CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Record review of Resident #11's admission record dated 10/25/23 documented a [AGE] year-old female admitted to the facility on [...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Record review of Resident #11's admission record dated 10/25/23 documented a [AGE] year-old female admitted to the facility on [DATE] and discharged on 09/20/23. The form further documented Resident #11 with diagnoses including, unspecified dementia (a group of thinking and social symptoms that interfere with daily functioning), muscle wasting and atrophy (a decrease of muscle mass and strength), age-related physical debility (group of symptoms related to age that cause frailty), lack of coordination (group of symptoms that cause impaired direction) , and unspecified hearing loss (inability to hear). Resident #11 was not identified as her own responsible party.
Record review of Resident #11's quarterly minimum data set (MDS) revealed a BIMS score of 99 indicating severe cognitive impairment. It further documented Resident #11 required a walker for mobility and required supervision when walking up to 10 feet. The MDS documented, Resident #11 did not use a wander/elopement alarm. Furthermore, the form documented a 0 when asked Has the resident wandered?, indicating the behavior had not been exhibited.
Record review of Resident #11's comprehensive care plan documented Resident #11 was an elopement risk/wanderer related to attempts to leave facility unattended with an initiated date of 09/19/23. Resident #11's care plan stated The resident's safety will be maintained through the review date and the resident will not leave the facility unattended through the review date with a revision date of 09/26/23. Interventions included, 09/19/23 elope from facility, door codes changed, 1:1 monitoring, moved to room closer to nurse station, wander guard, alarms checked and functional, critical behavior monitoring, will be transferred to secured unit upon bed availability .complete wandering evaluation tool .identify pattern of wandering . All with initiation date of 09/19/23.
Record review of Resident #11 physician order revealed an order to verify function of wander guard daily and wander guard in place .verify placement every shift for elopement with a start date of 09/20/23 and that was discontinued with no end date noted.
Record review of Resident #11 September 2023 licensed nurse administration record dated 10/26/23 revealed order had been completed and documented for every shift on 09/20/23 as ordered.
Record review of Resident #11 Wandering Evaluation completed upon admission on [DATE] at 08:23 a.m., documented a summary of finding score of four (4) indicating resident was a low risk for wandering. Resident #11 was not a wandering risk at that time.
Record review of Resident #11 wandering re-evaluation completed on 09/19/23 at 10:30 a.m. documented a summary of findings score of five (5) indicating resident was a low risk for wandering. Furthermore, document recorded Resident #11 was a wandering risk and interventions and care plans had been re-evaluated
Record review of Resident #11 progress notes with an effective date 09/19/23 at 12:24 p.m. and written by Staff M revealed a CNA last saw Resident #11 at approximately 09:00 a.m.
Record review of Resident #11's progress notes signed and dated 09/19/23 at 12:50 p.m. by Staff J quoted in part, family in to see Resident #11 at 10:30 a.m., Staff E assisted family with locating resident. Resident #11 not found in facility. Facility conducted 100% of room search in the facility. Resident was last seen in facility by Staff L at around 09:00 a.m. Staff began to search for Resident #11inside and outside facility, restaurants, gas stations, stores, and surrounding neighborhoods; however Resident #11 was not located anywhere. Local police department notified at approximately 11:00 a.m. DON spoke to Officer regarding details describing Resident #11's last whereabouts and clothing worn. At approximately 11:30 a.m., Resident #11 was located by local police department walking on a street. Resident #11 was brought back to facility. Physician and family were made aware.
Record review of Resident #11 Change of condition communication form dated 09/23 at 12:47 p.m. revealed the change in conditions, symptoms or signs to report: Pt (patient) had incident of elopement .this started on 09/19/23 . Nurse suggestion .Transfer to the hospital.
Record review of Resident #11's weekly skin evaluation signed and dated 09/19/23 at 12:59 p.m. revealed resident did not have any abnormal skin areas i.e., bruises, skin tears, pressure ulcers, non-pressure wounds etc.
Record review of Resident #11's pain evaluation signed and dated 09/19/23 at 12:59 p.m. revealed resident had no pain upon return to facility on 09/19/23.
Record review of Resident #11 progress notes with an effective date of 09/19/23 at 13:20 p.m. and written by Staff J quoted in part, Resident was returned to facility by PD at approximately 1200 p.m. Resident is alert and oriented x 2. Patient denies pain at this time. Head to toe assessment conducted, no bumps or lesions noted to head .doctor, new order received: transfer resident to DHR ER for evaluate and treat. FM A in facility and aware and in agreement.
Record review of Resident #11 progress notes with an effective date of 09/19/23 at 13:35 p.m. and written by Staff J, quoted in part, EMS in facility to transport resident to ER, family at bedside. Resident is calm and cooperative. Resident exited the facility at approximately 1330. Report called in by Staff E to ER staff.
Record review of Resident #11 progress notes with an effective date of 09/19/23 at 20:42 p.m., quoted in part, Resident arrived from [hospital] awake, alert and VWNL (vital signs within normal limits) denies any pain or discomfort N/O (new orders) Keflex (antibiotic) 500 (milligram) capsule give 1 cap (capsule) QID (four times a day) x 5 (times five) days. Order carried out. Initial dose given no adverse reactions noted.
Record review of Resident #11 progress notes with an effective date of 09/19/23 at 06:03 a.m., quoted in part, Resident slept well during the night continues. 1:1.
Record review of Resident #11 progress notes with an effective date of 09/20/23 at 10:46 a.m., quoted in part, Resident in room talking on the phone with a family member. 1:1 aide at bedside. Patient calm and cooperative. Wander guard in place to left wrist. Will continue to monitor.
Record review of TULIP (HHSC online incident reporting application on 10/24/23 at 09:00 a.m. revealed the facility made a self-reported incident on 09/19/23 at 10:30 a.m. regarding Resident #11's elopement.
Record review of the facility map and evacuation routes, revealed a total of nine (9) exits were identified as exit doors.
Initial rounds were conducted on 10/24/23 beginning at 11:00 a.m. throughout the facility. The facility was well lit, temperature was comfortable, and staff were seen appropriately interacting and assisting residents in their rooms and in the hallways. The facility was clean, well-lit, the ambient was comfortable with comfortable temperature and noise level. Resident rooms were clean, orderly, without any noted hazards or clutter. There were no sounds of yelling, screaming, or moaning. Residents in bed had their call lights within their reach. Call lights were observed activated and timely answered. Nurses were administering care and medications in a timely manner. Water and belongings were observed at the bedside of the residents and within their reach. No resident was observed to display any disrupting or aggressive behaviors. No injuries or bruising was noted on any resident that would raise suspicion of abuse or neglect. There were no active cases of COVID-19 positive residents in the building. Visitors were observed entering and exiting through the main entrance after being allowed entrance. Residents in designated smoking area being observed monitored. Other exit doors locked and secured with codes and screech alarm.
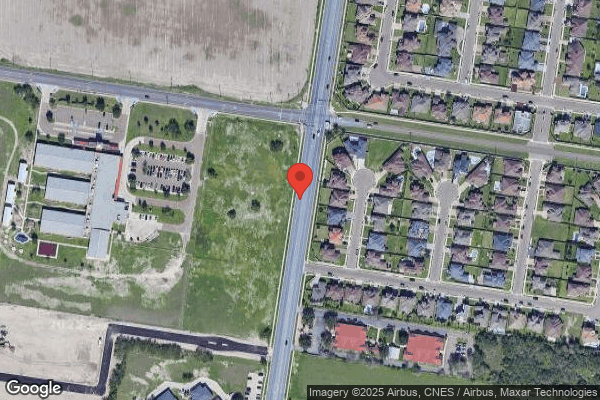
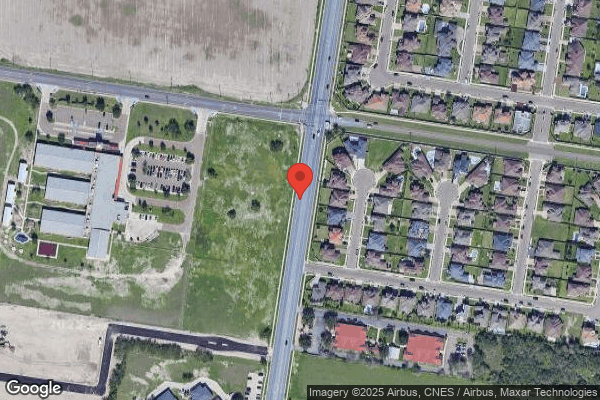
Observation on 10/24/23 at 11:00 a.m. of the surrounding streets revealed a highly trafficked four lane road with a center lane and a speed limit of 40 miles per hour.
In a telephone interview with FM A on 10/26/23 at 08:10 a.m. revealed she and an unnamed family member came to visit Resident #11 on 09/19/23. FM A stated she arrived at the facility at 09:55 a.m. and went straight to Resident #11's room. FM A stated after she did not find Resident #11 in her room, she decided to look in the room she was previously assigned to because she had been moved the day before. FM A stated again she could not find Resident #11. FM A stated she then decided to look in other areas of the facility including the activities area, designated smoking area, therapy, and the lounge. FM A stated that once she eliminated the areas where she believed Resident #11 could be, she then asked the staff for the whereabouts of Resident #11. FM A stated a staff member stated she was in the shower. FM A stated she decided to wait until Resident #11 came out from the shower, but after 20 minutes had gone by and Resident #11 did not come out from the shower, she inquired again to staff about the whereabouts of Resident #11. FM A stated staff then became involved in searching for Resident #11 all around the facility and police were called to assist in the search. FM A stated Resident #11 was found approximately two (2) hours after she initially arrived at the facility. FM A stated Resident #11 was brought back to the facility and then transferred to the emergency room for further evaluation. FM A stated Resident #11 mentioned she was upset about the room change the previous night, not being able to sleep and walking out the front door because she wanted to leave. FM A stated after she came back to the facility from the hospital, staff informed her Resident #11 would be transferred to a different nursing facility for safety.
In an interview on 10/26/23 at 11:15 am, with CNA L stated exit doors were secured with codes and alarms. CNA L stated residents and visitors did not have codes to the exit doors. CNA L stated the facility did have a designated smoking area where residents are able to go outside supervised. CNA L stated she last saw Resident #11 in her room after breakfast. CNA L stated Resident #11 went to restroom in her room and after briefly sitting on her bed she laid down. CNA L stated Resident #11 had mentioned to her that she had not slept the night before. CNA L stated Resident #11 was last seen at approximately 09:30 a.m. that morning wearing a pink sweater, brown blouse, and beige pants CNA L stated she did not see Resident #11 anymore and did not know her whereabouts until family came to ask for her at approximately 09:45 a.m. CNA L stated all staff went to look in every room, outside, rehab, activities room, parking area, and in the surrounding areas. Staff L stated she did not know what time, the location, who found Resident #11 and how she was brought back to the facility.
In an interview on 10/26/23 at 11:25 a.m., CNA J stated exit doors were secured with alarms that could be turned off by punching in a code. CNA J stated residents were allowed to go outside of the facility supervised to designated areas such as the smoking area. CNA J stated she was assigned to work shower duties the day Resident #11 was missing. CNA J stated Resident #11 had not showered and that Resident #11 had just been transferred from hall 200 to room [ROOM NUMBER]-A in hall 300. CNA J stated she was on break when FM A arrived at facility and search for Resident #11 was initiated. CN J stated residents were accounted for when doing walking rounds in the morning, as they are passing breakfast trays, when they round every two (2) hours. CNA J stated she does not know where Resident #11 was found or when. Staff J stated Resident #11 was brought back to the facility by police, she was taken to the hospital and when she came back she was put on 1:1 observation.
In an interview on 10/26/23 at 11:35 a.m. with LVN K stated he worked on hall 300 for approximately twelve (12) years as a floor nurse. LVN K stated he was not working the day of the incident; however, exit doors are secured by a code and an alarm with a 15 second delayed egress and a stop alarm (screech annunciator). LVN K stated that residents must ask staff for assistance to go outside in the assigned patio area.
