ENUMCLAW HEALTH & REHAB CENTER




Inspected within the last 6 months. Data reflects current conditions.
Enumclaw Health & Rehab Center has received a Trust Grade of D, indicating below-average performance with some concerns about care quality. It ranks #140 out of 190 facilities in Washington, placing it in the bottom half of all nursing homes in the state, and #35 out of 46 in King County, suggesting that only a few local options are better. The facility is worsening, with issues increasing from 21 in 2024 to 23 in 2025. While staffing is average with a turnover rate of 68%, which is concerning compared to the state average of 46%, the center does have adequate RN coverage. However, there are significant issues, including a failure to store food safely, risking potential food-borne illnesses, and inadequate therapeutic services for residents, which could lead to declines in their physical condition and quality of life.
- Trust Score
- D
- In Washington
- #140/190
- Safety Record
- Low Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 68% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $8,018 in fines. Higher than 62% of Washington facilities. Some compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 40 minutes of Registered Nurse (RN) attention daily — about average for Washington. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 65 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Washington average (3.2)
Below average - review inspection findings carefully
22pts above Washington avg (46%)
Frequent staff changes - ask about care continuity
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
20 points above Washington average of 48%
The Ugly 65 deficiencies on record
Sept 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure residents who were dependent on staff for assistance with Activities of Daily Living (ADLs - i.e. grooming, bathing, ea...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure specialized rehabilitative services were provided as determined by the physician's orders for 1 (Resident 53) of 2 resi...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to initiate, investigate, and resolve grievances for 6 of 12 sampled residents (Residents 2, 3, 4, 5, 6, 7, 8 ) reviewed for grie...
Read full inspector narrative →
Jun 2025
20 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide care in a manner that promoted dignity for 2 (Resident 13 & 18) of 17 sample residents reviewed. The facility failed t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0569
(Tag F0569)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure funds were reimbursed to the state Office of Financial Recove...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 24>
According to a 02/10/2025 Annual MDS, Resident 24 had no areas of concern for their dental status.
In an int...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the recommendation of a Level II Preadmission Screen and Resident Review (PASRR) evaluation was incorporated into the Care Plan (CP)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Medications Given Outside of Parameters>
<Resident 45>
According to a 05/27/2025 Significant Change Minimum Data Se...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure residents received proper assistive devices to maintain vision and hearing abilities for 1 (Resident 46) of 2 residents...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 3>
According to an 04/25/2025 Quarterly MDS, Resident 3 had multiple medically complex diagnoses, was dependent ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure specialized rehabilitative services were provid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
<Unit 500>
Observation on 06/12/2025 at 9:50 AM showed a unit 500 nurse run sheet left unattended in view on the unit 500 medication cart. The unit 500 nurse run sheet included resident's names,...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Hand Hygiene>
<Dining>
Observations of meal tray pass on 06/08/2025 at 12:53 PM, showed Staff V delivering a lunch ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Carpet>
Observations on 06/08/2025 at 8:52 AM, 06/11/2025 at 5:54 AM, and 06/13/2025 at 11:29 AM showed a large carpet st...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 3>
According to a 04/25/2025 Quarterly MDS, Resident 3 had multiple medically complex diagnoses including a hist...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0628
(Tag F0628)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 24>
Review of Resident 24's 07/15/2024 and 10/15/2024 Discharge MDS showed the resident was transferred to an ac...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 24>
According to a 05/09/2025 Quarterly MDS, Resident 24 had clear speech, understands, and was understood by ot...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Resident 24>
According to a 05/09/2025 Quarterly MDS, Resident 24 had clear speech, was able to understand, and be unders...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure treatments were done as ordered and documented by staff for 2 of 2 residents (Residents 52 & 28) reviewed for antibiot...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to ensure Narcotic Ledgers were accurate for 2 of 2 Narcotic Ledgers (500 cart & 200/300 cart) reviewed for accuracy. Failure to ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to ensure a medication error rate of less than 5 Percent (%). Failure to properly administer 5 of 28 medications for 2 of 5 resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <100 Unit>
<Resident 44>
Review of Resident 44's 06/09/2025 physician orders showed the resident did not have an ord...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to store, prepare, and serve food under sanitary conditions. Failure to ensure food items in the dietary department were properly...
