CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility did not ensure that residents were free from abuse for 2 of 2 (R58 and R237) ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility did not ensure that residents were free from abuse for 2 of 2 (R58 and R237) residents reviewed for sexual abuse. In addition, the facility did not provide a safe resident environment to protect other residents from abuse.
On 6/2/22, R237 reported an allegation of sexual abuse. The facility did not assess R237, did not investigate what occurred, did not implement increased monitoring of the accused R41, did not revised the accused R41's care plan to put measures in place to prevent further abuse.
On 6/11/22, R58 was involved in an incident of sexual abuse by R41. When staff notified R58's family, they asked to have a psychologist talk to R58 due to a history of abuse. The facility did not thoroughly investigate this incident of sexual abuse. The facility placed R41 on 15 minute checks which were not consistently implemented. R41 wheels himself about the facility and staff on different units were not aware of R41 needing supervision. Although not a smoker, R41 goes outside to sit on the patio which is not supervised. In addition, Surveyor was informed R41 had a room change as a result of this incident however; R41 was noted to be residing in the same room.
The facility did not implement interventions to protect residents from abuse.
The facility's failure to keep residents free from sexual abuse due to the facility's inaction after each incident, such as not reporting, not investigating, not assessing and not putting interventions in place to prevent further abuse placed female residents at risk for further abuse and created a situation of immediate jeopardy beginning on 6/2/22.
Administrator A was notified of the immediate jeopardy on 8/11/22 at approximately 12:00 PM.
The immediate jeopardy was removed on 8/19/22; however, the deficient practice continues at a scope and severity level of E (potential for harm/pattern) as the facility continues to implement and monitor its action plan.
Findings include:
The Facility policy titled: Abuse, Neglect and Exploitation revised 7/2022 documents (in part) .
.Policy:
It is the policy of this facility to provide protections for the health, welfare and rights of each resident by developing and implementing written policies and procedures that prohibit and prevent abuse, neglect exploitation and misappropriation of resident property.
Definitions:
Abuse means the willful infliction of injury, unreasonable confinement, intimidation, or punishment with resulting physical harm, pain or mental anguish. Abuse also includes the deprivation by an individual, including a caretaker, of goods or services that are necessary to attain or maintain physical, mental, and psychosocial well-being. Instances of abuse of all residents, irrespective of any mental or physical condition, cause physical harm, pain or mental anguish. It includes verbal abuse, sexual abuse, physical abuse and mental abuse including abuse facilitated or enabled through use of technology.
Willful means the individual must have acted deliberately, not that the individual must have intended to inflict injury or harm.
Sexual Abuse is non-consensual sexual contact of any type with a resident.
Physical Abuse includes, but is not limited to hitting, slapping, punching, biting and kicking. It also includes controlling behavior through corporal punishment.
Mental abuse includes, but is not limited to humiliation, harassment, threats of punishment or deprivation.
Neglect means failure of the facility, its employees or service providers to provide goods and services to a resident that are necessary to avoid physical harm, pain, mental anguish or emotional distress.
Mistreatment means inappropriate treatment or exploitation of a resident.
III. Prevention of Abuse, Neglect and Exploitation
The facility will implement policies and procedures to prevent and prohibit all types of abuse, neglect, misappropriation of resident property and exploitation that achieves:
A. Establishing a safe environment that supports, to the extent possible, a resident's consensual sexual relationship and by establishing policies and protocols for preventing sexual abuse, such as the identify when, how, and by whom determinations of capacity to consent to a sexual contact will be made and where this documentation will be recorded; and the resident's right to establish a relationship with another individual, which may include the development of or the presence of an ongoing sexually intimate relationship.
D. The identification, ongoing assessment, care planning for appropriate interventions, and monitoring of residents with needs and behaviors which might lead to conflict or neglect.
F. Providing residents, representatives and staff information on how and to whom they may report concerns, incidents and grievances without the fear of retribution; and providing feedback regarding the concerns that have been expressed.
V. Investigation of Alleged Abuse, Neglect and Exploitation
A. An immediate investigation is warranted when suspicion of abuse, neglect or exploitation, or reports of abuse neglect or exploitation occur.
B. Written procedures for investigations include:
1. Identifying staff responsible for the investigation;
3. Investigating different types of alleged violations;
4. Identifying and interviewing all involved persons, including the alleged victim, alleged perpetrator, witnesses, and others who might have knowledge of the allegations.
5. Focusing the investigation on determining if abuse, neglect, exploitation and/or mistreatment has occurred, the extent, and cause, and;
6. Providing complete and thorough documentation of the investigation.
VI. Protection of Resident
The facility will make efforts to ensure all residents are protected from physical and psychosocial harm during and after the investigation. Examples include but are not limited to:
A. Responding immediately to protect the alleged victim and integrity of the investigation.
B. Examining the alleged victim for any sign of injury, including a physical examination or psychosocial assessment if needed;
C. Increased supervision of the alleged victim and residents;
D. Room or staffing changes, if necessary, to protect the resident(s) from the alleged perpetrator;
E. Protection from retaliation;
F. Providing emotional support and counseling to the resident during during and after the investigation, as needed.
VII. Reporting/Response
1. Reporting of alleged violations to the Administrator, state agency, adult protective services, and to all other required agencies (e.g., law enforcement when applicable) within specified timeframe's:
a. Immediately, but not later than 2 hours after the allegation is made, if the events that cause the allegation involve abuse or result in serious bodily injury, or
b. Not later than 24 hours if the events that cause the allegation do not involve abuse and do not result in serious bodily injury.
2. Assuring that reporters are free from retaliation or reprisal;
4. Taking all necessary actions as a result if the investigation, which may include, but are not limited to, the following:
a. Analyzing the occurrence(s) to determine why abuse, neglect occurred and what changes are needed to prevent further occurrences;
b. Defining how care provision will be changed and/or improved to protect residents receiving services;
c. Training of staff on changes made and demonstration of staff competency after training is implemented;
d. Identification of staff responsible for implementation of corrective actions;
e. The expected date for implementation; and
f. Identification of staff responsible for monitoring the implementation of the plan.
R41 was involved in 2 alleged sexual abouse allegations with the first incident occurring on 6/2/22 involving R237 and a second incident occurring on 6/11/22 involving R58.
R41 was admitted to the facility on [DATE] and has diagnoses that include Alzheimer's Disease and Dementia. R41's Annual Minimum Data Set (MDS) dated [DATE] documents a Brief Interview for Mental Status score of 11 indicating moderate cognitive impairment for daily decision making skills.
R41's daughter was Power of Attorney (POA) until an Incapacity assessment dated [DATE] recommendations documented: De-activate POA for Healthcare. Is able to evaluate information well enough to give informed consent.
R41's Annual Minimum Data Set (MDS) dated [DATE] section E0200: Behavioral Symptoms - Presence & Frequency documents: A. Physical behavioral symptoms directed towards others (e.g., hitting, kicking, pushing, scratching, grabbing, abusing others sexually) - 0. Behavior not exhibited
R237 admitted to the facility on [DATE] and discharged on 6/30/22. Diagnoses included: Attention Deficit Hyperactivity Disorder, Dementia, Major Depressive Disorder and Rheumatoid Arthritis.
R237's BIMS dated 6/23/22 documented a score of 13 - indicating R237 as cognitively intact for daily decision making skills.
R58 admitted to the facility on [DATE] and has diagnoses that include: Schizophrenia, Major Depressive Disorder and Anxiety Disorder.
R58's Quarterly MDS dated [DATE] documents a BIMS score of 15 - indicating cognitively intact for daily decision making skills.
During review of a Facility Reported Incident dated 6/11/22 (which involved R41), Surveyor located progress notes entered on 6/4/22, which documented the Nurse Practitioner was called to inform about accusations against R41.
Surveyor asked Director of Nursing (DON)-B about the progress notes on 6/4/22 which documented accusations against R41 and monitoring closely due to accusations. Surveyor asked DON-B if R41 had previous incidents of sexual abuse. DON-B stated, Well, there was one time when he touched or rubbed another female residents' arm. Surveyor asked what accusation the progress notes on 6/4/22 was referring to. DON-B reported he did not know, but will find out. No additional information was provided by DON-B.
Nursing Home Administrator (NHA)-A provided Surveyor with a Facility Reported Incident dated 6/4/22. This Facility Reported Incident included the following;
Clinical Care Manager (CCM)-K statement dated 6/4/22 documents,
On 6/2/22 (R237) reported to me that a male resident kissed her on the cheek. R237 did not know who the resident was and reported it did not really bother her. Surveyor noted CCM-K did not get a full statement from R237 about what had occurred and did not follow up or investigate the allegation regarding R237 allegedly reporting being kissed on the cheek.
On 6/3/22 when CCM-K was leaving the building, R237 informed CCM-K she knew who the resident was. CCM-K stated: OK, you could let me know when I return. Surveyor noted although R237 informed CCM-K she could identify the resident involved in the alleged sexual abuse, CCM-K did not follow up or investigate the allegation.
On 6/4/22 CCM-K received a call from the Registered Nurse (RN) stating that R237 is telling them that the man touched her nightgown that day (6/2/22) also. CCM-K interviewed R237 on the phone and R237 stated R41 came into her room, lifted her nightgown and pointed at her private area and gestured for her to move her leg. R237 reported he lifted up the night gown, pointed at her private area, smiled and said me and you like he wanted sex. He kissed her cheek and she told him no way and to go away.
CCM-K's statement further documented DON-B was notified and she was directed to tell the RN to do the follow-up. There was no evidence an assessment was completed on R237 to determine her ability to consent.
Surveyor noted there was no follow up or thorough investigation related to the allegation of sexual abuse involving R237 and R41.
R41 does not have a care plan related to sexual behaviors. There was no evidence of increased monitoring of R41. There was no psychiatric or psychotherapy interventions to determine the possible cause of R41's behavior. There was no evidence the facility implemented any interventions following the incident on 6/2/22 to keep R237 and other residents safe, placing other residents in the facility at risk for sexual abuse.
Nine days later, on 6/11/22, another incident of sexual abuse occurred, this time between R41 and a different female resident (R58).
Graduate Practical Nurse (GPN)-E's statement documented she was walking down the hall and noticed R58 sitting on the couch. R41 was sitting behind R58 with his hand in the back of her brief near her butt. GPN-E told R41 to take his hand out R58's pants. The residents were separated and went back to their rooms. R58 was asked if she was OK and she reported yes, he was just rubbing my back. GPN-E reported the incident to the Supervisor.
Surveyor was unable to locate evidence an interview was completed with R58 following the incident.
There was no assessment of R58 to determine her ability to consent.
On 8/8/22 at 1:30 PM Surveyor asked DON-B if he had any additional information regarding the investigation and incident between R41 and R58. DON-B reported he did not have any additional information. Surveyor advised the investigation did not include an interview with R58, and asked if there were any other staff or resident interviews. DON-B stated, I guess there isn't.
On 8/7/22 at 2:19 PM Surveyor spoke with R58 in her room about the incident involving R41. R58 reported she was in the TV room and R41 placed his right hand near her groin (demonstrating with her right hand). Surveyor asked if R41's hand was on the inside or outside of her pants, to which she stated, Inside. R58 reported she did not ask R41 to put his hand in her pants, but did not tell him no, and did not stop him. R58 reported she let him do it for awhile, then told him to stop after a couple minutes. Surveyor asked if this bothered her, R58 replied, No. It's fine. I'm a grown woman.
On 8/9/22 NHA-A provided an interview with R58 dated 6/11/22.
Licensed Practical Nurse (LPN)-N statement documented, On 6/11/22 at roughly 3 :00 PM, she interviewed R58. R58 was asked how she was feeling, which she reported fine. She was asked about the interaction with R41. R58 reported he started to rub her shoulders and back, she liked it and it felt good. She did not ask him to do this. She stated he was touching inside the front of her pants. She reported she was not sad, upset or scared. LPN-N reassured her she did nothing wrong, and she was safe.