In an interview on 10/26/23 at 12:10 p.m. with LVN E stated she had worked at facility for approximately three (3) yeaars as a floor nurse. LVN E stated exit doors are secured with a code and an alarm with a 10 second delay and stop alarm. LVN E stated residents were not allowed to go outside unsupervised unless with staff or family member and depending on the resident's independent need. LVN E stated her shift on 09/19/23 started at 02:30 a.m. to assist a co-worker and was assigned to hall 300 including, Resident #11. LVN E stated Resident #11 was moved from 200 to hall 300 the day before. LVN E stated Resident #11 was not completely comfortable in her room and that Resident #11 spend her time at the nurse's station. LVN E stated Resident #11 was a smoker and had wanted to go outside. Staff E stated Resident #11 needed to wait for someone to assist her. LVN E stated her shift changed at 06:00 a.m. and her assignment changed to a different hall including the resident she was taking care of. LVN E stated she observed Resident #11 sitting at the nurse's station at approximately 08:40 a.m. LVN E stated Resident E went to her room to change her shirt because it was stained and returned to the bistro area around 08:50 a.m. wearing a blue shirt. LVN E stated family came to visit Resident #11 close to 10:00 a.m. LVN E stated she was approached by her supervisor and was asked the whereabouts of Resident #11. LVN E stated she assisted in searching for Resident #11 in the activities area, bistro, and smoking area. LVN E stated she knew Resident #11 was missing when Resident #11 could not be located in those areas. LVN E stated after code elopement was announced, she and other staff were assigned to look in all halls, restrooms, closets, locked and unlocked doors, in halls, outside parking lots, staff searched in each direction of the facility, drove in the surrounding areas of the facility. LVN E stated family and staff called Resident #11's cell phone multiple times and went unanswered or went to voicemail. LVN E stated Resident was found at approximately 11:30 a.m. on [NAME] Rd. in Edinburg and brought back to the facility by police. LVN E stated she performed a head-to-toe assessment immediately. LVN E mentioned no injuries were noted. LVN E stated Resident #11 was sent to hospital for further evaluation and treatment, an incident report was made, and in-service of staff was performed.
In an interview on 10/26/23 at 04:45 p.m., LVN D mentioned she has been employed at the facility for seventeen (17) years. LVN D stated she makes sure all residents are accounted for in the facility by performing a walking round on the hall she is assigned and count the residents to assure they are in the facility. LVN D stated staff should round on residents every two (2) hours or more often if needed. LVN D stated exit doors have a code. LVN D also mentioned residents should not know the code, and that if administration finds out residents know the codes, administration will change the codes frequently. She stated the exit codes were changed within the last week.
In an interview on 10/27/23 at 08:45 a.m., BOM U stated she had been employed at facility for approximately twenty-four (24) years. BOM U stated she was assigned to the reception area and her responsibilities included allowing entry and exit to visitors, staff and/or residents to the facility. BOM U stated visitors no longer have to sign in or out. BOM U stated visitors nor residents have entrance or exit codes. BOM U stated some residents were able to obtain codes because they watched staff punch the codes on the access keypad of the exit doors as they exited or entered the facility. BOM U stated exit doors have a code that must be punched in a keypad in order for the door to unlock and allow the person to enter or exit. BOM U stated emergency exit doors have a push bar that is equipped with a 15 second delayed egress and a stop alarm (screech annunciator). BOM U stated she accounts for residents by obtaining a printed report from admissions department. She stated she looked at the schedule to make sure all residents are in the facility and checks with the nurses if they are not. BOM U stated if she found a missing resident she would inform admissions and checked to see if the resident was at the facility. BOM U stated she has access to the computer where she could see resident pictures to identify the residents. BOM U stated the facility discouraged staff from sharing codes with other employees, staff, and visitors.
In an interview on 10/27/23 at 11:05 a.m., Resident #12 stated staff treated him well. Resident #12 stated he was happy with the services he was receiving at facility. Resident #12 denied pain or discomfort. Resident #12 stated staff brought him his medication on time. Resident #12 stated the doors have alarms and he cannot go out the exit doors. Resident #12 stated he needed to ask staff for assistance to go outside.
In an interview on 10/27/23 at 11:15 a.m.Resident #13 stated staff treated her well. Resident #13 stated she was happy with the services provided by the facility. Resident #13 stated she was comfortable and denied pain. Resident #13 stated staff brought her medication on time. Resident #13 stated she knows how to make complaints and to who in the facility to make them to. Resident #13 stated she is mostly in bed and does not usually go outside.
In an interview on 10/27/23 at 11:30 a.m., Resident #14 stated he was happy with the services he was receiving at the facility. Resident #14 stated he did not feel threatened and had not been hurt by staff. Resident #14 denied pain and stated he was comfortable. Resident #14 stated he went outside with the assistance of staff and did not know the codes to the doors.
In a telephone interview on 10/27/23 at 02:00 p.m., ADON C stated he had been employed with the facility for approximately 2 years. Staff C stated he accounted for residents by rounding in the morning. ADON C stated if a resident was out on pass, on an appointment or not in his/her room he would communicate with other staff to find out the whereabouts of the resident. ADON C stated medical records took a picture of the resident and uploaded it into the resident profile. ADON C stated everyone who had access to resident records had access to view the resident profile and was able to identify residents. ADON C stated the front door was always locked and staff did not allow residents to go through the front door unsupervised. ADON C stated only employees know the codes in order to deactivate the alarms to the doors. ADON C stated doors are secured by a magnet punch code to be unlocked and codes are not shared with visitors and residents. ADON C stated only management had access to door codes. ADON C mentioned employees, nurses and charge nurses do not have access to door codes. ADON C stated staff would notify management when door is opened without an alarm going off. ADON C stated there is one code for all staff members. ADON C stated if a resident is missing he would notify the charge nurse immediately and ask other staff including CNA and LVN about the whereabouts of the resident. ADON C stated that the process is usually immediately, but following the identification of a missing resident, the charge nurse and management team including the DON and the administrator would be notified. ADON C stated an onsite search would be conducted for the resident. ADON C stated an emergency code purple to all staff would be announced to indicate a missing resident. ADON C stated staff would search every door, closet, room, parking area would be searched, and the police would be called. ADON C stated this process usually is less than ten (10) minutes because all staff is assigned to a hall and the facility would know immediately whether the resident was within the facility. ADON C stated facility would then designate a staff member as the point of contact who would communicate to others of all updates. ADON C stated that meanwhile, the remaining facility staff would continue with the search on the outside of the facility. ADON C stated after code purple was initiated, the police department was called immediately, the family of the resident would be updated, and the physician would be notified within one (1) hour. ADON C stated that once the resident was found, code purple would be called off, a head-to-toe assessment would be performed, the physician and family would be updated. ADON C mentioned code purple or elopement incidents are self-reported incidents. He stated the facility would perform an in-service for the staff on elopement and the exit door codes would be changed. ADON C stated that facility staff performed an elopement risk assessment on admission to assess residents for risk of eloping. He stated that those residents who were high risk of elopement are moved closer to the nurse's station and the staff would maintain a closer observation to those residents. ADON C stated the facility was not a lockdown facility meaning the facility did not have a secure memory care unit. ADON C stated staff increased rounding on residents with high-risk elopement risk. He stated he had not observed cameras on the inside of the facility premises and only had observed a few on the outside. ADON C stated facility offers in-services weekly on different topics including abuse, neglect, and exploitation.
In an interview on 10/27/23 at 02:00 p.m., DON stated she had worked at the facility for four (4 years) and was responsible for in-servicing staff, oversight of floor staff and reporting to the administrator. DON stated certified nurse assistants (CNAs) round every two (2) to three (3) hours and as needed. She stated nurse's round at the beginning of their shift, during medication pass and at the end of their shift. DON stated that information is passed on report when a resident is out on pass and that a resident must be signed out if they do go on pass. DON stated if a resident is missing staff must go room to room, in the activity's areas, or in rehab to ensure residents are not in the facility. DON stated the resident roster is compared to each hallway to make sure all residents are accounted for. Staff A stated that if a resident is identified as missing, a code is announced to alert all staff of the missing resident. DON continued by stating that staff then are assigned to search in all areas of the facility. DON stated if the resident is not located within the facility, staff are assigned to go out of the premises in teams to search for the resident within a 3-mile radius in all directions. DON stated the police department, family and physician is then notified of the resident's elopement. DON stated that no more than 10 minutes of identifying a missing resident is a code for elopement activated and police are notified. DON stated facility exit doors are secured by alarms that must be deactivated with a code that was entered on a punch keypad. DON stated those codes are not shared with residents or visitors. DON stated the facility has identified residents who figure the codes out by observing staff members while entering the code on the keypad. DON stated that the facility prevents residents from accessing the codes by frequently changing the codes, changing them once the code has been breached or as often as needed. DON stated the facility prevents residents from entering/leaving the facility by assigning two receptionists between the hours of 08:00 a.m. and 08:00 p.m. DON stated after these hours, visitors must ring the doorbell, so the door is opened by a staff member at the nurse's station. DON stated the receptionists have access to the resident pictures that are on the resident profile and receptionists can identify residents who attempt to exit the front door unsupervised. DON stated Resident #11's family members arrived to visit with Resident on 09/19/23 and at approximately 10:30 a.m. approached LVN E to assist in locating resident within the facility. Staff A stated family and LVN E were not able to locate Resident #11 after searching on the premises themselves and delayed informing other staff of the resident's status because Resident #11 had not ever voiced desires to go home and had never had exit seeking behaviors. DON stated FM A and Staff E notified other staff members of the management at approximately 10:45. DON stated the facility activated the code for elopement at approximately 11:00 a.m. when police were notified. DON stated Resident #11 was located by local police department at 11:30 a.m., approximately two (2) miles from the facility. DON stated Resident #11 walked to a nearby hospital where she asked a woman (unknown name) for a ride to a local restaurant. DON stated Resident #11 stayed to have a drink at the restaurant and then walked home. DON stated Resident #11 knows the address to her apartment. DON stated Resident #11 was found walking with herself using her walker on [NAME] Road in the direction of her apartment. DON stated local police department brought Resident #11 back to the facility. DON stated staff performed a head-to-toe assessment, food and water was offered, and the physician was notified. DON stated Resident #11 was interviewed, and it was revealed she left through the front exit. DON stated she was unaware if Resident #11 piggybacked (walked out) with a group of other visitors or if Resident #11 held the door for 15 seconds so the alarm would not sound. DON stated that the facility was in-servicing staff and performing routine mock drills in order to better prepare staff and prevent a future elopement. DON stated the facility was also changing exit door codes frequently and incoming residents were screened to make sure their needs could be properly addressed. DON stated incoming residents with high score risk elopement risks would be placed on 1:1 until the facility was able to transfer them to a facility that could accommodate their needs.
In an interview on 10/30/23 at 09:55 a.m., Resident #15 in room stated she was happy with the services received at the facility. Resident #15 stated she does not feel threatened and was not hurt by facility staff. Resident #15 stated she did not always like the food; however, she knew how to file a complaint to the Administrator regarding her concerns. Resident #15 stated staff brought her medication on time. Resident #15 stated she did not know the codes to the exit doors, staff did want to share the codes with her, and that the doors had alarms. Resident #15 stated staff assist her if needing to go outside.
In an interview on 10/30/23 at 10:05 am, Administrator stated she had been employed by the facility for two (2) years and was responsible for the administrative duties of the facility. Stated she was also responsible for performing in-services on staff as well as DON and ADON C. Administrator stated topics of in-services provided to staff resident supervision, Stated best practice is for CNAs and nurses to round the assigned hallways when they start their shift, every two (2) hours and as needed. Nurses round when they start their shift, every two (2) hours and as needed on their assigned hallways. Administrator stated residents are accounted for in the facility by staff communicating during report and walking rounds. Stated exit doors are secured by maglocks (magnetic lock which is a locking mechanism that uses an electromagnetic field controlled by an electrical system that can be configured with a switch, keycard reader or biometric scanner) and a code that releases the maglock. Administrator stated the exit doors are also secured with a fifteen (15) second delayed egress and a stop alarm (screech annunciator). Stated exit door codes are changed monthly or as needed and are not shared with visitors or residents. Administrator stated the facility prevented visitors and residents from accessing the codes by offering in-services to staff on not sharing codes. Stated residents have accessed the codes before by watching staff members input the code as they are entering or exiting the facility. Administrator stated facility changed exit door codes as soon as facility identified a code had been breached and resident or visitor had learned or accessed a code. Stated facility had no working cameras at the exit doors. Administrator stated on 09/19/23 Resident #11's family member came to visit her. Stated floor staff notified her that Resident #11 was missing. Administrator stated the facility initiated their code purple (elopement protocol) immediately and followed their procedures. Adiminstrator stated they assigned a point of contact and assigned teams to search within the facility and outside of the facility. Stated that staff searched a radius of 1 mile in each direction of the facility. Staff B stated the police and physician were notified. Stated Resident #11 had been previously assessed and was not an exit seeker and never verbalized or gave any indication of wanting to leave. Administrator stated Resident #11 was found by local police department and returned to the facility unharmed. Stated a head-to-toe, pain, and skin assessment was performed upon Resident #11's return. Administrator stated family was at the facility, but physician was informed. Stated upon Resident #11's return, staff were in-serviced on elopement, a head count was performed on all residents, a secured clear box was placed over alarm over front door to prevent people from unplugging the maglock and deactivating it. Administrator stated facility prevented a reoccurrence of this incident by performing mock drills, changing exit door codes frequently, maintaining communication with staff regarding whereabouts of residents, and in-servicing staff on elopement.