Read full inspector narrative →
May 2024
21 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide care and services in a manner that maintained and promoted dignity while assisting with meals for 3 of 18 residents (R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide a comfortable, appropriately sized bed for 1 of 1 resident (Resident 15) reviewed for accommodation of needs. This fai...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
<Resident 28>
Review of Resident 28's census information showed Resident 28 was transferred to the hospital for low blood pressure and low blood-oxygen levels on 03/19/2024.
Review of Resident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a Significant Change in Status Assessment (SCSA), including Care Area Assessments (CAAs), was completed within 14 days for 1 of 1 re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a Pre-admission Screening and Resident Review (PASRR - a pro...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
<Resident 8>
According to the 02/26/2024 admission MDS, Resident 8 was understood and could understand by others in conversation. This MDS showed Resident 8 had no memory impairment and particip...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
<Resident 53>
Review of the 03/25/2024 Quarterly MDS, showed Resident 53 had no memory impairment and had diagnoses of a stroke with limited mobility to one side of their body. This assessment s...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
<Resident 29>
Review of Resident 29's May 2024 MAR showed the resident had a 10/24/2023 order for a cough relieving medication to be administered every four hours as needed for cough. A second o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide assistance with Activities of Daily Living (ADLs) for 3 (Residents 25, 15, & 218) of 3 residents who were assessed to ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure residents with Diabetes Mellitus (DM - a condition making the regulation of Blood Glucose [BG] more difficult) received...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure residents with hearing deficits were provided the assistance they were assessed to require for 1 of 1 residents (Reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
<Resident 8>
Review of the 02/26/2024 admission MDS showed Resident 8 did not have any memory impairment, was understood, and could understand others in conversation.
Review of a 03/18/2024 Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure 2 (Residents 9 & 118) of 5 residents reviewed for unnecessary medications were free from unnecessary psychotropic drugs. Failure to d...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure expired medications were disposed of timely for 2 of 2 medication carts and 1 of 1 central supply room and medications were stored sec...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
<Resident 35>
Review of Resident 35's 04/11/2024 admission MDS showed Resident 35 had severe cognitive impairment, could understand others, and was understood in conversation. This MDS showed Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide meals that accommodated resident food preferen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
<Resident 25>
According to a 04/18/2024 Annual MDS, Resident 25 was assessed to require hospice services.
Review of Resident 25's records showed hospice notes from February, March, and April 20...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to maintain infection control practices that provided a safe and sanitary environment to help prevent the transmission of communi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure 2 of 6 residents (Residents 218 & 15) reviewed ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to consistently serve meals within the posted timeframe's for 2 of 3 hallways (100/200 Hall Dining Cart) for meals served to resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** <Uncovered Food>
Observations of 200 Hall dining services on 05/10/2024 at 1:11 PM showed staff delivering lunch trays. Th...
Read full inspector narrative →
Nov 2023
6 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to develop comprehensive person-centered Care Plans (CP) for 6 (Residents 10, 13, 19, 39, 45 & 32) of 16 residents reviewed for C...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to post the daily nurse staffing information including the total number of and actual hours worked by licensed and unlicensed nur...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to maintain a Quality Assurance and Performance Improvement program (Q...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to provide the Specialized Rehabilitative Services of Physical Therapy,...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility administration failed to obtain and use resources to manage the facility effec...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to establish and maintain an infection prevention and con...
Read full inspector narrative →
Feb 2023
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0569
(Tag F0569)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility to notify 3 (Residents 3, 24, & 26) of 4 residents reviewed, who were Medicaid recipients, when their personal fund account balances reached $1800 (i....
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 36
Review of the 12/15/2022 Quarterly MDS showed Resident 36 had multiple medically complex diagnoses. This MDS showed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide Skilled Nursing Facility Advanced Beneficiary Notices (SNF ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 3
On 02/01/2023 at 8:42 AM, Resident 3 was observed wearing compression stockings to both legs. Resident 3 stated they ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 7
According to a 01/16/2023 Annual MDS, Resident 7 did not transfer in or out of their bed or use the toilet during the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure a restorative program was developed and initiat...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure expired medications, liquid feeding supplement, medical supplies, and intravenous (IV) solution were disposed of timely for 1 of 1 cen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Resident 16
Review of a 10/03/2022 Food Preference record showed Resident 16 disliked rice and casseroles.
