THE TERRACES AT SKYLINE




Inspected within the last 6 months. Data reflects current conditions.
The Terraces at Skyline has a Trust Grade of C+, which means it is slightly above average but not outstanding. It ranks #120 out of 190 facilities in Washington, placing it in the bottom half, and #26 out of 46 in King County, indicating that there are better local options available. The facility's trend is worsening, with issues increasing from 14 in 2024 to 18 in 2025. Staffing is a relative strength with a 4/5 star rating, although turnover is average at 50%. Notably, there have been no fines recorded, which is a positive sign. However, there are specific concerns that families should be aware of. For instance, the facility did not have proper Registered Nurse coverage for one day, which could compromise resident care. Additionally, there were failures in maintaining food safety standards, such as using expired sanitizing solution test strips, which could risk foodborne illnesses. On the positive side, the facility has excellent quality measures, but families should weigh these strengths against the weaknesses highlighted in the report.
- Trust Score
- C+
- In Washington
- #120/190
- Safety Record
- Low Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 50% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Washington facilities.
- Skilled Nurses ✓ Good
- Each resident gets 53 minutes of Registered Nurse (RN) attention daily — more than average for Washington. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 52 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Near Washington average (3.2)
Meets federal standards, typical of most facilities
Near Washington avg (46%)
Higher turnover may affect care consistency
The Ugly 52 deficiencies on record
Aug 2025
18 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a copy of the advance directive (a written document describi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0605
(Tag F0605)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure non-pharmacological (treating a health problem without using medications) interventions were in place for an antidepressant (medicat...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a Significant Change in Status Assessment (SCSA) Minimum Dat...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to accurately assess 1 of 15 residents (Resident 28), reviewed for res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop and/or implement a discharge care plan for 1 of 12 resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure Activities of Daily Living (ADL) assistance we...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to follow a therapeutic diet and to provide education to ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure disinfectants (cleaning products containing ch...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a Medication Regimen Review (MRR - a comprehensive assessment of resident's medications, performed by a pharmacist [a qualified prof...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure staff was provided education about COVID-19 (a viral illness that causes fever, difficulty breathing or possibly death) vaccination,...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure bed rails (bed enablers) were properly secured...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure proper storage, dating and labeling of respira...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to dispose expired medication in accordance with current...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure a detailed written description of the facility's water system was included in their water management program and/or ap...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to establish a grievance policy that designated a Grievance Official (an individual responsible for overseeing the grievance process) for 2 of...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to provide the required Registered Nurse (RN) coverage for 1 out of 30 days (08/03/2025), reviewed for staffing. This failure placed the resid...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure sanitizing solution test strips were not used after expiration date and failed to keep records of the sanitizing solut...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure infections related to initiation of antibiotic (medicine that prevents or treats infections) practices were based on the Center for ...
Read full inspector narrative →
Aug 2024
14 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure informed consent for an antidepressant (medication used to t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** RESIDENT 20
A review of Resident 20's face sheet showed they were admitted to the facility on [DATE].
A review of the medication...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide a written transfer/discharge notice to the resident and/or ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure bed hold (the opportunity to reserve a resident's current oc...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a Significant Change in Status Assessment (SCSA) Minimum Dat...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure resident-centered care and treatment were prov...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to thoroughly assess and stage a pressure ulcer (localiz...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** RESIDENT 20
A review of Resident 20's face sheet showed they were admitted to the facility on [DATE] with a diagnosis that inclu...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
SEVENTH FLOOR DINING ROOM
RESIDENT 235
Observation on 08/19/2024 at 8:56 AM, showed Staff E, LPN, checked Resident 235's blood pressure and oxygen saturation levels and then gave Resident 235 their me...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to provide the required Registered Nurse (RN) coverage for 6 of 92 days (10/07/2023, 10/08/2023, 10/15/2023, 10/21/2023, 10/22/2023 & 11/04/20...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to appropriately label/store medications/biologicals (diverse group of medicines made from natural sources) and/or medical suppl...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure expired food items were discarded after the expiration date or use by date and failed to have a working thermometer in...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** INFECTION CONTROL DURING MEDICATION PASS
A review of the facility's policy titled, Medication Administration, revised on 04/11/2...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Data
(Tag F0851)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure that direct care staffing information was submitted timely to the Centers for Medicare and Medicaid Services (CMS), for 1 of 1 quart...
Read full inspector narrative →
May 2023
20 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a copy of the Advance Directive (AD) was obtained from the r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a Notice of Medicare (national health program) Non-Coverage ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure allegations of abuse were reported to the State Agency (SA) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to identify allegations of abuse and ensure investigations were initia...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to conduct a timely significant change in status Minimum Data Set (MDS...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete and transmit resident assessment data to the Centers for M...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure residents with limited range of motion (ROM) re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure necessary respiratory care and services were p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** RESIDENT 3
Resident 3 admitted to the facility on [DATE] with a broken right arm.