Registered Nurse (RN)-O statement dated 6/11/22 documented he spoke to DON-B and was informed to keep the residents separated and start 15 minute checks for R41. RN-O called R58's son and daughter-in-law. Family in agreement but added that resident (R58) has had similar issues in her past and they would like to have psychologist talk with resident during the next visit to the facility.
R58's Psychiatric consult dated 7/8/22 documents (in part) .resident states doing good, feels mental health is stable, does not want medications adjusted. Denies auditory or visual hallucinations. Surveyor noted there was no mention of the sexual abuse incident between R58 and R41.
After reviewing the 6/11/22 Facility Reported Incident, Surveyor spoke with DON-B who stated, Staff was there and said they were both being flirty with each other.
Surveyor located no documentation in the facility self report or staff statements to support this statement. DON-B reported staff intervened when it turned to inappropriate touching. Surveyor asked DON-B if he interviewed the residents involved. DON-B stared at Surveyor and did not answer. After a long pause, DON-B reported he would look to see if there was any more information somewhere else. Surveyor asked if R41 speaks English. DON-B reported he does speak English, but has some cognitive deficits. Surveyor asked DON-B what was done after the incident. DON-B reported R41 was moved to another unit and 15 minute checks were initiated.
Surveyor noted the facility made no revisions to R41's care plan following either sexual abuse incident on 6/2/22 or 6/11/22. R41 has no care plan interventions related to sexually inappropriate behavior, and no care plan about 15 minute checks or increased monitoring. R41's Certified Nursing Assistant (CNA) care card did not include documentation of behaviors or increased monitoring.
CNA behavior charting included a standard template which included a column sexually inappropriate which Surveyor noted included no check marks for the past 30 days. There was no documentation of any further inappropriate sexual behavior or wandering into other resident rooms since the last incident on 6/11/22.
DON-B reported R41 transferred rooms after the incident on 6/11/22. Surveyor's review of R41's census revealed R41 has resided in the same room (on Skylight East) since November 2021 and was not moved as DON-B reported. In addition, 15 minute checks were not consistently completed. Surveyor's review of documentation revealed 15 minute check forms missing for 6/21/22, 6/28/22, 6/29/22, 6/30/22, 7/18/22, 7/22/22 and 7/25/22.
Surveyor reviewed 5 random 15 minute check forms for R41 which revealed incomplete documentation, indicating monitoring of R41 was not consistently completed:
Time started at midnight through 11:45 PM:
6/16/22 - blank/no entry of monitoring for the hours of 7:30 AM - 2:45 PM.
6/22/22 - blank/no entry of monitoring for the hours of Midnight - 6:15 AM or 3:15 PM - 11:45 PM.
6/27/22 - blank/no entry of monitoring for the hours of Midnight - 6:15 AM or 3:15 PM - 11:45 PM.
7/9/22 - blank/no entry of monitoring for the hours of Midnight - 2:30 PM.
7/23/22 - blank/no entry of monitoring for the hours of 6:45 AM - 2:45 PM.
On 8/8/22 at 11:10 AM Surveyor spoke with Certified Medication Aid (CMA)-D who works on Skylight north (back of building where R41 resides). CMA-D reported she is familiar with R41. She reported R41 is on 15 minute checks and stated, We all know if he's up and around in his wheelchair to keep eye on him, he can be a little grabby with women.
On 8/8/22 at 11:23 AM Surveyor spoke with Graduate Practical Nurse (GPN)-E who works on R58's unit. GPN-E reported she is familiar with R41 and who stated, Oh yes, I am very aware of (R41), he's on 15 minute checks. Surveyor asked if this is documented anywhere. GPN-E stated, Not really, pretty much everyone knows to keep eye when he is tooling around in his wheelchair.
Surveyor asked GPN-E if she knew why R41 was to be monitored, to which she replied, He's had some incidents with some of the female residents. When asked what type of incidents, GPN-E stated, Touching them.
On 8/8/22 at 11: 35 AM Surveyor spoke with RN-F who works on the Heritage unit (front of building near entrance). RN-F reported she knows who R41 is stating, I know he wheels himself around in the wheelchair. RN-F reported R41 does come to the front of the facility, on the Heritage unit, and she sometimes sees him go outside to sit. Surveyor asked RN-F if she has been informed of anything else regarding R41 such as increased monitoring, to which she replied, No.
Surveyor had observations of R41 sitting alone outside near the front entrance of the facility while on Survey.
On 8/10/22 at 2:11 PM Surveyor spoke with the Social Service Director (SSD)-C and asked what she could tell about the incident on 6/11/22 involving R41 and R58. SSD-C stated, Well, I know he tried to kiss her, and that's about it. SSD-C denied knowing anything else about the incident and reported DON-B was more involved. Surveyor asked SSD-C about the statement from R58's family that she has had similar issues in her past and they would like to have psychologist talk with her. Surveyor asked if she knew what issues the family was referring to. SSD-C stated, No, but maybe it has to do with her ex-husband taking advantage of her. When asked what she meant, SSD-C stated, Her sister-in-law told me her ex-husband took advantage of her sexually and she did not want her ex-husband to be allowed to take her out of the facility. SSD-C reported this conversation occurred after R58 was admitted to the facility and before the sexual incident between R58 and R41.
The facility was aware of R58's history of sexual abuse and the care plan was not revised to include information or interventions related to her previous sexual abuse.
The facility was aware of the allegation of sexual abuse that occurred between R41 and R237 on 6/2/22. The facility did not complete a thorough investigation of the allegation and no interventions were implemented to keep R237 and other residents safe.
Nine days later a second incident involving sexual abuse occurred this time between R41 and R58, with R58 having a history of sexual abuse by her ex-husband. The facility did not complete a thorough investigation and appropriate interventions were not implemented to keep R58 and other residents safe. R41 is mobile throughout the facility and staff on other units are not aware of his sexual behavior and increased monitoring, placing other vulnerable residents at risk.
Neither R237 nor R58 appeared overly distressed or upset by what had occurred. R58 even stated that it didn't bother her - she was a grown woman. It should be noted, however, given R58's history of sexual abuse, that she may have been used to being used and abused and that this was a familiar pattern to her to which she was accustomed. Her reaction was markedly incongruent to what a reasonable person might experience. Using the reasonable person concept, R58 or any other resident who is sexually abused could feel Recurrent (i.e., more than isolated or fleeting) debilitating fear/anxiety that may be manifested as panic, immobilization, screaming, and/or extremely aggressive or agitated behavior(s) (e.g., trembling, cowering) in response to an identifiable situation (e.g., approach of a specific staff member). A person who has been sexually assaulted could also experience Ongoing, persistent expression of dehumanization or humiliation in response to an identifiable situation .
The failure of the facility to keep residents free from sexual abuse due to the facility's inaction after each incident, such as not reporting, not investigating, not assessing and not putting interventions in place to prevent further abuse placed female residents at risk for further abuse. This created a reasonable likelihood for serious harm and, thus, created a finding of immediate jeopardy beginning on 6/2/22.
The immediate jeopardy was removed on 8/19/22 when the facility:
Medication reviews were conducted, psych evaluations conducted and the Medical Doctor reviewed the residents identified in this deficiency.
Education Policy and procedural updates were completed and non-Pharmacological Interventions identified for clinical staff. Staffing changes were made to protect the residents from the alleged perpetrator. Per policy on Abuse, Neglect, and Exploitation increased supervision was provided for the perpetrator.
A policy for Sexual Expression for residents was developed, brought through the Quality Assurance Program Improvement (QAPI), implemented and educated on.
Staff were educated on the policy for Sexual Expression of Residents as well as abuse, neglect and exploitation, and compliance with reporting allegations of abuse/neglect/exploitation.
Social Service, ADON, Unit Managers, Administrator and Associate Administrator received training trained on Sexuality and Intimacy in Long Term Care.
Assessments were completed for all residents using sexual expression assessment.
A care conference will be held for residents following the display of sexual expression where it will be determined the capacity of consent and review of solution that best meets the needs of and the protection of those involved.
Care plan audit were conducted for residents identified through sexual expression assessment with
updates as needed. Cardex Updates were completed for all residents identified through sexual expression assessment.
Residents displaying inappropriate sexual behaviors will be referred for a psychologist consult.
Any state reported incident will be evaluated through the RISK process as well as APIA.
APIA will review residents who triggered sexual expression assessment with the
Medical Director.
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility did not ensure 3 (R56, R12 and R71) of 3 residents received adequate supervision by staff to prevent accidents
*R56...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility did not ensure 3 (R56, R12 and R71) of 3 residents received adequate supervision by staff to prevent accidents
*R56 is severely cognitively impaired and was identified to be at high risk for elopement. R56 eloped from the facility on 5/31/22 after a staff person disabled the wanderguard alarm because of the number of times R56 had set it off. R56 was found approximately 1 mile from the facility without proper footwear in rainy weather. Staff was not aware that R56 had left the building for approximately 75 minutes before they noticed her missing and local law enforcement.
The facility's failure to ensure a door alarm was activated to alert staff if a resident with a Wanderguard bracelet attempted to leave out the door, the failure to have a care planned approach to monitor/supervise R56's whereabouts, the failure to know of R56's whereabouts and to conduct a thorough investigation into the elopement created a condition of an immediate jeopardy starting on 5/31/22.
The immediate jeopardy began on 5/31/22. NHA (Nursing Home Administrator)-A was notified of the immediate jeopardy on 8/11/22 at 12:00 PM. The immediate jeopardy was removed on 8/19/22.
The deficient practice continues at a scope and severity level of E (potential for harm/pattern) as the facility continues to implement and monitor the effectiveness of their removal plan and as evidenced by the following noncompliance for R12 and R71.
* The facility did not conduct a through investigation when facility staff spilled a hot beverage on R12's lap.
* R71 was admitted with a fractured neck following a fall at assisted living and wears a cervical collar. R71 fell 15 times in 4.5 months following admission. The facility did not conduct through investigations of R71's falls including a root cause analysis and did not revise R71's care plan to reduce the risk of further falls and injury.
Findings include:
1. R56 was admitted to the facility on [DATE] with diagnoses of subdural hemorrhage, metabolic encephalopathy and dementia without behavioral disturbance.
R56's admission MDS (Minimum Data Set) assessment dated [DATE] documents a BIMS (Brief Interview for Mental Status) score of 03, indicating R56 is severely impaired for daily decision making skills. R56's admission MDS indicates resident requires supervision to limited assistance with activities of daily living including transfers and ambulation. Resident's gait is coded as not stable but able to stabilize without staff assistance. R56 does not require the use of mobility devices. R56's admission MDS indicates R56 exhibits wandering behavior on a daily basis.
An Elopement assessment dated [DATE] indicates R56 is at risk for elopement.
R56's comprehensive care plan dated 5/24/22 indicates resident is at risk for falls and includes intervention of wearing proper footwear when out of bed. R56's comprehensive care plan dated 3/28/22 indicates R56 is at risk for elopement due to attempts to leave facility. Interventions include;
Redirection of [R56] from exit doors,
Distract from wandering with pleasant diversion including offering activities and snacks, and Placement of Wanderguard bracelet to the left ankle.
R56's Wanderguard is to be checked for placement every shift and checked for function on night shift by nursing staff. This is being documented by nursing staff on the R56's MAR (Medication Administration Record).
Surveyor reviewed R56's medical record. Surveyor noted a Facility self report dated 6/7/22. The facility's self report indicates on 5/31/22 at 10:23 PM, R56 was found to be missing by facility staff. ADON (Assistant Director of Nursing)-H via phone directed nursing staff to initiate a missing resident code at the facility and to call local law enforcement. ADON-H notified DON (Director of Nursing)-B. NHA (Nursing Home Administrator)-A was notified of missing resident via phone.
