CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a resident's smoking location was away from a ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a resident's smoking location was away from a high traffic thoroughfare, dry grassy area, and had a receptacle for disposing of lit cigarettes and ashes for 1 of 1 sampled resident (Resident 30) reviewed for smoking This failure placed all residents a risk for avoidable accidents, injuries, and the potential risk of fire.
On 07/17/2023 At 2:10 PM, the facility was notified of an immediate jeopardy (IJ) at CFR 483.25 (d)(1)(2) F689, related to the facility's failure to ensure the resident had a safe smoking environment, and all residents remained free of fire risks. The facility removed the immediacy on 07/18/2023, with onsite verification from investigators, by providing a safe smoking location on the facility property and a cigarette receptacle for the resident to dispose of cigarettes and ashes. Additionally, the facility provided education to the resident and all staff of the location and the safe disposal practice.
Findings included .
Record review of the facility's policy titled, Smoking Policy - Residents, revised on 02/24/2023, showed the following:
1.
The facility was a smoke-free campus and that included outside patios and parking lots.
2.
That smoking offsite posed risks to residents and included weather related illnesses, accidents and injuries.
3.
The facility did not consider admitting any resident who smoked.
4.
Residents considered for admission must agree in writing, to not smoke at the facility, either on or off campus.
5.
Residents were not permitted to store smoking material with them or in their rooms. Those items were to be removed from or turned over to the facility until the resident was discharged .
6.
Residents would be assessed for safe smoking upon admission to the facility. This assessment included: a resident's ability to smoke independently and safely, and the ability to safely mobilize off-campus.
Review of the National Weather Service report for 07/17/2023, showed there were Red Flag (warm temperatures, very low humidities, and stronger winds combined to produce an increased risk of fire danger) critical fire and wind warnings for Eastern [NAME].
<Resident 30>
Review of Resident 30's Electronic Health Record (EHR), showed the resident admitted to the facility on [DATE] with diagnoses to include a history of seizures, and long-term smoker. Resident 30's comprehensive assessment, dated 05/03/2023, showed the resident had no cognitive deficits. There was no signed copy of the expectations related to this facility's nonsmoking policy for Resident 30.
Record review of Resident 30's care plan, dated 05/19/2023, showed Resident 30 smoked cigarettes and that the facility was a non-smoking facility. The care plan showed Resident 30 was to retrieve and return their smoking supplies each time they left the premises.
Resident 30's Smoking Safety Evaluation, dated 06/21/2023, was conducted 57 days after admission to the facility.
Review of the facility's progress notes, dated 04/29/2023, showed Resident 30 smoked four cigarettes a day, and showed that Resident 30 used tobacco.
Record review of the progress notes, dated 05/06/2023, showed Resident 30's cigarettes were in the medication cart. The note further showed Resident 30 knew they had to do the following: get cigarette supplies from medication cart, sign out, go off property, and return smoking supplies to the nurse upon return.
Record review of the facility's progress notes, dated 05/24/2023 and 06/01/2023, showed Resident 30 smoked cigarettes and continued to smoke.
Observation and interview on 07/17/2023 at 10:12 AM, showed a cigarette carton was located on Resident 30's bedside table and contained cigarette butts. Resident 30 stated that they smoked off grounds in front of the facility. Resident 30 said their smoking supplies were kept in the nurse's cart.
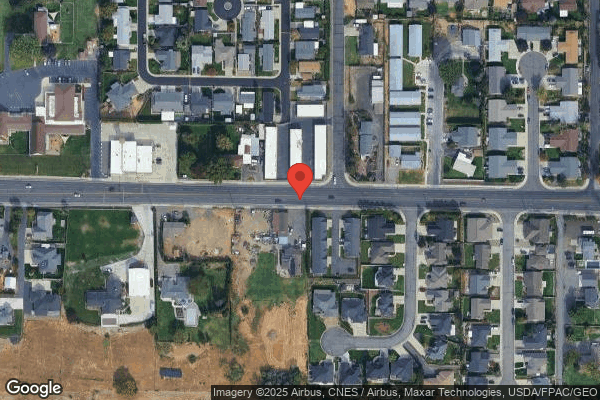
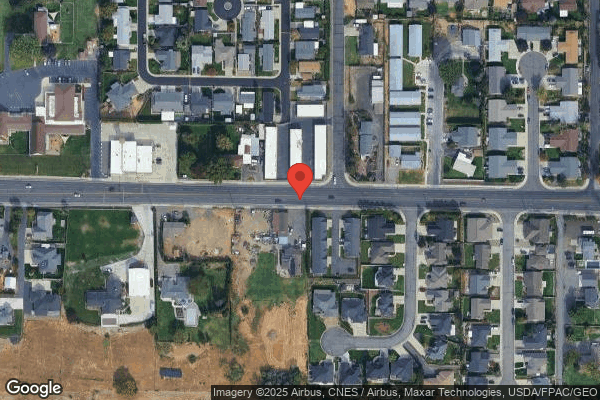
Observation and interview on 07/17/2023 at 11:20 AM, showed Resident 30 sat on their walker on the sidewalk parallel to a busy street near an intersection, with the rear wheels of their walker on dry grass. The roadway was busy with traffic in both directions. There were 30 plus cigarette butts in the area, about the size of 10 feet by 10 feet, on the dry grass behind where Resident 30 sat. Across the driveway there was another place that was a low, grassy and dry, leafy area about 3 feet by 3 feet in size and contained about 8 cigarette butts. Resident 30 stated that they sat there because there was no place on the property for them to smoke. Resident 30 said they flicked their ashes as they smoked, put the cigarette butts out on the metal of their walker and put the cigarette butts in an empty cigarette package. Resident 30 said they took the package of cigarette butts into the facility. Resident 30 further stated that they did not know this was a nonsmoking facility prior to being admitted .
During an interview on 07/17/2023 at 1:13 PM, Staff P, Licensed Practical Nurse, said Resident 30 signed themselves out when they wanted to smoke and obtained their supplies from the nurse. Staff P showed the surveyor Resident 30's smoking supplies which were on the cart, and they matched the cigarette butts found outside.
During an interview on 07/20/2023 at 12:51 PM, Resident 30 stated that they began to smoke cigarettes four to five days after they were admitted to the facility. Resident 30 said their smoking supplies were kept in the nurse's cart and that they were not allowed to keep those items in their room. Resident 30 stated that when they wanted to smoke, they got their supplies from the nurse, signed out, went out to smoke, signed in, and turned their supplies into the nurse. Resident 30 stated that they were not allowed to smoke in the employee smoking area and was told by facility staff they had to go off the property. Resident 30 further said staff told them that the sidewalk was considered off grounds.
During an interview on 07/18/2023 at 4:22 PM, Staff A, Administrator, stated that they were aware Resident 30 was signing out and going to the edge of the sidewalk near the street to smoke. Staff A further stated that there were limited places for the residents who smoked to leave the property as the facility was a non-smoking facility.
Reference: WAC 388-97-1060 (3)(g)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to provide a dignified dining experience during two of two...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to provide a dignified dining experience during two of two dining observations. On 07/16/2023, during the lunch service, the facility failed to provide meals to all residents at a table at the same time for 6 residents (Residents 33, 9, 15, 47, 31 and 1) who waited 10 minutes after Resident 42 and Resident 27 were served; and the facility failed to ensure 1 of 3 staff (Staff G) observed talked with the resident for whom they were providing assistance rather than conducting social conversations with other staff, Staff G fed Resident 33 without engaging the resident and had a conversation with Staff L, NA, that did not include the residents. On 07/19/2023 during dinner service, the facility failed to provide meals to all residents at a table at the same time for 4 o4 residents (Residents 5, 7, 32, and 55.) This failure placed residents at risk to feel diminished and disrespected.
Findings included .
Review of CMS §§483.10(a)-(b)(1)&(2) for dignity while dining and the Dining Observation pathway in the Long Term Care Survey Process dated 01/2018 showed the facility promotes resident independence and dignity while dining by serving all of the resident at a table at the same time, staff talk with the resident while they are providing assistance, and staff refrain from social conversations with other staff.
Review of the Dining Observation pathway in the Long Term Care Survey Process dated 01/2018 showed the facility promotes resident independence and dignity while dining by serving all of the resident at a table at the same time, staff talk with the resident while they are providing assistance, and staff refrain from social conversations with other staff.
Resident 33. Review of the resident's medical record showed they were admitted to the facility on [DATE] with diagnoses to include dementia (a loss of mental ability severe enough to interfere with normal activities of daily living) and anxiety disorder (the mind and body's reaction to stressful, dangerous, or unfamiliar situations). Review of the 04/13/2023 comprehensive assessment showed the resident had severe cognitive impairment and needed extensive assistance with eating meals (their meals fed by staff.)
Resident 9. Review of the resident's medical record showed they were admitted to the facility on [DATE] with diagnoses to include dementia and aphasia (a condition characterized by either partial or total loss of the ability to communicate verbally or using written words). Review of the 07/03/2023 comprehensive assessment showed the resident had severe cognitve impairment and needed extensive assistance with eating meals.
Resident 15. Review of the resident's medical record showed they were admitted to the facility on [DATE] with diagnoses to include dementia, Multiple Sclerosis (a potentially disabling disease of the brain and spinal cord) and Parkinson's Disease (a progressive disorder that affects the nervous system and the parts of the body controlled by the nerves). Review of the 05/03/2023 comprehensive assessment showed the resident had intact cognition and required one staff to assist with meals.
Resident 47. Review of the resident's medical record showed they were admitted to the facility on [DATE] with diagnoses to include dementia, aphasia, and an anxiety disorder. Review of the 06/05/2023 comprehensive assessment showed the resident had severe cognitive impairment and needed extensive assistance with eating meals.
Resident 31. Review of the resident's medical record showed they were admitted to the facility on [DATE] with diagnoses to include Alzheimer's Disease (a common form of dementia, believed to be caused by changes in the brain, usually beginning in late middle age, characterized by memory lapses, confusion, emotional instability, and progressive loss of mental ability), aphasia and stroke (when the blood supply to part of the brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients). Review of the 04/20/2023 comprehansive assessment showed the resident had severe cognitive impairment and needed extensive assistance with eating meals.
Resident 1. Review of the resident's medical record showed they were admitted to the facility on [DATE] with diagnoses to include dementia and aphasia. Review of the 05/03/2023 comprehensive assessment showed the resident had severe cognitive impairment and needed extensive assistance with eating meals.
Resident 42. Review of the resident's medical record showed they were admitted to the facility on [DATE] with diagnoses to include dementia. Review of the 06/10/2023 comprehensive assessment showed the resident had severe cognitive impairment and needed extensive assistance with eating meals.
Resident 27. Review of the resident's medical record showed they were admitted to the facility on [DATE] with diagnoses to include dementia and stroke. Review of the 06/13/2023 comprehensive assessment showed the resident had moderate cognitive impairment and limited meal assistance with staff supervision and meal set up.
<Lunch Observation>
Observaton on 07/16/2023 at 11:55 AM, during lunch in the dining room, Resident 42 was served their meal at a table with three other residents, (Resident 15, Resident 9, and Resident 33). The remaining residents were served at 12:07 PM (12 minutes later).
On 07/16/2023 at 11:55 AM, during lunch in the dining room, Resident 27 was served their meal at a table with three other residents, (Resident 47, Resident 31, and Resident 1). The remaining residents were served their lunch at 12:07 PM (12 minutes later).
During the lunch meal at 12:10 PM, Staff G, Nursing Assistant (NA) was seated to the left of Resident 33 and fed them their meal without telling the resident what they were eating. The staff would raise the spoon in front of the resident's lips and the resident would open and take the spoon of food in their mouth. Staff G continued feeding the resident without speaking to them; however, Staff G was having a conversation with Staff L, NA, also seated at the table and feeding another resident.
<Dinner Observation>
Observation on 07/19/2023, at 5:03 PM, showed Residents 5, 7, 32 and 55 sat at the same dining room table waiting for dinner. Residents 5 and 32 received their meals at 4:50 PM. Resident 55 received their meal ten minutes later at 5:00 PM. Resident 7 received their meal a total of sixteen minutes later at 5:06 PM.