Interview on 11/01/2023 at 2:00 p.m., The Administrator said they change the code monthly or as needed. She said if they find out the codes have been compromised, they will change it immediately.
Record review of maintenance logbook documentation stating Year 2023 Codes doors marked each exit tested for months April through October.
Record review of facility in-service training report revealed facility had a training with staff including nursing staff, social worker, administrative/office, food service and maintenance personnel over Elopement and Wandering Residents on 09/19/23.
Record review of facility in-service training report revealed facility had a training with staff including nursing staff, social worker, administrative/office, food service and maintenance personnel over Abuse and Neglect/Resident Supervision, Answer Call lights in a timely manner on 09/19/23 with the following evaluations, comments, suggestions: Elopement process: follow proper protocol for elopement events: Meet nurses' station, search all areas of facility, search all areas outside, search does not end until patient is found, ensure codes are changed, monitor as needed for safety of residents.
Record review of facility in-service training report revealed facility had an elopement mock drill with staff including nursing staff, social worker, administrative/office, food service and maintenance personnel on 09/22/23 with the following contents or summary of training session: follow proper elopement protocols, exit door codes changed monthly or as needed, supervise residents that exhibit exit seeking behaviors, monitor for exit seeking behaviors/contact family if behaviors are exhibited.
Record review of facility in-service training report revealed facility had an elopement mock drill with staff including nursing staff, social worker, administrative/office, food service and maintenance personnel on 09/25/23 with the following contents or summary of training session: follow proper elopement protocol, codes for exit doors will be changed monthly [TRUNCATED]
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on Observations and interviews, the facility failed to provide a safe, sanitary, and comfortable environment for 1 of 1 (R...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on Observations and interviews, the facility failed to provide a safe, sanitary, and comfortable environment for 1 of 1 (Resident #30 reviewed for the environment in that:
The facility did not secure a bottle of liquid disinfectant; R #30 was found with liquid disinfectant in his possession and near his mouth.
This failure could place residents at risk of living in an unsafe, unsanitary, and uncomfortable environment
The findings included:
Record review of R #30 's file reflected [AGE] year-old male with original admission date of 01/17/19 and last admission date of 03/28/23. His diagnosis included: Displaced fracture of fifth cervical vertebra, muscle wasting and atrophy, unsteadiness of feet, lack of coordination, Major depressive disorder, Parkinson's Disease, Dysphagia, and acute pain due to trauma.
Record review of R #30's MDS assessment dated [DATE] reflected BIMS was not conducted as R #30 was rarely/never understood. Functional status indicated R #30's ADL of eating (how resident eats and drinks) required extensive assistance for ADL self-performance and limited assistance for ADL support. R #30 uses a wheelchair. Functional Abilities and Goals indicated substantial/maximal assistance (helper does more than half the effort, helper lifts or holds trunk or limbs and provides more than half the effort) for picking up an object (the ability to bend/stoop from a standing position to pick up a small object, such as a spoon, from the floor).
Record review of R #30's Care Plan dated 07/27/23 reflected on 06/19/23 R #30 had a possible ingestion of liquid disinfectant. R #30 will be free of complications from possible ingestion of liquid disinfectant through review period. Date initiated: 06/20/23. Interventions: contacted poison control center on 06/19/23, informed staff to keep hazardous chemicals away from resident's reach, MD and RP notified, and provided oral care.
Record review of the incident report dated 06/19/23 at 11:59 AM reflected incident location: therapy room. Incident description: LVN S was called to the therapy area because R #30 may have consumed liquid disinfectant. Therapy staff said that R #30 had the spray bottle nozzle at his mouth but was not sure if he consumed any. Upon entering the therapy area, R #30 was found sitting in his wheelchair awake, alert, and oriented as usual and calm. LVN S immediately smelled his breath and did not notice any unusual smell. LVN S smelled the liquid disinfectant and R #30's breath had no comparison. R #30 denied consuming any liquid disinfectant. R #30's mouth was rinsed, and oral care was given. R #30 denied any mouth, throat, or esophageal burning sensation. R #30 and staff denied any dry heaves, vomiting, or spitting out liquid disinfectant. RP and NP were notified. Orders received from NP: oral care and call poison control center. R #30 was not taken to the hospital. No injuries observed at time of incident or post incident. Pre-disposing environmental factors: none. Pre-disposing physiological factors: confused, incontinent, gait imbalance, impaired memory, and weakness. Other info: liquid disinfectant within R #30's reach. Notified RP on 06/19/23 at 11:35 AM. Notified MD on 06/19/23 at 11:40 AM.
Record review of progress notes for R #30 reflected -
On 06/19/23 at 11:40 AM documented by, LVN S. LVN S was called to the therapy area because R #30 may have consumed liquid disinfectant. Therapy staff said that R #30 had the spray bottle nozzle at his mouth but was not sure if he consumed any. Upon entering the therapy area, R #30 was found sitting in his wheelchair awake, alert, and oriented as usual and calm. LVN S immediately smelled his breath and did not notice any unusual smell. LVN S smelled the liquid disinfectant and R #30's breath had no comparison. R #30 denied consuming any liquid disinfectant. R #30's mouth was rinsed, and oral care was given. R #30 denied any mouth, throat, or esophageal burning sensation. R #30 and staff denied any dry heaves, vomiting, or spitting out liquid disinfectant. RP and NP were notified. Orders received from NP: oral care and call poison control center.
On 06/19/23 at 11:45 AM, documented by, LVN S. LVN S called poison control center and explained the situation of liquid disinfectant and the immediate treatment that was rendered. As per poison control center, liquid disinfectant is non-corrosive once it is diluted. R #30 was asymptomatic of burning sensation of throat, esophagus, and mouth. There did not appear to be significant problems or reaction to product. Orders given- monitor for changes, mental changes, burning of mouth, and esophagus for 24 hours. If vomiting occurs, send to ER. Give 8 ounces of water every hour for 4 hours.
On 06/19/23 at 12:55 PM, documented by, LVN S. R #30 was awake, alert, and oriented as usual and calm. Ate 100% of lunch. R #30 denied any burning of throat, esophagus, or mouth. No nausea or vomiting. No diarrhea or upset stomach. Normal behavior.
On 06/19/23-06/23/23 progress notes reflected R #30 continued to be monitored. No signs or symptoms noted. R #30 ate without issue, and no abnormalities noted.
Observation on 10/30/23 at 11:40 AM noted the liquid and wipe disinfectants in the therapy department in a cabinet by the sink against the wall on the right side of the room. The cabinet did not have a lock but was closed shut.
In an interview with LVN S on 10/30/23 at 11:50 AM. LVN S said she worked on 06/19/23 with R #30. LVN S said she vaguely remembered the incident. LVN S said she was called to the therapy department because R #30 had possibly ingested a liquid disinfectant. LVN S said she did not recall who notified her, but it was a therapy staff. LVN S said she went to the therapy department where R #30 was located. LVN S said she assessed R #30 and immediately smelled R #30's breath. LVN S said she smelled the disinfectant and R #30's breath and mouth did not smell like the disinfectant. LVN S said she called notified the doctor. LVN S said the doctor instructed LVN S to call poison control and to do oral care for R #30. LVN S said she called poison control and called the manufacturer for the disinfectant. LVN S said poison control instructed LVN S to monitor R #30 for any signs or symptoms of ingestion. LVN S said poison control said if R #30 demonstrated any nausea, vomiting or any symptoms, then to transport him to the hospital. LVN S said R #30 was not sent out to the hospital. LVN S said the manufacturer instructed LVN S to monitor R #30 and to make sure R #30 was eating good. LVN S said she also checked R #30's mouth and R #30 did not have any redness or irritation. LVN S said she checked R #30's vitals and vital signs were normal. LVN S said she continued to monitor R #30. LVN S said R #30 ate well, had no signs of pain, and did not exhibit other symptoms such as redness to his throat or eyes. LVN S said that was the first time something like this had happened during the time she had worked. LVN S said R #30 was not known to get things like the disinfectant or attempt to grab things. LVN S said R #30 could not speak but he was able to communicate his basic needs. LVN S said the therapy staff informed LVN S that R #30 had the bottle in his hand. LVN S said she did not recall if the therapy staff said R #30 had sprayed the bottle or not, but LVN S said she did not believe R #30 sprayed it. LVN S said she remember the label on the disinfectant bottle said something like to call the company which LVN S did. LVN S said the manufacturer said if R #30 had ingested the disinfectant it would not hurt him because the liquid was diluted, but the manufacturer did instruct LVN S to monitor for symptoms such as burning of the throat, mouth, and esophagus. LVN S said the disinfectants were usually kept under lock and key, at least in the halls and rooms. LVN S said R #30 was in the therapy department. LVN S said was not sure how the disinfectant was kept safe in that department. LVN S said the doctor gave the orders to monitor for signs and symptoms such as vomiting, nausea, or burning sensation, call poison control, and provide oral care, which LVN S did. LVN S said R #30 did not show any signs or symptoms of ingesting the disinfectant, R #30 was interacting, in good spirits, eating well, and there were no reports of symptoms. LVN S said she followed what poison control, and the manufacturer instructed her to do. LVN S said she also notified the DON, the doctor, and RP. LVN S said she followed the protocol for the incident once she was notified.
In an interview with DOR on 10/30/23 at 11:55 AM. DOR said she worked on 06/19/23 with R #30 and recalled the incident. DOR said the therapists follow the infection control protocol after each resident. DOR said they wipe down the equipment or area used and spray it with disinfectant. DOR said she remembered working with R #30 to see if he could drink from a straw. DOR said she was going to check if R #30 could use a straw easier if it was shorter, so she went to her office to get scissors to cut the straw. DOR said her office was a few feet away from the table where R #30 was sitting. DOR said there were two tables in the main area of the therapy department and the tables were side by side. DOR said R #30 was sitting on one table and the bottle of disinfectant was on the other table. DOR said she was not sure how R #30 was able to reach the disinfectant. DOR said she went to her office for a second, then went back to R #30, and R #30 had the bottle in his hand and close to his mouth. DOR said she could not recall if the nozzle was facing R #30 or if the nozzle was open or closed. DOR said she could not recall if there was any residual liquid on the nozzle. DOR said she was not sure what happened or if R #30 had ingested any of the liquid, so DOR called the nurse right away to have the nurse check R #30. DOR said she did not know if R #30 ingested the liquid or not, but DOR did not want to run the risk of not getting R #30 checked in case. DOR said she did not recall which nurse responded, but the nurse went to the therapy department. DOR said the nurse assessed R #30 and notified the doctor. DOR said the doctor's orders were to monitor R #30 to see if there were signs or symptoms of R #30 ingesting the disinfectant such as redness, burning of the mouth, or vomiting. DOR said DOR and the nurse had R #30 try to squeeze the disinfectant spray bottle to see if R #30 had the strength to squeeze it but could not get R #30 to do it. DOR said R #30 did have Parkinson's and did not have the ability to follow through with command. DOR said the nurse checked R #30's mouth. DOR said the disinfectant had a strong scent, and the nurse indicated R #30's mouth did not smell like the disinfectant. DOR said DOR had not used the disinfectant yet. DOR said she assumed one of the other therapists had used it or left it on the table and forgot to put it away. DOR said the bottle was not even close to R #30, but it was on a table nearby him. DOR said she did not know if R #30 reached for the bottle and how R #30 was able to get the bottle. DOR said R #30 did have the ability to pick up the bottle. DOR said the bottle was not full, so it was not very heavy, but depending on the day sometimes R #30 was able to do more than other days. DOR said on this day, R #30 was able to pick up the bottle as DOR witnessed R #30 holding the bottle in his hand. DOR said an incident like this had never happened before. DOR said she did not know what to do, so DOR's immediate reaction was to notify the nurse. DOR said the therapy department was in-serviced to always put the disinfectants back in their place. DOR said she did not recall the exact time, but this happened early in the morning on 06/19/23. DOR said she did not remember who was working or if anyone saw R #30 get the bottle. DOR said R #30 was only receiving speech therapy. DOR said she had not encountered this behavior with R #30 where he would grab things. DOR said when it comes to eating, R #30 could grab onto the cup and the spoon. DOR said R #30 knew what food was or what he could eat. DOR said this caught her off guard. DOR said the nurse did not note any injury to R #30 from what the nurse told her. DOR said the nurse was going to continue monitoring R #30. DOR said the disinfectant used to be kept under lock and key in DOR's office, but the key was lost. DOR said the disinfectant was kept in a cabinet under the sink where the therapists could get it. DOR said the disinfectants were kept safely in that cabinet, away from the residents' reach. DOR said that day, someone left the bottle on the table, but they should have put it back in the cabinet after using it.
