WESLEY HOMES DES MOINES HEALTH CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Wesley Homes Des Moines Health Center has received a Trust Grade of D, indicating below-average performance with some concerns regarding care quality. It ranks #123 out of 190 facilities in Washington, placing it in the bottom half, and #27 out of 46 in King County, meaning there are better local options available. The facility is improving, having reduced the number of issues from 23 in 2023 to 21 in 2024. Staffing is rated at 3 out of 5 stars with a turnover rate of 40%, which is lower than the state average, suggesting that staff are relatively stable. However, the facility has faced significant fines totaling $33,540, which is concerning for compliance issues. Specific incidents raised by inspectors include a failure to properly assess and treat a resident's hip fracture after a fall, leading to harm and reduced quality of life. Additionally, there were issues with adequate supervision for residents, resulting in a wrist fracture for another resident due to falls. On a positive note, the quality measures rating is excellent at 5 out of 5 stars, indicating that when care is delivered, it meets high standards. Overall, while the facility has strengths in stability and quality measures, the serious incidents and below-average trust grade raise valid concerns for families considering this nursing home.
- Trust Score
- D
- In Washington
- #123/190
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ○ Average
- 40% turnover. Near Washington's 48% average. Typical for the industry.
- Penalties ⚠ Watch
- $33,540 in fines. Higher than 78% of Washington facilities, suggesting repeated compliance issues.
- Skilled Nurses ✓ Good
- Each resident gets 55 minutes of Registered Nurse (RN) attention daily — more than average for Washington. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 58 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (40%)
8 points below Washington average of 48%
Facility shows strength in quality measures, fire safety.
The Bad
Near Washington average (3.2)
Meets federal standards, typical of most facilities
Near Washington avg (46%)
Typical for the industry
Above median ($33,413)
Moderate penalties - review what triggered them
The Ugly 58 deficiencies on record
Oct 2024
21 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure informed consent (a process explaining the risks and benefits of a treatment prior to use) was obtained prior to administration of ps...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to thoroughly investigate and rule out abuse/neglect for 1 of 1 sample...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 46>
Review of Resident 46's 08/31/2024 Discharge Return Anticipated MDS showed the resident was transferred to a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the Preadmission Screening and Resident Review (PASRR) proce...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a Pre-admission Screening and Resident Review (PASRR - a pro...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to develop and/or implement a comprehensive Care Plan (C...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Wandering>
<Resident 213>
According to the 09/23/2024 admission MDS, Resident 213 admitted to the facility on [DATE...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure the resident environment was free of accident h...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure 1 of 3 sampled residents (Residents 212) with u...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure 1 of 3 sampled residents (Resident 33) reviewe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0728
(Tag F0728)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure staff with a Nursing Assistant Registered (NAR) certificate completed a Certified Nursing Assistant (CNA) class and passed the state...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure 3 (Residents 3, 35, & 53) of 5 residents reviewed for unnece...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure a medication error rate of less than 5 Percent (%). Failure to properly administer 28 of 35 medications for 4 of 6 resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure dietary orders pertaining to the consistency o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation interview and record review the facility failed to store, prepare and serve food in accordance with food service safety standards. The failure to cover, label and date stored food...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected 1 resident
Based on observation and interview the facility failed to ensure 2 of 3 garbage dumpsters and 1 of 2 recycling dumpsters were properly covered, the surrounding areas were kept clean, and free of trash...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to provide assistance with Activities of Daily Living (ADL), related to cleanliness and grooming for 5 (Residents 2, 3, 24, 35, &...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Enhanced Barrier Precautions (EBP)>
Review of the facility policy Enhanced Barrier Precautions dated 07/26/2024 showed th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to develop, implement and maintain an in-service training program that ensured 4 of 4 Nursing Aides (Staff H, I, J & K) completed the required...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to ensure nurse and nurse aide staff had the appropriate competencies and skill sets to provide nursing and related services, to assure residen...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to implement a facility-wide system for Antibiotic (ABO) Stewardship (a program to improve how ABO medications are prescribed, treating bacter...
