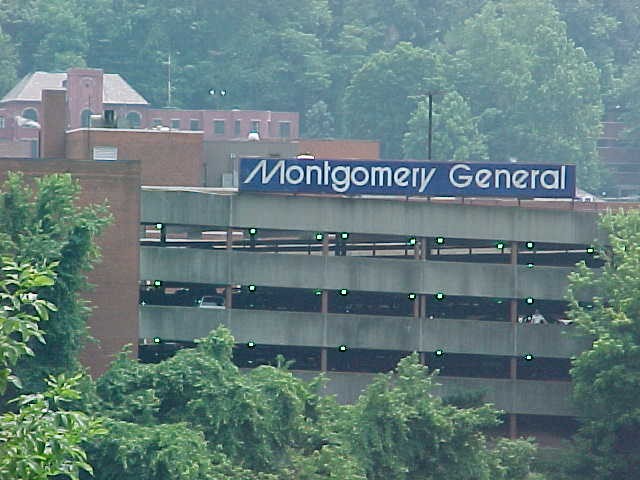
MONTGOMERY GENERAL HOSPITAL



Inspected within the last 6 months. Data reflects current conditions.
Montgomery General Hospital has a Trust Grade of C, which means it is average compared to other nursing homes-neither particularly good nor bad. It ranks #77 out of 122 facilities in West Virginia, placing it in the bottom half, and #4 out of 6 in Fayette County, indicating that there are only three other options available locally. The facility appears to be improving, as the number of issues reported decreased from 17 in 2023 to 13 in 2025. Staffing is stable, with a 0% turnover rate, which is excellent compared to the state average of 44%. However, there are some concerns: the facility has had issues with bed rail safety assessments and failed to notify family members regarding hospital transfers for residents, which could potentially impact their well-being. Overall, while there are strengths in staffing and an improving trend, families should be aware of these significant shortcomings as they consider this facility.
- Trust Score
- C
- In West Virginia
- #77/122
- Safety Record
- Low Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most West Virginia facilities.
- Skilled Nurses ✓ Good
- Each resident gets 52 minutes of Registered Nurse (RN) attention daily — more than average for West Virginia. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 39 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below West Virginia average (2.7)
Below average - review inspection findings carefully
The Ugly 39 deficiencies on record
May 2025
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and Staff interview the facility failed to ensure residents who room together were served lunch in a dignified manner, by not surveying meals at the same time. This was a random o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation and staff interview, the facility failed to ensure privacy and confidentially during medication administration. Facility Census: 28.
Findings Include:
a) Computer on the Medicatio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on Record review and staff interview the facility failed to provide an accurate MDS diagnosis of Parkinsonism. This was found to be true for one (1) of 15 residents whose Minimum Data Set (MDS) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to provide an accurate Pre-admission Screening and Resident Review (PASARR) containing all diagnoses for Resident #22 and #23. Resident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review, staff interview, and resident interview the facility failed to develop or implement a care plan related to nutrition and diagnoses. This failed practice was found true for toe ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation and staff interview, the facility failed to maintain the environment of which it had control over to remain free of accident hazards due to the medication cart being unlocked. Fac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record review, resident representative interview and staff interview, the facility failed to document all meal intake percentages for Resident #26, who was identified with weight loss. This w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident interview, record review and staff interview, the facility failed to offer a pneumococcal vaccination to Resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0628
(Tag F0628)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and staff interview, the facility failed to notify the Medical Power of Attorney (MPOA) in writing of th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations and Staff interview the facility failed to ensure foods were probably labelled and discarded when out of date. This failed practice had the potential to affect more than a limite...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, staff interview, resident interviews, and documentation review, the facility failed to maintain a proper infection prevention and control in the environment. Facility census 28.
...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on observation and staff interview, the facility failed to ensure the tray line milk cooler had proper seals to maintain safe temperatures for the milk/juice by holding it under 40 degrees Fahre...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected most or all residents
Based on observation, record review and staff interview, the facility failed to use appropriate alternatives prior to installing bed rails and failed to assess each resident for the risk of entrapment...
Read full inspector narrative →
Nov 2023
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and staff interview, the facility failed to ensure a dignified dining experience for Resident #1. This was a random opportunity for discovery. Resident identifier: #1. Facility ce...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation and staff interview the facility failed to ensure a call light device was always accessible to Resident #12. This failed practice was a random opportunity for discovery and had th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation and staff interview, the facility failed to provide residents with a safe, clean, comfortable, and homelike environment. Ceiling tiles were observed to be stained in three (3) res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on record review and staff interview, the facility failed to ensure appropriate information was communicated to the recei...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to ensure one (1) of two (2) residents reviewed for the care area of pre-admission screening and resident review (PASARR) were referred ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on record review and staff interviews, the facility failed to ensure the resident's Pre admission Screening and Resident Review (PASARR) reflected pre-admission diagnoses for one (1) of two (2) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview the facility failed to implement care plans
for three (3) of 26 Residents whose care...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on staff interview and record review, the facility failed to revise the care plan after Resident #1's dentures were lost. This was true for one (1) of fifteen residents whose care plans were rev...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, record review and staff interview, the facility failed to ensure a resident receiving oxygen had a physician's order for usage. This was found for one (1) of one (1) Resident rev...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observation, record review, and staff interview the facility failed to administer an extended-release medication within the appropriate guidelines for Resident #1. This failed practice was a ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on observation, policy review, resident council meeting and staff interview the facility failed to make grievances forms accessible to all residents and/or residents family/representatives resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
Based on record review, Resident Council meeting and staff interviews, the facility failed to implement an ongoing resident centered activities program designed to meet the interest of and support the...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected multiple residents
Based on record review and staff interview, the facility failed to have documentation to support ongoing communication, coordination and collaboration between the nursing home and the dialysis center ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on record review and staff interview the facility failed to ensure nurse staffing information was posted on a daily basis. This was a random opportunity for discovery and has the potential to af...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation and staff interview the facility failed to maintain proper infection control standards during wound care. This failed practice was a random opportunity for discovery and had the p...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview the facility failed to administer and complete pneumococcal vaccines series for three...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Data
(Tag F0851)
Could have caused harm · This affected most or all residents
Based on observation and staff interview, the facility failed to ensure licensed nurse staffing information based on payroll information was accurately reported to the Centers for Medicare and Medicai...
