LEA HILL REHABILITATION AND CARE CENTER




Inspected within the last 6 months. Data reflects current conditions.
Lea Hill Rehabilitation and Care Center has a Trust Grade of B, indicating it is a good choice for families seeking care, although it is not the top tier. It ranks #20 out of 190 facilities in Washington, placing it in the top half, and #4 out of 46 in King County, meaning only three local facilities are rated higher. The facility is improving, with a reduction in issues from 15 in 2024 to 14 in 2025. Staffing is rated 4 out of 5, which is a strength, though the turnover rate of 55% is slightly above the state average. However, the facility has been fined $30,258, which is concerning as it suggests ongoing compliance issues. Regarding care incidents, one serious finding indicated that a resident did not receive timely wound care as prescribed, leading to worsening pressure ulcers. Additionally, the facility failed to provide proper written notifications for transfers or discharges, risking misalignment with residents' care goals. A concern was also noted about food safety practices in the kitchen, as staff did not maintain sanitizer solutions correctly, which could lead to foodborne illnesses. While there are strengths in staffing and an overall excellent rating, these specific incidents highlight areas needing improvement.
- Trust Score
- B
- In Washington
- #20/190
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 55% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ⚠ Watch
- $30,258 in fines. Higher than 94% of Washington facilities. Major compliance failures.
- Skilled Nurses ✓ Good
- Each resident gets 73 minutes of Registered Nurse (RN) attention daily — more than 97% of Washington nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 39 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Near Washington avg (46%)
Higher turnover may affect care consistency
Below median ($33,413)
Moderate penalties - review what triggered them
The Ugly 39 deficiencies on record
Sept 2025
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure privacy for 1 of 1 resident (Resident 7) observed for medication administration via Gastric Tube (GT -tube inserted thr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0605
(Tag F0605)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to offer nonpharmacological interventions to 3 of 5 residents (Residents 3, 29, & 45), monitor specific target behaviors for 1 o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0628
(Tag F0628)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide the resident and/or the resident's representative and Ombud...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure 3 (Residents 2, 8, & 5) of 12 sample residents ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure Pre-admission Screening and Resident Review (PASRR - a menta...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to develop and/or implement comprehensive Care Plans (CP) for 3 of 16 residents (Resident 29, 7, & 3) whose CPs were reviewed. F...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to clarify physician orders to include medication dosing ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure residents who were dependent on staff for assistance with Activities of Daily Living (ADLs - i.e. grooming, bathing, ea...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure weekly skin assessments were completed for 1 (R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure enteral nutrition (the delivery of nutrients through a feeding tube directly into the stomach) was administered in acc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure proper storage of medications for 1 of 2 staff (Staff F - Registered Nurse) observed during medication administration ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure staff used appropriate Personal Protective Equi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure 2 of 2 residents (Resident 8 & 7) reviewed for ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to ensure cold food was held at 41-degree Fahrenheit (F) or lower during lunch preparation. Failure by the facility to ensure foo...
Read full inspector narrative →
Jul 2024
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 13>
Review of a 06/01/2024 admission MDS, Resident 13 had difficulty hearing, was sometimes understood, and coul...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 13>
According to the 06/01/2024 admission MDS, Resident 13 had a diagnosis of a progressive memory loss disease....
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a Pre-admission Screening and Resident Review (PASRR - a process to determine if a potential nursing home resident had mental health...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 21>
According a 04/18/2024 Significant Change MDS, Resident 21 had moderate memory impairment. The assessment sh...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure 1 resident (Resident 3) of 3 reviewed for vision and hearing were provided the assistance and/or adaptive devices they ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 21>
According a 04/18/2024 Significant Change MDS, Resident 21 had moderate memory impairment. The assessment sh...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Urinary Catheter>
<Facility Policy>
According to the facility policy titled, Catheter Care, dated [DATE], residents...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to assess, monitor, and record intake for 1 (Resident 8) of 1 resident reviewed for enteral feeding (a medical process used to pr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Oxygen Signage>
<Resident 241>
Observations on 06/28/2024 at 8:20 AM and on 07/01/2024 at 8:33 AM showed Resident 2...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure, 1 of 5 (Resident 13) residents reviewed for unnecessary medications was adequately monitored to prevent excessive duration of medic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure 2 (Residents 21 & 238) of 5 residents reviewed for unnecessary medications were free from unnecessary psychotropic medications. Faci...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
<<Following Physician Orders>
<Resident 13>
According to the 06/01/2024 MDS, Resident 13 was unable to control their blood sugars and received insulin (medication that helped to contro...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to consistently perform Hand Hygiene (HH) before and aft...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement a system to ensure residents received required written no...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to ensure resident meals were prepared in accordance with professional standards of food safety for 2 of 2 facility kitchens. The failure to ens...