Per Police report, officers arrived at the facility on 5/31/22 at approximately 10:34 PM. Facility staff showed police officers the facility's wandering book which included photos of R56.
On 5/31/22 at approximately 10:37 PM, Police were called to investigate a suspicious person from a concerned citizen in the community. Officers found R56 approximately 1 mile from the facility wearing a hooded sweatshirt, pants and stocking feet with no shoes.
Police returned R56 to the facility on 5/31/22 at approximately 11:00 PM. A head to toe assessment was conducted upon resident's return which found resident to be without injury. Residents pants and socks were notably soiled with mud as it had been raining off and on during the evening of 5/31/22.
Surveyor noted the National Weather Service indicated that the lowest recorded temperature on 5/31/22 was 57 degrees Fahrenheit. Surveyor could not confirm through documentation or interviews conducted by facility staff that R56 had been seen on 5/31/22 after 6:30 PM.
On 8/10/22 at 4:00 PM, Surveyor met with NHA-A to discuss R56's elopement and elopement investigation. Surveyor asked NHA-A if the facility has cameras for surveillance. NHA-A informed Surveyor on 5/31/22 an agency nurse presumably became annoyed with the number of times R56 set off the Wanderguard alarm to the doorway at the end of the hall, and she turned off the alarm. NHA-A reported they had video footage of a former agency nurse, who is no longer employed by the facility, disabling the skylight north exit doors code alert system, leaving the exit without an engaged alarm.
Surveyor noted there were 4 residents with Wanderguard bracelets on this unit; all would have had the opportunity to leave out the unalarmed door at the end of the unit.
Surveyor asked NHA-A if they had conducted interviews of facility staff who worked on 5/31/22 in relation to R56's elopement. NHA-A told Surveyor that it hadn't occurred to him to interview staff because of the video footage of the individual eloping through the Skylight North exit door. NHA-A reported R56 was in the facility until approximately 9:15 PM when there was footage of an individual exiting through the Skylight North exit door. Surveyor asked how it was confirmed that the exiting individual was R56. NHA-A told Surveyor that it was difficult to see the camera footage due to condensation on the camera lens from rain. NHA-A indicated at 10:30 PM staff noticed R56 was missing and were unable to find him in the building. The LPN called ADON-H who instructed LPN to initiate a code and to call local law enforcement. Police arrived at 10:34 PM. Police responded to a call placed by a concerned citizen and located R56. The police returned R56 to the facility on 5/31/22 at about 11:00 PM. R56 was not injured.
On 8/10/22 at 10:05 AM, Surveyor interviewed Maintenance Director-U. Surveyor asked Maintenance Director-U who is responsible for checking the functionality of the facility's code alert system. Maintenance Director-U informed surveyor that they had not been checking the facility's exit doors for code alert functioning until 8/8/22. Maintenance Director-U informed surveyor that they are planning to check exit doors for code alert system every Monday, Wednesday, and Friday.
On 8/10/22 at 1:35 PM, Clinical Care Manager-K was interviewed by Surveyor. Surveyor asked Clinical Care Manager-K how nursing staff would know how to identify a resident who is at risk for elopement. Clinical Care Manager-K told Surveyor that residents who wander would be listed in the facility's wander books, which are available at the main entrance, activity department, maintenance department, kitchen and nursing station. The wander books include resident photos, demographic information and location of their Wanderguard devices. Surveyor asked Clinical Care Manager-K how often a resident who is at risk for elopement should be checked on by staff. Clinical Care Manager-K told Surveyor that if a resident is at risk for elopement that they should be checked on frequently. Surveyor asked Clinical Care Manager-K to define what frequently would mean to them. Clinical Care Manager-K told Surveyor that they would expect a resident at risk for elopement to be checked on about every 15 minutes.
On 8/10/22 at 3:20 PM, Surveyor conducted an interview with ADON-H. Surveyor asked ADON-H how nursing staff would know how to identify a resident who is at risk for elopement. ADON-H told Surveyor that residents who wander would be listed in the facility's wander books. Surveyor asked ADON-H how often a resident who is at risk for elopement should be checked on by staff. ADON-H K told Surveyor that if a resident is at risk for elopement that they should be checked on at least every half hour. Surveyor asked ADON-H what they had recalled about R56's elopement on 5/31/22. ADON-H told Surveyor that they had not been in the building at the time of R56's elopement but received a call from facility staff asking for direction. ADON-H had spoken to a nurse who is no longer is employed by the facility and directed them to initiate a wandering code at the facility and to call the police. ADON-H then notified DON-B. ADON-H did not have any further involvement related to R56's elopement investigation.
Surveyor asked NHA-A how often the code alert system should be checked for functioning. NHA-A says that they would like the system checked daily but knows that it has not recently been checked daily due to changes in maintenance staff. NHA-A told surveyor that they are in negotiations to upgrade the code alert system at this time as their system is antiquated.
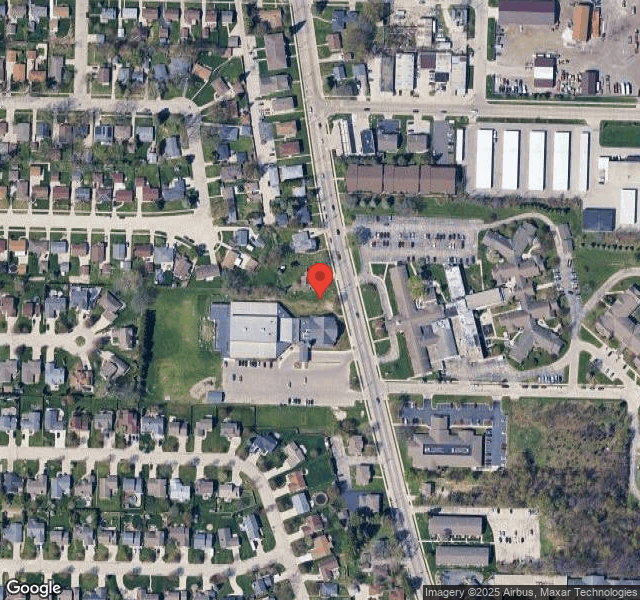
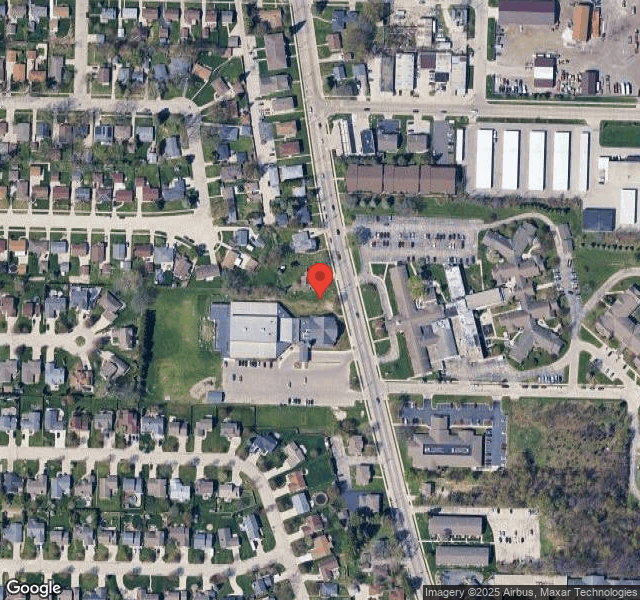
Surveyor shared concerns related to R56's elopement on 5/31/22 related to the facility's inability to identify when R56 was last checked on and staff disabling the facility's door alarm system allowing for R56 to elope without the door alarm sounding. R56 wandered approximately 1 mile from the facility while raining without appropriate footwear. This facility is also located on a high traffic state highway.
R56's elopement care plan was not updated after R56's elopement on 5/31/22, which causes continued concern for R56's safety.
The facility's failure to ensure a door alarm was activated to alert staff if a resident with a Wanderguard bracelet attempted to leave out the door, the failure to have a care planned approach to monitor/supervise R56's whereabouts, the failure to know of R56's whereabouts, and the failure to conduct a thorough investigation into the elopement created a reasonable likelihood for serious harm given R56's cognitive status and the facts that R56 was outside at night in rainy conditions. This led to a finding of immediate jeopardy starting on 5/31/22.
The IJ was removed on 8/18/22 when;
~ Assessments were conducted for all residents identified to be at risk for wandering.
~ Orders were updated to include Wander Guard Placement for all residents who need wander guards.
~ Care plan audits were conducted for all residents identified to be at risk for wandering.
Cardexs were updates for all residents identified to be at risk for wandering.
~ The facility's Wander books were updated including policy and demographics. The Wanderguard books were updated to include distractions specific to each resident at risk. Structured activities, diversions, re-orientations strategies, food, television and conversations for identified residents.
~ 15 minute checks for preventative measures were implemented for resident identified in this deficiency.
~ Education for all staff on Elopement and Wandering resident policy was completed including tips for elopement prevention. Non-Pharmacological interventions were discussed for nursing staff.
~ The Procedure for wander/door alarm inspection for maintenance was updated.
Nursing staff demonstrated deactivation and activation of the door alarm system.
Alarm keys were removed from all key rings but for the supervising nurse set and DON.
The door alarm will be replaced when able.
~ Elopement drills will be performed weekly X4, bi-weekly X2 months, monthly X3, and quarterly thereafter for 6 months. Results will be brought through Quality Assurance Process Improvement (QAPI).
~ Door alarm audits daily for 30 days and 3 x week for 11 months. Results will be brought through QAPI. QAPI to review quarterly residents at risk for wandering with the Medical Director.
The deficient practice continues at a scope and severity level of E (potential for harm/pattern) as evidenced by;
2. On 8/7/22 at 11:20 a.m. R12 informed Surveyor about three or four months ago she received a burn on her leg. Surveyor inquired what had happened. R12 explained a dietary worker was bringing in her tray, the cup of coffee was knocked over and scalded her legs. R12 indicated there was a sheet and blankets over her legs and she couldn't take the blanket off which was full of hot coffee. R12 informed Surveyor the dietary worker didn't know what to do and she asked him to take off the sheet.
The nurses note dated 4/8/22 documents when staff brought her supper tray to her room res (resident) moved her TV tray and a cup of coffee spilled on her right lower leg no redness noted no blisters applied cold wash cloth to area immediately, no increase in warmth to area. 3 blankets were on res at the time the coffee spilled on res, res requested to go to ER (emergency room) writer called [name of] her son and made aware. [name of] NP (nurse practitioner) aware [name of] ambulance called to transport to ER (emergency room). RN (Registered Nurse) supervisor was present with writer for skin check.
The nurses note dated 4/8/22 documents, On call RN made aware of res going to ER and the spilled coffee that occurred.
The nurses note dated 4/8/22 documents res returned to facility. right lower leg wrap with kerlix and Vaseline gauze. res had no c/o (no complaint) pain or discomfort at this time. new order received.
The hospital after visit summary dated 4/8/22 under diagnoses documents thermal burn & superficial burn of right lower leg, initial encounter.
The physician order with an order date of 4/8/22 includes a treatment of cleanse right lower leg with normal saline, pat dry, apply Vaseline gauze and wrap with kerlix daily. This treatment was discontinued on 5/9/22.
The nurses note dated 4/9/22 documents, Resident in good spirits. No c/o discomfort to RL (right lower) calf. Area that sustained burn is wrapped. Res stated they told her to leave wrap on a few days. She also stated that the bed she was in at hosp (hospital) had a scale and she weighed 55kg (kilograms).
The nurses note dated 4/9/22 documents, Resident monitored for RLE (right lower extremity). Lower leg is wrapped. No drainage. Complaining of burning sensation. Given Tylenol for comfort twice this evening.