Read full inspector narrative →
Apr 2022
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
.
Based on medical record review and staff interview the facility failed to notify a resident representative of a change in condition. This was discovered for one (1) of four (4) residents reviewed fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
.
Based on medical record review and staff interview the facility failed to accurately complete a Minimum Data Set (MDS) assessment for Resident #25 in the area of restraints and alarms. This was foun...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
.
Based on medical record review and staff interview the facility failed to develop an accurate comprehensive person-centered care plan for a resident receiving respiratory services. This was discover...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
.
Based on medical record review and staff interview the facility failed to revise a care plan in the area of fall risk. This was discovered for one (1) of fourteen care plans reviewed during the Long...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
.
Based on medical record review and staff interview, the facility failed to ensure the resident's environment was as free from accident hazards as possible. The medication cart was observed to be unl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
.
Based on observation and staff interview, the facility failed to ensure oxygen therapy was administered in accordance with professional standards of practice. Resident #134's oxygen tubing and humid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
.
Based on medical record review and staff interview, the facility failed to ensure residents were assessed for pneumococcal vaccination status and offered vaccination if appropriate. This was true fo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
.
Based on observation and staff interview the facility failed to properly store food in a safe and sanitary manner in accordance with the professional standards for food service safety. The foods sto...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0885
(Tag F0885)
Could have caused harm · This affected multiple residents
.
Based on medical record review and staff interview, the facility failed to inform all residents, their representatives, and families by 5:00 PM the next calendar day following the occurrence of a si...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • No fines on record. Clean compliance history, better than most West Virginia facilities.
- • 39 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • Grade C (50/100). Below average facility with significant concerns.
About This Facility
What is Montgomery General Hospital's CMS Rating?
CMS assigns MONTGOMERY GENERAL HOSPITAL an overall rating of 2 out of 5 stars, which is considered below average nationally. Within West Virginia, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Montgomery General Hospital Staffed?
CMS rates MONTGOMERY GENERAL HOSPITAL's staffing level at 3 out of 5 stars, which is average compared to other nursing homes.
What Have Inspectors Found at Montgomery General Hospital?
State health inspectors documented 39 deficiencies at MONTGOMERY GENERAL HOSPITAL during 2022 to 2025. These included: 39 with potential for harm.
Who Owns and Operates Montgomery General Hospital?
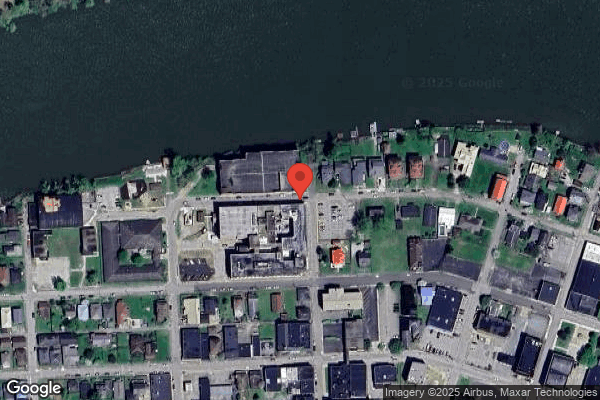
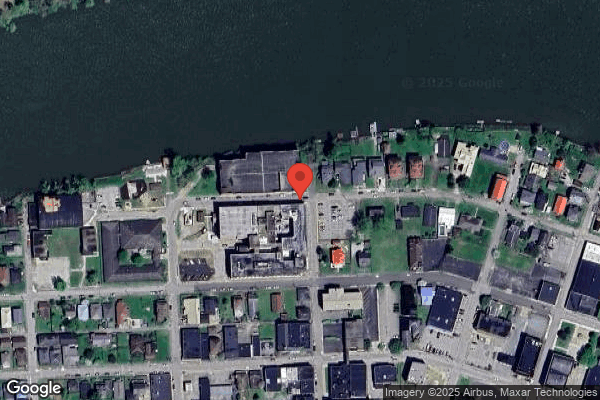
MONTGOMERY GENERAL HOSPITAL is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 44 certified beds and approximately 33 residents (about 75% occupancy), it is a smaller facility located in MONTGOMERY, West Virginia.
How Does Montgomery General Hospital Compare to Other West Virginia Nursing Homes?
Compared to the 100 nursing homes in West Virginia, MONTGOMERY GENERAL HOSPITAL's overall rating (2 stars) is below the state average of 2.7 and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Montgomery General Hospital?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Montgomery General Hospital Safe?
Based on CMS inspection data, MONTGOMERY GENERAL HOSPITAL has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in West Virginia. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Montgomery General Hospital Stick Around?
MONTGOMERY GENERAL HOSPITAL has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Montgomery General Hospital Ever Fined?
MONTGOMERY GENERAL HOSPITAL has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Montgomery General Hospital on Any Federal Watch List?
MONTGOMERY GENERAL HOSPITAL is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.