Read full inspector narrative →
Aug 2023
21 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0569
(Tag F0569)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure funds were reimbursed to the state Office of Financial Recovery (OFR), within 30 days of resident discharge or death, for 2 (Resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 7>
Review of a 05/15/2023 Quarterly MDS showed Resident 7 admitted to the facility on [DATE] and had diagnoses o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to notify State Survey Agency (SA) of an unwitnessed fall with injury in an area not generally vulnerable to trauma for 1 of (Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed ensure a system by which the office of the State Long-Term Care Ombuds...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure baseline Care Plans (Baseline CP - individualized instructio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 47>
According to the 07/03/2023 admission MDS Resident 47 had multiple medically complex diagnoses including fra...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 9>
According to the 05/16/2023 Quarterly MDS Resident 9 was assessed to make their own decisions, was understood...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
<Resident 9>
According to 05/16/2023 Quarterly MDS Resident 9 had diagnosis of heart failure, depression, and Schizophrenia (mental illness affecting a person's ability to think, feel and behave...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
<Resident 41>
<Translation and/or Interpretation of Facility Services Policy>
An undated facility Translation and/or Interpretation of Facility Services Policy showed residents would have ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to assess for bladder needs to alert and oriented residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident Room>
Observation on 08/03/2023 at 5:01 PM in room [ROOM NUMBER] showed Resident 7 had a bottle of liquid pain m...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
<Resident 41>
According to the 05/23/2023 Quarterly MDS, Resident 41 did not have any problems with mouth or facial pain, discomfort, or difficulty with chewing.
Resident 41's 05/24/2023 nutrit...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to provide privacy during personal care for 1 of 19 (Resident 1) residents and to cover Foley Catheter bags (FC- a tube placed in...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to ensure resident rooms had access to fresh air, were clean, free of cl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure 3 of 6 (Residents 59,12 & 33) residents reviewe...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview the facility failed to ensure the environment was free of accident hazards on 3 (100 Hall, 20...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to put into practice protocols necessary to optimize the treatment of ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to ensure food was stored, prepared, and transported in a sanitary manner, and in accordance with professional standards of food ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to update the Facility Assessment (FA - a required document that comprehensively assesses the levels and types of care provided, the demograph...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Refer to F881 - Antibiotic Stewardship Program.
Refer to F882 - Infection Preventionist Qualifications/Role.
REFERENCE: WAC 388-97-1320 (1)(a).
Based on observations, interview, and record review the ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure there was a designated Infection Preventionist (IP) who worked at least part-time at the facility responsible for the facility's eff...
Read full inspector narrative →
Mar 2023
2 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
.
Based on observations, interviews, and record reviews the facility failed to ensure one of two residents (Resident 2) reviewed for falls with fractures, received care and services according to profe...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on observations, interviews, and record review the facility failed to provide adequate supervision, implement care interventions, and/or complete a thorough investigation of accidents for 2 of 2...
Read full inspector narrative →
May 2022
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to effectively implement the abuse, neglect, and misappropriation policy for 2 (Residents 31 & 73) of 14 residents reviewed for grievances. Fac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 87
According to the 05/04/2022 admission MDS-an assessment tool, Resident 87 readmitted to the facility on [DATE], was ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0678
(Tag F0678)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review the facility failed to ensure residents had physician orders to reflect their code status ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide the necessary care and services in accordance with professi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure 1 (Resident 87) of 1 resident reviewed for inco...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide care and services to identify potential weight...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 87
According to the 05/04/2022 MDS Resident 87 readmitted to the facility on [DATE] with diagnoses including respirator...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 87
According to the 05/04/2022 Admissions MDS, Resident 87 was cognitively intact, required supervision for eating, and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0569
(Tag F0569)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure funds were reimbursed to the individual, or the state Office...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 87
According to the 05/04/2022 MDS Resident 87 readmitted to the facility on [DATE] with diagnoses including respirator...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to effectively implement their Grievance Policy and Procedures for 1 (Residents 73) of 7 residents who participated in the 05/17/2022 Resident...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide assistance with activities of daily living (AD...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure expired (outdated) medications were returned to...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and review of facility policy, the facility failed to store, prepare, distribute, and serve food in accordance with professional standards for food service safety fo...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 40% turnover. Below Washington's 48% average. Good staff retention means consistent care.