In an interview with DON on 10/30/23 at 1:00 PM. DON said she was aware that there was an incident on 06/19/23 where R #30 possibly ingested a liquid disinfectant. DON said the incident happened in the therapy department. DON said the therapist notified the nurse, and the nurse assessed R #30 and notified the doctor and RP. DON said the nurse, LVN S, called poison control. DON said DOR immediately removed R #30 from that area and removed any chemical from within the residents' reach. DON said LVN S spoke to poison control who instructed LVN S to monitor for sore throat, nausea, vomiting, and diarrhea. DON said R #30 did not exhibit any symptoms. DON said LVN S smelled R #30's breath and smelled the disinfectant to see if it smelled the same and it did not. DON said DOR stated someone had just finished disinfecting the area. DON said DOR stated the bottle was close to where R #30 was. DON said DOR quickly went to her office, and when DOR returned to the area, DOR saw R #30 had the bottle's nozzle close to R #30's mouth. DON said DOR was not sure if R #30 sprayed the bottle or if R #30 was about to spray it and DOR caught it on time. DON said DOR notified LVN S either way, and LVN S assessed R #30. DON said LVN S assessed R #30's oral mucosa (mouth) and noted no signs of ingestion. DON said R #30 denied any pain. DON said R #30 did not show symptoms such as vomiting or trying to spit out any kind of liquid or substance. DON said LVN S rinsed R #30's mouth and provided oral care in case R #30 did spray the disinfectant. DON said if the therapy department staff had just used the disinfectant, the staff should have put it away. DON said she was unsure of who left the bottle on the table, but it was the staff's responsibility to ensure it was not within reach. DON said the disinfectant should not have been within reach and the disinfectant should have been under lock and key or at least in a safe location. DON said in the housekeeping carts, the disinfectants were locked. DON said she was unsure if there was a policy regarding how to store disinfectants or if the policy indicated the disinfectants had to be under lock and key. DON said for safety purposes, the disinfectants and other chemicals should be kept away from residents in a safe place. DON said residents should not be able to get their hands on those liquids. DON said there was an incident report for this. DON said the incident report indicated therapy staff but did not specify who exactly left the bottle on the table. DON said therapy staff did do an in-service on not leaving behind any products within the residents' reach. DON said when LVN S assessed R #30 there were on abnormalities. DON said R #30 was able to eat without complications. DON said R #30 was able to swallow water. DON said the doctor said if the facility identified any abnormalities to call the doctor back, but there were no changes. DON said R #30's mouth was not bleeding, red, and did not exhibit any changes. DON said there was no need to send R #30 to the hospital. DON said there was no nausea or vomiting. DON said R #30 was not known to have behaviors of ingesting such liquids or other inedible items. DON said R #30 was not known to grab things randomly. DON said R #30 was not on any special supervision. DON said R #30 tried to speak but stuttered because of his Parkinson's, so he would get frustrated and stop speaking. DON said it was hard to know exactly how much R #30 understood. DON said R #30 could nod his head yes or no, but it was more to communicate his basic needs. DON said R #30 would likely not be able recall if asked about this incident. DON said an incident like this had not happened before as far as a resident possibly ingesting chemicals or cleaners. DON said the staff responded appropriately as far as getting the nurse to assess, obtaining, and carrying out doctor's orders, calling poison control, and monitoring R #30. DON said staff failed to remove the bottle from within R #30's reach. DON said the only time the disinfectants or chemicals should have not been in a safe location, was if they were being used. DON said R #30 was not injured from this incident. DON said R #30 could have possibly been injured. DON said R #30 could have had vomiting, irritation to the throat, developed sores in his mouth, and could have suffered other possible side effects that the poison control representative told them to monitor for such as a burning sensation to the mouth, throat, and esophagus. DON said the incident could have also resulted in a serious injury to R #30. DON said nobody witnessed R #30 actually spray the bottle or ingest the disinfectant, but the possibility still existed.
In an interview with Administrator on 10/30/23 at 2:10 PM. Administrator said on 06/19/23 R #30 grabbed a spray bottle for a liquid disinfectant and had it close to R #30's mouth. Administrator said DOR caught it right away, but because it was close to R #30's mouth, DOR notified the nurse and followed the protocol. Administrator said Administrator thought she did submit a self-report for that incident. Administrator said if R #30 had in fact ingested the liquid disinfectant, then it would have been a reportable incident because it was a substance that could be harmful. Administrator said the facility was not sure if R #30 ingested the disinfectant, but the facility staffed the incident with corporate/upper management team. Administrator said LVN S had called poison control, called the doctor, and called the family. Administrator said LVN S followed what poison control said to do and followed the doctor's orders. Administrator said R #30 was not injured and continued to not have any negative side effects. Administrator said Administrator did not recall who left the bottle on the table or how R #30 was able to obtain the bottle. Administrator said there was an incident report completed for that as it was considered an incident. Administrator said the therapy department was not supposed to have anything within reach of the residents. Administrator said the disinfectants and chemicals should be at least in a cabinet, preferably under lock and key. Administrator said she was unsure if there was a policy regarding where to store such disinfectants. Administrator said an unknown therapy staff left the bottle of disinfectant on the table. Administrator said the staff did not have it behind a closed door or cabinet. Administrator said the disinfectant should have been placed inside a closed unit or at least behind a cabinet. Administrator said the disinfectant bottle should not have been on the table. Administrator said the facility did not know who left it out. Administrator said the incident report did not have any interviews with staff to figure out who left the bottle out or how R #30 was able to obtain the bottle. Administrator said the progress notes noted the staff called poison control and followed the doctor's orders, and how the staff monitored R #30 for any changes. Administrator said Administrator could not recall if any staff were in-serviced for this incident. Administrator said R #30 did not exhibit any signs or symptoms that R #30 did ingest the disinfectant. Administrator said R #30 could have been harmed if he did ingest the disinfectant.
In an interview with Administrator on 10/30/23 at 3:45 PM. Administrator said the incident was not a reportable because there were no negative outcomes to R #30. Administrator said the facility continued to monitor R #30 for days and there were no injuries. Administrator said the incident report and progress notes noted the investigation and actions taken by the facility upon discovering the incident.
Record review of the in-service record dated 06/20/23 for Topic: properly securing cleaning agents. Summary of training session: will supervise residents during therapy sessions, will keep cleaning agents out of residents' reach, when not in use (cleaning agents) will be properly stored, and in the event of exposure, staff will appropriately notify (nursing staff, RP, MD, etc.) DOR completed the in-service. Sign-in sheet indicated five therapy staff were in-serviced.
Record Review of the facility's General Housekeeping Policies (undated) reflected:
All bleaches, detergents, disinfectants, insecticides and other potentially hazardous substances are labeled and kept in a safe place accessible only to employees
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement written policies and procedures to prohibit and prevent a...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement written policies and procedures to prohibit and prevent abuse and neglect for 1 of 1 resident (R #30) reviewed for incident reporting.
The facility failed implement their policy and did not report an allegation of neglect for R #30 for an incident on 06/19/23.
This failure could place residents at risk of abuse, neglect, and not having incidents reported appropriately.
The findings included:
Record review of the Abuse, Neglect, and Exploitation Policy (implemented 08/15/22)
Reporting/Response:
The facility will have written procedures that include:
1.
Reporting of all alleged violation to the Administrator, state agency, adult protective services and to all other required agencies (e.g. law enforcement when applicable) within specified timeframes:
a.
Immediately, but no later than 2 hours after the allegation is made, if the events that cause the allegation involve abuse or result in serious bodily injury, or
b.
Not later than 24 hours if the events that cause the allegation do not involve abuse and do not result in serious bodily injury.
Record review of R #30 's file reflected [AGE] year-old male with original admission date of 01/17/19 and last admission date of 03/28/23. His diagnosis included: Displaced fracture of fifth cervical vertebra, muscle wasting and atrophy, unsteadiness of feet, lack of coordination, Major depressive disorder, Parkinson's Disease, Dysphagia, and acute pain due to trauma.
Record review of R #30's MDS assessment dated [DATE] reflected BIMS was not conducted as R #30 was rarely/never understood. Functional status indicated R #30's ADL of eating (how resident eats and drinks) required extensive assistance for ADL self-performance and limited assistance for ADL support. R #30 uses a wheelchair. Functional Abilities and Goals indicated substantial/maximal assistance (helper does more than half the effort, helper lifts or holds trunk or limbs and provides more than half the effort) for picking up an object (the ability to bend/stoop from a standing position to pick up a small object, such as a spoon, from the floor).
Record review of R #30's Care Plan dated 07/27/23 reflected on 06/19/23 R #30 had a possible ingestion of liquid disinfectant. R #30 will be free of complications from possible ingestion of liquid disinfectant through review period. Date initiated: 06/20/23. Interventions: contacted poison control center on 06/19/23, informed staff to keep hazardous chemicals away from resident's reach, MD and RP notified, and provided oral care.
In an interview with LVN S on 10/30/23 at 11:50 AM. LVN S said she worked on 06/19/23 with R #30. LVN S said she was called to the therapy department because R #30 had possibly ingested a liquid disinfectant. LVN S said she went to the therapy department where R #30 was located. LVN S said she assessed R #30 and did not note any abnormalities. LVN S said the doctor gave the orders to monitor for signs and symptoms, such as vomiting, nausea, or burning sensation, call poison control, and provide oral care, which LVN S did. LVN S said R #30 did not show any signs or symptoms of ingesting the disinfectant, R #30 was interacting, in good spirits, eating well, and there were no reports of symptoms. LVN S said she followed what poison control, and the manufacturer instructed her to do.
In an interview with DOR on 10/30/23 at 11:55 AM. DOR said she worked on 06/19/23 with R #30 and recalled the incident. DOR said she went to her office for a second, then went back to R #30, and R #30 had the bottle in his hand and close to his mouth. DOR said she could not recall if the nozzle was facing R #30 or if the nozzle was open or closed. DOR said she could not recall if there was any residual liquid on the nozzle. DOR said she was not sure what happened or if R #30 had ingested any of the liquid, so DOR called the nurse right away to have the nurse check R #30. DOR said the nurse assessed R #30 and notified the doctor. DOR said the doctor's orders were to monitor R #30 to see if there were signs or symptoms of R #30 ingesting the disinfectant such as redness, burning of the mouth, or vomiting. DOR said she assumed one of the other therapists had used the disinfectant or left it on the table and forgot to put it away. DOR said the bottle was not even close to R #30, but it was on a table nearby him. DOR said she did not know if R #30 reached for the bottle and how R #30 was able to get the bottle. DOR said R #30 did have the ability to pick up the bottle. DOR said the bottle was not full, so it was not very heavy. DOR said she did not recall the exact time, but this happened early in the morning on 06/19/23. DOR said she did not remember who was working or if anyone saw R #30 get the bottle. DOR said the disinfectants were kept safely in a cabinet, away from the residents' reach. DOR said that day, someone left the bottle on the table, but they should have put it back in the cabinet after using it.