Read full inspector narrative →
Apr 2023
10 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure 1 of 3 residents (Resident 23) reviewed for pr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to inform a resident or the resident's representative of treatment risks and benefits, treatment options, and treatment alternati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to develop and implement a process to ensure residents have an Advanced Directive (AD) for 3 of 15 residents (Residents 9, 11, & 20) reviewed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 23
Review of a 03/17/2023 admission MDS showed Resident 23 admitted to the facility on [DATE] and was assessed to have ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure residents were free from unnecessary psychotropic drugs (medications that affect mental state). The failure to provide non-medicatio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure a medication error rate of less than 5 percent (%). Failure of 1 of 2 nurses (Staff H) to properly administer 2 of 30 m...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure incident investigations were completed according to professional standards for 2 of 5 residents (Residents 11 & 6) reviewed for acci...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to implement a competency-based education program to ensure 4 of 8 (Staff B, C, I & Z) and 1 supplemental (Staff D) nursing staff...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
TBP - Contact Precautions
Facility Policy
According to the undated IPCP policy, all staff were responsible for following all policies and procedures related to their isolation program including TBP. T...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview the facility failed to ensure expired foods were identified and discarded, did not ensure equipment was clean and secure, and ensure staff implemented proper hand hy...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • 39 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $30,258 in fines. Higher than 94% of Washington facilities, suggesting repeated compliance issues.
About This Facility
What is Lea Hill Rehabilitation And's CMS Rating?
CMS assigns LEA HILL REHABILITATION AND CARE CENTER an overall rating of 5 out of 5 stars, which is considered much above average nationally. Within Washington, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Lea Hill Rehabilitation And Staffed?
CMS rates LEA HILL REHABILITATION AND CARE CENTER's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 55%, compared to the Washington average of 46%. RN turnover specifically is 64%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Lea Hill Rehabilitation And?
State health inspectors documented 39 deficiencies at LEA HILL REHABILITATION AND CARE CENTER during 2023 to 2025. These included: 1 that caused actual resident harm and 38 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
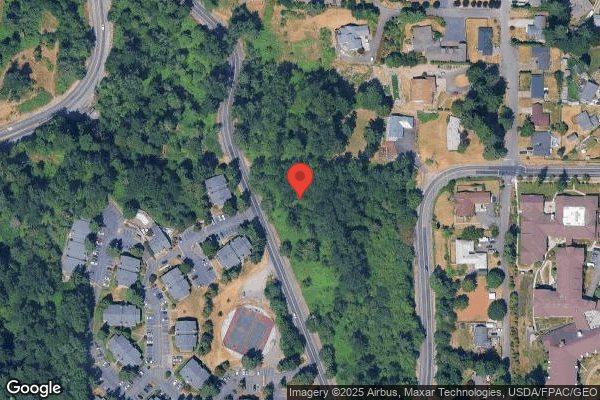
Who Owns and Operates Lea Hill Rehabilitation And?
LEA HILL REHABILITATION AND CARE CENTER is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 36 certified beds and approximately 32 residents (about 89% occupancy), it is a smaller facility located in AUBURN, Washington.
How Does Lea Hill Rehabilitation And Compare to Other Washington Nursing Homes?
Compared to the 100 nursing homes in Washington, LEA HILL REHABILITATION AND CARE CENTER's overall rating (5 stars) is above the state average of 3.2, staff turnover (55%) is near the state average of 46%, and health inspection rating (4 stars) is above the national benchmark.
What Should Families Ask When Visiting Lea Hill Rehabilitation And?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Lea Hill Rehabilitation And Safe?
Based on CMS inspection data, LEA HILL REHABILITATION AND CARE CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 5-star overall rating and ranks #1 of 100 nursing homes in Washington. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Lea Hill Rehabilitation And Stick Around?
LEA HILL REHABILITATION AND CARE CENTER has a staff turnover rate of 55%, which is 9 percentage points above the Washington average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Lea Hill Rehabilitation And Ever Fined?
LEA HILL REHABILITATION AND CARE CENTER has been fined $30,258 across 1 penalty action. This is below the Washington average of $33,381. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Lea Hill Rehabilitation And on Any Federal Watch List?
LEA HILL REHABILITATION AND CARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.