On 07/21/2023 at 2:48 PM, Staff B, Director of Nursing, stated they expected the staff to talk with the residents their are feeding and no carry conversatons with other staff that the residents were not included. They stated they were not aware of all residents being served at the same time, but it made sence.
Reference: WAC 388-97-0180 (1-4)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to protect the personal privacy for 2 of 3 residents (Res...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to protect the personal privacy for 2 of 3 residents (Resident 40, and 31) observed for urinary catheter (a hollow, partially flexible tube that collects urine from the bladder and leads to a drainage bag) care or incontinent care. This failure placed the resident at risk for loss of the right to personal privacy.
Findings included .
Record review of the facility's policy titled, Catheter Care (a process to clean a urinary catheter tube where it exits the body), dated 07/10/2023, showed that staff were to provide privacy, cover the resident with a sheet, exposing only the perineal (the area of the body between the anus and the genitals) area.
Record review of the facility's undated resident admission Packet showed that the resident had the right to personal privacy that included personal care.
Resident 40. Review of the resident's medical record showed they were admitted to the facility on [DATE] with diagnoses to include obstructive uropathy (condition where urine flow has been partially or completely blocked), Urinary Tract Infection (UTI, infection of any part of the urinary system) and dementia (a loss of mental ability severe enough to interfere with normal activities of daily living). Review of the 06/24/2023 comprehensive assessment showed the resident had severe cognitive impairment and required extensive staff assistance for activities of daily living.
During a concurrent observation and interview on 07/17/2023 at 10:10 AM Staff F, Nursing Assistant (NA), was observed to provide catheter care for Resident 40. The resident was in a private room with the head of their bed right next to the door opening, there was a privacy curtain hanging on a track near the head of the bed. The NA did not pull the privacy curtain to block view of the resident's body should the door open during the procedure. During the care, Staff F pulled down the sheets to the resident's knees and opened the resident's brief to expose their genitals. After the catheter care was finished, Staff F left the resident's genitals exposed when they left the side of the bed to obtain a clean brief.
Resident 31. Review of the resident's medical record showed they were admitted on [DATE] with diagnosis to include Alzheimer's disease (a brain disorder that slowly destroys memory and thinking skills and eventually, the ability to carry out simple tasks), and a stroke (occurs when something blocking of blood supply to part of the brain or when a blood vessel in the brain bursts). Review of the comprehensive assessment, dated 04/20/2023, showed the resident had severe cognitive impairment and required extensive assistance of two staff members for all activities of daily living.
During a concurrent observation and interview on 07/19/2023 at 10:48 AM, Staff DD, NA, and Staff CC, Licensed Practical Nurse, stated that they had a new order for an air mattress to alternate resident while in bed. Staff DD had pulled the curtain for privacy, the curtain length was above the resident bed, exposed the head of the bed that was next to the door and did not cover the foot of the bed where their roommate resided. Both staff members proceeded with the dressing change and did not notice that the curtain did not cover the resident's care area or give them privacy during the dressing change. During the dressing change someone opened the resident's room door and quickly shut the door. Staff DD stated that they did not notice that the curtain was so short and that they would have to talk with housekeeping about a different curtain.
During an interview on 07/20/2023 at 3:48 PM Staff B, Director of Nursing (DON) stated that the expectation would be the nurse to provide privacy for all cares.
During a follow up interview on 07/21/2023 at 2:39 PM, Staff B stated that the privacy curtain should have been closed by the staff during catheter care and staff should not have left them exposed when getting supplies.
Reference: WAC 388-97-0360 (1)(d)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure three of the seven required components (identif...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure three of the seven required components (identification, investigation, and reporting) in of the prevention of abuse and neglect policy were consistently implemented for 2 of 4 residents (Residents 26 and 213) reviewed for abuse/neglect. This failure prevented the facility from identifying the extent and nature of the occurrence, interview all individuals involved, and placed the residents at risk for unidentified abuse and/or neglect.
Findings included .
Review of the facility's policy, titled Abuse, Neglect, Mistreatment and Misappropriation of Resident Property, dated 09/21/2022, showed the facility would .identify and assess all possible incidents of abuse .Investigate and report any allegations of abuse .
Resident 213. Review of the resident's Electronic Health Record (EHR) showed, the resident was admitted to the facility on [DATE] with diagnoses to include an infection in their urine, and alcoholism (any drinking of alcohol that results in significant mental or physical health problems).
Review of the resident's 07/06/2023 baseline care plan showed the resident was alert, oriented, and able to make their needs known.
During a concurrent observation and interview, on 07/16/2023 at 11:18 AM, Resident 213 stated a few days ago they had an incontinent episode and used their call light for assistance to get cleaned up. Resident 213 stated a caregiver abruptly entered the room, and began tossing their personal belongings (purse, bag, and cellular phone) they had with them on the bed, to the side and the bottom of the bed. The caregiver then tossed their cords (cellular charging and call light) off of the bed, where they fell onto the floor in between the wall and the bed. The resident identified Staff H, Nursing Assistant (NA), as the caregiver. The resident further stated they reported the incident to the head staff during their care conference and informed them they no longer wanted that caregiver providing care for them.
Review of the facility's Incident Reporting Log, dated 07/05/2023 to 07/17/2023, showed no incident/investigation had been logged for the allegation above.
Review of the facility's Grievance/Concern Log, dated 07/06/2023 to 07/17/2023, showed no grievance had been logged for the allegation made by Resident 213.
During an interview, on 07/18/2023 at 2:57 PM, with Staff B, Director of Nursing (DON), along with Staff A, Administrator, Staff B stated that they did not investigate the allegation by Resident 213 because I seen that as more of a customer concern rather than an allegation of abuse. Staff B further stated the customer's concern was written up as a grievance. Review of the grievance report showed Staff B's signature.
Review of the grievance report, dated 07/12/2023, showed Resident 213 reported they felt like an aide had thrown [Resident 213] belongings when helping [Resident 213] in bed. The grievance further showed a statement made by Staff H, NA, that Resident 213 had gotten upset with them because they accidentally dropped their charger on the floor and claimed they had thrown their stuff around. [Resident 213] was also calling me names.
Resident 26. Review of the resident's EHR showed, the resident admitted to the facility on [DATE] with diagnoses to include depression and a disorder that caused muscle weakness and possible loss of muscle function.
The most recent quarterly assessment, dated 05/19/2023, showed the resident's cognition was moderately impaired and required extensive assistance of two staff members for activities of daily living (ADL's) except for eating.
During an interview on 07/16/2023 at 10:50 AM, Resident 26 stated that there was a care staff member that was mean and yelling at me.
Review of the facility's Incident Reporting log, dated 07/05/2023 to 07/17/2023, showed no incident/investigation had been logged for the allegation above from Resident 26.
Review of the facility's Grievance/Concern Log dated 06/07/2023 to 06/27/2023, showed the alleged abuse allegation was logged as a customer service issue on 06/27/2023.
During an interview on 07/18/2023 at 12:57 PM, Staff B, stated that they had ruled out the incident with Resident 26 and Staff J, NA, as a customer service issue, not an allegation of abuse.
During an interview on 07/19/2023 at 12:38 PM, with Resident 26's Representative (RR), they stated the incident happened on 06/23/2023. The RR further stated when they came in to visit Resident 26, the resident was very upset and crying. The resident told them that their NA yelled at them for not asking the Restorative Aide to toilet the resident and that any NA could do that, the resident did not need to call them to do it. Additionally, that the resident did not want to talk about what happened, they explained to the resident that they could not help with the problem if they did not know what happened. The resident representative identified Staff J as the alleged perpetrator.
During an interview on 07/19/2023 at 12:38 PM, with Resident 26's RR, stated that they reported Staff J and the allegation to Staff C LPN/ADON who did not recognize an allegation of verbal abuse and wrote out a grievance form that had been forwarded to the Director of Nursing.
During an interview on 07/21/2023 at 8:40 AM, Staff B stated they did not realize that Resident 26 was upset and crying. Staff B acknowledged that the grievance was an allegation of abuse and stated they would be working on an investigation right away.
During an interview on 07/22/2023 at 11:22 AM, Staff A stated the expectation was to immediately report to the State Agency, notify Administration, and to begin the investigation. Staff A's expectation from staff was to protect the resident, stay with the resident, call the nurse or administrative staff. Staff A stated that staff needed to ensure to protect, report, to investigate and notify the representative and physician. Staff A also expected staff to document on the reporting log and follow that guidance.
WAC Reference: 388-97-0640 (1) (2)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to issue a written transfer notice to a resident and/or legal represen...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to issue a written transfer notice to a resident and/or legal representative and to the state Ombudsman for 2 of 3 residents (Resident 49 and 59) reviewed for hospitalizations. This failure placed residents at risk of not being informed of their condition, unmet care needs and a diminished quality of life.
Findings included .
Record review of the facility's policy titled, Transfer/Notification of Ombudsman, dated 07/2023, showed residents will be given written transfer information and reason for the transfer upon leaving the facility if they are able to understand the information. If hospitalized and they are unable to understand or family is not able to be reached, the admission Coordinator will visit the resident in the hospital the next day to review the reason for the discharge. The social service department will be responsible for notifying the state ombudsman office of all of the discharges and transfers out to include discharge to hospital .
Resident 49. Electronic Health Record (EHR) review showed the resident was admitted to the facility on [DATE]. Review of the 06/23/2023 comprehensive assessment showed the resident had severe cognitive impairment.
Review of a nursing progress note dated 05/18/2023 at 2:44 PM showed that Resident 49 was transported to the emergency department from a medical appointment due to a rapid change in level of consciousness and they were then admitted to the hospital with diagnoses of hypotension (a blood pressure reading below the specified limit (90/60 mmHg (millimeters of mercury), normal is 120/70 mmHg) and can cause dizziness, blurred vision and tiredness) and a urinary tract infection (Infection of any part of the urinary system).
EHR review showed no transfer/discharge notice was given to the resident or their representative for Resident 49's discharge to the hospital.
During a telephone interview on 07/19/2023 at 2:00 PM, Resident 49's representative stated they were notified by the facility when the resident was transported to the emergency department; however, no written notice of transfer was provided to them.
Resident 59. Review of the resident's EHR showed they were admitted to the facility on [DATE] with diagnoses including recent stroke (a condition in which blood supply is cut off to the brain) and dysphagia (inability to safely swallow).
Review of a progress note, dated 07/12/2023, showed the resident's gastrostomy tube (GT, a tube inserted into the abdomen to receive fluids and nutrition) had become dislodged. The physician was notified, and the resident was sent to the hospital to have the GT re-inserted.
Further review of the EHR showed no evidence of a transfer/discharge notice had been given to the resident or their representative when transferred/discharged to the hospital on [DATE].
During an interview on 07/20/2023 at 12:52 PM Staff O, Admissions Coordinator, stated they were aware of the facility policy for them to deliver transfer/discharge notices to residents in the hospital, but they had not been asked to do so for about a year.
During an interview on 07/20/2023 at 1:27 PM, Staff E, Social Services Director, stated they had not been involved in any Ombudsman notification.
During an interview on 07/20/2023 at 3:00 PM, Staff R, Registered Nurse, stated months ago when they worked the evening shift, they would fill out the paperwork related to transfer to the hospital, call the family and discuss the bed hold; however, they did not recall giving the resident or representative copies of the notice.
During an interview on 07/21/2023 at 8:44 AM, Staff A, Administrator, stated the facility had not been following the policy requirements for resident written discharge/transfer notices or sending the notice to the state ombuds.
Reference: WAC 388-97-0120(2) (a-d)
This is a repeat citation from the Statement of Deficiencies dated 06/16/2022.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide a written bed-hold notice, at the time of transfer or withi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide a written bed-hold notice, at the time of transfer or within 24 hours of transfer to the hospital, for 2 of 3 Residents (Resident 49 and 59), reviewed for hospitalization. This failure placed the resident or their representative at risk for a lack of knowledge regarding their right to hold their bed while in the hospital.
Findings included .
Record review of the facility's policy titled, Bed-Holds and Returns, dated 07/2023, showed all resident will be given transfer / bed hold information upon leaving the facility if they are able to understand the information. If they are unable to understand or family is not able to be reached, the admission coordinator will visit the resident in the hospital the next day to review the hold policy.