The nurses note dated 4/10/22 documents, Pt (patient) is being followed for RLE where coffee got spilled. Pt is alert and orientated per baseline. RLE wrapped. Pt has no c/o pain or discomfort at this time. Pt is in bed sleeping.
The dietary note dated 4/11/22 includes documentation of Resident is being followed for coffee got spilled, resident agreed to special mug with cover for beverages. Kitchen aware.
On 8/8/22 at 1:41 p.m. Surveyor asked CCM (Clinical Care Manager)-K if she was aware of R12 being burned by spilled coffee. CCM-K informed Surveyor apparently there was a day the tray tipped in the room and R12 was burned with coffee. CCM-K informed Surveyor she was not working that day but knows R12 was on report after.
On 8/8/22 at approximately 3:00 p.m. Surveyor asked Administrator-A for the Facility's investigation regarding R12 being burned by coffee.
On 8/9/22 at 8:42 a.m. Surveyor asked Administrator-A if there is an investigation for when R12 was burned by spilled coffee. Administrator-A informed Surveyor he is still looking for the investigation and wasn't aware of the incident until yesterday.
On 8/9/22 at 12:52 p.m. Surveyor asked Administrator-A if he was able to locate an investigation for R12. Administrator-A informed Surveyor he has an IRIS which is the Facility's incident report which he will bring to Surveyor.
On 8/9/22 at 1:03 p.m., Surveyor reviewed the Facility's incident report dated 4/8/22 which documents for initial reported description, When staff brought her supper tray to her room res (resident) moved her TV tray and a cup of coffee spilled on her right lower leg no redness noted no blisters applied cold wash cloth to area immediately. no increase in warmth to area. 3 blankets were on res at the time of the coffee spilled on res. res requested to go to ER (emergency room) writer called [name of] her son and made aware. [Name of] NP (Nurse Practitioner) aware [name of]ambulance called to transport to ER. RN supervisor was present with writer for skin check.
Under immediate action reported documents cool wash cloth applied blankets removed skin check done.
Under section for review follow up for contributing factors is checked for Patient/Family - Failure to Follow Plan of Care.
The Facility did not investigate R12's burn caused by spilled coffee to prevent further occurrences to R12 or other Residents. There is no evidence the Facility investigated the temperature of coffee when Residents receive this beverage to determine if the temperature is too hot, if there are other Residents at risk and what interventions were implemented to prevent this occurrence to other Residents.
3. The Fall and Fall Risk, Managing Policy from 2001 Med-Pass Inc (Revised March 2018) under the section Resident-Centered Approaches to Managing Falls and Fall Risk documents If falling recurs despite initial interventions, staff will implement additional or different interventions, or indicate why the current approach remains relevant.
R71 was admitted to the facility on [DATE] with diagnoses which includes dementia with behavioral disturbances, hypertension, anxiety disorder, panic disorder, and depressive disorder.
The at risk for injury related to falls care plan initiated 3/1/22 & revised 6/6/22 has the following approaches:
* Encourage me frequently to ask for assistance or use call bell for any assistance. Initiated & revised 3/1/22.
* Encourage me to be in common areas when I am awake. Initiated & revised on 3/1/22.
* Encourage me to walk short distances assisted by staff when physically able, to avoid attempting self ambulation. Initiated 7/13/22.
* Insure Broda Chair is reclined to prevent falling forward. Initiated 6/14/22.
* Please check and change or toilet me every midnight to prevent me from self transferring or self toileting d/t TTWB (toe touch weight bearing) status and to prevent falls or injuries. Initiated & revised 3/1/22.
* Provide frequent reminders to ask for assistance, rather than attempting to provide self care. Initiated 5/17/22.
* Resident was moved to room closer to nurses station. Initiated 3/2/22.
* Safety mat next to bed to prevent injury. Initiated 6/4/22.
* PT (physical therapy) evaluate and treat as ordered or PRN (as needed). Initiated & revised 3/1/22.
* Be sure my call light is within reach when I am in my room and encourage me to use it before attempting to transfer. Initiated & revised 3/1/22.
* Educate me/family/caregivers about safety reminders and what to do if a fall occurs. Initiated & revised 3/1/22.
* I need activities that minimize the potential for falls while providing diversion and distraction. Initiated & revised 3/1/22.
* I need to be evaluated for, and supplied appropriate adaptive equipment or devices as needed. Re-evaluate and as needed for continued appropriateness. Initiated & revised 3/1/22.
* Encourage me to participate in activities that promote exercise, physical activity for strengthening and improved mobility as tolerated. Initiated & revised 3/1/22.
* Ensure that I am wearing appropriate footwear when out of bed. Initiated & revised 3/1/22
* Make sure that my floor/path is clutter free and properly lighted. Initiated & revised 3/1/22.
* Keep my bed in low position when I am in it to prevent me from rolling out and being injured. Initiated 3/1/22.
The actual fall with no injury care plan initiated & revised on 3/1/22 includes approaches of:
* Continue interventions on the at risk plan. Initiated & revised 3/1/22.
* For no apparent acute injury, determine and address causative factors of the fall. Initiated & revised 3/1/22.
* Keep resident in common areas when awake for safety due to severe dementia and anxiety. Initiated & revised 3/1/22.
* Monitor/document/report PRN ( as needed) x (times ) 72h (hour) to MD (medical doctor) for s/sx (signs/symptoms): Pain, bruises, change in mental status, New onset: confusion, sleepiness, inability to maintain posture, agitation. Initiated & revised 3/1/22.
* Neuro-checks x 5 hours. Initiated & revised 3/1/22.
* Pharmacy consult to evaluate medications. Initiated & revised 3/1/22.
* Promote activities that promote exercise and strength building where possible. Provide 1:1 activities if bed bound. Initiated & revised 3/1/22.
* PT (physical therapy) consult for strength and mobility. Initiated & revised 3/1/22.
The admission MDS (Minimum Data Set) with an assessment reference date of 3/2/22 has a BIMS (brief interview mental status) score of 13 which indicates cognitively intact. R71 requires extensive assistance with two plus person physical assist for bed mobility, transfer, & toilet use, ambulated in room once or twice with two plus person physical assist, is occasionally incontinent of urine and continent of bowel. R71 is coded as having fallen within one month of admission, fell during two to six months prior to admission and had a fracture related to a fall in the six months prior to admission. R71 has fallen since admission with no injury.
The Fall CAA (Care Area Assessment) dated 3/11/22 under analysis of findings for nature of the problem/condition documents [AGE] year old female patient with Dx (diagnoses) of multiple fractures, dementia, HTN (hypertension), anxiety, depression, GERD (gastroesophageal reflux), failure to thrive, DM2 (diabetes mellitus), HLD (hyperlipidemia), Vitamin D deficiency, insomonia, and glaucoma admitted to facility status post fall who demonstrates decreased mobility, weakness, and pain. Patient had unwitnessed fall in room on 3/1/22; was sent to ER (emergency room) for evaluation with no injury noted. CAA triggered due to need for staff assistance to stabilize during transfers and ambulation, recent history of fall with fracture prior to admission, fall in facility post admission, and use of antianxiety and antidepressant medications.
The fall risk assessment dated [DATE], 3/15/22, 3/17/22, 3/26/22, 3/27/22, 4/12/22, 4/18/22, 5/12/22, 5/16/22, 6/4/22, 6/8/22, 6/13/22 & 7/13/22 all have scores indicating R71 is at high risk for falls with the exception of 4/6/22 which has a score indicating moderate risk.
The nurses note dated 3/1/22 documents Resident is alert and can make needs known. Resident tried self transferring several times. Resident also had complaints of wanting to go to the bathroom, and was toileted several times with 2 outputs. No complaints of pain, burning or any discomfort with urination. Resident has a neck collar on that should remain on at all times. Resident is a high fall risk. No cough, no SOB (shortness of breath), no respiratory issues, and no sudden loss of taste. No complaints of pain or discomfort noted. Will continue to monitor.
FALL #1
The nurses note dated 3/1/22 documents Resident had unwitnessed fall in her room. She was sitting on the floor next to bed, head up and arms and legs at normal position. Able to move upper and lower extremities. No respiratory distress. No s/s (signs/symptoms) of active bleeding. No new skin issues noted. [name of] NP (Nurse Practitioner) was notified. Order to send her for evaluation. [name] was also notified. VSS (vital signs) stable.
The Resident Fall Data Collection Tool for fall dated 3/1/22 under summary statement/root cause documents Resident admitted to SNF (skilled nursing facility) post fall in assisted living resulted in resident going to hospital and fracture of C, C2 diagnosed. C-Collar was on at times. Resident very anxious (baseline). Doesn't use call light for assistance. Resident on commode and attempted to transfer self to bed. Resulted in resident losing balance. Resident sent to ER for evaluation related to her already diagnosed C1-C2 fracture as a precautionary measure. Sent back, no new orders or diagnosis related fall. Moved to room closer to nurses station.
R71's falls care plan was updated 3/2/22 with the intervention to move to a room closer to nurses station.
FALL #2
The nurses note dated 3/15/22 documents Observed res (resident) lying on her right side in fetal position in skylight south dining room area. Wheelchair was behind res. no c/o (complaint of) pain or discomfort. cervical collar in place. ROM WNL (range of motion within normal limits) RN (Registered Nurse) present. Called [name] and order to send out to [name of hospital] ER (emergency room). Contacted friend [name]. [Name of] ambulance contacted. Res remained on the floor. Pillow placed under her head. T (temperature) 97.6 P (pulse) 72 R (respirations) 18 B/P (blood pressure)125/71 Pox (pulse oximetry) 98 RA (room air).
The nurses note dated 3/16/22 documents 0050 (12:50 a.m.) return from ER per stretcher, assisted back to bed by [name of] EMS (emergency medical services), no new order received from ER.
The IRIS (incident report) dated 3/15/22 under initial reported description documents Unwitnessed fall. Resident was found lying on the floor on her right side in a fetal position. No respiratory distress. Able to move upper and lower extremities. No skin injuries were noted. No s/s of active bleeding. No s/s of pain.
Under contributing factors is checked for patient/family - failure to follow plan of care & patient/family - patient altered mental status.
The Resident Fall Data Collection Tool for fall dated 3/15/22 under summary statement/root cause documents Observed resident in skylight south dining room lying on right side in fetal position. Denies pain. Range of motion within normal limits for resident cervical collar in place T97.6, B/P (blood pressure) 125/71, pulse 72, respiration 18, Pox 98% on room air. Sent resident out to [name of hospital] per order to send when fall present. order received to send to emergency room. remained on the floor pillow placed under head. RN (registered nurse) present.
This is a summary statement and does include a root cause for R71's fall.
This fall data collection tool does not include staff statements/interviews as to who last observed R71, when was she observed, were prior interventions in place, etc.
The RN Supervisor/Unit Manager Review is blank for summary statement/root cause.
R71's falls care plan was not revised until 5/17/22.
FALL #3
The nurses note dated 3/17/22 documents Resident was in the dining room eating breakfast and somehow got up and walked away from her Broda chair. Found by staff on the floor. Writer was called to assess resident. Resident on the floor with her cervical collar in place. Resident denied pain when asked. Resident to be sent out to hospital for eval and treat for existing neck injury. Updated Guardian [name] and informed NP [name]. Called up [name of] Ambulance for transport and [name of hospital] nurse [name] for report.
The nurses note dated 3/17/22 documents Resident was very restless and keep trying to get out of Broda chair. Requested for toileting and toileted x (times) 3. Unable to redirect. 1:1 supervision given until 2100 (9:00 p.m.) No new injury noted from her fall. C Collar in place. Transfer with 1 assist. Occasional calling out for help.
The IRIS (incident report) dated 3/17/22 under initial reported description documents Resident was eating breakfast in the dining room in Lead unit and was sitting in Broda chair. Somehow stood up and walked away from chair. Resident has history of multiple falls.