In an interview with DON on 10/30/23 at 1:00 PM. DON said she was aware that there was an incident on 06/19/23 where R #30 possibly ingested a liquid disinfectant. DON said the staff responded appropriately as far as getting the nurse to assess, obtaining, and carrying out doctor's orders, calling poison control, and monitoring R #30. DON said staff failed to remove the bottle from within R #30's reach. DON said the only time the disinfectants or chemicals should have not been in a safe location, was if they were being used. DON said R #30 was not injured from this incident. DON said R #30 could have possibly been injured. DON said R #30 could have had vomiting, irritation to the throat, developed sores in his mouth, and could have suffered other possible side effects that the poison control representative told them to monitor for such as a burning sensation to the mouth, throat, and esophagus. DON said the incident could have also resulted in a serious injury to R #30. DON said nobody witnessed R #30 actually spray the bottle or ingest the disinfectant, but the possibility still existed.
In an interview with Administrator on 10/30/23 at 2:10 PM. Administrator said on 06/19/23 R #30 grabbed a spray bottle for a liquid disinfectant and had it close to R #30's mouth. Administrator said DOR caught it right away, but because it was close to R #30's mouth, DOR notified the nurse and followed the protocol. Administrator said Administrator thought she did submit a self-report for that incident to the state survey agency. Administrator said if R #30 had in fact ingested the liquid disinfectant, then it would have been a reportable incident because it was a substance that could be harmful. Administrator said the facility was not sure if R #30 ingested the disinfectant, but the facility staffed the incident with corporate/upper management team. Administrator said LVN S had called poison control, called the doctor, and called the family. Administrator said LVN S followed what poison control said to do and followed the doctor's orders. Administrator said R #30 was not injured and continued to not have any negative side effects. Administrator said she did not recall who left the bottle on the table or how R #30 was able to obtain the bottle. Administrator said there was an incident report completed for that as it was considered an incident. Administrator said the therapy department was not supposed to have anything within reach of the residents. Administrator said the disinfectants and chemicals should have been at least in a cabinet, preferably under lock and key. Administrator said Administrator was unsure if there was a policy regarding where to store such disinfectants. Administrator said an unknown therapy staff left the bottle of disinfectant on the table. Administrator said the staff did not have it behind a closed door or cabinet. Administrator said the disinfectant bottle should not have been on the table. Administrator said the facility did not know who left it out. Administrator said the incident report did not have any interviews with staff to figure out who left the bottle out or how R #30 was able to obtain the bottle. Administrator said the progress notes noted the staff called poison control and followed the doctor's orders, and how the staff monitored R #30 for any changes. Administrator said Administrator could not recall if any staff were in-serviced for this incident. Administrator said R #30 did not exhibit any signs or symptoms that R #30 did ingest the disinfectant. Administrator said R #30 could have been harmed if he did ingest the disinfectant.
In an interview with Administrator on 10/30/23 at 3:45 PM. Administrator said the incident was not a reportable because there were no negative outcomes to R #30. Administrator said the facility continued to monitor R #30 for days and there were no injuries. Administrator said the incident report and progress notes noted the investigation and actions taken by the facility upon discovering the incident.
Record review of the incident report dated 06/19/23 at 11:59 AM reflected incident location: therapy room. Incident description: LVN S was called to the therapy area because R #30 may have consumed liquid disinfectant. Therapy staff said that R #30 had the spray bottle nozzle at his mouth but was not sure if he consumed any. Upon entering the therapy area, R #30 was found sitting in his wheelchair awake, alert, and oriented as usual and calm. LVN S immediately smelled his breath and did not notice any unusual smell. LVN S smelled the liquid disinfectant and R #30's breath had no comparison. R #30 denied consuming any liquid disinfectant. R #30's mouth was rinsed, and oral care was given. R #30 denied any mouth, throat, or esophageal burning sensation. R #30 and staff denied any dry heaves, vomiting, or spitting out liquid disinfectant. RP and NP were notified. Orders received from NP: oral care and call poison control center. R #30 was not taken to the hospital. No injuries observed at time of incident or post incident. Pre-disposing environmental factors: none. Pre-disposing physiological factors: confused, incontinent, gait imbalance, impaired memory, and weakness. Other info: liquid disinfectant within R #30's reach. Notified RP on 06/19/23 at 11:35 AM. Notified MD on 06/19/23 at 11:40 AM.
Record review of progress notes for R #30 reflected -
On 06/19/23 at 11:40 AM documented by, LVN S. LVN S was called to the therapy area because R #30 may have consumed liquid disinfectant. Therapy staff said that R #30 had the spray bottle nozzle at his mouth but was not sure if he consumed any. Upon entering the therapy area, R #30 was found sitting in his wheelchair awake, alert, and oriented as usual and calm. LVN S immediately smelled his breath and did not notice any unusual smell. LVN S smelled the liquid disinfectant and R #30's breath had no comparison. R #30 denied consuming any liquid disinfectant. R #30's mouth was rinsed, and oral care was given. R #30 denied any mouth, throat, or esophageal burning sensation. R #30 and staff denied any dry heaves, vomiting, or spitting out liquid disinfectant. RP and NP were notified. Orders received from NP: oral care and call poison control center.
On 06/19/23 at 11:45 AM, documented by, LVN S. LVN S called poison control center and explained the situation of liquid disinfectant and the immediate treatment that was rendered. As per poison control center, liquid disinfectant is non-corrosive once it is diluted. R #30 was asymptomatic of burning sensation of throat, esophagus, and mouth. There did not appear to be significant problems or reaction to product. Orders given- monitor for changes, mental changes, burning of mouth, and esophagus for 24 hours. If vomiting occurs, send to ER. Give 8 ounces of water every hour for 4 hours.
On 06/19/23 at 12:55 PM, documented by, LVN S. R #30 was awake, alert, and oriented as usual and calm. Ate 100% of lunch. R #30 denied any burning of throat, esophagus, or mouth. No nausea or vomiting. No diarrhea or upset stomach. Normal behavior.
On 06/19/23-06/23/23 progress notes reflected R #30 continued to be monitored. No signs or symptoms noted. R #30 ate without issue, and no abnormalities noted.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that all alleged violations involving abuse, neglect, or mis...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that all alleged violations involving abuse, neglect, or mistreatment, were reported immediately to the State Survey Agency, within two hours if the events that cause the allegation involve abuse or result in serious bodily injury, or not later than 24 hours if the events that cause the allegation do not involve abuse and do not result in serious bodily injury, for 1 of 1 resident (R #30) reviewed for abuse/neglect.
The facility failed to report allegations of resident neglect for R #30 for an incident on 06/19/23 to the State Survey Agency within the allotted time frame.
This failure could place all residents at increased risk for potential abuse due to unreported allegations of abuse and neglect.
The findings included:
Record review of R #30 's file reflected [AGE] year-old male with original admission date of 01/17/19 and last admission date of 03/28/23. His diagnosis included: Displaced fracture of fifth cervical vertebra, muscle wasting and atrophy, unsteadiness of feet, lack of coordination, Major depressive disorder, Parkinson's Disease, Dysphagia, and acute pain due to trauma.
Record review of R #30's MDS assessment dated [DATE] reflected BIMS was not conducted as R #30 was rarely/never understood. Functional status indicated R #30's ADL of eating (how resident eats and drinks) required extensive assistance for ADL self-performance and limited assistance for ADL support. R #30 uses a wheelchair. Functional Abilities and Goals indicated substantial/maximal assistance (helper does more than half the effort, helper lifts or holds trunk or limbs and provides more than half the effort) for picking up an object (the ability to bend/stoop from a standing position to pick up a small object, such as a spoon, from the floor).
Record review of R #30's Care Plan dated 07/27/23 reflected on 06/19/23 R #30 had a possible ingestion of liquid disinfectant. R #30 will be free of complications from possible ingestion of liquid disinfectant through review period. Date initiated: 06/20/23. Target date: 06/19/23 . Interventions: contacted poison control center on 06/19/23, informed staff to keep hazardous chemicals away from resident's reach, MD and RP notified, and provided oral care.
Record review of the incident report dated 06/19/23 at 11:59 AM reflected incident location: therapy room. Incident description: LVN S was called to the therapy area because R #30 may have consumed liquid disinfectant. Therapy staff said that R #30 had the spray bottle nozzle at his mouth but was not sure if he consumed any. Upon entering the therapy area, R #30 was found sitting in his wheelchair awake, alert, and oriented as usual and calm. LVN S immediately smelled his breath and did not notice any unusual smell. LVN S smelled the liquid disinfectant and R #30's breath had no comparison. R #30 denied consuming any liquid disinfectant. R #30's mouth was rinsed, and oral care was given. R #30 denied any mouth, throat, or esophageal burning sensation. R #30 and staff denied any dry heaves, vomiting, or spitting out liquid disinfectant. RP and NP were notified. Orders received from NP: oral care and call poison control center. R #30 was not taken to the hospital. No injuries observed at time of incident or post incident. Pre-disposing environmental factors: none. Pre-disposing physiological factors: confused, incontinent, gait imbalance, impaired memory, and weakness. Other info: liquid disinfectant within R #30's reach. Notified RP on 06/19/23 at 11:35 AM. Notified MD on 06/19/23 at 11:40 AM.
Record review of progress notes for R #30 reflected -
On 06/19/23 at 11:40 AM documented by, LVN S. LVN S was called to the therapy area because R #30 may have consumed liquid disinfectant. Therapy staff said that R #30 had the spray bottle nozzle at his mouth but was not sure if he consumed any. Upon entering the therapy area, R #30 was found sitting in his wheelchair awake, alert, and oriented as usual and calm. LVN S immediately smelled his breath and did not notice any unusual smell. LVN S smelled the liquid disinfectant and R #30's breath had no comparison. R #30 denied consuming any liquid disinfectant. R #30's mouth was rinsed, and oral care was given. R #30 denied any mouth, throat, or esophageal burning sensation. R #30 and staff denied any dry heaves, vomiting, or spitting out liquid disinfectant. RP and NP were notified. Orders received from NP: oral care and call poison control center.
On 06/19/23 at 11:45 AM, documented by, LVN S. LVN S called poison control center and explained the situation of liquid disinfectant and the immediate treatment that was rendered. As per poison control center, liquid disinfectant is non-corrosive once it is diluted. R #30 was asymptomatic of burning sensation of throat, esophagus, and mouth. There did not appear to be significant problems or reaction to product. Orders given- monitor for changes, mental changes, burning of mouth, and esophagus for 24 hours. If vomiting occurs, send to ER. Give 8 ounces of water every hour for 4 hours.
On 06/19/23 at 12:55 PM, documented by, LVN S. R #30 was awake, alert, and oriented as usual and calm. Ate 100% of lunch. R #30 denied any burning of throat, esophagus, or mouth. No nausea or vomiting. No diarrhea or upset stomach. Normal behavior.
On 06/19/23-06/23/23 progress notes reflected R #30 continued to be monitored. No signs or symptoms noted. R #30 ate without issue, and no abnormalities noted.
In an interview with LVN S on 10/30/23 at 11:50 AM. LVN S said she worked on 06/19/23 with R #30. LVN S said she was called to the therapy department because R #30 had possibly ingested a liquid disinfectant. LVN S said she went to the therapy department where R #30 was located. LVN S said she assessed R #30 and did not note any abnormalities. LVN S said the doctor gave the orders to monitor for signs and symptoms such as vomiting, nausea, or burning sensation, call poison control, and provide oral care, which LVN S did. LVN S said R #30 did not show any signs or symptoms of ingesting the disinfectant, R #30 was interacting, in good spirits, eating well, and there were no reports of symptoms. LVN S said she followed what poison control, and the manufacturer instructed her to do.