Record review of the facility's undated resident admission Packet showed for bed holds and readmission the facility will hold the resident's bed at no charge for up to 24 hours. Should the resident wish to have their bed held beyond these 24 hours they must notify the facility before the 24 hours has passed. The cost for holding the bed is 75% to the private room and board rate per day.
Resident 49. Electronic Health Record (EHR) review showed the resident was admitted to the facility on [DATE]. Review of the 06/23/2023 comprehensive assessment showed the resident had severe cognitive impairment.
Review of a nursing progress note dated 05/18/2023 at 2:44 PM showed that Resident 49 was transported to the emergency department from a medical appointment due to a rapid change of condition and they were then admitted to the hospital.
Review of the EHR showed no documentation that a bed hold notice was given to the resident or their representative for Resident 49's discharge to the hospital.
During a telephone interview on 07/19/2023 at 2:00 PM, Resident 49's representative stated they were notified by the facility when the resident was transported to the emergency department; however, no bed hold policy discussed, nor did they receive a copy.
Resident 59. Review of the resident's EHR showed they were admitted to the facility on [DATE] following a recent stroke (a condition in which blood flow is cut off from the brain) and dysphagia (impaired swallowing ability).
Review of a progress note dated 07/12/2023 showed the resident was sent to the hospital to have their gastrostomy tube (GT, a tube inserted into the abdomen to receive fluids and nutrition) re-inserted.
Additional review of Resident 59's progress notes after returning to the facility on [DATE] did not show evidence that Residnt 59 had been given a Bed Hold Policy.
During an interview on 07/20/2023 at 3:43 PM, Resident 59 stated they did not remember recieving a Bed Hold Policy when they discharged back to the hospital on [DATE].
During an interview on 07/20/23 at 12:52 PM Staff O, Admissions Coordinator, stated they were aware of the facility policy for them to deliver bed hold notices to residents in the hospital, but they had not been asked to do so for about a year.
During an interview on 07/20/2023 at 2:55 PM, Staff Q, Business Office Manager, stated the bed hold policy was within the transfer out packet and the nurses fill them out, obtained signatures and the completed form should be uploaded into the resident's electronic health record.
During an interview on 07/20/2023 at 3:00 PM, Staff R, Registered Nurse, stated months ago when they worked the evening shift, they would fill out the paperwork related to transfer to the hospital, call the family and discuss the bed hold; however, they did not recall giving the resident or representative copies of the notice.
During an interview on 07/21/2023 at 8:44 AM, Staff A, Administrator, stated the facility had not been following the policy requirements for resident bed hold notices at the time of discharge to the hospital.
Reference: WAC 388-97-0120(4)(a)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to accurately assess 3 of 5 residents (Residents 49, 17, ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to accurately assess 3 of 5 residents (Residents 49, 17, and 20) whose Minimum Data Sets (MDS - an assessment tool) were reviewed. Failure to ensure accurate assessments related to Vision (Residents 49 and 17) and Communication (Resident 20), placed residents at risk for unidentified and/or unmet needs.
Findings included .
<Vision>
Resident 49. Electronic Health Record (EHR) review showed the resident was admitted to the facility on [DATE] with diagnoses to include Diabetes Mellitus (a metabolic disorder in which the body has high sugar levels for prolonged periods of time). Review of the 06/23/2023 Minimum Data Set comprehensive assessment showed the resident had adequate vision (sees fine detail, such as regular print in newspapers/books), did not have corrective lenses and had moderate cognitive impairment. Review of the preference section of the MDS showed Resident 49 indicated it was somewhat important to have stuff to read.
During an observation and interview on 07/17/2023 at 8:54 AM, Resident 49 was in bed with the head of bed elevated. There were several facility handouts on the resident's overbed table that included activities and the next day meal menu. Resident 49 stated they could not see writing that small and they had glasses at home.
Review of Resident 49's MDS assessments, dated 04/11/2023 and 05/30/2023, also indicated the resident had adequate vision and did not have corrective lenses. The assessments were completed by Staff W, Licensed Practical Nurse and MDS Coordinator.
Resident 17. Review of the resident's EHR showed the resident was admitted to the facility on [DATE] with diagnoses including, pulmonary fibrosis (lung condition which causes thickening and scarring of the lung) and liver disease.
Review of the most recent comprehensive assessment, dated 07/07/2023, showed the resident was cognitively intact and had adequate vision to read regular print.
During an interview on 07/19/2023 at 3:15 PM, Resident 17 stated they had very poor vision related to cataracts (occurs when the lenses of the eye becomes cloudy and impairs vision) and they had trouble reading regular print.
Record review of the vision assessment section of the Resident Assessment Instrument (RAI) manual (an assessment tool used to gather definitive information of a resident that must be addressed in an individualized care plan) dated 10/2019 showed the instructions to assess a resident's vision included asking the resident to look at regular-sized print in a book or newspaper and ask the resident to read aloud.
During an interview on 07/21/2023 at 2:55 PM Staff B, Director of Nursing, stated Staff W, License Practical Nurse (LPN) worked remotely to complete the MDS assessments, did not come to the facility and had Staff N, Nursing Assistant/Restorative Aide assist with the resident hands on assessments using video conference.
During an interview on 07/21/2023 at 03:11 PM, Staff N stated they assisted Staff W with resident bedside assessments using conference zoom on a computer. Staff N stated that Staff W would ask the resident about their pain, hearing and if they had dentures. Staff N stated there were no assessments of the resident's vision.
During a telephone interview on 07/21/2023 at 3:19 PM, Staff W, stated their process of completing the MDS remotely was no different than in person or over Zoom. I do my interview with [Staff N]'s help by phone or Zoom. When asked about how they accomplished the hands-on assessments, Staff W stated, which ones, I don't know of that assessment? Staff W was directed to Resident 49's 06/23/2023 MDS and the resident was assessed to have adequate vision and no corrective lenses. Then to the vision section of the RAI manual gave instructions to assess a resident's vision. Staff W stated during their interview with Resident 49, [they] did not have glasses on and the resident did not express that they had difficulty reading. Staff W stated that they did not assess Resident 49's vision. Further Staff W stated No, I am not asking them to read anything.
<Communication>
Resident 20. Review of the resident's EHR showed the resident was admitted to the facility on [DATE] with multiple diagnoses to include expressive aphasia (a condition where a person may understand speech, but they have difficulty speaking fluently themselves).
Review of the 01/23/2023 and 04/22/2023 MDS/comprehensive assessments, showed the resident had clear speech and could speak distinct intelligible words. The assessments further showed the resident usually made himself understood (difficulty communicating some words or finishing thoughts but is able if prompted or given time).
During an interview on 07/16/2023 at 10:35 AM, Resident 20 was unable to answer the surveyors interview questions in detail. The resident was able to nod their head yes or no (up/down for yes, and side to side for no) and was able to gesture or point to an object if they wanted it. When asked if they had family that they would like me to speak with instead, the resident nodded their head up and down, indicating yes.
During an interview on 07/17/2023 at 11:17 AM, Resident 20's Representative (RR 20), stated the resident had been non-verbal for several years and staff were to use simple yes and no questions when communicating with them. RR 20 further stated the resident used to use a picture board but refused to use it anymore.
During an interview on 07/18/2023 at 4:05 PM, Staff T, Hospitality Aide, stated Resident 20 did not speak and when they spoke to the resident they would talk slowly, point, and ask simple questions. Resident was able to respond by pointing or nodding their head yes or no.
During an interview on 07/19/2023 at 1:23 PM, Staff U, Nursing Assistant (NA), stated when speaking to Resident 20 they would ask simple questions until I find the right need that [Resident 20] wants, then they will respond with a head nod yes or no, takes a while because you have to point and ask a lot of things before you know what [Resident 20] wants. Staff U further stated the resident did not verbally respond, and they have attempted to use a picture board for communicating but the resident refused to use it.
During an interview on 07/19/2023 at 1:27 PM, Staff V, NA, stated Resident 20 does not talk and I will ask questions and hand gestures related to what I think he might need until [Resident 20] nods yes or no.
During an interview on 0/21/2023 at 4:46 PM, Staff B, stated that the expectation was that the MDS/comprehensive assessments were to be accurate.
Reference: WAC 388-79-1000(1)(b)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 26. Review of the resident's EHR showed the resident admitted to the facility on [DATE] with diagnoses to include and m...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 26. Review of the resident's EHR showed the resident admitted to the facility on [DATE] with diagnoses to include and muscle wasting. The record further showed no PASARR had been completed for Resident 26 since admission.
Review of the comprehensive assessment, dated 05/19/2023, showed the resident's cognition was moderately impaired. The assessment further showed the resident had little interest in doing things, felt tired and had little energy, and felt bad about themselves.
During an interview on 07/20/2023 at 4:28 PM, Staff E stated that Resident 26 had come from home and an outside mental health provider stated that they were going to fill out a PASARR for the resident. The resident was admitted four months ago and still had no PASARR. Staff E further stated the resident was admitted in February 2023 and that they were responsible for review and completion of the PASARRs and would start working on Resident 26's.
WAC Reference: 388-97-1975 (1)(2)(4)
Based on interview and record review, the facility failed to review the Pre-admission Screening and Resident Review (PASARR, a tool used to identify if a person may have an intellectual disability (ID) or related condition (RC), or a serious mental illness [SMI]) for accuracy upon admission for 1 of 6 residents (Resident 7) reviewed for PASARR services. Additionally, the facility failed to ensure a resident received a PASARR Level I ( an inital assessment to determine whether an individual might have (SMI) or (ID)) which was required prior to admission to the facility. This failure placed the residents at risk for unidentified mental health needs.
Findings included .
Resident 7. Review of the Electronic Health Record (EHR) showed the resident admitted to the facility on [DATE] with multiple serious mental health diagnoses to include dementia (impaired ability to remember, think, or make decisions that interferes with doing everyday activities), paranoid schizophrenia (a pattern of behavior where a person feels distrustful and suspicious of other people and acts accordingly, delusions and hallucinations are two off those symptoms), bipolar disorder (a serious mental illness that causes unusual shifts in mood, ranging from extreme highs to lows), depression ( a mood disorder that causes a persistent feeling of sadness and loss of interest and can interfere with your daily activities of life), anxiety (a disorder that causes episodes of intense, excessive, and persistent worry and fear about everyday situations), personality disorder (a mental health condition where people have a lifelong pattern of seeing themselves and reacting to others in ways that cause problems) and a delusional disorder ( a belief or altered reality that is persistently held despite evidence or agreement to the contrary).
Review of Resident 7's comprehensive assessment, dated 07/02/2023, showed the resident's cognition was moderately impaired.
Review of the Resident's PASARR, dated 08/09/2022, showed the resident had no diagnosis of dementia and the only Serious Mental Illness diagnosis identified was schizophrenia.
During an interview on 07/21/2022 at 10:00 AM, Staff E, Social Services Director (SSD), stated they were responsible for ensuring the accuracy of the PASARR's prior to admission, then again quarterly and as needed. Staff E stated when a PASARR was received from the hospital, they reviewed and made any changes that were needed and then would have made a referral for specialized services as needed. Staff E further stated, I could use some training on them (PASARRs).Staff E additionally stated, the PASARR for Resident 7 was identified as incorrect on their quarterly assessment of 07/02/2023 but had no time to correct it since then. I definitely believe the resident would require specialized services if the assessment had been completed accurately.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to implement a Care Plan related to wearing a hearing aid...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to implement a Care Plan related to wearing a hearing aid for 1 of 1 sampled residents (Resident 14). This failure resulted in Resident 14 having unmet care needs and was at risk for a diminished quality of life.
Findings included .
Resident 14. Review of the 05/25/2023 comprehensive assessment showed that the resident was admitted to the facility with diagnosis including Anxiety and hemiparesis ( partial / complete loss of strength to one side of the body), and the resident's cognition was moderately impaired.
Observation on 07/16/2023 at 9:14 AM, showed Resident 14 sat in their wheelchair watching television (TV). Resident 14 could not hear the surveyor during the survey screening process. When asked if they wore hearing aids, Resident 14 did not answer. Resident 14's roommate said Resident 14's hearing aid was at the nurse's station.