Review of the comprehensive MDS assessment dat...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0729
(Tag F0729)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to obtain registry verification to ensure staff met competency evaluation requirements before allowing to serve as a nurse aide for 1 of 3 sta...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure medications were labeled and dated for 1 of 2 medication storage rooms (7th floor medication room) reviewed for medica...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents and resident representatives were provided educati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure Certified Nursing Assistants (CNAs) had the required abuse and neglect and/or dementia management training annually for 1 of 3 staff...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** RESIDENT 12
Resident 12 admitted to the facility on [DATE] with wounds to their coccyx (tailbone)/sacral (bottom of spine) and l...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** RESIDENT 329
Resident 329 admitted to the facility on [DATE].
Review of Resident 329's EHR showed no documentation that a summar...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Review of the facility policy titled, Restraint and Device dated 10/25/2017, showed that The care plan identifies the type of re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure foods stored in the refrigerator and kitchen s...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** INFECTION CONTROL SURVEILLANCE
Review of the facility's Infection Control Prevention and Control Program dated 04/03/2023, show...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed to develop and implement an antibiotic stewardship program (ASP) to promote appropriate use of antibiotics, failed to obtain/analyze and make a...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure the daily nurse staffing form was accurately posted and updated with actual hours worked for each shift for 30 out of ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • No fines on record. Clean compliance history, better than most Washington facilities.
- • 52 deficiencies on record. Higher than average. Multiple issues found across inspections.
About This Facility
What is The Terraces At Skyline's CMS Rating?
CMS assigns THE TERRACES AT SKYLINE an overall rating of 3 out of 5 stars, which is considered average nationally. Within Washington, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is The Terraces At Skyline Staffed?
CMS rates THE TERRACES AT SKYLINE's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 50%, compared to the Washington average of 46%. RN turnover specifically is 60%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at The Terraces At Skyline?
State health inspectors documented 52 deficiencies at THE TERRACES AT SKYLINE during 2023 to 2025. These included: 52 with potential for harm. While no single deficiency reached the most serious levels, the total volume warrants attention from prospective families.
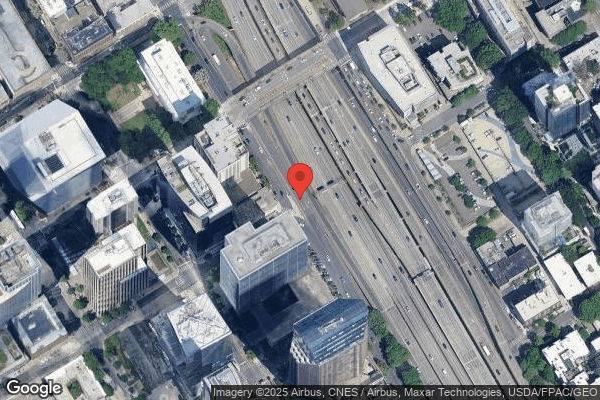
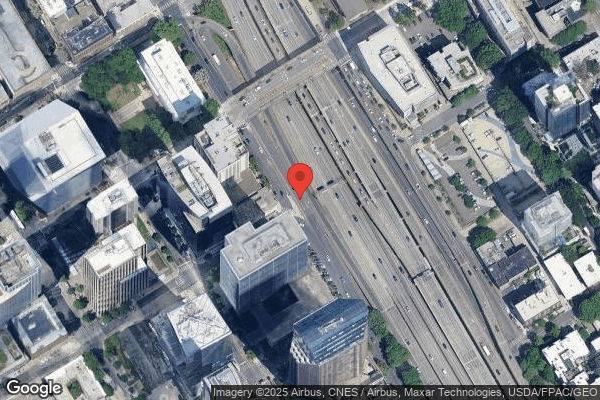
Who Owns and Operates The Terraces At Skyline?
THE TERRACES AT SKYLINE is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 34 certified beds and approximately 28 residents (about 82% occupancy), it is a smaller facility located in SEATTLE, Washington.
How Does The Terraces At Skyline Compare to Other Washington Nursing Homes?
Compared to the 100 nursing homes in Washington, THE TERRACES AT SKYLINE's overall rating (3 stars) is below the state average of 3.2, staff turnover (50%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting The Terraces At Skyline?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is The Terraces At Skyline Safe?
Based on CMS inspection data, THE TERRACES AT SKYLINE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in Washington. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at The Terraces At Skyline Stick Around?
THE TERRACES AT SKYLINE has a staff turnover rate of 50%, which is about average for Washington nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was The Terraces At Skyline Ever Fined?
THE TERRACES AT SKYLINE has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is The Terraces At Skyline on Any Federal Watch List?
THE TERRACES AT SKYLINE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.