she did not know what caused this failure. The MDS Coordinator stated her Regional MDS Coordinator monitored the MDS process.
During an interview on 11/20/2024 at 03:15 the Regional MDS Coordinator stated she did not know why a discharge MDS dated [DATE] would not have been electronically transmitted within the proper time frame. The Regional MDS Coordinator stated a discharge MDS should have been electronically transmitted within 7 days of discharge. The Regional MDS Coordinator stated she did not know how this failure occurred and did not believe this would affect the resident.
During an interview on 11/20/2024 at 03:20 PM the DON stated she was not aware of any discharge MDS not being electronically transmitted in timely manner. The DON stated she did know how this failure occurred and did not believe this failure would affect the discharged resident.
Review of facility's policy titled: Electronic Transmission of the MDS dated Revised November 2019 revealed:
All MDS assessments (e.g., admission, annual, significant change, quarterly reviews, etc.) and discharge and reentry records are completed and electronically encoded into our facility's MDS information system and transmitted to CMS' QIES Assessment Submission and Processing (ASAP) system in accordance with current OBRA regulations governing the transmission of MDS data.
All staff members responsible for completion of the MDS receive training on the assessment, data entry, and transmission processes, in accordance with the MDS RAI Instruction Manual, before being permitted to use the MDS information system. A copy of the MDS RAI Instruction Manual is maintained by the Resident Assessment Coordinator .