In an interview with DOR on 10/30/23 at 11:55 AM. DOR said she worked on 06/19/23 with R #30 and recalled the incident. DOR said she went to her office for a second, then went back to R #30, and R #30 had the bottle in his hand and close to his mouth. DOR said she could not recall if the nozzle was facing R #30 or if the nozzle was open or closed. DOR said she could not recall if there was any residual liquid on the nozzle. DOR said she was not sure what happened or if R #30 had ingested any of the liquid, so DOR called the nurse right away to have the nurse check R #30. DOR said the nurse assessed R #30 and notified the doctor. DOR said the doctor's orders were to monitor R #30 to see if there were signs or symptoms of R #30 ingesting the disinfectant such as redness, burning of the mouth, or vomiting. DOR said she assumed one of the other therapists had used the disinfectant or left it on the table and forgot to put it away. DOR said the bottle was not even close to R #30, but it was on a table nearby him. DOR said she did not know if R #30 reached for the bottle and how R #30 was able to get the bottle. DOR said R #30 did have the ability to pick up the bottle. DOR said the bottle was not full, so it was not very heavy. DOR said she did not recall the exact time, but this happened early in the morning on 06/19/23. DOR said she did not remember who was working or if anyone saw R #30 get the bottle. DOR said the disinfectants were kept safely in a cabinet, away from the residents' reach. DOR said that day, someone left the bottle on the table, but they should have put it back in the cabinet after using it.
In an interview with DON on 10/30/23 at 1:00 PM. DON said she was aware that there was an incident on 06/19/23 where R #30 possibly ingested a liquid disinfectant. DON said the staff responded appropriately as far as getting the nurse to assess, obtaining, and carrying out doctor's orders, calling poison control, and monitoring R #30. DON said staff failed to remove the bottle from within R #30's reach. DON said the only time the disinfectants or chemicals should have not been in a safe location, was if they were being used. DON said R #30 was not injured from this incident. DON said R #30 could have possibly been injured. DON said R #30 could have had vomiting, irritation to the throat, developed sores in his mouth, and could have suffered other possible side effects that the poison control representative told them to monitor for such as a burning sensation to the mouth, throat, and esophagus. DON said the incident could have also resulted in a serious injury to R #30. DON said nobody witnessed R #30 actually spray the bottle or ingest the disinfectant, but the possibility still existed.
In an interview with Administrator on 10/30/23 at 2:10 PM. Administrator said on 06/19/23 R #30 grabbed a spray bottle for a liquid disinfectant and had it close to R #30's mouth. Administrator said DOR caught it right away, but because it was close to R #30's mouth, DOR notified the nurse and followed the protocol. Administrator said she thought she did submit a self-report for that incident to the state survey agency. Administrator said if R #30 had in fact ingested the liquid disinfectant, then it would have been a reportable incident because it was a substance that could be harmful. Administrator said the facility was not sure if R #30 ingested the disinfectant, but the facility staffed the incident with corporate/upper management team. Administrator said LVN S had called poison control, called the doctor, and called the family. Administrator said LVN S followed what poison control said to do and followed the doctor's orders. Administrator said R #30 was not injured and continued to not have any negative side effects. Administrator said Administrator did not recall who left the bottle on the table or how R #30 was able to obtain the bottle. Administrator said there was an incident report completed for that as it was considered an incident. Administrator said the therapy department was not supposed to have anything within reach of the residents. Administrator said the disinfectants and chemicals should have been at least in a cabinet, preferably under lock and key. Administrator said she was unsure if there was a policy regarding where to store such disinfectants. Administrator said an unknown therapy staff left the bottle of disinfectant on the table. Administrator said the staff did not have it behind a closed door or cabinet. Administrator said the disinfectant bottle should not have been on the table. Administrator said the facility did not know who left it out. Administrator said the incident report did not have any interviews with staff to figure out who left the bottle out or how R #30 was able to obtain the bottle. Administrator said the progress notes noted the staff called poison control and followed the doctor's orders, and how the staff monitored R #30 for any changes. Administrator said she could not recall if any staff were in-serviced for this incident. Administrator said R #30 did not exhibit any signs or symptoms that R #30 did ingest the disinfectant. Administrator said R #30 could have been harmed if he did ingest the disinfectant.
In an interview with Administrator on 10/30/23 at 3:45 PM. Administrator said the incident was not a reportable because there were no negative outcomes to R #30. Administrator said the facility continued to monitor R #30 for days and there were no injuries. Administrator said the incident report and progress notes noted the investigation and actions taken by the facility upon discovering the incident.
Record review of the Abuse, Neglect, and Exploitation Policy (implemented 08/15/22)
Reporting/Response:
The facility will have written procedures that include:
1.
Reporting of all alleged violation to the Administrator, state agency, adult protective services and to all other required agencies (e.g. law enforcement when applicable) within specified timeframes:
a.
Immediately, but no later than 2 hours after the allegation is made, if the events that cause the allegation involve abuse or result in serious bodily injury, or
b.
Not later than 24 hours if the events that cause the allegation do not involve abuse and do not result in serious bodily injury.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to have evidence that all alleged violations involving abuse, neglect,...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to have evidence that all alleged violations involving abuse, neglect, or mistreatment, were thoroughly investigated for 1 of 1 resident (R #30) reviewed for abuse/neglect.
The facility failed to thoroughly investigate an alleged violation of neglect when R #30 was found with a bottle of liquid disinfectant in his possession near his mouth.
This failure could place all residents at increased risk for potential neglect due to uninvestigated allegations of abuse and neglect.
The findings included:
Record review of R #30 's file reflected [AGE] year-old male with original admission date of 01/17/19 and last admission date of 03/28/23. His diagnosis included: Displaced fracture of fifth cervical vertebra, muscle wasting and atrophy, unsteadiness of feet, lack of coordination, Major depressive disorder, Parkinson's Disease, Dysphagia, and acute pain due to trauma.
Record review of R #30's MDS assessment dated [DATE] reflected BIMS was not conducted as R #30 was rarely/never understood. Functional status indicated R #30's ADL of eating (how resident eats and drinks) required extensive assistance for ADL self-performance and limited assistance for ADL support. R #30 uses a wheelchair. Functional Abilities and Goals indicated substantial/maximal assistance (helper does more than half the effort, helper lifts or holds trunk or limbs and provides more than half the effort) for picking up an object (the ability to bend/stoop from a standing position to pick up a small object, such as a spoon, from the floor).
Record review of R #30's Care Plan dated 07/27/23 reflected on 06/19/23 R #30 had a possible ingestion of liquid disinfectant. R #30 will be free of complications from possible ingestion of liquid disinfectant through review period. Date initiated: 06/20/23. Interventions: contacted poison control center on 06/19/23, informed staff to keep hazardous chemicals away from resident's reach, MD and RP notified, and provided oral care.
Record review of progress notes for R #30 reflected -
On 06/19/23 at 11:40 AM documented by, LVN S. LVN S was called to the therapy area because R #30 may have consumed liquid disinfectant. Therapy staff said that R #30 had the spray bottle nozzle at his mouth but was not sure if he consumed any. Upon entering the therapy area, R #30 was found sitting in his wheelchair awake, alert, and oriented as usual and calm. LVN S immediately smelled his breath and did not notice any unusual smell. LVN S smelled the liquid disinfectant and R #30's breath had no comparison. R #30 denied consuming any liquid disinfectant. R #30's mouth was rinsed, and oral care was given. R #30 denied any mouth, throat, or esophageal burning sensation. R #30 and staff denied any dry heaves, vomiting, or spitting out liquid disinfectant. RP and NP were notified. Orders received from NP: oral care and call poison control center.
On 06/19/23 at 11:45 AM, documented by, LVN S. LVN S called poison control center and explained the situation of liquid disinfectant and the immediate treatment that was rendered. As per poison control center, liquid disinfectant is non-corrosive once it is diluted. R #30 was asymptomatic of burning sensation of throat, esophagus, and mouth. There did not appear to be significant problems or reaction to product. Orders given- monitor for changes, mental changes, burning of mouth, and esophagus for 24 hours. If vomiting occurs, send to ER. Give 8 ounces of water every hour for 4 hours.
On 06/19/23 at 12:55 PM, documented by, LVN S. R #30 was awake, alert, and oriented as usual and calm. Ate 100% of lunch. R #30 denied any burning of throat, esophagus, or mouth. No nausea or vomiting. No diarrhea or upset stomach. Normal behavior.
On 06/19/23-06/23/23 progress notes reflected R #30 continued to be monitored. No signs or symptoms noted. R #30 ate without issue, and no abnormalities noted.
Record review of the incident report dated 06/19/23 at 11:59 AM reflected incident location: therapy room. Incident description: LVN S was called to the therapy area because R #30 may have consumed liquid disinfectant. Therapy staff said that R #30 had the spray bottle nozzle at his mouth but was not sure if he consumed any. Upon entering the therapy area, R #30 was found sitting in his wheelchair awake, alert, and oriented as usual and calm. LVNS immediately smelled his breath and did not notice any unusual smell. LVN S smelled the liquid disinfectant and R #30's breath had no comparison. R #30 denied consuming any liquid disinfectant. R #30's mouth was rinsed, and oral care was given. R #30 denied any mouth, throat, or esophageal burning sensation. R #30 and staff denied any dry heaves, vomiting, or spitting out liquid disinfectant. RP and NP were notified. Orders received from NP: oral care and call poison control center. R #30 was not taken to the hospital. No injuries observed at time of incident or post incident. Pre-disposing environmental factors: none. Pre-disposing physiological factors: confused, incontinent, gait imbalance, impaired memory, and weakness. Other info: liquid disinfectant within R #30's reach. Notified RP on 06/19/23 at 11:35 AM. Notified MD on 06/19/23 at 11:40 AM.
In an interview with LVN S on 10/30/23 at 11:50 AM. LVN S said she worked on 06/19/23 with R #30. LVN S said she was called to the therapy department because R #30 had possibly ingested a liquid disinfectant. LVN S said she went to the therapy department where R #30 was located. LVN S said she assessed R #30 and did not note any abnormalities. LVN S said the doctor gave the orders to monitor for signs and symptoms such as vomiting, nausea, or burning sensation, call poison control, and provide oral care, which LVN S did. LVN S said R #30 did not show any signs or symptoms of ingesting the disinfectant, R #30 was interacting, in good spirits, eating well, and there were no reports of symptoms. LVN S said she followed what poison control, and the manufacturer instructed her to do.
In an interview with DOR on 10/30/23 at 11:55 AM. DOR said she worked on 06/19/23 with R #30 and recalled the incident. DOR said she went to her office for a second, then went back to R #30, and R #30 had the bottle in his hand and close to his mouth. DOR said she could not recall if the nozzle was facing R #30 or if the nozzle was open or closed. DOR said she could not recall if there was any residual liquid on the nozzle. DOR said she was not sure what happened or if R #30 had ingested any of the liquid, so DOR called the nurse right away to have the nurse check R #30. DOR said the nurse assessed R #30 and notified the doctor. DOR said the doctor's orders were to monitor R #30 to see if there were signs or symptoms of R #30 ingesting the disinfectant such as redness, burning of the mouth, or vomiting. DOR said she assumed one of the other therapists had used the disinfectant or left it on the table and forgot to put it away. DOR said the bottle was not even close to R #30, but it was on a table nearby him. DOR said she did not know if R #30 reached for the bottle and how R #30 was able to get the bottle. DOR said R #30 did have the ability to pick up the bottle. DOR said the bottle was not full, so it was not very heavy. DOR said she did not recall the exact time, but this happened early in the morning on 06/19/23. DOR said she did not remember who was working or if anyone saw R #30 get the bottle. DOR said the disinfectants were kept safely in a cabinet, away from the residents' reach. DOR said that day, someone left the bottle on the table, but they should have put it back in the cabinet after using it.
In an interview with DON on 10/30/23 at 1:00 PM. DON said she was aware that there was an incident on 06/19/23 where R #30 possibly ingested a liquid disinfectant. DON said the staff responded appropriately as far as getting the nurse to assess, obtaining, and carrying out doctor's orders, calling poison control, and monitoring R #30. DON said staff failed to remove the bottle from within R #30's reach. DON said the only time the disinfectants or chemicals should have not been in a safe location, was if they were being used. DON said R #30 was not injured from this incident. DON said R #30 could have possibly been injured. DON said R #30 could have had vomiting, irritation to the throat, developed sores in his mouth, and could have suffered other possible side effects that the poison control representative told them to monitor for such as a burning sensation to the mouth, throat, and esophagus. DON said the incident could have also resulted in a serious injury to R #30. DON said nobody witnessed R #30 actually spray the bottle or ingest the disinfectant, but the possibility still existed.