Observation and interview on 07/17/2023 at 8:59 AM, showed Resident 14 was not wearing their hearing aid and said the nurse had it. Resident 14 stated that sometimes they have a hard time hearing the TV and turns the volume up. Resident 14 said the facility made them turn their TV down because it was too loud for their roommate.
Observation on 07/18/2023 at 2:39 PM, showed Resident 14 did not have their hearing aid on. Resident 14's TV was on and at a low volume. Resident 14 sat in their wheelchair watching the Entertainment Channel.
Observation on 07/18/2023 at 3:24 PM, showed Resident 14 did not have their hearing aid on. Resident 14's TV was on and at a low volume. Resident 14 sat in their wheelchair watching an older movie on TV.
Observation on 07/19/2023 at 11:05 AM, showed two nursing assistance helped Resident 14 get out of bed and exit the room in their wheelchair. Resident 14 did not have their hearing aid on.
Observation on 07/19/2023 at 1:36 PM, showed Resident 14 did not have their hearing aid on. Resident 14 sat in their wheelchair and looked at the TV screen. The TV volume was low.
Observation on 07/19/2023 at 5:08 PM, showed Resident 14 sat at a table in the dining room eating their dinner. Resident 14 did not have their hearing aid on.
Record review of Resident 14's Minimum Data Set, dated [DATE], showed Resident 14 was able to hear, with minimal difficulty, when they wore a hearing aid.
Record review of Resident 14's Care Area Assessment, dated 07/19/2023, showed Resident 14 had impaired hearing due to hearing loss. The assessment further showed Resident 14 was able to hear with minimal difficulty when they wore a hearing aid.
Record review of Resident 14's Care Plan, dated 04/02/2023, showed Resident 14 had a hearing loss in their right ear. The Care Plan further showed Resident 14's hearing aid was to be put on their right ear in the morning and removed at bedtime.
During an interview on 07/19/2023 at 3:21 PM, Staff Z, Licensed Practical Nurse, stated that Resident 14 had a hearing aid, and they wore it. Staff Z stated that Resident 14's hearing aid was put on their ear in the morning, and that they takes it off at bedtime and put it in a case on the medication cart. Staff Z took the case out of the medication cart, opened it, and Resident 14's hearing aid was in the case.
During an interview on 07/19/2023 at 3:43 PM, Staff Y, Nursing Aide Certified, stated that Resident 14 had a hearing deficit and when they talked to Resident 14, they did not understand what Staff Y said. Staff Y stated that Resident 14 had a hearing aid and when they wore it, they could hear pretty well. When Resident 14 did not wear it, they had trouble hearing. Staff Y stated that Resident 14's hearing aid was either on their ear or the nurses had it. Staff Y stated that it would be difficult for Resident 14 to hear their TV if they did not have their hearing aid on. Staff Y stated that Resident 14 stayed in their room and watched TV.
During an interview on 07/20/2023 at 1:16 PM, Staff B, Director of Nursing, stated that they expected staff to provide Resident 14 with their hearing aid according to their Care Plan.
Reference: WAC 388-97-1020(1), (2)(1)(b)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure that 2 of 5 residents (Resident's 59 and 6) revi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure that 2 of 5 residents (Resident's 59 and 6) reviewed for dental care received goods and services to maintain their ability to perform oral care. The facility did not ensure the resident's oral care equipment was consistently set up for the residents to participate in this aspect of Activities of Daily Living (ADLs, activities related to personal care). This failure placed residents at risk for unmet care needs and a deterioration in their oral health status.
Findings included .
Resident 59. Review of the residents Electronic Health Record (EHR) showed the resident was admitted to the facility on [DATE] with diagnosis of a recent stroke (a condition in which the blood supply is cut off from the brain). As a result of the stroke the resident had left sided weakness and dysphagia (impaired ability to swallow).
Review of Resident 59's most current comprehensive assessment, dated 07/05/2023, showed the resident was cognitively intact and required assistance for personal hygiene which included oral care.
Review of the resident's care plan, dated 07/15/2023, showed staff were to set the resident up at the sink to perform their own oral care with supervision three times daily.
During a concurrent observation and interview on 07/20/2023 at 11:12 AM showed Resident 59 with dark crusty debris their upper left and right incisor teeth (the resident was missing most of their teeth in the front and on the bottom. The resident stated they had received oral care only once since admission to the facility.
During an additional observation and interview on 07/21/2023 at 11:45 AM, Resident 59's teeth still showed dark crusty debris on the residents upper incisors and the residents breath had a foul odor. The resident stated they were not getting any assistance with their oral care and stated it should be a part of the rent.
Resident 6. Review of the resident's EHR showed the resident was admitted to the facility on [DATE] with diagnoses including, vascular dementia (brain damage caused by multiple strokes) and major depression.
The most recent comprehensive assessment dated [DATE] showed the resident had cognitive impairment and required extensive assistance for personal hygiene which included oral care.
Resident 6's care plan dated 04/26/2023 showed directives for oral care which included to set the resident up at the sink, apply toothpaste on the toothbrush and provide verbal cues to the resident to complete oral care with physical assistance as needed.
During an observation on 07/19/2023 at 4:04 PM the resident was in the dining room sitting at a table. The resident introduced themselves to the surveyor and was noted to have some food debris on their front teeth. When asked if their teeth had been brushed that day the resident stated I don't know.
During an interview on 07/19/2023 at 4:24 PM, the resident's representative stated they were concerned because the resident did not consistently get their teeth brushed. and stated the equipment for oral care was at the Resident 6's sink and was never used as the toothbrush was always dry and in the same place stored in a plastic bag by the sink.
Resident 6's representative further stated the resident had recently gone to the dentist who found food lodged in the residents teeth related to poor oral care.
Record review of a dental note, dated 06/29/2023, showed the resident needed more oral care as there was food and debris stuck in the residents teeth. The dentist ordered the resident to have oral care twice daily with warm water rinses after meals to maintain oral health.
In an interview on 07/21/2023 at 3:46 PM, Staff B, Director of Nursing, acknowledged that the NA staff should be assisting residents with oral care per the care plan.
Reference WAC 388-97-1060(2)(a)(ii)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide a one-to-one individualized activity program f...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide a one-to-one individualized activity program for cognitive stimulation for 1 of 1 sampled resident (Resident 1). This failure placed Resident 1 at risk of decreased cognitive ability and diminished quality of life.
Findings included .
Record review of Resident 1's Minimum Data Set, dated [DATE], showed Resident 1 had memory problems and their skills for making daily decisions was moderately impaired.
Record review of Resident 1's Care Area Assessment, dated 07/21/2023, showed Resident 1 had cognitive loss.
Record review of Resident 1's Care Plan, dated 08/02/2013, showed Resident 1 had impaired cognitive functioning related to a medical condition, and that the facility was to offer an ongoing structured activity program for intellectual stimulation.
Observation on 07/16/2023 at 11:24 AM, showed Resident 1 sat in their wheelchair and watched television (TV).
Observation on 07/17/2023 at 8:41 AM and at 10:00 AM, showed Resident 1 sat in their wheelchair and watched a cartoon on the Cartoon Network channel.
Observation on 07/18/2023 at 1:37 PM, 2:41 PM, 3:01 PM, and at 3:27 PM, showed Resident 1 sat in their wheelchair and watched a cartoon on the Cartoon Network channel.
Observation on 07/19/2023 at 1:49 PM, showed Resident 1 lying in bed with their eyes closed.
Observation on 07/20/2023 at 9:56 AM, 10:46 AM, and at 1:09 PM, showed Resident 1 sat in their wheelchair and watched a cartoon on the Cartoon Network channel.
Observation on 07/20/2023 at 2:35 PM, showed Resident 1 lying in bed with their eyes open.
Observation on 07/21/2023 at 10:52 AM, showed Resident 1 sat in their wheelchair with their TV off.
During an interview on 07/21/2023 at 1:14 PM, Staff D, Activity Director, stated that Resident 1 had a 1:1 (one staff worked with 1 resident) structured activity program per their goal. Staff D was unable to provide documentation for this activity.
Reference: WAC 388-97-0940 (1)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to consistently follow physician ordered eating recommenda...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to consistently follow physician ordered eating recommendations for 1 of 1 resident (Resident 59) reviewed for safe swallowing guidelines. This failure placed the resident at risk for choking, aspiration (a condition where food or liquids are breathed into the lungs), and an overall decline in their health status.
Findings included .
Resident 59. Review of the resident's Electronic Health Record (EHR) showed the resident was admitted to the facility on [DATE] following a stroke (damage to the brain from an interruption in blood flow) and dysphagia (impaired ability to safely swallow).
The EHR showed the resident had a gastrostomy tube (GT a tube inserted into the abdomen) placed on 06/23/2023 while at the hospital to maintain their hydration and nutritional status and their inability to safely swallow food and liquids.
The most current comprehensive assessment, dated 07/05/2023, showed the resident was cognitively intact and required total assistance from staff for nutrition via the GT.
A progress note, dated 07/12/2023, showed the resident's GT had become dislodged therefore, they were sent back to the hospital to have it replaced. The resident returned to the facility on [DATE].
Review of a hospital speech evaluation dated 07/12/2023 showed the resident's ability to swallow had improved therefore their diet was upgraded to a soft diet with thin liquids. There were specific instructions for staff to follow related to the risk of choking and aspiration which included;
- upright positioning for eating
- one on one supervision to provide reminders for dysphagia protocol
- alternate small bites and sips, one at a time, bite/sip to clear oral residue
Record review of the resident's care plan, updated on 07/15/2023, showed the resident .may eat a soft diet with thin liquids. Aspiration Precautions in place. Supervision assist required. Alternating 1 bite with 1 sip .
An observation on 07/19/2023 at 5:00 PM, showed Resident 59 sitting at a table in the dining room. Staff N, Nursing Assistant, (NA), was sitting at the same table. Resident 59's food tray arrived and was placed in front of them. The resident began eating, taking two to three bites at a time without alternating a bite of food with a sip of liquid. The resident coughed several times before Staff LL, NA, sat down beside Resident 59 and provided supervision and reminders to take one bite of food and alternate with a sip of liquid.
During an interview on 07/19/2023 at 5:15 PM, Staff N stated they were not aware that Resident 59 had specific feeding guidelines or required supervision during their meal. Staff N stated they were only working with the other resident at the table.
In an interview on 07/20/2023 at 10:28 AM, Staff M, Speech Language Pathologist, stated they were surprised when the resident returned from the hospital with orders to begin eating and drinking. Staff M explained that it was important for the resident to take sips of liquid after each bite of food to avoid the food building up in the back of their throat which could cause a aspiration or choking.
An additional dining room observation on 07/21/2023 at 11:54 AM showed Resident 59 feeding themselves unsupervised taking two to three bites of food at without alternating bites with fluids. The resident coughed several times before Staff N sat down at the table and reminded them to alternate a bite of food with a sip of liquid.
During an interview on 07/21/2023 at 3:45 PM, Staff B, Director of Nurses, stated the staff should be following Resident 59's feeding recommendations to ensure their safety when eating and drinking.
Reference WAC [PHONE NUMBER]60(1)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure residents received proper treatment and assisti...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure residents received proper treatment and assistive devices to maintain their vision for 2 of 3 residents (Resident 49 and 59) reviewed for vision. Failure to assist residents to obtain vision services/devices, placed the residents at risk for decreased self-care, social interaction and participation in activities.
Findings included .
Resident 49. Electronic Health Record (EHR) review showed the resident was admitted to the facility on [DATE] with diagnoses to include Diabetes Mellitus (a metabolic disorder in which the body has high sugar levels for prolonged periods of time). Review of the 06/23/2023 comprehensive assessment showed the resident had adequate vision (sees fine detail, such as regular print in newspapers/books) and moderate cognitive impairment.
During an interview on 07/17/2023 at 8:54 AM, Resident 49 was in bed with the head of bed elevated. There were several facility handouts on the resident's overbed table in front of them that included information about activities and the next day's meal menu. Resident 49 stated they could not see writing that small and they would need their glasses that they had at home. Resident 49 stated It would be nice to see to read, and if they made me an eye appointment, I would go.