Under contributing factors is checked for patient/family - failure to follow plan of care & patient/family - patient altered mental status.
The Resident Fall Data Collection Tool for fall dated 3/17/22 under summary statement/root cause documents Resident is a fall risk. Has been in bed or Broda chair and walking away from it. Resident this morning was in lead dining room sitting in Broda chair and somehow stood up and walked away from Broda chair. Found lying on the floor.
The RN Supervisor/Unit Manager Review for summary statement/root cause documents Resident has history of multiple falls. Has anxiety self transfers.
This fall data collection tool does not include staff statements/interviews as to who last observed R71 & when, were prior interventions in place or the root cause of R71's fall.
R71's falls care plan was not revised until 5/17/22.
FALL #4
The nurses note dated 3/26/22 documents Resident found on the floor @ 11:30 a.m. Found side lying on the floor next to Broda chair in dining room in lead unit. Resident is alert. Cervical collar in place. Informed NP [name]. Updated Guardian [name]. Called up [name] Ambulance to transport . Called up [hospital name] ER nurse [name] to give report. Sent resident to ER for further eval and treat. Left message to phone of Caseworker [name] to call facility for update.
The nurses note dated 3/26/22 documents Pt returned from ER with NNO (no new orders) at this time.
The IRIS (incident report) dated 3/26/22 under initial reported description documents Found resident lying on her side on the floor next to Broda chair in Lead dining room.
Under contributing factors is checked for communication - language barrier or comprehension deficit, patient/family - failure to follow plan of care & patient/family - patient altered mental status.
The Resident Fall Data Collection Tool for fall dated 3/26/22 under summary statement/root cause documents Resident frequent faller. Somehow resident walked away from Broda chair while in the dining room.
The RN Supervisor/Unit Manager Review for summary statement/root cause documents Resident frequent falls history. Resident tries to self transfer most of the time.
This fall data collection tool does not include staff statements/interviews as to who last observed R71 & when, were prior interventions in place or the root cause of R71's fall.
R71's falls care plan was not revised until 5/17/22.
FALL #5
The nurses note dated 3/27/22 documents was notified by RN supervisor that my resident fell. The aides on that hall said they found her on the floor crawling to her bed, she was in her wheelchair the last they saw her. I notified the doctor on call as well as her #1 emergency contact. I called [name] but they told me to call 911 because they already had two pickups from this facility. Vital signs 116/68 Pulse 77 T 97.3 and R 18. No pain or injuries noted.
The nurses note dated 3/27/22 documents Writer called [hospital name] ER and was told the pt will be discharged back to the facility shortly.
The nurses note dated 3/28/22 documents No new orders from the ER.
Surveyor was not provided with an IRIS (incident report) for R71's 3/27/22 fall.
The Resident Fall Data Collection Tool for fall dated 3/27/22 under summary statement/root cause documents Resident found on floor crawling to bed, was in wheelchair.
The RN Supervisor/Unit Manager Review for summary statement/root cause was not included in this resident fall data collection tool.
This fall data collection tool does not include staff statements/interviews as to who last observed R71 & when, were prior interventions in place or the root cause of R71's fall.
R71's falls care plan was not revised until 5/17/22.
FALL #6
The nurses note dated 4/3/22 documents Patient noted to be lying on right side on dining room floor on Skylight South unit. UWF (unwitnessed fall) with abrasion noted to left knee. RN (Re[TRUNCATED]
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the Facility did not ensure that 5 (R12, R71, R14, R35, R31 ) of 18 Residents reviewed rece...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the Facility did not ensure that 5 (R12, R71, R14, R35, R31 ) of 18 Residents reviewed received treatment and care in accordance with professional standards of practice.
* R12's bowel movements were not being monitored.
R12 did not have a bowel movement on 7/14/22, 7/15/22, 7/16/22, & 7/17/22. No bowel assessment was completed on 7/14/22, 7/15/22, 7/16/22, 7/17/22, 7/18/22. Review of R12's July MAR (medication administration record) shows neither milk of magnesia 30 ml prn ( as needed) or Bisacodyl suppository 10 mg prn was administered during this time.
R12 did not have a bowel movement on 7/19/22, 7/20/22, or 7/21/22. No bowel assessment was completed on 7/19/22, 7/20/22, 7/21/22, 7/22/22. Review of R12's July MAR shows neither milk of magnesia 30 ml prn or Bisacodyl suppository 10 mg prn was administered during this time.
R12 is checked as not having any bowel movement on 7/24/22. On 7/25/22 R12 is documented as not having a bowel movement & small bowel movement, and on 7/26/22 no bowel movement. No bowel assessment was completed on 7/24/22, 7/25/22, 7/26/22 and 7/27/22. Review of R12's July MAR shows neither milk of magnesia 30 ml prn or Bisacodyl suppository 10 mg prn was administered during this time. R12 did receive Senna-Docusate sodium 8.6-50 mg on 7/25/22.
On 8/4/22 R12 is checked as not having a bowel movement and small bowel movement, 8/5/22 & 8/6/22 no bowel movements, 8/7/22 there is no documentation for bowel movements, & 8/8/22 is checked as having no bowel movements. R12 did not receive any as needed bowel medication during this time.
On 8/3/22, R12 requested to go to the hospital and returned back to the facility on 8/3/22 with a diagnosis of constipation. On 8/6/22, R12 returned to the hospital and was diagnosed with constipation and fecal impaction. The hospital after visit summary dated 8/6/22 under diagnoses documents Fecal Impaction and Constipation, unspecified constipation type.
* Neuro checks were not consistently completed following unwitnessed falls for R71.
* R31, R35, & R14 did not have sleep assessment completed.
Example involving R12 rises to a scope and severity level of G (harm/isolated)
Findings include:
1. R12's diagnoses include hemiplegia and hemiparesis following non traumatic intracranial hemorrhage affecting left non dominate side, adjustment disorder, and depressive disorder.
R12 receives a regular diet with regular texture and thin consistency liquids.
The quarterly MDS (Minimum Data Set) with an assessment reference date of 5/10/22 has a BIMS (Brief Interview Mental Status) score of 14 which indicates cognitively intact. R12 requires extensive assistance with two plus person physical assist for bed mobility, has transferred only once or twice with two plus person physical assist, doesn't ambulate and is dependent with two plus person physical assist for toilet use. R12 is coded as always being incontinent of bowel.
On 8/7/22 at 11:01 a.m. Surveyor observed R12 in bed on her back with the head of the bed elevated. R12 informed Surveyor she went to the hospital due to pain in her leg. R12 explained she was taken off a narcotic because she was getting constipated. R12 informed Surveyor at the hospital they did lab work and a CT scan which showed an area of impaction. R12 informed Surveyor she had to be disimpacted in the emergency room. R12 also informed Surveyor staff thought her constipation was opoid induced but she was impacted and no one caught it.
Surveyor reviewed R12's active physician orders as of 8/11/22 and the following pain medications:
Fentanyl patch 12.5 mcg (microgram) every 3 days with an order date of 4/17/22
Ketorolac Tromethamine 10 mg (milligrams) every 6 hours as needed with an order date of 11/22/21
Hydromorphone HCL 2 mg every 4 hours as needed with an order date of 10/4/21
Surveyor noted bowel medications of:
Bisacodyl Suppository 10 mg every 24 hours as needed with an order date of 7/29/21
Linzess 145 mcg once daily with an order date of 7/29/21
Milk of magnesia 30 ml (milliliter) every 24 hours as needed with an order date of 7/29/21
Polyethylene Glycol 17 grams as needed for constipation with an order date of 8/3/22
Senna Plus 8.6-50 mg 1 tablet daily with an order date of 8/6/22
Senna Plus 8.6-50 mg 2 tablets at bedtime with an order date of 8/6/22.
On 8/11/22 at 7:59 a.m. Surveyor asked CCM (Clinical Care Manager)-K how Resident's bowel movements are monitored. CCM-K informed Surveyor the CNA's (Certified Nursing Assistant) document in point of care. CCM-K explained they get an alert if a Resident does not have a bm (bowel movement) in three days. If no bm in three days then the nurse is to do a bowel assessment with the Resident and provide an intervention if necessary. Surveyor asked if bowel assessments are documented. CCM-K informed Surveyor any physical assessment should be documented in the nurses notes. Surveyor asked who receives the alert that a Resident has not had a bm in 3 days. CCM-K informed Surveyor everyone does, the floor nurse & managers and the alert comes in their care management dashboard. CCM-K informed Surveyor small bowel movements do not count as having a bowel movement, only medium or large. CCM-K informed Surveyor the first intervention is to provide the Resident with milk of magnesia. If the milk of magnesia doesn't work within the shift then a Bisacodyl suppository would be administered. CCM-K informed Surveyor if the suppository doesn't work then they should notify the doctor or NP (nurse practitioner). CCM-K also informed Surveyor if during the bowel assessment the Resident's abdomen is extended, or it there are no bowel sounds or hypoactive bowel sounds then the nurse should notify the doctor right away.
Surveyor reviewed R12's bowel documentation for the past 30 days. Surveyor noted
R12 is checked as not having any bowel movement on 7/14/22, 7/15/22, 7/16/22, & 7/17/22. An alert should have been sent as R12 went 4 days without a bowel movement.
Surveyor reviewed R12's nurses notes and was unable to locate a bowel assessment on 7/14/22, 7/15/22, 7/16/22, 7/17/22 and 7/18/22. Review of R12's July MAR (medication administration record) shows neither milk of magnesia 30 ml prn (as needed) nor Bisacodyl suppository 10 mg prn was administered during this time.
R12 is documented as having a large bowel movement on 7/18/22.
Senna-Docusate Sodium 8.6-50 mg with directions to give 2 tablets at hour of sleep was started on 7/19/22 and was discontinued on 7/27/22. On 7/27/22 Senna-Docusate Sodium 8.6-50 mg was ordered with directions to give one tablet every 12 hours.
R12 did not have a bowel movement on 7/19/22, 7/20/22, or 7/21/22. Surveyor reviewed R12's nurses notes and was unable to locate a bowel assessment on 7/19/22, 7/20/22, & 7/21/22. Review of R12's July MAR (medication administration record) shows neither milk of magnesia 30 ml prn nor Bisacodyl suppository 10 mg prn was administered during this time.
R12 is documented as having a large bowel movement on 7/22/22.
R12 is checked as not having any bowel movement on 7/24/22. 7/25/22 is documented as not having a bowel movement & small bowel movement, and on 7/26/22 no bowel movement.
Surveyor reviewed R12's nurses notes and was unable to locate a bowel assessment on 7/24/22, 7/25/22, 7/26/22, or 7/27/22. Review of R12's July MAR (medication administration record) shows neither milk of magnesia 30 ml prn nor Bisacodyl suppository 10 mg prn was administered during this time. R12 did receive Senna-Docusate sodium 8.6-50 mg on 7/25/22.
On 7/27/22 R12 had a medium bowel movement.
The nurses note dated 8/3/22 documents Writer was called to resident's room for resident wanting to go to hospital. Writer asked what was going on and resident said she wants Suboxone injection for her constipation. Explained to resident that it is not medication for constipation and offered Laclulose for her constipation. Resident refused. Offered Dulcolax suppository and prune juice but refused as well as all stool softeners. Informed NP [name]. NP [name] came to resident's room, spoke to resident but insist on going to the hospital.
The nurses note dated 8/3/22 documents Resident returned from hospital with the following orders: Stop taking Senna-S 50-8.6 mg and Miralax. New order for Miralax 17 g (grams) daily as needed for constipation.
The hospital after visit summary dated 8/3/22 under diagnoses documents Right lower quadrant abdominal pain & Constipation, unspecified constipation type.