In an interview with Administrator on 10/30/23 at 2:10 PM. Administrator said on 06/19/23 R #30 grabbed a spray bottle for a liquid disinfectant and had it close to R #30's mouth. Administrator said Administrator did not recall who left the bottle on the table or how R #30 was able to obtain the bottle. Administrator said there was an incident report completed for that as it was considered an incident. Administrator said the therapy department was not supposed to have anything within reach of the residents. Administrator said the disinfectants and chemicals should have been at least in a cabinet, preferably under lock and key. Administrator said Administrator was unsure if there was a policy regarding where to store such disinfectants. Administrator said an unknown therapy staff left the bottle of disinfectant on the table. Administrator said the staff did not have it behind a closed door or cabinet. Administrator said the disinfectant bottle should not have been on the table. Administrator said the facility did not know who left it out. Administrator said the incident report did not have any interviews with staff to figure out who left the bottle out or how R #30 was able to obtain the bottle.
In an interview with Administrator on 10/30/23 at 3:45 PM. Administrator said the incident report and progress notes noted the investigation and actions taken by the facility upon discovering the incident.
Record review of the facility's Abuse, Neglect, and Exploitation Policy (implemented 08/15/22)
Investigation of Alleged Abuse, Neglect, and Exploitation
A. An immediate investigation is warranted when suspicion of abuse, neglect, or exploitation, or reports of abuse, neglect, or exploitation occur.
B. Written procedures for investigations include:
3. Investigating different types of alleged violations.
4. Identifying and interviewing all involved persons, including the alleged victim, alleged perpetrator, witnesses, and others who might have knowledge of the allegations.
5. Focusing the investigation on determining if abuse, neglect, exploitation, and/or mistreatment has occurred, the extent, and cause.
6. Providing complete and thorough documentation of the investigation.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Smoking Policies
(Tag F0926)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to follow their established smoking policy for 4 of 4 smoking area (Resident # 5, Resident #6, Resident #9 and Resident #10) resi...
Read full inspector narrative →
Based on observation, interview and record review, the facility failed to follow their established smoking policy for 4 of 4 smoking area (Resident # 5, Resident #6, Resident #9 and Resident #10) residents reviewed for smoking.
The facility did not follow their policy regarding residents that smoke must be always supervised. Residents R#5, R#6, R#9, R#10 were observed smoking outside without staff supervision.
This failure could place residents at risk for smoking-related injuries and fires in the facility.
Findings included:
During an observation of the smoking area on 10/24/2023 at 2:50 p.m., four residents were observed smoking unsupervised. The door that leads outside to the smoking area had a pin pad and required a code to open. When residents wanted to come back in, they must ring the doorbell and staff will open the door.
Interview on 10/24/2023 at 2:52 p.m., the DON identified those four residents as Resident #5, Resident #6, Resident #7, and Resident #8. The DON said they should have been supervised and was not sure why they were not. The DON said Staff E was scheduled to supervise the residents during smoking breaks on 10/24/2023.
Interview on 10/24/2023 at 3:11 p.m., Staff E said she was in charge of supervising the residents out in the smoking area on 10/24/2023. She said escorted Resident #5, Resident #6, Resident #7, and Resident #8 out to the smoking area at about 1:30 p.m. While she was outside with them, Staff C called her to go back inside to assist a resident at 2:00 p.m. She said after she assisted the resident, she stayed inside. She said she checked on all four residents multiple times by observing them through a window next to the exit door but did not go back outside with them. Staff E said when she was about to go outside with the residents, she saw the DON and surveyor outside the residents, so she decided to go back to the nurse's station.
Interview on 10/25/2023 at 11:18 a.m., Resident #5, said he was an occasional smoker. He said there have been times in which they are not supervised. He said staff will let them out and they must ring the bell when they are ready to come back in.
Interview on 10/25/2023 at 11:25 a.m., Resident #6, said was a smoker. He said there have been times in which they are not supervised. He said staff will let them out and they must ring the bell when they are ready to come back in.
Interview on 10/25/2023 at 11:35 a.m., Resident #9, said he smoked several times a day. He said he watched staff enter the code and memorized it. He said once he memorized the code, he goes outside to smoke without notifying staff. He said there have been times in which they are not supervised. He said staff will let them out and they must ring the bell when they are ready to come back in.
Interview on 10/25/2023 at 11:45 a.m., Resident #10 said she was an occasional smoker. She said there have been times in which they are not supervised. He said staff will let them out and they must ring the bell when they are ready to come back in.
Record review of facility's smoking schedule reflected, residents are allowed to smoke at 9:00 am, 11:00 am, 1:30 pm, 3:30 pm, and 6:30 pm. Policy had no date.
Record review of facility's smokers list reflected 7 residents who smoke.
Record review of facility's smoking/tobacco policy (no date) reflected:
Policy Statement: The facility respects the resident's right to smoke.
Policy Interpretation and Implementation:
All tobacco products will be kept by the facility staff. This includes, but is not limited to, smoking tobacco, chewing tobacco, matches, lighters, and all other types of smoking paraphernalia.
All residents will be allowed to smoke, with supervision, in the designated areas and times as stated in the Smoking/Tobacco Acknowledgment.
Smoking blankets, portable fire extinguisher and state approved ashtrays will be available in the designated areas.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide pharmaceutical services including procedures t...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide pharmaceutical services including procedures that ensure the accurate administering of all drugs and biologicals, to meet the needs of 4 of 4 (Resident #1, Resident #2, Resident #3, Resident #4) residents reviewed for pharmacy services.
Staff D and Staff E failed to accurately document on eMAR they administered Resident #1, Resident #2, Resident #3, and Resident #4's scheduled medications:
Resident #1: Systane, Atorvastatin Calcium, Erythromycin ointment, GenTeal ointment, Trazodone, Doxycycline, Hydralazine, Meclizine, Mexitrol, Keppra, MiraLAX, and Thiamine.
Resident #2: Carvedilol, Levetiracetam, Metformin, Artificial Tears, and Ticagrelor.
Resident #3: Divalproex Sodium, Mirtazapine, Trazodone, and Zoloft.
Resident #4: Pravastatin, Trazodone, Eliquis, Lactulose, and Keppra
These failures placed residents at risk for not receiving the therapeutic benefits of the prescribed medications and side effects from missed doses.
Findings included:
1.
Interview on 10/26/2023 at 11:21 a.m., Resident #1 said he did not get his eye drops and other medications on time or not get them at all. Resident #1 said his only concern he had was the administration of his medication.
Record review of Resident #1's face Sheet, dated 10/30/23, reflected he was a [AGE] year-old male admitted to facility on 09/13/2022. His diagnosis included nontraumatic intracerebral hemorrhage, dysphagia, dysarthria, spondylosis, filamentary keratitis (right eye), superficial keratitis (right eye), retention of urine, seizures and chronic systolic (congestive) heart failure.
Record review of Resident #1's Physician's orders reflected:
Systane Hydration PF Ophthalmic Solution 0.4-0.3 % instill 1 drop in both eyes four times a day for dryness, Atorvastatin Calcium Tablet 10 mg give 1 tablet by mouth at bedtime for hyperlipidemia, Erythromycin Ophthalmic ointment 5 mg/gm instill 1 application in both eyes at bedtime for Filamentary Keratitis GenTeal Tears Solution 0.1-0.2-0.3% (Artificial Tear Solution) Instill 1 drop in right eye every 12 hours for dry eyes (indefinite) Trazodone HCI Tablet 100 mg give 1 tablet by mouth at bedtime for depression, Doxycycline Hyclate Oral Tablet 100 mg give 1 tablet by mouth two times a day for pneumonia/copd exacerbation for 7 days, Hydralazine HCI Oral tablet 25 mg give 1 tablet by mouth three times a day for HTN may hold if BP <110/60, Meclizine HCI Oral Tablet 25 mg give 1 tablet by mouth three times a day for vertigo, Mexitrol ointment 3.5-10000-0.1 (Neomycin-Polymyxin-Dexameth) instill 1 application in both eyes four times a day for keratitis, Levetiracetam (Keppra) 100 mg/ml SOLN give 2.5 ml by mouth two times a day for seizure disorder, MiraLAX Powder 17 gm/scoop give 17 grams by mouth two times a day for constipation mix with 8 oz of water, and Thiamine HC Tablet 100 mg give 1 tablet by mouth two times a day for supplement.
Record review of Resident #1's eMAR for the month of February 2023 revealed:
Systane Hydration was not signed off on 02/10/2023 at 1:00 p.m.
Record review of Resident #1's eMAR for the month of September 2023 revealed:
Atorvastatin Calcium Tablet was not signed off on 09/13, 09/14, 09/15, 09/18, 09/20, 09/21, 09/23, 09/25, and 09/27 at 9:00 p.m.
Doxycycline Hyclate was not signed off on 09/15 at 5:00 p.m.
Erythromycin Ointment was not signed off on 09/25 and 09/27 at 9:00 p.m.
GenTeal Tears was not signed off on 09/12, 09/13, 09/14, 09/15, 09/18, 09/20, 09/21, 09/23, 09/25, and 09/27 at 8:00 p.m.
Hydralazine HCI was not signed off on 09/23, 09/25, and 09/27 at 8:00 p.m.
Keppra Solution was not signed off on 09/12 and 09/15 at 5:00 p.m.
Meclizine HCI was not signed off on 09/23, 09/25, and 09/27 at 8:00 p.m.
Mexitrol Ointment was not signed off on 09/25 and 09/27 at 5:00 p.m.
MiraLAX powder was not signed off on 09/12 and 09/15 at 5:00 p.m.
Systane Hydration was not signed off on 09/12, 09/13, 09/14, 09/15, 09/18, 09/20, 09/21, 09/23, 09/25, and 09/27 at 8:00 p.m.
Thiamine HCI was not signed off on 09/12 at 5:00 p.m.
Trazodone HCI was not signed off on 09/12, 09/13, 09/14, 09/15, 09/18, 09/20, 09/21, 09/23, 09/25, and 09/27 at 8:00 p.m.
Record review of Resident #1's eMAR for the month of October 2023 revealed:
Atorvastatin Calcium was not signed off on 10/23 at 9:00 p.m.
Erythromycin Ointment was not signed off on 10/23 at 8:00 p.m.
GenTeal Tears was not signed off on 10/23 at 8:00 p.m.
Systane Hydration was not signed off on 10/23 at 8:00 p.m.
Trazodone HCI was not signed off on 10/23 at 8:00 p.m.
2. Record review of Resident #2's face sheet dated 11/01/2023 reflected he was a [AGE] year-old male with the diagnosis of anoxic brain damage, encephalopathy, STEMI myocardial infarction, cardiac arrest, persistent vegetative state, and ventricular tachycardia.
Observation on 10/26/2023 at 2:00 11:45 a.m., Resident #2 was observed lying in bed asleep. He was receiving IV fluids, G-Tube and non-interviewable.
Record review of Resident #2's Physician's order reflected:
Carvedilol tablet 3.125 mg give 1 tablet via F-Tube two times a day for HTN-hold if spd < 100or dpb <60
Metformin HCI Tablet 500 mg give 1 tablet via PEG-Tube two times a day for DM
Levetiracetam Solution 100 mg/ml (Keppra) give 5 ml enterally every 12 hours for seizures
Artificial Tears Ophthalmic Solution (artificial tear solution) instill 1 drop in both eyes three times a day for dry eyes
Ticagrelor Tablet 90 mg (blood thinner) give one tablet enterally two times a day related to ST Elevation (STEMI) Myocardial Infarction
Record review of Resident #2's eMAR for the month of September 2023 reflected:
Artificial Tears was not signed off on 09/14 at 9:00 p.m.
Carvedilol Tablet was not signed off on 09/14 at 9:00 p.m.
Levetiracetam Solution (Keppra) was not signed off on 09/14 at 9:00 p.m.
Metformin was not signed off on 09/14 at 9:00 p.m.
Ticagrelor was not signed off on 09/14 at 9:00 p.m.
Record review of Resident #3's face sheet dated 11/01/2023 reflected she was an [AGE] year-old female admitted to facility on 02/11/2022 with a diagnosis of dementia, age-related physical debility, epilepsy, hypertension, major depressive disorder, bipolar disorder, and insomnia.