- • 58 deficiencies on record, including 2 serious (caused harm) violations. Ask about corrective actions taken.
- • $33,540 in fines. Higher than 94% of Washington facilities, suggesting repeated compliance issues.
- • Grade D (45/100). Below average facility with significant concerns.
About This Facility
What is Wesley Homes Des Moines's CMS Rating?
CMS assigns WESLEY HOMES DES MOINES HEALTH CENTER an overall rating of 3 out of 5 stars, which is considered average nationally. Within Washington, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Wesley Homes Des Moines Staffed?
CMS rates WESLEY HOMES DES MOINES HEALTH CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 40%, compared to the Washington average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Wesley Homes Des Moines?
State health inspectors documented 58 deficiencies at WESLEY HOMES DES MOINES HEALTH CENTER during 2022 to 2024. These included: 2 that caused actual resident harm and 56 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Wesley Homes Des Moines?
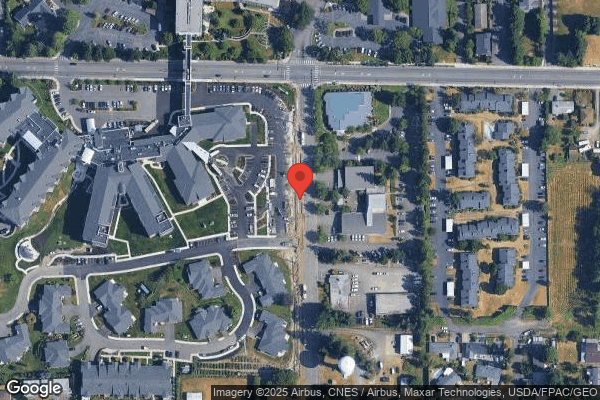
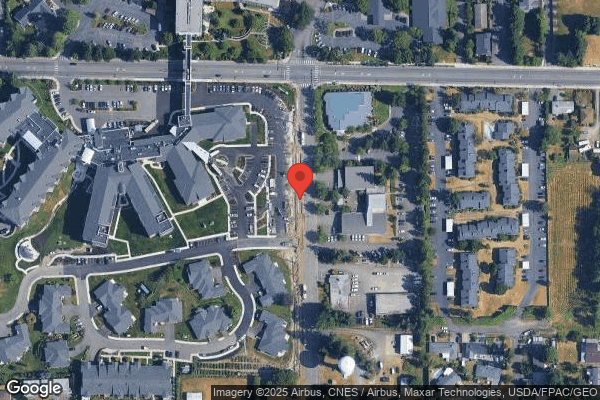
WESLEY HOMES DES MOINES HEALTH CENTER is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 148 certified beds and approximately 67 residents (about 45% occupancy), it is a mid-sized facility located in DES MOINES, Washington.
How Does Wesley Homes Des Moines Compare to Other Washington Nursing Homes?
Compared to the 100 nursing homes in Washington, WESLEY HOMES DES MOINES HEALTH CENTER's overall rating (3 stars) is below the state average of 3.2, staff turnover (40%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Wesley Homes Des Moines?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Wesley Homes Des Moines Safe?
Based on CMS inspection data, WESLEY HOMES DES MOINES HEALTH CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in Washington. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Wesley Homes Des Moines Stick Around?
WESLEY HOMES DES MOINES HEALTH CENTER has a staff turnover rate of 40%, which is about average for Washington nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Wesley Homes Des Moines Ever Fined?
WESLEY HOMES DES MOINES HEALTH CENTER has been fined $33,540 across 1 penalty action. The Washington average is $33,414. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Wesley Homes Des Moines on Any Federal Watch List?
WESLEY HOMES DES MOINES HEALTH CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.