During an interview on 07/19/2023 at 10:27 AM, Staff E, Social Service Director, stated they were just assigned last week to arrange resident appointments. Staff E stated, I was not aware [Resident 49] needed glasses to see.
During an interview on 07/20/2023 at 3:33 PM, Staff D, Activity Director, stated Resident 49 refuses to participate in many activities.
During a telephone interview on 07/21/2023 at 10:00 AM, Resident 49's representative (RR 49) stated they were aware the resident needed glasses but was unable to obtain their current glasses from their home. RR 49 stated that Resident 49 had a vision appointment a couple months ago and could not go due to being in the hospital. RR 49 stated they had not heard from the facility staff about any new appointments.
During an interview on 07/21/2023 at 1:07 PM, Staff EE, Activity Assistant, stated they would always read the daily handouts to [Resident 49] and did not know the resident could not see without their glasses.
During an interview on 07/21/2023 at 2:39 PM, Staff B, Director of Nursing, was informed of Resident 49's inaccurate vision assessment, and the resident needed corrective lenses. Staff B stated they were not aware the resident needed glasses.
Reference: WAC 388-97-1060(3)(a)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure pharmacy recommendations were followed up on for 1 of 5 resid...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure pharmacy recommendations were followed up on for 1 of 5 resident (Resident 25), reviewed for unnecessary medications. This failure placed the resident at risk of inaccurate dosing of medication, adverse side effects, and receiving a medication longer than medically necessary.
Findings included .
Review of the facility policy titled Medication Regimen Review (MRR) dated July 2021, showed the MRR involved reporting of findings with recommendations for improvement. Recommendations are acted upon and documented by the facility staff and/or the prescriber.
Resident 25. Review of the resident's Electronic Health Record (EHR) showed, the resident admitted to the facility on [DATE] with multiple diagnoses which included depression and psychotic disorder. Review of the comprehensive assessment, dated 06/23/2023, showed the resident's cognition was moderately impaired.
Review of the pharmacy recommendation, dated 6/19/2023, showed the pharmacist recommended to change Resident 25's current medications due to excessive daytime sleep. As of 7/19/2023 (one month after the recommendation) the recommendations were not followed up or/ acted upon.
During an interview on 07/22/2023 at 8:43 AM, Staff B, Director of Nursing, (DON) stated the pharmacy recommendations get placed into the provider box, the physician then takes the recommendations and wrote their orders. The order then goes to Staff C, Licensed Practical Nurse (LPN), who would process the orders and take them to medical records to be scanned into the resident's chart.
During an interview on 07/22/2023 at 8:45 AM Staff C stated that once recommendations were received, they reviewed them and processed the orders. Once the orders were processed, they then gave them to medical records for scanning. Staff C stated they communicated the recommendations to the nurses on the carts and informed them of any change in medications. Staff C further stated that they at times would notify the DON of the recommendations.
During an interview on 07/22/2203 at 9:13 AM with Staff B and Staff E, Social Services Director, Staff B stated that they were not aware of what the recommendations were for the residents. Staff E stated that the resident had the right to sleep.
Reference: WAC 388-97-1300(4)(c)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0572
(Tag F0572)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to periodically review resident rights with residents during their stay at the facility for 7 of 7 sampled residents (Residents 5, 27, 32, 38,...
Read full inspector narrative →
Based on interview and record review, the facility failed to periodically review resident rights with residents during their stay at the facility for 7 of 7 sampled residents (Residents 5, 27, 32, 38, 46, 54, and 55). This failure placed residents at risk of not understanding their rights and a reduced ability to self-advocate.
Findings included .
Record review of the facility's undated policy titled, admission Agreement - appendix D [facility name] Resident Rights, showed this policy did not address the review of resident rights.
During an interview on 07/18/2023 at 9:09 AM, Representatives of the Resident Council (Residents 5, 27, 32, 38, 46, 54, and 55), stated that they were not aware of staff reviewing resident rights.
During an interview on 07/19/2023 at 11:15 AM, Staff D, Activity Director, stated that they did not review resident rights at the Resident Council meetings.
During an interview on 07/19/2023 at 11:35 AM, Staff A, Administrator, stated that the Social Services Director reviewed resident rights with residents.
During an interview on 07/19/2023 at 11:44 AM, Staff E, Social Services Director, stated that they did not go over resident rights during care conferences. Staff E further stated that there was no documentation to show resident rights were periodically reviewed.
Reference: WAC 388-97-0300 (1)(a), (7)(b)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0577
(Tag F0577)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure current state survey results were available for 7 of 7 sampled residents (Residents 5, 27, 32, 38, 46, 54, and 55) to e...
Read full inspector narrative →
Based on observation, interview and record review, the facility failed to ensure current state survey results were available for 7 of 7 sampled residents (Residents 5, 27, 32, 38, 46, 54, and 55) to examine. This failure prevented residents, family members, and visitors from exercising their rights to examine these documents.
Findings included .
Record review of the facility's undated policy titled, admission Agreement - appendix D [facility name] Resident Rights, showed residents had the right to examine the most recent results of the facility's state survey or inspections.
During an interview on 07/18/2023 at 9:09 AM, Resident Council Representatives (Residents 5, 27, 32, 38, 46, 54, and 55), stated that they did not know where state survey results were available to them to read.
Observation on 07/19/2023 at 11:16 AM, showed a hard covered three-ring binder located outside of the business office. The most recent copy of state survey results in this binder was dated 03/30/2023. There were other state survey investigations, dated 05/18/2023 and 06/02/2023, that were not included in the book.
During an interview on 07/19/2023 at 11:35 AM, Staff A, Administrator, stated that state survey results were printed and put into a book near the business office. Staff A confirmed the most recent state survey results in the book was dated 03/30/2023.
Reference: WAC 388-97-0480
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to document, periodically review, and revise Advanced Directives related to residents' wishes for 9 of 9 sampled residents (Residents 1, 7, 8,...
Read full inspector narrative →
Based on interview and record review, the facility failed to document, periodically review, and revise Advanced Directives related to residents' wishes for 9 of 9 sampled residents (Residents 1, 7, 8, 21, 26, 30, 31, 44 and 213), reviewed for Advanced Directives. This failure prevented residents from having their health care decisions and preferences known in advance, and when they were unable to communicate this information.
Findings included .
Record review of the facility's undated policy titled, Advance directives (legal documents that provide instructions for medical care when a person is unable to communicate their own wishes) will be respected in accordance with state law and facility policy, showed:
1.
A copy of residents' Advance Directives would be placed in their medical record.
2.
The residents' decision to accept or decline an Advance Directives would be documented in the medical records.
3.
The Interdisciplinary Team would conduct an annually review, with the resident, their Advance Directives.
Record review of the 9 sampled residents' Electronic Health Records on 07/18/2023, showed, no documentation related to Advance Directives or residents' decisions to accept or decline this document.
During an interview on 07/18/2023 at 12:54 PM and at 1:38 PM, Staff E, Social Services Director, stated that the process for Advanced Directives was that they received a copy of residents' Advanced Directives when a resident was admitted , and that the documents were kept in their health records. Additionally, they were unable to locate Advanced Directives for the 9 sampled residents. Staff E stated they were unaware of the process for conducting reviews of Advanced Directives with residents and did not conduct those reviews, nor document residents' Advanced Directives on their decisions to accept or decline this document. Further stated a nurse would look for the Advanced Directives documents when needed.
During an interview on 07/18/2023 at 2:10 PM, Staff K, Licensed Practical Nurse (LPN) Care Manager, stated they provided and went over a form titled Advanced directive and Physician Order for Life Sustaining Treatment (POLST) and residents signed this form. Also, a resident's signature on this form indicated they went over the Planning Ahead packet and the POLST form with them. Staff K stated they did not document when a resident did not have an Advanced Directives document and that they communicated this information verbally at their stand-up meeting, that there was no paper process. Further, they did not know how often Advanced Directives were reviewed.
During an interview on 07/19/2023 at 2:13 PM, Staff B, Director of Nursing, stated the Resident Case Manager provided an admission packet and residents signed they received the information. Staff B said they did not know if this was documented. Staff B stated the Advanced Directives should be scanned into the residents' charts and if residents had Advanced Directives, it would be in their Care Plan. Further, if residents did not have Advanced Directives it would not be in their Care Plan.
Reference 388-97-0300 (1)(b), (3)(a-c)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to provide a clean and comfortable homelike environment for 7 of 10 resi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to provide a clean and comfortable homelike environment for 7 of 10 resident rooms (rooms 2, 3, 4, 20, 32, 35 and 55), 3 of 3 shower rooms (Team 1 shower room, Team 2 shower/bath room and Team 3 shower room), and missing/damaged wood panel flooring were also observed in one of five hallways (Team 2 hallway) all reviewed for safe, comfortable, and sanitary environment, 2 of 5 hallways in resident care areas (Middle and Kitchen hallways) reviewed for comfortable sound levels. These failures placed residents at risk for a diminished quality of life.
Findings included .
Resident rooms
An observation on 07/16/2023 at 2:10 PM, in room [ROOM NUMBER], showed a six-drawer dresser was missing the third drawer on the left side of the dresser. The drawer front face was off and in the corner of the room with missing particle/pressed board and sharp pieces were exposed.
An observation on 07/16/2023 at 2:46 PM in room [ROOM NUMBER], showed gouges (grooves or holes) on the wall near the window.
An observation on 07/16/2023 at 3:41 PM, in room [ROOM NUMBER] showed small gouges on the wall at the end of the bed. The floor was marked with long black marks throughout the room.
During an observation on 07/17/2023 at 9:27 AM, in room [ROOM NUMBER], there were blue tape strips on the floor. Staff AA stated blue tape strips are placed instead of transfer poles and that transfer poles are no longer used in the facility.
An observation on 07/17/2023 at 9:37 AM, room [ROOM NUMBER], had two inch by four-inch piece of wood at end of the bed, loose with sign stating not to move the bed related to the wall damage. The wall had paint peeling off and gouges on the wall next to the piece of wood.
Shower Rooms
An observation on 07/17/2023 at 9:43 AM, showed team 3 shower room, across from room [ROOM NUMBER], had a toilet with dark brown/black material on the outside of toilet-bowl and the shower tile had black/pink substance on the floor in between the grout.
An observation on 07/17/2023 at 10:33 AM, showed team 1 shower room/bath, across the hall from room [ROOM NUMBER], had a drain cover missing which left the drain open. Further observation showed in between the tile flooring the grout had a black substance.
An observation on 07/17/2023 at 10:38 AM, showed team 2 shower room across room [ROOM NUMBER], had a shower handle that had a yellowish, brown-stained towel that was taped around the handle of the sprayer. The floor tile had pink substance in between the grout.
Noise Levels
During an interview on 07/16/2023 at 10:47 AM, Resident 54, in room [ROOM NUMBER] complained that the overhead fan to the bathroom was loud.
An observation on 07/18/2023 at 1:13 PM, in room [ROOM NUMBER], showed resident 26 was sitting down in the restroom, and requested the staff to shut off the light/fan due to the loud noise the overhead fan was making.
On 07/18/2023 at 9:09 AM during the Resident Council Meeting, it was stated that the noise at night was terrible. Barrels rolled down the hall and made a lot of noise, the wheels rattled and needed new wheels.
During a concurrent observation and interview on 07/18/2023 at 2:28 PM, in room [ROOM NUMBER], the resident representative of Resident 36, stated that the laundry room door [on the dirty side] slammed shut when staff go in and out of the laundry room, and the laundry-carts are loud and rolling at all hours up and down the halls.
During an interview on 07/21/2023 at 3:02 PM, Staff AA, Maintenance Director, stated that they were trying to replace broken furniture and has been taking inventory. Staff AA further stated that they had no official order yet for the new furniture. Staff AA then stated that the general maintenance was done weekly, monthly and they completed annual inspections. Staff AA stated they were aware of the issues of the barrels and door noise but had to prioritize repairs in the facility. Staff AA stated that once a resident was discharged , the rooms that needed repairs were part of the readiness program and were repaired at the time of discharge. Additionally, Staff AA stated the staff were to use the tells system ( A web-based software that is designed to help track facility maintenance and building services) for the needed facility/room repairs and staff were not currently utilizing the system.