On 8/4/22 R12 is checked as not having a bowel movement and small bowel movement, 8/5/22 & 8/6/22 no bowel movements, 8/7/22 there is no documentation for bowel movements, & 8/8/22 is checked as having no bowel movements. R12 did not receive any as needed bowel medication during this time.
The nurses note dated 8/4/22 documents Resident is monitored due to constipation. Ketorolac was given due to left hip pain and effective.
The nurses note dated 8/5/22 documents No c/o (complaint of) constipation noted this night shift. Tolerates fluids.
The nurses note dated 8/6/22 documents Alert and able to make needs known, no c/o constipation or abdominal discomfort. C/o lower back pain, prn pain med given with good result. Slept well, no further complaints.
The hospital after visit summary dated 8/6/22 under diagnoses documents Fecal Impaction and Constipation, unspecified constipation type.
The nurses note dated 8/7/22 documents Patient returned from ER (emergency room) per ambulance and new order noted for Senna S but patient already is on.
The nurses note dated 8/8/22 documents No c/o ABD (abdominal) pain or discomfort noted. BS (bowel sounds) x (times) 4. Resting in bed. No BM noted.
The nurse note dated 8/9/22 documents Resident taking scheduled Senna plus, abdomen soft nontender with bowel sounds x4 quads. (quadrants). no nausea or vomiting. ate both meals this shift.
On 8/11/22 at 12:12 p.m. Administrator-A and Corporate Consultant-M were informed of the above.
2. The Neurological Assessment policy & procedure from Med-Pass Inc. (Revised October 2010) under General Guidelines documents 1. Neurological assessments are indicated:
a. Upon physician order;
b. Following an unwitnessed fall;
c. Following a fall or other accident/injury involving head trauma; or
d. When indicated by resident's condition.
R71's diagnoses include dementia with behavioral disturbances, hypertension, anxiety disorder, panic disorder, and depressive disorder.
On 8/10/22 at 7:51 a.m. Surveyor asked ADON (Assistant Director of Nursing)-H when neuro checks are completed for a Resident who has fallen. ADON-H informed Surveyor per the paper neuro checks are completed every 15 minutes four times, 30 minutes two times and every 1 hour four times.
On 8/10/22 at 8:10 a.m. ADON-H informed Surveyor after the paper neuro checks, which end after 1 hour four times, the Resident is put on the 24 hour report and is monitored, meaning neuro checks are done every shift for 3 days. Surveyor inquired where these neuro checks can be located. ADON-H informed Surveyor neuro checks should be in the progress notes. Surveyor inquired what if the neuro checks aren't in the progress notes. ADON-H informed Surveyor if they aren't there she doesn't know what to say.
On 8/10/22 at approximately 8:15 a.m. Surveyor reviewed R71's medical record and noted the following:
* The nurses note dated 4/12/22 documents Informed by CNA (Certified Nursing Assistant) that resident slid self from Broda chair while dinner trays were being passed, no injury noted, assisted back into Broda chair with 2 assist and gait belt. Call placed to [name of] Hospice and spoke with [name] RN, will send out nurse to assess resident. Left voice mail for guardian [name] to call facility and voice mail left for CM (Case Manager) [name] to call facility.
The neuro check flow sheet dated 4/12/22 are incomplete at 1640 (4:40 p.m.), 1655 (4:55 p.m.), 1710 (5:10 p.m.), 1725 (5:25 p.m.), 1755 (5:55 p.m.), 1810 (6:10 p.m.), 1910 (7:10 p.m.), 2010 (8:10 p.m.), &2110 (9:10 p.m.). The sections for consciousness level, responds to tactile stimuli, responds to visual stimuli, hand grasp & visual response to light have not been completed. At 2210 (10:10 p.m.) the sections for consciousness level, responds to tactile stimuli, responds to visual stimuli, hand grasp, visual response to light, & vital signs have not been completed.
The nurses note dated 4/13/22 at 11:46 a.m. includes documentation of neuro check negative. There is no other documentation of neuro checks each shift for three days.
* The nurses note dated 4/18/22 documents Resident monitored for fall. Agitated this afternoon. Had an unwitnessed fall in hallway. Managed to get to her room and get into bed. Hospice and POA notified. Hospice nurse will be coming tomorrow morning to evaluate her.
There is no evidence neuro checks were completed for R71 following the 4/18/22 fall with the exception of nurses note dated 4/20/22 at 1:46 p.m. which includes documentation of neuro checks negative.
* The nurses note dated 5/12/22 documents Writer was notified that that resident was on the floor. She was found sitting on hallway in front of her room. Resident was alert and verbally responsive. Able to move upper and lower extremities. No injuries noted from fall. No s/s of active bleeding. Resident denies pain. Resident was transferred to Broda chair. [name] hospice was notified and [name] too.
The neuro check flow sheet dated 5/12/22 are incomplete at 2030 (8:30 p.m.), 2045 (8:45 p.m.), 2100 (9:00 p.m.), 2130 (9:30 p.m.), 2200 (10:00 p.m.), & 2300 (11:00 p.m.) for consciousness level. At 2400 (12:00 a.m.) 1:00 a.m. & 2:00 am the sections for consciousness level, responds to tactile stimuli, responds to visual stimuli, hand grasp, visual response to light, & vital signs have not been completed. Surveyor was unable to locate documentation neuro checks were completed each shift for three days following the paper neuro check flow sheet.
* The IRIS (incident report) dated 5/16/22 under initial reported description documents Resident was alone in the common dining area. She scooted herself off the chair onto the floor. Found sitting on her butt. Zero injuries. Neuro checks WNL (within normal limits). Zero c/o (complaint of) pain. Under contributing factors is checked for patient/family - failure to follow plan of care.
There is no evidence neuro checks were completed for R71 following the 5/16/22 fall.
* The nurses note dated 6/4/22 documents Med tech from S. South notified writer that resident was found sitting on the floor at hallway at S. South in front of her room. Prior to unwitnessed fall, resident was lying in bed and sleeping. Writer found resident sitting on the floor with arms and legs in a normal position. Resident is alert and verbally responsive. No respiratory distress. Able to move upper and lower extremities. No injuries were noted during skin assessment. No s/s of active bleeding. Resident denies pain. [name] was notified. [name] RN from [name of] Hospice was notified too. Hospice said that nurse will come to facility to assess resident tomorrow (6/5/22).
The neuro check flow sheet dated 6/4/22 are incomplete at 0055 (12:55 a.m.), 0155 (1:55 a.m.), 0255 (2:55 a.m.). The for sections for consciousness level, responds to tactile stimuli, responds to visual stimuli, hand grasp, visual response to light, & vital signs have not been completed. Sleeping was written across the vital sign sections. At 0355 (3:55 a.m.) the section for consciousness level, responds to tactile stimuli, responds to visual stimuli, hand grasp, & visual response to light were not completed.
The nurses notes dated 6/6/22 at 9:43 a.m. & 6/7/22 at 9:53 a.m. includes documentation of neuro check negative. There is no other documentation of neuro checks each shift for three days.
* The nurses note dated 6/8/22 documents Resident observed sitting on the floor by her room res stated she slid out of bed landing on her buttocks. no c/o pain or discomfort. ROM WNL (range of motion within normal limits) for Resident. alert per res baseline. RN present for body check Contacted [name] NP who is on call for [Physician's name]. [Name] POA called and message left with case worker [name] to call facility. res transferred into wheelchair and is sitting in common area with staff. T 97.7 P 68 R 16 B/P 122/64.
The neuro check flow sheet dated 6/8/22 are incomplete at 2315 (11:15 p.m.) 0015 (12:15 a.m.), 0115 (1:15 a.m.), 0215 (2:15 a.m.) & 0315 (3:15 a.m.). The sections for consciousness level, responds to tactile stimuli, responds to visual stimuli, hand grasp, visual response to light, & vital signs have not been completed.
Surveyor was unable to locate documentation neuro checks were completed each shift for three days following the paper neuro check flow sheet.
* The nurses note dated 7/13/22 documents Patient discovered on the floor in the dining room on Skylight South. Patient was sitting on her bottom with palms against floor at time of discovery. She is awake, alert and oriented to self and situation which is her baseline. Patient appears restless. When asked what she was trying to do at the time of fall, pt. stated she was looking at the ground and wanted to sit down. No indication of injury, no new open areas or redness noted. Pt. follows simple commands. PERRLA (pupils equal, round, reactive to light and accommodation). Hand grasps firm. Upper and lower extremities assessed. No c/o pain or discomfort when asked. VS (vital signs) obtained by floor nurse. Pt. wearing gripper socks. Pt. assisted back to chair. CNA and floor nurse with patient at this time. [name] NP updated. [name] (guardian) updated on fall.
Surveyor was unable to locate any further neuro checks following R71's 7/13/22 fall.
On 8/11/22 at 12:12 p.m. Administrator-A and Corporate Consultant-M were informed of the above.
5. R31 was admitted to the facility on [DATE] with diagnoses of depression and insomnia. The quarterly MDS assessment dated [DATE] indicate R31 is cognitively impaired needs extensive assistance with bed mobility, dressing, hygiene and transfers.
The 7/24/22 physician orders indicate R31 was prescribed Trazadone 100 mg (milligrams) at night for insomnia.
On 8/10/22 Surveyor reviewed R31 medical record and there wasn't a sleep assessment or care plan addressing R31 insomnia.
On 8/10/22 at 2:30 p.m. during the daily exit meeting with NHA A and Corporate Consultant M, Surveyor explained R31 is receiving Trazadone for insomnia and does not have a sleep assessment and care plan addressing the insomnia. Corporate Consultant M stated anyone on a sleep medication should have a sleep assessment done. NHA A and Corporate Consultant M understood the concern and had no further information.
3. Surveyor reviewed R14's medical record on 8/10/22.
According to the July and August 2022 Medication Administration Record (MAR), R14 has physician's orders dated 6/14/22 for Melatonin Capsule 3 MG give 1 capsule by mouth at bedtime for sleep with 5mg for a total of 8 mg. R14 has been receiving the Melatonin capsules at HS daily.
Surveyor reviewed a Behavior Solutions Inc. (BSI) psych note dated 8/3/22 which documented in part; Melatonin 8 mg at HS for insomnia . sleep pattern varies per resident and he notes sometimes I can't sleep. Melatonin was increased at last visit to address with no improvement per resident, denies napping. Resident with stable mood on decrease dose of Paxil however insomnia continues to be a concern per resident. Wound recommend obtaining a sleep study to assess sleep pattern with follow up in 2 months.
Recommendation: Sleep study X3 nights and update BSI if abnormal.
R14's 8/18/22 annual Minimum Data Set (MDS) was not yet complete however, R14's last quarterly MDS dated [DATE] indicates R14 as having a Brief Interview for Mental Status score of 11 indicating R14 is moderately impaired for daily decision making skills. The quarterly MDS indicates R14 does not have trouble falling asleep, staying asleep or sleeping too much.
R14 has a care plan addressing the use of an antidepressant initiated 5/28/19 with an intervention of monitoring/document side effects and effectiveness of the antidepressant and to monitor/document/report to MD prn ongoing s/sx of depression unaltered by antidepressant meds: sad, irritable, anger, crying, shame, disrupted sleep . initiated on 5/28/19 however; R14's care plan does not identify R14 as having a concern with sleep, nor does it address R14 as having a sleep study conducted. R14's care plan does not address R14's use of Melatonin for sleep or interventions that may assist R14 with sleep.
On 8/8/22 02:45 pm Surveyor interviewed Assistant Director of Nursing H who stated she has been employed at the facility since the end of December 2021 and that no sleep assessments have been conducted since that time.
On 8/10/22 Surveyor interviewed Clinical Care Manager LPN K regarding Behavior Solution's recommendation for R14 to have a sleep assessment. Clinical Care Manager K stated the Behavior Solution's recommendation would first go to the pharmacist and Director of Nursing for their review before being scanned in. Clinical Care Manager LPN K was not aware of any sleep assessment having been conducted for R14.