An observation on 02/03/2023 at 12:58 showed Resident 16 was finished with lunch and was con...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to obtain a Physician Order (PO) for hospice care, and to ensure the d...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 10
According to a 12/28/2022 Annual MDS, Resident 10 was assessed to have multiple medically complex diagnoses includin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure notification of room change was consistently provided prior ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to establish a system that ensured residents who were transferred to t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Provider Notification Outside Parameters
Resident 35
According 11/16/2022 Significant Change in Status Assessment MDS, Resident ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 10
According to a 12/28/2022 Annual MDS, Resident 10 had no cognitive impairment and had diagnoses including anxiety, d...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** REFERENCE WAC: 388-97-1320(1)(a)(c).
Glucometer
Facility Policy
Review of the updated February 2017 Disinfecting Glucometer poli...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • 65 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • Grade D (43/100). Below average facility with significant concerns.
- • 68% turnover. Above average. Higher turnover means staff may not know residents' routines.
About This Facility
What is Enumclaw Health & Rehab Center's CMS Rating?
CMS assigns ENUMCLAW HEALTH & REHAB CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Washington, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Enumclaw Health & Rehab Center Staffed?
CMS rates ENUMCLAW HEALTH & REHAB CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 68%, which is 22 percentage points above the Washington average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 71%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Enumclaw Health & Rehab Center?
State health inspectors documented 65 deficiencies at ENUMCLAW HEALTH & REHAB CENTER during 2023 to 2025. These included: 65 with potential for harm. While no single deficiency reached the most serious levels, the total volume warrants attention from prospective families.
Who Owns and Operates Enumclaw Health & Rehab Center?
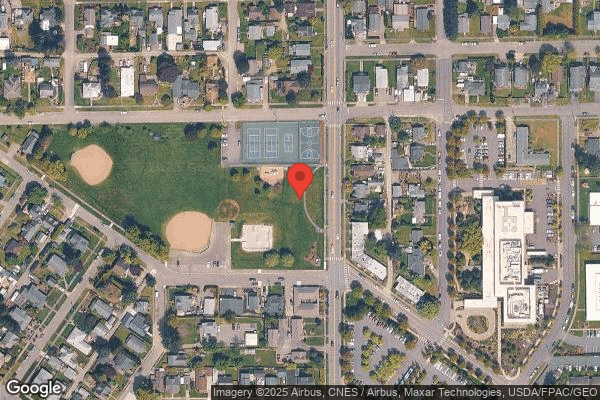
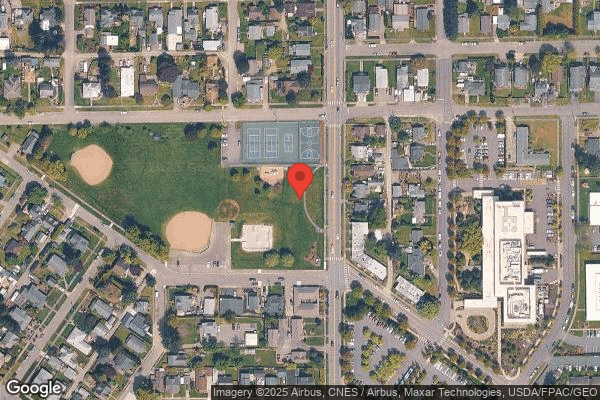
ENUMCLAW HEALTH & REHAB CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by EMPRES OPERATED BY EVERGREEN, a chain that manages multiple nursing homes. With 92 certified beds and approximately 67 residents (about 73% occupancy), it is a smaller facility located in ENUMCLAW, Washington.
How Does Enumclaw Health & Rehab Center Compare to Other Washington Nursing Homes?
Compared to the 100 nursing homes in Washington, ENUMCLAW HEALTH & REHAB CENTER's overall rating (2 stars) is below the state average of 3.2, staff turnover (68%) is significantly higher than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Enumclaw Health & Rehab Center?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's high staff turnover rate.
Is Enumclaw Health & Rehab Center Safe?
Based on CMS inspection data, ENUMCLAW HEALTH & REHAB CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Washington. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Enumclaw Health & Rehab Center Stick Around?
Staff turnover at ENUMCLAW HEALTH & REHAB CENTER is high. At 68%, the facility is 22 percentage points above the Washington average of 46%. Registered Nurse turnover is particularly concerning at 71%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Enumclaw Health & Rehab Center Ever Fined?
ENUMCLAW HEALTH & REHAB CENTER has been fined $8,018 across 1 penalty action. This is below the Washington average of $33,159. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Enumclaw Health & Rehab Center on Any Federal Watch List?
ENUMCLAW HEALTH & REHAB CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.