During an interview on 07/22/2023 at 9:18 AM Staff A, Administrator, stated that about the nighttime noise. They were not able to substantiate.
Reference: WAC 388-97-0880
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 44. Review of the resident's EHR showed, the resident admitted to the facility on [DATE] with multiple diagnoses which ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 44. Review of the resident's EHR showed, the resident admitted to the facility on [DATE] with multiple diagnoses which included delusional disorder, paranoid personality, and dementia. Review of the comprehensive assessment, dated 05/17/2023, showed the resident's cognition was moderately impaired.
During an interview on 07/16/2023 at 11:41 AM Resident 44, stated they had not been involved with care conferences.
Review of the progress note dated 11/08/2022 showed that the facility held a care conference, with no documentation that the resident had attended the meeting.
During an interview on 07/21/2023 at 2:07 PM, Staff E stated, they had not been doing the quarterly care plan meetings due to only having one RCM, which made the care conferences hard to get to.
During an interview on 07/22/2023 at 9:13 AM, with Staff B, Director of Nursing, and Staff E, Staff B stated they were aware the facility needed to work on its processes for care conferences and that they had not been coordinated consistently.
Based on observation, interview, and record review, the facility failed to ensure the coordination of care conferences for 3 of 4 residents (Residents 20, 30 and 44); and failed to update or revise care plan changes for fall interventions and resident preferences for 2 of 4 residents (1 and 30) reviewed for care plan timing and revision. This failure placed the residents at risk for unmet and unidentified care needs and decreased quality of life.
Findings included .
Review of the facility's policy, dated 07/2023, titled Care Conferences showed there were no procedure or processes for implementing the policy. The policy did not list the physician (or delegated Non-Physician Practitioner) as part of the Interdisciplinary Team (IDT), nor did it show how the physician would be involved. The policy listed the Nursing Assistant (NA) would be included only if applicable the policy showed no documentation how the facility would involve the resident or Resident Representative (RR). The policy further showed no notification timeframes or accessibility options for ensuring the resident or RR could participate in the care planning process.
Resident 20. Review of Resident 20's Electronic Health Record (EHR) showed, the resident admitted to the facility on [DATE] with diagnoses to include aphasia (absence of speech), depression, and anxiety (a feeling of fear, dread, and uneasiness). Review of the comprehensive assessment dated [DATE] showed, the resident's cognition could not be assessed due to being non-verbal and unable to actively participate in the cognition assessment.
Review of the care plan, dated 04/23/2023, showed the resident could respond to simple yes/no questions, or by using hand gestures and pointing.
During a phone interview, on 07/17/2023 at 11:38 AM, the RR stated the resident or themself did not get invited to care conferences. The RR stated they had received calls after what I am assuming were care conferences and the facility would update the RR on what the facility thought was best for my [Resident 20]. The RR further stated the last time the facility called the RR, was to inform them they had discontinued a psychotropic medication (a group of drugs that can affect mood, behavior, perception, and thoughts) that Resident 20 had used long term. The RR stated that was why they would like to be more involved in those types of decisions.
During an interview, on 07/21/2023 at 10:00 AM, Staff E, Social Services Director (SSD), stated resident care conferences should be scheduled within the first 72 hours of admission, with each comprehensive assessment or as needed. Staff E stated they attempted to involve the resident and the RR but there were some that declined or did not want to be involved, I do not document that in their EHR or care plan that. Staff E further stated the facility had not scheduled care conferences for their long-term residents since before their employment to the facility (February 2023) due to the facility had one Resident Care Manager (RCM) and didn't want to overwhelm them with more work. Staff E further stated this is an area they have identified as an issue.
Resident 1
<Care Plan not updated with preferred activities>
Record review of the facility's policy titled, [Corporation] - Activity Programs, reviewed on 07/2023, showed the following:
1.
Activities were offered based on resident assessment and preferences.
2.
The activity program included group, independent, individual, and assisted individual activities to meet the needs and interest of residents.
3.
Activities were provided to reflect the choices and rights of residents.
4.
Activities reflected the hobbies and personal preferences of residents.
Record review of Resident 1's comprehensive assessment, dated 05/03/2023, showed the following activity preferences were very important for Resident 1: have books, newspapers, and magazines to read, listen to music, be around animals, keep up with the news, do things with groups of people, do favorite activities, go outside to get fresh air, and participate in religious services.
Record review of Resident 1's Care Plan, dated 08/02/2013, showed Resident 1 was to be offered an ongoing structured activity program for intellectual stimulation, and sensory/memory activities were to be offered at least two times weekly.
Record review of Resident 1's Activity's Director Interview Assessment, undated, showed Resident 1 preferred the following activities: arts and crafts; watching sports; listening to music; looking at magazines; going outside when the weather was nice, gardening, visiting with others, doing things with other people, and watching TV. This assessment further showed Resident 1 enjoyed participating in the following types of group activities: entertainment, Bingo, movies, cooking, and special events.
Record review of the facility's Activity Calendar for July 2023, undated, showed an activity called BINGO was scheduled for 07/18/2023 at 2:30 PM.
Observation on 07/18/2023 at 2:41 PM showed Resident 1 sat in a wheelchair and watched a cartoon on the Cartoon Network TV channel.
Record review of the facility's Activity Calendar for July 2023, undated, showed an activity called Summer Craft was scheduled for 07/20/2023 at 2:30 PM.
Observation on 07/20/2023 at 02:35 PM, showed Resident 1 lying in bed with their eyes open.
During an interview on 07/21/2023 at 12:45 PM, Staff FF, Activity Assistant, stated that they brought the facility's Daily Chronicle (a set of papers that contained the facility's daily meal choices, crossword puzzles and pictures to color) to Resident 1. Staff FF stated that they sat and colored with Resident 1 when they had time.
During an interview on 07/21/2023 at 1:14 PM, Staff D, Activity Director, stated that they conducted activity assessment interviews with residents to know what activities they preferred. Staff D provided a copy of Resident 1's assessment to the surveyor.
Resident 30
<Care Conference not Accommodate Resident's Participation>
Record Review of Resident 30's comprehensive assessment, dated 05/03/2023, showed the resident had a BIMS score of 15 (means cognitively intact). Diagnosis to include Epilepsy and dementia.
Record Review of Resident 30's Care Conference Summary, dated 05/01/2023, showed Resident 30 was not in attendance for their Care Conference.
Record Review of Resident 30's Progress Note, dated 05/01/2023, showed Resident 30 had a scheduled care conference. At 1:00 PM Resident 30 had not yet returned from their lunch outing and Resident 30's family member requested that the meeting go on without [them] present. The care conference was held without Resident 30 in attendance.
During an interview on 07/20/2023 at 1:30 PM, Staff E, Social Services Director, stated that Resident 30 was independent and cognitively intact. Staff E stated that they scheduled a care conference for Resident 30 on 05/01/2023. Staff E stated that Resident 30 was not at the facility at the time of the care conference. Staff E stated that they did not reschedule the care conference so that Resident 30 could attend.
During an interview on 07/21/2023 at 9:21 AM, Staff A, Administrator, stated that if a resident has a BIMS (a test to evaluate cognitive function) of 15, the family cannot have a care conference without them. Staff A stated that a Care Conference should not be scheduled if the Resident was out of the building.
Resident 30
<Care Plan not revised with fall interventions>
During an observation and interview on 07/17/2023 at 10:29 AM, showed Resident 30's right elbow was covered with a bandage. Resident 30 stated that they had fell last night while they were outside smoking a cigarette. Resident 30 said the wind blew their cigarette butt onto the ground, they bent over to pick it up, and then fell over backwards. Resident 30 stated that staff saw that the skin on their right elbow was broken open and asked what happened.
Record review of Resident 30's Electronic Medication Administration Record, dated 07/17/2023, showed to monitor Resident 30 for a post-fall three times a day for three days.
Record review of Resident 30's Care Plan, dated 04/26/2023, showed Resident 30 was assessed to be a moderate risk for falls and that he had a history of falls.
During an interview on 07/22/2023 at 8:10 AM, Staff B, Director of Nursing Services, stated that the facility investigated Resident 30's fall on 07/17/2023. Staff B stated that Resident 30's Care
Plan was not revised to include the interventions from the facility investigation regarding their fall.
Reference: WAC 388-97-1020(2)(c)(d)(f), (4)(b)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 25. Review of the resident's EHR showed, the resident admitted to the facility on [DATE] with multiple diagnoses which ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 25. Review of the resident's EHR showed, the resident admitted to the facility on [DATE] with multiple diagnoses which included depression and psychotic disorder (severe mental disorder that cause abnormal thinking and perceptions). Review of the comprehensive assessment, dated 06/23/2023, showed the resident's cognition was moderately impaired. and required extensive assistance of one staff member for activities of daily living. The assessment also showed the resident received a routine antipsychotic medication, had no GDR attempted, and no contraindicated statement from the provider.
Review of Resident 25's February 2023 Medication Administration Record (MAR) showed the resident received an order on 02/07/2023 for a routine antipsychotic medication (Seroquel). The MAR did not reflect a stop date or a decrease in dose.
Review of the pharmacy recommendation, dated 6/19/2023, showed the pharmacist recommended to change Resident 25's current medications due to excessive daytime sleep. As of 07/19/2023, the recommendations were not followed up or/ acted upon.
<No Stop Date>
Resident 7. Review of the resident's EHR showed, the resident admitted to the facility on [DATE] with multiple diagnoses which included anxiety. Review of the comprehensive assessment dated [DATE] showed the resident's cognition was moderately impaired.
Review of the resident's 07/2023 MAR showed the resident received an order on 03/02/2023 for a PRN antianxiety medication (Lorazepam, a brand of anti-anxiety medication). The order did not indicate a stop date and showed no documentation of an expected duration of use.
During an interview on 07/21/2023 at 3:26 PM, Staff B, Director of Nursing, stated they expected when a PRN psychotropic medication order was obtained and entered into the EHR, there should have been a stop date for 14 days from the start date. Also present was Staff C, Assistant Director of Nursing, who stated they had identified that medication had been entered by the night nurse, who really didn't know about our stop time (regulation requirement for as needed psychotropic medication).
During an interview on 07/25/2023 at 12:58 PM, Staff S, Pharmacy Consultant, stated they did not recommend removing Resident 7's PRN anxiety medication due to the resident had admitted to hospice services, I made a mistake and I need to improve in that area.
Reference: WAC 388-97-1060 (3)(k)(i)
Based on observation, interview and record review, the facility failed to initiate gradual dose reductions (GDR- stepwise tapering of a dose to determine if symptoms, conditions, or risks could be managed by a lower dose or if the dose or medication could be discontinued) or obtain a rationale from the physician or prescribing practitioner that a GDR was clinically contraindicated for 2 of 5 residents (Residents 12 and 25) reviewed for unnecessary medication; and the facility failed to ensure as-needed (PRN) psychotropic medications (medications capable of affecting the mind, emotions, and behavior) were limited to 14 days without providing a physician-documented rationale or duration for 1of 2 residents (Resident 7) reviewed for PRN psychotropic medication use. These failures placed residents at risk of being over medicated, medical complications related to the side effects, and diminished quality of life.
Findings included .
Record review of the facility's undated policy titled, Antipsychotic (a class of medications used to treat psychosis and other mental and emotional conditions) and Psychotropic Medication Use, showed that antipsychotic medications will be prescribed at the lowest possible dosage and for the shortest period of time and are subject to gradual dose reduction and re-review. The interdisciplinary team (IDT) which includes the Registered Pharmacist, Medical Director, Psych Provider, Social Worker and Nursing will review psychotropic medications during the antipsychotic monthly meeting and per significant change. Further review of the policy showed PRN psychotropic medications used longer than 14 days would require physician-documented rationale and the order should reflect the duration of the order.
<Gradual Dose Reduction>
Resident 12. Electronic Health Record (EHR) review showed the resident was admitted to the facility on [DATE] with diagnoses to include depression and dementia (a loss of mental ability severe enough to interfere with normal activities of daily living) with hallucinations (a sensory perception that occurs in the absence of an actual external stimulus and usually arises from neurological disturbance).