On 8/10/22 at 2:45 pm, Surveyor shared with Administrator A and Corporate Consultant M, that no sleep study was located in R14's medical record. Corporate Consultant M indicated an awareness of needing to conduct sleep studies.
4. On 8/9/22 Surveyor reviewed R35's medical record.
On 8/9/22, Surveyor interviewed R35 who reported leaving for dialysis at 4:15 am, chair time from 5-8:30 am back by 9:30 am, 3 times a week.
Surveyor reviewed R35's admission Minimum Data Set (MDS) dated [DATE] which indicates R35 has a Brief Interview for Mental Status score (BIMS) of 15 indicating R35 is cognitively intact for daily decision making skills. This MDS indicates yes for R35 having trouble falling or staying asleep or sleeping too much. The MDS also indicates R35 is noted as feeling tired with little energy.
A 06/22/2022 14:02 (2:02pm) Social Services Note Text documents: Care Plan meeting held today with resident and Power of Attorney's knowledge. No concerns expressed at this time. Resident requires assistance with ADL's (activities of daily living) and transfers. Resident is alert and able to express self well. Resident continues on Trazodone (antidepressant) for insomnia, Duloxetine for depression and Aripiprazol and Seroquel for Hallucinations and Bipolar disorder.
R35's August 2022 Medication Administration Record (MAR) and physician orders indicate Melatonin tablet 3 mg give 1 tablet by mouth in the evening for insomnia with a start date of 7/30/22. R35's August MAR indicates R35 has been receiving this daily at 2100 (9:00 pm).
R35's August 2022 MAR also has an order for Trazodone HCI tablet 50 mg give 1 tablet by mouth every 24 hours as needed (PRN) for depression related to depression, unspecified with a start date of 7/30/22. The MAR indicates R35 received this on 8/1/22.
R35's plan of care does not reflect R35's use of Melatonin for insomnia nor any indication that a sleep assessment was completed. R35 has no interventions to assist with R35's sleep issues.
On 8/8/22 02:45 pm, Surveyor interviewed Assistant Director of Nursing (ADON) H as to whether a sleep assessment was conducted for R35. ADON H reported she has been at the facility since the end of December and no sleep assessment has been completed since that time. ADON- H stated the MD ordered Trazadone for depression and it is PRN, receiving it on 8/1/22.
On 8/10/22 at 2:45 pm, Surveyor shared with Administrator A and Corporate Consultant M, that no sleep study was located in R35's medical record. Corporate Consultant M indicated an awareness of needing to conduct sleep studies.
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews with staff, the facility did not provide consistent interventions to prevent...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews with staff, the facility did not provide consistent interventions to prevent the development of pressure injuries for 5 of 8 residents (R26, R75, R19, R71, R12) at risk for pressure injuries.
* R26 was observed with their heels not being offloaded on 8/7/22. On 8/8/22, R26 was noted with an unstageable pressure injury to the left heel.
* R75 was observed not wearing pressure reducing heel boots throughout the survey.
* On 7/15/22, R19 who was assessed at risk for the development of pressure injuries acquired a stage 3 pressure injury to the left heel. On the initial assessment for R19's left heel pressure injury there was no documentation of the percentage of the wound bed for granulation tissue & slough. There was no indication the facility used pressure relieving boots or offloaded R19's heels prior to the development of this pressure injury.
R19's left heel was not assessed from 7/22 through 8/4/22. The facility did not identify R19 having a pressure injury to the left heel until it was a Stage 3.
* R71 was observed with heels not being offloaded throughout the survey.
* R17 was observed with heels not being offloaded throughout the survey.
* R12 was observed with heels not being offloaded throughout the survey.
Examples for R26 and R19 rises to a scope and severity level of a G (harm/isolated)
Findings include:
1. R26 was admitted to the facility on [DATE] with diagnoses of vascular dementia with behavioral disturbance, cerebral vascular accident and hemiplegia to left upper and lower extremities. R26's Quarterly MDS (Minimum Data Set) assessment dated [DATE] indicates that R26 requires extensive assistance of 1 staff member with bed mobility.
Per R26's medical record, a Braden assessment conducted on 8/8/22 indicates a score of 14, which indicates R26 is at moderate risk for pressure injuries.
On 8/07/22 at 9:10AM, R26 was observed in bed with heels directly on their mattress laying on right side wearing a hospital gown and incontinence product in bed. No pressure relief boots were noted at this time. R26 is unable to reposition self independently due to hemiplegia to their left upper and lower extremities. R26 requires assistance to move their extremities.
On 8/07/22 at 12:10 PM, R26 was observed in bed with heels directly on their mattress laying on right side wearing hospital gown and incontinence product in bed. No pressure relief boots were noted at this time. R26 is unable to reposition self independently due to hemiplegia to their left upper and lower extremities. R26 requires assistance to move their extremities.
On 8/07/22 at 2:30 PM, R26 was observed in a wheelchair wearing shoes to bilateral feet.
On 8/08/22 at 9:02 AM, R26 was observed in a wheelchair, wearing a pressure relieving boot to the left foot.
On 8/08/22 at 11:22 AM, R26 was observed in a wheelchair, wearing a pressure relieving boot to the left foot.
O8/08/22 at 1:32 PM, R26 was observed resting in bed on their back wearing a pressure relieving boot to the left foot.
On 8/09/22 at 12:32 PM, R26 was observed resting in bed on their back wearing a pressure relieving boot to the left foot.
On 8/09/22 at 3:17 PM, Surveyor reviewed R26's CNA (Certified Nursing Assistant) care [NAME] form. R26's [NAME] indicates that pressurve relieving heel boots are to be worn at all times when in bed.
On 8/10/22 at 9:30 AM, Surveyor conducted interview with CNA-I. Surveyor asked CNA-I how they would know if a resident is at risk for pressure injuries and if they would need specialty equipment such as pressure relieving heel boots. CNA-I told Surveyor that this information should be on the resident's [NAME].
On 8/10/22 at 9:52 AM, Surveyor observed Clinical Care Manager-J conducting dressing change to R26's left heel. Surveyor observed a circular wound to the left heel with approximately 80% of wound bed covered in yellow fibrous slough tissue. Surveyor asked Clinical Care Manager-J if a resident is at risk for pressure injuries or has pressure injuries to their feet if they should wear pressure relieving heel boots. Clinical Care Manager-J responded that unless the resident was ambulatory and it would be a safety risk, they would prefer that residents at risk for pressure injuries should wear bilateral heel boots. Clinical Care Manager-J indicated that R26 has had previous pressure injuries to the left heel in the past.
Surveyor questioned whether a resident should wear heel boots at all times if they have a pressure injury. Clinical Care Manager-J stated, Yes I would like them to wear heel boots when they have pressure injuries to heel. If resident is ambulatory with a foot wound, they should only wear them in bed per Wound MD recommendations so they do not sustain an injury. R26 has had this same injury before so we do not recommend she wear shoes.
On 8/10/22 at 3:20 PM, Surveyor conducted an interview with ADON (Assistant Director of Nursing)-H. Surveyor asked ADON-H if residents at risk for pressure injuries or with current pressure injuries should wear pressure relieving heel boots. ADON-H responded that residents at risk for pressure injuries should have heel boots in place to lessen the risk of acquiring pressure injuries unless it poses a safety risk to the resident.
On 8/10/22 at 4:00 PM, Surveyor shared serious concerns with NHA (Nursing Home Administrator)-A related to R26's observations of no pressure relieving heel boots in place to bilateral feet per CNA [NAME] on 8/7/22 and the discovery of an unstageable pressure injury to the left heel on 8/8/22. The facility provided no additional information to the Surveyor at this time.
2. R75 was admitted to the facility 9/21/20 with diagnoses of juvenile arthritis, bilateral hand contractures and dementia. R75's Significant change MDS dated [DATE] indicates that R75 requires extensive assistance of 1 staff for bed mobility. R75 has range of motion limitations to their upper and lower extremities. R75's Braden assessment dated [DATE] indicates R75 has a score of 12, indicating R75 is at high risk for pressure injuries. R75 was enrolled in hospice/comfort care on 1/21/22 due to severe protein malnourishment and failure to thrive.
On 8/07/22 at 9:10 AM, R75 was observed laying on their right side wearing hospital gown and incontinence product in bed. R75's heels are observed directly on their mattress.
On 8/07/22 at 11:30 AM, R75 was observed laying on their right side wearing a hospital gown and incontinence product in bed. R75's heels are observed directly on their mattress.
On 8/07/22 at 1:35 PM, R75 was observed laying on their right side wearing a hospital gown and incontinence product in bed. R75's heels are observed directly on their mattress.
On 8/07/22 at 3:05 PM, R75 was observed laying on their right side wearing a hospital gown and incontinence product in bed. R75's heels are observed directly on their mattress.
On 8/08/22 at 8:26 AM, R75 was observed laying on their right side wearing a hospital gown and incontinence product in bed. R75's heels are observed directly on their mattress.
On 8/08/22 at 10:36 AM, R75 was observed laying on their right side wearing a black and white striped sweater and incontinence product in bed. R75's heels are observed directly on their mattress.
On 8/08/22 at 11:35 AM, R75 was observed laying on their right side wearing a black and white striped sweater and incontinence product in bed. R75's heels are observed directly on their mattress.
On 8/08/22 at 1:38 PM, R75 was observed laying on their right side wearing a black and white striped sweater and incontinence product in bed. R75's heels are observed directly on their mattress.
On 8/09/22 at 9:08 AM, R75 was observed laying on their right side wearing hospital gown and incontinence product in bed. R75's heels are observed directly on their mattress.
On 8/10/22 at 9:30 AM, Surveyor conducted an interview with CNA-I. Surveyor asked CNA-I how they would know if a resident is at risk for pressure injuries and if they would need specialty equipment such as pressure relieving heel boots. CNA-I told Surveyor that this information should be on the resident's [NAME]. Surveyor observed R75's heels at this time and did not identify any open areas at this time. R75 does not have pressure relieving heel boots in place at the time of observation.
On 8/10/22 at 9:52 AM, Surveyor conducted an interview with Clinical Care Manager-J. Surveyor asked Clinical Care Manager-J if a resident is at risk for pressure injuries or has pressure injuries to their feet if they should wear pressure relieving heel boots. Clinical Care Manager-J responded that unless the resident was ambulatory and it would be a safety risk, they would prefer that residents at risk for pressure injuries should wear bilateral heel boots. Clinical Care Manager-J indicated that R75 should wear bilateral heel boots.
On 8/10/22 at 3:20 PM, Surveyor conducted interview with ADON-H. Surveyor asked ADON-H if residents at risk for pressure injuries or with current pressure injuries should wear pressure relieving heel boots. ADON-H responded that residents at risk for pressure injuries should be put in place to lessen risk of acquiring pressure injuries unless it poses a safety risk to the resident.
On 8/10/22 at 4:00 PM, Surveyor shared concern with NHA-A related to observations of R75 not wearing pressure relieving heel boots to bilateral feet per CNA [NAME] on 8/7/22-8/10/22. The facility provided no additional information to the Surveyor at this time.
3. R19's diagnoses includes Congestive Heart Failure, Alzheimer's Disease, Diabetes Mellitus,hypertension and dementia.
The pressure injury CAA (care area assessment) dated 2/22/22 under analysis of finding for nature of the problem/condition documents [AGE] year old female with Dx (diagnoses) of spinal stenosis, CHF (congestive heart failure), Alzheimer's disease/dementia, CKD3 (chronic kidney disease 3), DM2 (diabetes mellitus 2), HTN (hypertension), morbid obesity, HLD (hyperlipidemia), OSA (obstructive sleep apnea), Vit (vitamin) D deficiency, gastric ulcer, depression, and anemia exhibits potential for pressure ulcer/injuries due to need for extensive assistance with bed mobility, incontinence of bowel and bladder, and Braden score of 12.
