STAFHOLT HEALTH AND REHABILITATION OF CASCADIA




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Stafholt Health and Rehabilitation of Cascadia has a Trust Grade of B, indicating it is a solid choice for care, sitting in the top half of Washington state facilities at #43 out of 190. Within Whatcom County, it ranks #3 out of 8, meaning there are only two local options that rate higher. The facility is improving, with issues decreasing from 22 in 2024 to just 5 in 2025. Staffing is rated good with 4 out of 5 stars, although the 51% turnover rate is average compared to the state average of 46%. However, the facility has been fined $47,182, which is concerning but aligns with the average for the state. While the nursing home offers strong RN coverage, exceeding 98% of state facilities, there have been specific incidents of concern. For example, two residents experienced severe weight loss due to inadequate meal supervision and nutritional assessments, which could lead to further health issues. Additionally, there were failures in medication storage that could risk residents receiving ineffective treatments, and staff were found to lack necessary qualifications in dietary management. Overall, while there are strengths in care quality and staffing, these incidents highlight areas that need attention.
- Trust Score
- B
- In Washington
- #43/190
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 51% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $47,182 in fines. Higher than 61% of Washington facilities. Some compliance issues.
- Skilled Nurses ✓ Good
- Each resident gets 87 minutes of Registered Nurse (RN) attention daily — more than 97% of Washington nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 59 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Near Washington avg (46%)
Higher turnover may affect care consistency
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 59 deficiencies on record
Sept 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure 1 of 1 resident (Resident 1) received medically related soci...
Read full inspector narrative →
Mar 2025
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that 1 of 5 residents (Resident 155) reviewed for informed c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure resident care plans were reviewed and revised fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide services that ensured a resident's abilities i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to assess and implement resident centered pain interventi...
Read full inspector narrative →
Oct 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to provide notification to the resident's representative of a change in...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure 3 of 3 residents (Residents 1, 2 and 3) who had orders for da...
Read full inspector narrative →
Aug 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure 1 of 3 residents (Resident 2), reviewed for non-pressure re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure dental services was coordinated for 1 of 3 sampled resident...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0678
(Tag F0678)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure 3 of 6 facility nursing staff responsible for providing cardi...
Read full inspector narrative →
Jul 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure residents had the right to voice grievances related to call light response time, missing personal items, and excessive wait times wit...
Read full inspector narrative →
Apr 2024
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure 2 of 3 resident's (Resident 3 and 4) choice of bathing frequ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to provide the required refund for 1 of 4 sampled residents and/or thei...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to thoroughly investigate an allegation of potential abuse and neglect ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to arrange hospice services for 1 of 1 resident (Resident 2) reviewed ...
Read full inspector narrative →
Feb 2024
12 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .
Based on observation, interview, and record review the facility failed to offer assistance and supervision with meals, consist...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure criminal background checks were completed for 2 of 5 sampled facility staff (Staff U and V) and failed to ensure the Omnibus Reconci...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure 1 of 1 resident (Resident 28) reviewed for resp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure that routine dental services were coordinated ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, and interview, the facility failed to provide a homelike environment for 1 of 2 dining rooms (East Dining ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <RESIDENT 8>
Resident 8 admitted to the facility on [DATE] with diagnoses to include stroke affecting their left side, maj...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <RESIDENT 41>
Resident 41 admitted to the facility on [DATE] with diagnoses to include stroke, diabetes type 2 (a conditio...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <RESIDENT 8>
Resident 8 admitted to the facility on [DATE] with diagnoses to include stroke affecting their left side, maj...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to serve meals that were at a safe temperature and appeti...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure staff were compliant with Infection Prevention ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review the facility failed to ensure pneumococcal vaccines (a vaccine that protects against pneum...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
Based on observations, interview, and record review the facility failed to ensure drugs and biologicals were stored in accordance with state and federal laws for 2 of 2 medication refrigerators (East ...
Read full inspector narrative →
Dec 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to ensure 1 of 1 resident (Resident 1) had their rights respected and honored when their choice to have a personal phone to commun...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure residents were free from accidents for 1 of 3 r...
Read full inspector narrative →
Apr 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop and implement a comprehensive person-centered care plan to ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to comprehensively assess the physical, mental, and psychosocial needs of a resident with dementia and identify the risks and de...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure 3 of 3 residents (Residents 1, 2 and 3) reviewe...
Read full inspector narrative →
Nov 2022
27 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide advanced written notice for room changes, to include the re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to assess resident bathing preferences for 1 of 3 residents (14) revie...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to provide 3 of 3 residents (14, 4, 43) required and/or timely notice...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to provide a homelike environment in 3 of 3 resident rooms (rooms [ROOM ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to comprehensively assess and monitor the need for physi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure Minimum Data Set (MDS) assessments were accurate for three o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** RESIDENT 40
Resident 40 admitted to the facility 09/06/2022 with diagnosis to include diabetes (chronic condition that effects t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to review and revise care plans for 2 of 2 residents (6, a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to discuss and provide the necessary written discharge instructions fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** RESIDENT 41
Resident 41 admitted on [DATE] with diagnoses to include lung disease and stroke. The resident was admitted on hospi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <BLOOD SUGAR PARAMETERS>
Review of the facility policy titled, Diabetic Management, revised 01/28/2022 showed if a residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure residents were provided with interventions to m...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure 1 of 2 residents (41) reviewed for respiratory care and trea...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure a bedrail assistive device was placed on a resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on interview and record review, the facility failed to ensure one of five residents (27) were free from unnecessary psych...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure complete and accurate clinical records were maintained for 3...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that hospice services met professional standards for one of ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the infection prevention and control Antibiotic Stewardship ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to conduct comprehensive assessments of a resident's need...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** RESIDENT 26
Resident 26 admitted to the facility on [DATE] with diagnosis including Parkinson's and swallowing difficulty.