Review of the 06/30/2023 comprehensive assessment showed the resident had severe cognitive impairment and required extensive physical assistance for activities of daily living. The resident also received a routine antipsychotic medications, had no GDR attempted, and no physician contraindicated statement.
Review of Resident 12's 04/11/2023 revised care plan showed a focus plan for delusions (a fixed false belief that is resistant to reason or confrontation) and hallucinations, and a focus plan for the antipsychotic medication Seroquel (an antipsychotic medication that works by changing the actions of chemicals in the brain.)
Review of the EHR physician orders showed Resident 12 was started on Seroquel on 08/05/2022 at 12.5 milligrams (mg) once at bedtime for hallucinations. Then on 10/12/2022 the dose was increased to 25 mg at bedtime. The medication was last increased on 12/09/2022 to 50 mg at each bedtime.
Review of the 03/10/2023 at 11:42 AM Psychotropic Medication Review progress note showed the resident was on Seroquel 50 mg for dementia with behavioral disturbance. The progress note showed no documentation of discussions of a GDR for the resident's Seroquel.
Review of a 06/21/2023 Psychiatric Nurse Practitioner showed Resident 12's auditory and visual hallucinations had improved with use of Seroquel.
During an observation on 07/16/2023 at 9:31 AM and 1:47 PM, Resident 12 was dressed and lying on their right side in bed with their eyes closed.
During an observation on 07/17/2023 at 9:11 AM, Resident 12 was dressed, groomed, and lying in bed on their right side with eyes closed.
During an observation on 07/18/2023 at 3:00 PM, Resident 12 was dressed, awake and lying in bed, on their right side. The resident stated they did not want to get up out of bed.
During an interview on 07/18/2023 at 3:03 PM, Staff GG, Nursing Assistant (NA), stated they had not seen Resident 12 agitated lately.
During an interview on 07/18/2023 at 3:08 PM, Staff Z, Licensed Practical Nurse (LPN), stated [Resident 12] was very confused and was checked on frequently. The resident does not like to get out of bed and eats their lunch on the side of the bed.
During an interview on 07/19/2023 at 2:42 PM with Staff B, Director of Nursing (DON) and Staff C, LPN/Assistant DON, stated psychotropic medication meetings occurred monthly. Staff C, while reviewing Resident 12's EHR, stated they could not find any psychotropic medication meetings for Resident 12 in 2022 or 2023.
During a telephone interview on 07/21/2023 at 10:00 AM, Resident 12's Representative stated there had not been any discussions at the care conference about a gradual dose reduction for Resident 12 and they belived the resident would benefit from a GDR. They stated they visit [Resident 12] once a month and all they want to do was lay in bed and says they are waiting for their husband to to come home.
During an interview on 07/21/2023 at 2:53 PM, Staff B, stated they recalled meeting on Resident 12, but cannot find any notes since March 2023. Staff B stated they did not discuss GDRs for Resident 12 and now realized how stable the resident had been and there should have been a GDR attempted.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure medications, biologicals, and testing supplies were labeled, dated, or discarded when expired for 1 of 1 medication ro...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to ensure medications, biologicals, and testing supplies were labeled, dated, or discarded when expired for 1 of 1 medication room and 1 of 1 treatment cart reviewed for medication storage. These failures placed residents at risk of receiving compromised or ineffective medications.
Findings included .
Review of the facility's 07/2021 policy, titled Medication Storage in the facility showed, medications dispensed by the pharmacy will be kept in the container they were dispensed in with the pharmacy label. The policy further showed outdated medications will be disposed of according to the facility procedures for destroying medications.
An observation on 07/20/2023 at 10:39 AM, with Staff K, Licensed Practical Nurse Care Manager in attendance, of the medication room showed:
•
66- bottles of hand sanitizer, 4 fluid ounces (oz) each that expired on 03/2023.
•
16 fluid oz bottle, half full bottle of hydrogen peroxide (a mild antiseptic used on the skin to prevent infection of minor cuts, scrapes, and burns) that expired on 07/2022.
•
1- full box of 200 and 1 partial box of 42 alcohol prep pads (pads used to help clean the skin and can be used on cuts, scrapes, and abrasions prior to bandaging) were dried out (per Covidien manufacturers recommendations, they should be discarded after two years of shelf life or when they dry out).
•
1-1200 milligram (mg) bottle of 100 soft gel fish oil capsules, three quarters full, expired 4/2023.
•
16- Intravenous (IV) starter kits (gloves, tourniquet, tape, prep pad) that expired on 01/31/2023.
•
90- green capped, 4 ml empty blood collection tubes expired on 04/30/2023.
•
40- orange capped, 4ml empty blood collection tubes that expired on 02/28/2023.
•
99- blue capped, 6 ml empty blood collection tubes that expired on 04/30/2023.
•
2 red capped bacterial swabs that expired on 04/17/2021
•
11- respiratory virus swab collection tubes that expired on 05/15/2022
During an interview on 07/20/2023 at 11:48 AM, Staff C, Assistant Director of Nursing (ADON), stated the facility uses supplies to start IVs and to obtain blood for labs. Staff C further stated it's everyone's responsibility for keeping the medication room organized and clean and to discard expired medications and supplies.
During an observation and concurrent interview on 07/21/2023 at 11:06 AM, the treatment cart had three opened bottles of multi-dose Lidocaine (a local anesthetic), unlabeled and undated. Staff CC, LPN, stated they kept the bottles of lidocaine just in case needed to use again, that they should have removed them from the treatment cart.
During an interview on 07/21/2023 at 3:08 PM, Staff B, Director of Nursing, stated they would expect all medications to be dated upon opening and a label with a specific resident's name and indication for use.
WAC Reference: 388-97-1300(2)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure implementation of infection prevention and cont...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure implementation of infection prevention and control practices for for 1) hand hygiene was completed and gloves were changed by staff between soiled and clean tasks for 2 of 3 residents (Resident 40 and 59) observed for personal care, 2) hand hygiene that was not appropriately performed by 7 of 10 staff, observed during meal services, 3) failure to perform hand hygiene wound care for 1 of 2 residents (Resident 24) observed during a wound care procedure and, 4) failure to follow contact precautions for 1 of 1 resident (Resident 28) reviewed for compliance with Transmission Based Precautions. These failures placed the residents at risk for acquiring infectious diseases and a diminished quality of life.
Findings included .
<Soiled to Clean Task>
Record review of the facility's policy titled, Catheter (a hollow, partially flexible tube that collects urine from the bladder and leads to a drainage bag) Care, dated 08/10/2023, showed that staff were to wash their hands prior to putting on gloves to provide catheter care. After cleaning the resident's catheter and perineal (the area of the body between the anus and the genitals) area, remove gloves, hand wash and apply clean gloves prior to redressing the resident and cleaning up supplies.
Resident 40. Review of the resident's Electronic Health Record (EHR) showed they were admitted to the facility on [DATE] with diagnoses to include; obstructive uropathy (condition where urine flow has been partially or completely blocked), urinary tract infection (UTI, infection of any part of the urinary system) and dementia (a loss of mental ability severe enough to interfere with normal activities of daily living). Review of the 06/24/2023 comprehensive assessment showed the resident had severe cognitive impairment and required extensive staff assistance for activities of daily living.
On 07/17/2023 at 10:10 AM, Resident 40, received urinary catheter care from Staff F, Nursing Assistant (NA). The NA washed their hands at the room sink and put on gloves to provide the catheter care. After the procedure was completed, the NA with the same now soiled gloves on, opened dresser drawers, changed the resident's brief, positioned and covered the resident. Then with the soiled gloves on, the NA opened the room door, took the water basin to the shower room, opened the door with the soiled gloves on and emptied the water from the basin. With the same soiled gloves, Staff F returned to Resident 40's room, opened the door, then removed the gloves and washed their hands at the room sink.
Resident 59. Review of the resident's EHR showed they were admitted on [DATE] following a stroke (a condition when blood supply is cut off from the brain) and dysphagia (a condition that effects a persons ability to swallow).
Review of Resident 59's most recent comprehensive assessment, dated 07/06/2023, showed the resident required extensive assistance from staff for toileting and incontinent care.
During an observation on 07/19/2023 at 12:46 PM, Staff LL, NA entered Resident 59's room and informed them they were going to provide incontinent care. Staff LL put on gloves without performing hand hygiene and obtained washcloths. Staff LL (with their gloved hands) turned on the water to wet the cloths. Staff LL proceeded to perform incontinent care on Resident 59 with the same contaminated gloves they had used to turn on the faucet at the sink.
Staff LL completed incontinent care and bagged up the soiled washcloths, assisted the resident with a new brief and dressed them. Staff LL rearranged items on the residents bedside table without changing their gloves or performing hand hygiene.
<Meal Services>
Observation on 07/16/2023 at 11:35 AM showed a hall cart with meals, was in the hallway. Resident 49's meal was brought to their room and placed on their bedside table. Staff G, NA, repositioned Resident 49 in their bed, repositioned the bedside table and prepped Resident 49's food. Staff G did not change their gloves between repositioning Resident 49 and prepping their meal.
During an observation on 07/06/2023 at 11:41 AM, Staff EE, Activities Assistant, was observed passing out drinks to residents who were sitting in the dining room. Staff EE stated this is our pre-dining social group before the lunch trays arrive. Staff EE was observed coughing into their hands and without performing hand hygiene continued to make and pass out drinks to the residents.
During an observation on 07/16/2023 at 12:00 PM, Staff G and Staff LL, entered the dining room and began assisting various residents with their clothing protectors and positioning at the tables. After the meal trays arrived, Staff G and LL passed out the trays to the residents without performing hand hygiene.
Observation on 07/16/2023 at 12:03 PM, showed Staff V, NA, went to the meal cart, took a tray of food off the cart, and brought it to the dining room table where Resident 47 sat. Staff V placed Resident 47's tray on the table, adjusted their wheelchair, went back to the meal cart and took another tray off the cart. Staff V did not perform hand hygiene.
Observation on 07/16/2023 at 12:06 PM, showed Staff JJ, NA, placed a clothing protector on Resident 1, touched their wheelchair, sat down, took a spoon and assisted Resident 1 with eating their pureed carrots. Staff JJ did not perform hand hygiene.
Observation on 07/16/2023 at 12:09 PM, showed Staff II, Administrator's Assistant, touched a resident's wheelchair, then sat down at Resident 31's dining table and assisted them with their meal. Staff II did not perform hand hygiene.
Observation on 07/16/2023 at 12:22 PM, showed Staff JJ, NA, lifted up Resident 1's clothing protector to cover their cough and then picked up and gave Resident 27 their glass of milk. Staff JJ did not perform hand hygiene.
Observation on 07/16/2023 at 12:28 PM, showed Staff JJ re-entered the dining room, wiped their nose, then sat down and assisted Resident 47 with their meal. Staff JJ did not perform hand hygiene.
Observation on 07/19/2023 at 4:50 PM, showed Staff N, Rehabilitation Aide, brought a tray of food to Resident 27 and set it down on the dining table. Staff N, adjusted Resident 27's wheelchair, then pulled a chair to the same dining table and touched Resident 27's glass of milk. Staff N sat down in the chair and assisted Resident 27 their meal. Staff N did not perform hand hygiene.
<Wound Treatments>
Resident 24. Review of Resident 24's EHR showed the resident admitted to the facility on [DATE] with diagnoses including; a right heel wound infection. The comprehensive assessment, dated 05/19/2023 showed the resident's cognition moderately impaired.
An observation on 07/18/2023 at 12:44 PM, showed Staff CC, Licensed Practical Nurse (LPN), during a wound dressing change of Resident 20's right heel, assisted the resident to their right side, removed their sock and a gauze sock that had been covering the wound, donned gloves without hand hygiene, removed the dressing with visible brownish, yellow drainage, and cleansed the wound with wound cleanser and gauze. Staff CC doffed the gloves (take off/remove), reached into their uniform pocket and obtained a cellular phone device, no hand hygiene, donned new gloves, and proceeded to pick up the cell phone and take pictures of the wound's appearance and size. Staff CC set the phone down, and with the same gloves, applied a skin barrier to the outer part of the wound, applied a fiber gel to the wound, and covered with a foam dressing. Staff CC, with the same gloves, applied a clean tube gauze sock, and assisted the resident back to their previous position. Staff CC then performed hand hygiene, applying friction to their hands with soap and water for less than 10 seconds.