3. Observation of Resident #3 on 10/27/2023 at 8:00 a.m., she was lying in bed and was non-verbal.
Record review of Resident #3's Physician's order reflected:
Divalproex Sodium Tablet delayed release 500 mg give 1 tablet by mouth at bedtime for Labile Mood Disorder
Mirtazapine Oral Tablet 7.5 mg give 1 tablet by mouth at bedtime for poor appetite
Trazodone HCI oral tablet 100 mg give 1 tablet by mouth at bedtime for insomnia/depression
Zoloft tablet 50 mg (sertraline HCI) give 1 tablet by mouth at bedtime for depression
Record review of Resident #3's eMAR for the month of September 2023 reflected:
Divalproex Sodium was not signed off on 09/13, 09/14, 09/15, 09/18, 09/20, 09/23, 09/25, and 09/27 at 8:00 p.m.
Mirtazapine Oral tablet was not signed off on 09/12, 09/13, 09/14, 09/15, 09/18, 09/20, and 09/23 at 8:00 p.m.
Trazodone was not signed off on 09/12, 09/13, 09/14, 09/15, 09/18, 09/20, 09/23, 09/25, and 09/27 at 8:00 p.m.
Zoloft tablet was not signed off on 09/12, 09/13, 09/14, 09/15, 09/18, 09/20, 09/23, 09/25, and 09/27 at 8:00 p.m.
Record review of Resident #3's eMAR for the month of October 2023 reflected:
Divalproex Sodium was not signed off on 10/23 at 8:00 p.m.
Mirtazapine was not signed off on 10/23 at 9:00 p.m.
Trazodone was not signed off on 10/23 at 8:00 p.m.
Zoloft was not signed off on 10/23 at 8:00 p.m.
4. Record review of Resident #4's face sheet dated 11/01/2023 reflected she was [AGE] year-old female who was admitted to facility on 04/14/2023 with diagnosis of cerebral palsy, restlessness and agitation, acute pain due to trauma, major depressive disorder (recurrent, moderate), Type 2 diabetes, hyperlipidemia, and hypertension.
Observation on 10/27/2023 at 8:45 a.m., Resident was observed on her wheel-chair self-propelling down her hall. She was able to speak but was non-interviewable.
Record review of Resident #4's Physician's order reflected:
Eliquis Oral Tablet 5 mg (apixaban) give 1 tablet by mouth two times a day for DVT prevention
Keppra Oral Solution 100 mg/ml (Levetiracetam) give 2.5 ml by mouth three times a day for Labile Moods
Lactulose Oral Solution 20 gm/30 ml give 30 ml by mouth two times a day for constipation
Pravastatin Sodium Oral Tablet 20 mg give 1 tablet by mouth at bedtime for hyperlipidemia
Trazodone HC Oral Tablet 50 mg give 1 tablet by mouth at bedtime for insomnia/depression
Record review of Resident #4's eMAR for the month of September 2023 reflected:
Eliquis was not signed off on 09/20 at 4:00 p.m.
Keppra was not signed off on 09/12, 09/13, 09/14, 09/15, 09/18, 09/20, 09/21, 09/23, 09/25, and 09/27 at 8:00 p.m.
Lactulose was not signed off on 09/15 and 09/20 at 5:00 p.m.
Pravastatin was not signed off on 09/12, 09/13, 09/14, 09/15, 09/18, 09/20, 09/21, 09/23, 09/25, and 09/27 at 8:00 p.m.
Record review of Resident #4's eMAR for the month of October 2023 reflected:
Keppra was not signed off on 10/23 at 8:00 p.m.
Pravastatin Sodium was not signed off on 10/23 at 8:00 p.m.
Trazodone HCI was not signed off on 10/23 at 8:00 p.m.
Interview on 10/26/2023 at 2:00 p.m., the DON said she and the facility's 2 ADON's conducted daily audits of resident's record which includes eMAR's during their morning meetings. Each morning the system shows a dashboard alerting them if there were any signature missing on the MAR, skilled MAR, treatment MAR. The DON said she was not aware of any blanks on Resident #1, #2, #3 and #4's eMAR. The DON she said would provide the names of the staff members who failed to sign off on the medications for Resident #1, Resident #2, Resident #3, and Resident #4 for the months of February 2023, September 2023, and October 2023. She said she would have to check with the nursing staff to see why those medications were not signed off. She said per facility's policy LVN's, and Med Aides must sign off all medications. She said there are codes staff should use for when a resident refuses, is out of facility, or medication is not available but said the eMAR must never be left blank.
Interview on 10/27/2023 at 8:00 a.m., Resident #1 said since state was at the facility, he is getting his medication on time.
Interview on 10/27/2023 at 8:30 a.m., the DON said she had narrowed it down to Staff D and Staff E who had failed to sign off medications for Resident #1, #2, #3, and #4. All four residents were in the same hall and said the problem seemed to be during the evening shift (02:00-10:00 pm).
Interview on 10/27/2023 at 1:45 p.m., Staff D said administered all the pills to Resident #1 on 10/23/2023 but had forgotten to administer his eye drops. She said on 10/23/2023 she had gone into Resident #1's room to give him a nebulizer treatment, which he refused, and he had requested his medications. She said she knew he had eye drops scheduled but forgot to administer them because Resident #1 did not remind her. Staff D also revealed she had forgotten to sign off the 3 pills she had administered on the eMAR. Staff D said by forgetting to sign off a resident's eMAR the resident is at risk of receiving a [NAME] dose and forgetting to administer any medication the resident treatment would be delayed.
Interview on 10/31/2023 at 10:00 a.m., Staff E said her regular shift is 2:00-10:00 p.m. She said had not realized she had forgotten to sign off medications on eMAR until the DON told her on 10/26/23. She said she could not say why she had forgotten to sign off medications she administered for Resident #1, #2, #3, and #4. She said she might have gotten distracted in assisting other residents but said there was no excuse. She said, I cannot come out with something specific as to why I forgot to sign the eMAR.
Interview on 10/31/2023 at 10:30 a.m. Staff C said he is part of the team that conducted morning audits. He said the team is made up the facility's DON, and 2 ADON's. He said he occasionally assisted with Med Pass, and knew the LVN's, and Med Aides get interruptions. He said walking out of a resident's room they get confronted by other residents, family members or accidents happen (falls), and they get distracted and forget to sign the eMAR. Staff C said during their morning meetings their systems gives out alerts if any signatures are missing on the eMAR, Skilled Mar, and treatment MAR. Staff C said If they discover an eMAR was not signed, they call the staff member that was assigned to that hall/time and verify the medication was administered. They always take their word and at that time either Staff C or the staff member signed the eMAR. Staff C said he did not have an answer as to why he did not catch the blanks on Resident #1, #2, #3, and #4's eMAR. He said by not signing the eMAR a resident is at risk of receiving a double dose. He said ADON's/DON conducted quarterly trainings to licensed staff and one of the topics was medication administration which included 1. Medications to be administered on a timely manner as scheduled, 2. MAR will be signed by person administering medications after med. Pass, 3. Charge Nurse and Med Aides are to follow the 5 rights: right patient, right medication, right time, right dose, and right route. He said LVN's and Med Aides are trained 4 times a year on Med Administration.
Interview on 10/31/2023 at 2:00 p.m., the Administrator said she did not know why Staff D and Staff E had not signed off the Resident #1, Resident #2, Resident #3, and Resident #4's eMAR. She said she did not have a reason as to why her DON and ADON's did not capture the missing signatures.
Interview on 10/31/2023 at 2:40 p.m., the facility's Pharmacist went over all medications not signed off on Resident #1, Resident #2, Resident #3, and Resident #4's eMAR and stated:
Resident #1:
Missed doses of Systane and GenTeal, negative effect could have been eye dryness/irritation.
Missed doses of Erythromycin Ophthalmic, would not have caused any negative effects because he had been on it indefinite and was being used as a prophylaxis (maintenance).
Missed dose of Doxycycline, 1 missed dose would not have a negative effect.
Missed doses of Meclizine negative effect could have been he might have experienced dizziness.
Missed doses of Hydralazine negative effects would be determined if the resident's blood pressure were elevated the next morning. Staff A checked eMAR and blood pressure was within range the next morning, therefore no negative effect.
Missed doses of Mexitrol, she said there were no negative effect since it had been only 2 doses missed.
Missed doses of Keppra, no negative effect since only 2 doses were missed and he had been on it indefinite. She said it would not have caused any seizure activity because he still had it in his system.
Missed doses of MiraLAX might have caused constipation.
Missed doses of Thiamine would not have caused a negative effect since it was being used as a supplement.
Resident #2:
Missed doses Carvedilol, no negative effect since resident had been on this medication for over 1 year and blood pressure was within normal range the next morning.
Missed dose of Levetiracetam (Keppra), no negative effect since resident had been on this medication since he was admitted and has not had any seizure activity since he was admitted .
Missed dose of Artificial Tears, the only negative effect could be dryness and irritation to both eyes.
Missed dose of Ticagrelor, no negative affect since resident had been on this medication is being used as a prophylaxis.
Resident #3:
Missed dose of Zoloft, no negative affect since it was just one dose
Missed dose of Divalproex, negative effects could bring back her symptoms of depression.
Missed dose of Mirtazapine, no negative effect as this medication was being used to stimulate her appetite. DON verified her weight was stable.
Missed dose of Trazadone, the only negative effect could be not being able to sleep at night.
Resident #4:
Missed dose of Pravastatin, labs would have to be run to see if any negative effect occurred. Staff A looked back at her lab results (cholesterol) history and had been within normal range.
Missed doe of Eliquis, no negative effect since it was only one dose.
Missed dose of Trazodone/Keppra possible negative effect could be not being able to sleep at night and/or behavior problems.
Missed dose Lactulose possible negative affect could be constipation.
Interview on 11/01/2023 at 11:00 a.m., the DON said every morning the system showed a dashboard alerting if there were any signature missing on the eMAR, Skill MAR, or Treatment MAR. She said she and the 2 ADON's reviewed the alerts for the day before. She said did not remember if they had been alerted on the missing signatures for Resident #1, #2, #3, and #4 eMAR. She said, we missed it, there's really no explanation. The DON if staff forget to sign off any medication on their eMAR the resident was at risk of getting a double dose.
Interview on 11/02/2023 at 9:17 a.m. Nurse Practitioner for Resident #1 went over all medications not signed off on Resident #1's eMAR and stated:
Resident #1:
Missed doses of Systane and GenTeal, negative effect could have been eye dryness/irritation.
Missed doses of Erythromycin Ophthalmic, would not have caused eye redness.
Missed dose of Doxycycline, 1 missed dose would not have a negative effect.
Missed doses of Meclizine negative effect could have been he might have experienced dizziness.
Missed doses of Hydralazine a negative could have been elevated blood pressure. Blood pressure readings for the morning after were normal, so there was no negative effect.
Missed doses of Mexitrol, no negative effect since it was only 2 missed doses
Missed doses of Keppra, no negative effect since only 2 doses missed and he had not had any seizure activity since he was admitted to facility.
Missed doses of MiraLAX might have caused constipation.
Missed doses of Thiamine would not have caused a negative effect since it was being used as a supplement.
Interview on 11/02/2023 at 3:45 p.m., Nurse Practitioner went over Resident #3 and Resident #4's medications not signed off on their eMAR and stated:
Resident #3:
Missed doses of Divalproex, Trazodone, Mirtazapine and Zoloft were being used for psychiatric purposes and a negative effect would have been feeling moody and behavior problems. She said because she has a diagnosis of dementia those symptoms would not have been apparent therefore, no negative affect.
Resident #4:
Missed doses of Pravastatin, no negative side effects.
Missed dose of Eliquis, no negative side effect since it was only 1 missed dose.
Missed doses Trazodone might have caused sleeping problems.
Missed doses of Lactulose might have caused constipation.
Missed doses of Keppra might have caused behavior problems since it was being used for psychiatric purposes.
Record review of facility's Medication Administration policy implemented on 10/24/2022 reflected:
Policy:
Medications are administered by licensed nurses, or other staff who are legally authorized to do so in this state, as ordered by the physician and in accordance with professional standards, in a manner to prevent contamination or infection.
Policy Explanation and Compliance Guidelines:
17. Sign MAR after administered. For those medications requiring vital signs, record the vital signs onto the MAR.
20. Correct any discrepancies and report to nurse manager.