Revi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure annual Nurse Aide (NA) performance reviews were completed for six of six employees (J, Q, R, S, T, and U ) files reviewed who had be...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the staff were compliant with Infection Preven...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on interview, the facility failed to ensure that unless the facility employed a full time Registered Dietitian, the director of food and nutrition services had completed an academic program in n...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure proper heat sanitation of dishware in 1 of 1 high-temperature dishwashing machines. This failed practice placed reside...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure a designated and qualified staff person was at the facility to serve as an Infection Preventionist (IP). This failure placed the res...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure nurse staffing information postings were current, accurate, and posted in one of two prominent locations. These failure...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Garbage Disposal
(Tag F0814)
Minor procedural issue · This affected multiple residents
Based on observation and interview, the facility failed to ensure 1 of 1 garbage storage areas was maintained in a sanitary condition due to a failure to contain all trash within the dumpsters. This f...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 harm violation(s), $47,182 in fines, Payment denial on record. Review inspection reports carefully.
- • 59 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $47,182 in fines. Higher than 94% of Washington facilities, suggesting repeated compliance issues.
About This Facility
What is Stafholt Of Cascadia's CMS Rating?
CMS assigns STAFHOLT HEALTH AND REHABILITATION OF CASCADIA an overall rating of 5 out of 5 stars, which is considered much above average nationally. Within Washington, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Stafholt Of Cascadia Staffed?
CMS rates STAFHOLT HEALTH AND REHABILITATION OF CASCADIA's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 51%, compared to the Washington average of 46%.
What Have Inspectors Found at Stafholt Of Cascadia?
State health inspectors documented 59 deficiencies at STAFHOLT HEALTH AND REHABILITATION OF CASCADIA during 2022 to 2025. These included: 1 that caused actual resident harm, 56 with potential for harm, and 2 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
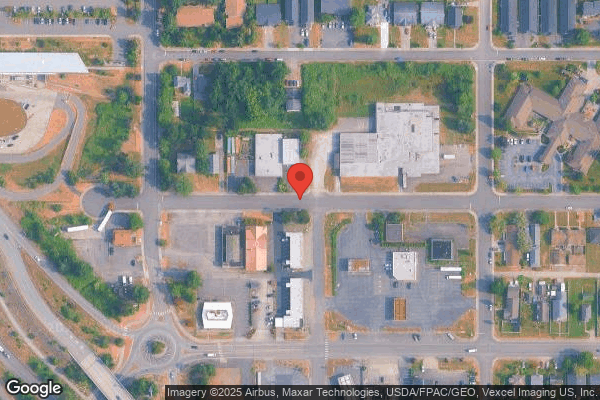
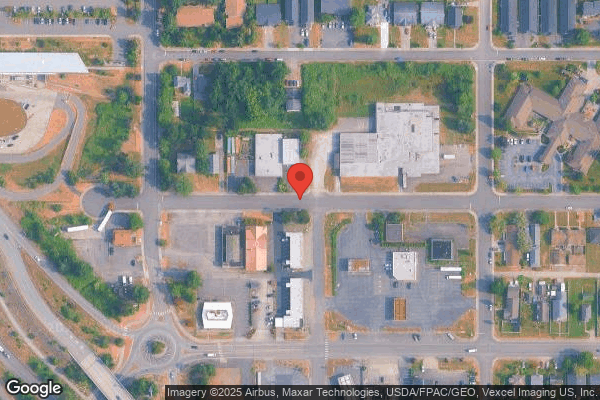
Who Owns and Operates Stafholt Of Cascadia?
STAFHOLT HEALTH AND REHABILITATION OF CASCADIA is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by CASCADIA HEALTHCARE, a chain that manages multiple nursing homes. With 57 certified beds and approximately 50 residents (about 88% occupancy), it is a smaller facility located in BLAINE, Washington.
How Does Stafholt Of Cascadia Compare to Other Washington Nursing Homes?
Compared to the 100 nursing homes in Washington, STAFHOLT HEALTH AND REHABILITATION OF CASCADIA's overall rating (5 stars) is above the state average of 3.2, staff turnover (51%) is near the state average of 46%, and health inspection rating (4 stars) is above the national benchmark.
What Should Families Ask When Visiting Stafholt Of Cascadia?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Stafholt Of Cascadia Safe?
Based on CMS inspection data, STAFHOLT HEALTH AND REHABILITATION OF CASCADIA has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 5-star overall rating and ranks #1 of 100 nursing homes in Washington. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Stafholt Of Cascadia Stick Around?
STAFHOLT HEALTH AND REHABILITATION OF CASCADIA has a staff turnover rate of 51%, which is about average for Washington nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Stafholt Of Cascadia Ever Fined?
STAFHOLT HEALTH AND REHABILITATION OF CASCADIA has been fined $47,182 across 2 penalty actions. The Washington average is $33,551. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Stafholt Of Cascadia on Any Federal Watch List?
STAFHOLT HEALTH AND REHABILITATION OF CASCADIA is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.