An observation and concurrent interview, on 07/20/2023 at 2:51 PM, showed Staff CC, during a wound dressing change of Resident 20's right heel, donned gloves, removed the old dressing that had brownish-yellow drainage, applied anesthetic (a substance that reduces the risk of infection) to the wound, cleansed the heel with gauze and wound cleanser, applied wound gel to the base of the wound, then covered the wound/gel with an orange heel dressing. Staff CC, with the same gloves then applied a gauze sock over the dressing, and fit the resident with a heel lift boot. When finished, Staff CC disposed of the garbage, and rinsed hands with water only for less than 10 seconds, dried, and exited the room. Staff CC then went to the hand sanitizer on the wall, and sanitized hands. Staff CC stated they normally don't wash hands with soap and water even though the dressing had drainage when removed, and further stated they don't always change their gloves during wound dressing changes.
<Contact Precautions>
Resident 28. Review of Resident 28's EHR, showed the resident admitted to the facility on [DATE] with diagnoses to include a urine infection with an extended spectrum beta-lactamase (ESBL, enzymes produced by some bacteria that may make them resistant to some antibiotics) bacteria and a colostomy bag (a bag that attaches to the colon to collect feces waste). The comprehensive assessment, dated 07/04/2023, showed the resident's cognition was moderately impaired.
An observation on 07/16/2023 at 8:57 AM, showed Resident 28 had a Contact Precautions (precautions that are intended to prevent transmission of infectious agents, including epidemiologically important microorganisms, which are spread by direct or indirect contact with the patient or the patient's environment) sign on the outside of the door and a personal protective equipment (equipment worn to minimize exposure to a variety of hazards) bin outside the door. The sign further showed, staff caring for the resident should wear a gown and gloves for all interactions that involve contact with the patient and the patient environment, and to clean hands before entering and leaving the room.
An observation on 7/16/2023 at 11:52 AM, showed Resident 28 was sitting on the edge of the bed, room smelled of strong urine odor that could be smelled from the hallway, and a urinal sitting on resident's nightstand next to the bed, half full of urine. The resident stood up from the bed, grabbed their front wheeled walker (FWW), exited the room, and walked down the middle hallway towards the front of the office.
An observation and concurrent interview, on 07/18/2023 at 4:22 PM, showed Staff L, NA, entered Resident 28's room and cleaned up garbage off the bedside table, then, ungloved, picked up the resident's urinal and carried it down the middle hallway to the dirty utility, uncovered. When Staff L exited the dirty utility room seconds later, they had donned gloves, took the clean urinal back to the room, exited the room with the gloves on, went to obtain water, brought it back to the room, and then removed gloves, no hand hygiene. Staff L exited the room and went across the hall and used hand sanitizer for hand hygiene. Staff L stated the resident had been on precautions for an infection in their urine and when providing care they should wear personal protective equipment (PPE) and sanitize their hands before and after. I should have used PPE and a bag when handling the urine, I messed up and just forgot.
An observation and concurrent interview on 07/19/2023 at 1:41 PM, Resident 28 exited their room with their FWW, and walked to the sitting area to watch television. Upon leaving the room, Resident 28 informed Staff U, NA, their bed was ready to be changed. Staff U entered the resident's room, donned gloves and no other PPE, and proceeded to change the resident's urine soiled linen on their bed. Staff U stated PPE should have been worn when coming in contact with fluids or feces and hands should be washed after cares were performed. Staff U did not know if they should have donned PPE to change urine soiled linen or if they should provide hand hygiene to the resident, prior to them leaving their room.
An observation on 07/19/2023 at 1:55 PM, Resident 28 was sitting in the sitting area, when Staff N, Restorative Aide, came to get the resident for their daily exercises, the chair the resident had been sitting on had not been sanitized upon leaving the sitting area. Staff N and Resident 28 then walked to the gym where Resident 28 sat on a type of exercise bike. The resident exercised for 12 minutes, was assisted off the bike, and assisted out of the gym by Staff N, and the exercise bike had not been sanitized prior to leaving the gym.
During an interview, on 07/20/2023, at 2:39 PM, Staff C, Infection Preventionist (IP), stated they would expect staff to wear PPE in Resident 28's room when emptying urinals, changing soiled bed linens, or coming in contact with anything the resident might have touched (garbage on bedside table). Additionally, Staff C would expect that staff are ensuring Resident 28's hands are sanitized before exiting the room, after exercising, and that surfaces touched are sanitized. Staff C further stated their expectation for staff hand hygiene during wound treatments should have been done when donning and doffing gloves, after touching soiled, dirty areas and then to clean areas, and when finished and exiting the room. Staff C further stated they had not completed hand hygiene audits since taking over the IP position.
During an interview on 07/20/2023 at 3:11 PM, Staff B stated they would expect the staff would have conducted hand hygiene before and after donning/doffing their gloves, when going from a dirty area to a clean area, and upon entering and exiting a room. Staff B further stated when there was a wound dressing with drainage, they would expect hand hygiene to be completed with soap and water.
During an additional interview on 07/21/2023 at 10:41 AM, Staff C, stated that their overall expectation was for staff to follow infection prevention standards put into place to decrease the risk of spreading infections.
Reference WAC 388-97-1320(1)(c)
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure the food was palatable, attractive, and at a saf...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure the food was palatable, attractive, and at a safe and appetizing temperature for 7 of 7 residents (Residents 5, 38, 54, 32, 55, 46, and 27) interviewed about meal satisfaction during the Resident Council meeting, and 2 of 4 residents (Residents 49 and 30) reviewed for meal palatability. Additionally, Resident 49 was served eggs for breakfast routinely even though eggs were listed as a dislike. This failure placed the residents at risk for weight change, less than adequate nutritional intake, and dissatisfaction with meals.
Findings included .
Record review of the facility's policy titled, Food and Nutrition Services, dated 07/2023, showed that food and nutrition services staff will inspect food trays to ensure that the correct meal is provided to each resident, the food appears palatable and attractive, and it is served at a safe and appetizing temperature.
<Meal Satisfaction>
Record review of Resident Council Meeting Minutes, dated 02/01/2023, showed the representatives had a concern about the meals. The Resident Council Meeting Minutes showed that there were no salt and pepper shaker on the dining room tables and not enough seasoning on the food. They submitted this concern to the facility and the corrective action response from the facility showed residents had to request individual packets of salt and pepper.
During an interview on 07/18/2023 at 9:09 AM, the Representatives of the Resident Council meeting stated that there was a lot of sauce on the food; the food that was supposed to be hot was not hot all the time; the milk was always warm; and the did not seem to have spices, salt, or pepper.
During an interview on 07/20/2023 at 11:45 AM, Staff BB, Food Manager, stated that residents could request individual packets of salt and pepper.
<Meal Palatablilty>
Resident 49. Electronic Health Record (EHR) review showed the resident was admitted to the facility on [DATE] with diagnoses to include Diabetes Mellitus (a metabolic disorder in which the body has high sugar levels for prolonged periods of time). Review of the 06/23/2023 comprehensive assessment showed the resident had moderate cognitive impairment and required supervision and set up for meals.
During an interview on 07/17/2023 at 8:50 AM, Resident 49 was sitting in their bed with the overbed tray in front of them. When asked how breakfast was today, they stated they did not like it. Resident 49 stated the food was cool, and the juice and milk were warm and there was scrambled eggs and I do not like eggs.
During an observation on 07/18/23 at 11:38 AM, Resident 49 was eating their lunch. There was a meat patty, green beans, and watermelon. There was a glass of juice and milk. They stated this meal tasted good today, but it was cool when it arrived and the drinks were warm.
During an interview on 07/19/23 10:00 AM, Resident 49 stated breakfast was good and warm today; however, I got eggs again and I don't like eggs and I did not eat them.
Review of a 04/18/2023 progress noted from Staff BB, Food Manager, showed Resident 49 disliked eggs and did not want them for breakfast.
Resident 30. EHR review of Resident 30's Diet Order, dated 04/26/2023, showed Resident 30 had a regular diet with thin liquids with no added salt.
During an interview on 07/17/2023 at 10:17 AM, Residient 30 stated that the food looked almost edible but that they would never serve it to anyone. They stated that they only had a choice between two meals and there was no substitue meal if they did not like it. Resident 30 stated that foods that were supposed to be hot were not hot and that the facility did not reheat the food. Resident 30 stated that the weekend meals ran about an hour to an hour and a half late and the food might be warm when they received it. Resident 30 stated that the food was bland and that they had their own spices.
A concurrent observation and interview on 07/18/2023 at 11:48 AM, showed Resident 30 ate their meal. Resident 30 stated that they had peas, onions, squash, and a leather pork chop that was too hard to chew. Resident 30 stated that the food was warm but not hot and that it all tasted the same. Observation of the half cut up pork chop showed it looked dry on the plate.
<Test Tray>
During observation of kitchen lunch serve out on 07/20/23 at 11:20 AM showed a double sided insulated cart set next to the stove/grill with the hot food in pans and plated by Staff HH, Cook. The meal plate was then set in a plate insulator and covered with insulated cover. Then the plate was placed on the pre-setup tray that included glasses of milk, juice, ice cream cup, and flat wear. A tray was set up for Resident 30 at 11:25 AM and a duplicate tray was set up at that time for testing. The cart had 10 trays, was closed and staff were notified the lunch cart was ready for the 100 hall. The cart was picked up by Staff DD, Nursing Assistant (NA) at 11:27 AM. Resident 30's tray delivered at 11:29 AM and the test tray was delivered at the same time to the surveyor conference room.
The food temperatures were checked by Staff BB with a digital thermometer and while the surveyor was observing:
baked beans- 135 degrees Fahrenheit (F)
pork rib- 133 degrees F
cold macaroni salad- 74.6 (served on hot plate) degrees F
cranberry juice- 56.3 degrees F
milk- 52.8 degrees F
chocolate hi-calorie drink- 57 degrees F
ice cream cup- 24 degrees F
During an interview on 07/20/2023 at 11:41 AM, Staff BB stated the steam table in the dining room was broken and had not worked for one year or so, and that was why the food was plated from the stove. Staff BB stated they were waiting for approval for a mobile steam table that can go to the dining room for serving out. Staff BB stated the air conditioner had not worked properly in the kitchen for about one year. Staff BB stated they tested the ambient air temperature at the stove, next to the tray cart at 11:22 AM and the temperature of the air was 130 degrees F (too hot for frigerated items on trays nearby to maintain a cool temperature.)
Observation on 07/20/2023 at 11:45 AM showed Resident 30 was served their lunch. At the same time, a test tray of the same meal was delivered to a surveyor. This meal consisted of beans, pork rib, macaroni salad, vanilla ice cream and white and chocolate milk.
During an interview on 07/20/2023 at 11:45 AM, the surveyor that taste tested the test tray stated that the hot foods were warm, the macaroni salad was warm and bland, the milks were not cold enough and the ice cream was melting. Staff BB agreed with the surveyor as they tasted the food and liquids on the test tray.
During an interview on 07/20/2023 at 12:48 PM, Resident 30 stated that the macaroni salad was bland, the hot food was warm, the milk was not cold enough and that the ice cream was melted a bit.
During an interview on 07/20/2023 at 2:11 PM, Staff BB stated they were concerned about the milk temperature during the test tray, so they brought a 120 milliliter (ml) plastic cup of milk from the refrigerator and the milk temp was 34.2 degrees F and set it where the meal trays are set up for meals near the stove. Staff BB stated they retested the temperature of the milk after sitting for 15 minutes and the milk was 52.9 degrees F. Staff BB stated that was just not acceptable.
During an interview on 07/21/2023 at 8:27 AM, Staff A, Administrator, stated they were aware there were cooling issues in the building and had the repair people out this week. Staff A stated they were also working on ordering a new steam table for the dining room. Staff A stated they were not aware of the resident's food complaints related too cool food and warm drinks.
Reference: WAC 388-97-1100(1), (2)