The at risk for skin breakdown care plan initiated & revised on 3/3/22 documents the following approaches:
* Encourage me/assist me with repositioning routinely and PRN (as needed). Initiated & revised 3/3/22.
* Follow facility policies/protocols for the prevention/treatment of skin breakdown. Initiated & revised 3/3/22.
* I have a pressure reducing cushion in my chair. Initiated & revised 3/3/22.
* Inform me/family/caregivers of any new area of skin breakdown. Initiated 3/3/22.
* Monitor/document/report to MD (medical doctor) PRN changes in skin status: appearance, color, wound healing, s/sx (signs/symptoms) of infection, wound size (length x (times) width x depth), stage. Initiated 3/3/22.
* Pressure relieving mattress on bed. Initiated 3/3/22.
Surveyor noted the at risk for skin breakdown care plan does not address offloading R19's heels.
The Braden assessment dated [DATE] has a score of 15 which indicates at risk.
The quarterly MDS (Minimum Data Set) with an assessment reference date of 5/20/22 documents a BIMS (brief interview mental status) score of 3 which indicates severe impairment. R19 requires extensive assistance with two plus person physical assist for bed mobility, is dependent with two plus person physical assist for transfer & toilet use and does not ambulate. R19 is always incontinent of urine and bowel, is at risk for pressure injuries and is coded as not having any pressure injuries.
The weekly wound tracking dated 7/15/22 for the question where is the wound located documents left posterior heel, for the question was this condition/wound present on admission is no, and wound classification is Pressure Injury Stage 3. Measurements are 2.2 cm (centimeter) length, 1.7 cm width, & depth 0.4 cm. The wound progress/evaluation documents first observation, no reference. The visible tissue is checked or granulation tissue and slough. Surveyor noted this assessment does not document the percentage of granulation tissue & slough in the wound bed.
The physician orders dated 7/15/22 for the left heel documents to cleanse with wound cleanser, pat dry, apply medihoney to wound bed, cover with dry dressing and change daily on the day shift for Stage 3 wound and as needed.
After R19 developed a stage 3 pressure injury, the Facility developed a care plan for I have a pressure ulcer to my left heel-stage 3 care plan initiated & revised 7/15/22 documents the following approaches:
* Assess/record/monitor wound healing (FREQ). Measure length, width and depth where possible. Assess and document status of wound perimeter, wound bed and healing progress. Report improvements and declines to the MD. Initiated 7/15/22.
* I require supplemental protein, amino acids, vitamins, minerals as ordered to promote wound healing. Initiated 7/15/22.
* Measure wounds weekly and notify MD of any s/s of worsening or if not improving. Initiated 7/15/22.
* Monitor my wound with dressing changes and PRN. Monitor for s/s of infection/worsening (redness, increased pain/tenderness/drainage, edema, warmth) PRN. Initiated 7/15/22.
* Offer to assist me with toileting routinely and PRN. Assist with incontinence care as needed to keep skin warm and dry. Provide barrier cream after incontinence care and PRN. Initiated 7/15/22.
* Provide treatments as ordered. Initiated 7/15/22.
* Seen by [name of wound company] wound. Initiated & revised 7/22/22.
Although this care plan does not include any approaches to offload R19's heels, Surveyor noted in the CNA (Certified Nursing Assistant) documentation heel boots at all times was being initialed starting during the evening shift on 7/15/22.
Prior to this date the dates & times are X out indicating R19 did not have heel boots. Also starting during the evening shift on 7/15/22 the CNA's were initialing to elevate legs/feet when sitting to avoid pressure to heels. Prior to the evening shift on 7/15/22 the dates & times are X out.
The nurses note dated 7/16/22 documents Dressing dry & intact to left heel. No complaint of pain or signs/symptoms of discomfort noted. Heels elevated.
The wound doctor initial wound evaluation & management summary dated 7/21/22 for history of present illness documents, At the request of the referring provider, [physician's name], a thorough wound care assessment and evaluation was performed today. She has a stage 3 pressure wound to the left heel for at least 2 days duration. There is light sero-sanguineous exudate. There is no indication of pain associated with this condition.
For etiology documents Pressure. MDS 3.0 documents 3 and wound size documents 2 x (times) 1.5 x 0.2. Granulation tissue is 100%. Recommendations are off-load wound, float heels in bed.
The nurses note dated 7/21/22 documents Pt. (Patient) was seen by [name of wound doctor] and wound nurse for wound to left heel. Wound assessment and evaluation performed by wound MD. Pt. has a stage 3 wound to her left heel. Light serosanguineous drainage noted with 100% granulation tissue. Pt. denies pain. Pt. will continue with current orders. Wound cleansed and tx (treatment) applied. Heel boots in place. [name of resident representative] updated. Pt. will be seen on the next weekly wound round.
The weekly wound tracking dated 7/22/22 for the question where is the wound located documents sacrum, for the question was this condition/wound present on admission is no, and wound classification is Pressure Injury Stage 3. Measurements are 2 cm (centimeter) length, 1.5 cm width, & depth 0.1 cm. The wound progress/evaluation documents first observation, no reference. The visible tissue is checked or granulation tissue. Percentage of necrotic tissue present in wound is 0.
After R19 developed a Stage 3 pressure injury on her sacrum the Facility developed a care plan I have a pressure ulcer to my sacrum stage 3 on 7/22/22 with all approaches dated 7/22/22 of the following:
* Assess/record/monitor wound healing (FREQ). Measure length, width and depth where possible. Assess and document status of wound perimeter, wound bed and healing progress. Report improvements and declines to the MD.
* I require supplemental protein, amino acids, vitamins, minerals as ordered to promote wound healing.
* Measure wounds weekly and notify MD of any s/s of worsening or if not improving.
* Monitor my wound with dressing changes and PRN. Monitor for s/s of infection/worsening (redness, increased pain/tenderness/drainage, edema, warmth) PRN.
* Offer to assist me with toileting routinely and PRN. Assist with incontinence care as needed to keep skin warm and dry. Provide barrier cream after incontinence care and PRN.
* Provide me with treatments per my orders.
* Seen by [name of wound company] wound.
The wound doctor progress note dated 7/28/22 documents The patient's visit has been rescheduled.
The nurses note dated 7/28/22 documents Wound visit rescheduled. Pt. did not want to go back to bed for assessment. Family from out of town visiting with patient.
There is no assessment of R19's Stage 3 sacrum and left heel pressure injuries until 8/4/22. This assessment was 14 days for R19's left heel and 13 days for the sacrum.
The wound doctor's wound evaluation & management summary dated 8/4/22 for focused wound exam (site 1) for etiology documents Pressure, MDS 3.0 Stage is 3 and wound size is 1.5 x 1.5 x 0.2 cm. Slough is 20% and granulation tissue is 80%.
The nurses note dated 8/4/22 documents Pt. was seen by [name of wound doctor] and wound nurse for multiple wounds. Wound to sacrum has resolved. Improvement noted to heel wound. Pt. denies pain. Pt. will continue with current orders. Wound cleansed and tx applied. Heel boots in place. Pt. will be seen on the next weekly wound round.
On 8/7/22 at 9:40 a.m. Surveyor observed R19 sitting in a Broda chair in the dining area. Surveyor observed R19 is wearing pressure relieving boots.
On 8/8/22 at 7:39 a.m. Surveyor observed R19 awake in bed on her back with the head of the bed elevated. Surveyor observed R19 is wearing pressure relieving boots.
On 8/8/22 at 11:16 a.m. Surveyor asked CMA (Certified Medication Aide)-X when R19 started wearing pressure relieving boots. CMA-X informed Surveyor she doesn't know the exact date but it's been a couple weeks.
On 8/8/22 at 12:47 p.m. Surveyor asked CCM (Clinical Care Manager)-J, who is the Facility's wound nurse, how she is informed a Resident has developed a pressure injury. CCM-J informed Surveyor if someone has a wound and she's in the facility staff will call her to take a look. CCM-J informed Surveyor she will measure the wound, get a treatment in place through the NP (nurse practitioner) or wound MD, make sure the family has been updated, make sure there is a care plan in place, complete a Braden assessment and complete the unavoidable form for every wound. CCM-J explained if the pressure injury is found on the weekend she will assess the pressure injury on Monday and the wound doctor will see the Resident on Thursday as this is the only day the wound doctor comes in. CCM-J explained the nurse can assess the pressure injury but they are not allowed to Stage. CCM-J indicated the nurse can measure and describe the wound bed. CCM-J informed Surveyor once the wound doctor sees the Resident she no longer completes the Resident's weekly wound tracking. Surveyor informed CCM-J on the initial assessment for R19's left heel pressure injury there was no documentation of the percentage of the wound bed for granulation tissue & slough. CCM-J stated there is no place to document this and they only document the percentage of necrotic tissue. Surveyor inquired if R19 ever refuses. CCM-J informed Surveyor R19 refused when her family was here otherwise she doesn't refuse. Surveyor informed CCM-J of the concern R19's pressure injuries not assessed after the family left or another day and noted there was no assessment of the pressure injuries until 8/4/22 approximately two weeks later. Surveyor inquired why the pressure injury wasn't identified until it was a Stage 3. CCM-J informed Surveyor she couldn't tell Surveyor as she doesn't see everybody every week. CCM-J informed Surveyor when a new admission comes in she sees them for the first 3 to 4 weeks and then the nurses on the floor need to do their assessments.
On 8/9/22 at 10:12 a.m. to 10:16 a.m. Surveyor observed the treatment for R19's left heel pressure injury with CCM-J and CNA-Y. There was no deficient practice identified during this treatment observation.
On 8/9/22 at 10:17 a.m. Surveyor asked CCM-J how R19 developed the pressure injury on her left heel. CCM-J informed Surveyor R19 was wearing a certain kind of shoe which rested on the foot pad of the Broda chair. CCM-J indicated she didn't know if it was the shoe or foot pad of the Broda.
4. R12's diagnoses includes hemiplegia and hemiparesis following intracranial hemorrhage, depressive disorder, and anxiety disorder.
The at risk for skin breakdown care plan initiated 7/30/21 includes an approach dated 7/30/21 of Elevate my heels off of my mattress with a pillow or other device.
The quarterly MDS (Minimum Data Set) with an assessment reference date of 5/10/22 documents a BIMS (brief interview mental status) score of 14 which indicates cognitively intact. R12 requires extensive assistance with two plus person physical assist for bed mobility, transferred only once or twice during the assessment period with two plus person physical assist, and does not ambulate. R12 is at risk for developing pressure injuries and is coded as not having any pressure injuries.
On 8/7/22 at 11:15 a.m. Surveyor observed R12 in bed on her back with the head of the bed elevated. There is a pressure relieving boot on R12's left foot and the right foot is not being offloaded. R12 did not have a boot on the right foot.
On 8/8/22 at 7:35 a.m. Surveyor observed R12 asleep in bed on her back with the head of the bed elevated. Surveyor observed R12's heels are resting directly on the mattress and the pressure relieving boot is in a chair in the corner of R12's room.
On 8/8/22 at 11:04 a.m. Surveyor observed R12 continues to be asleep in bed on her back with the head of the bed elevated. Surveyor observed R12's heels are resting directly on the mattress and the pressure relieving boot is in a chair in the corner of R12's room.
On 8/8/22 at 1:31 p.m. Surveyor observed R12 in bed visiting with the visitor. R12 is on her back with the head of the bed elevated. R12's heels are not being offloaded and the pressure relieving boot continues to be in the chair in the corner of the room. Surveyor asked R12 asked about the pressure relieving boot on the chair. R12 informed Surveyor she hasn't had the boot on all day.
On 8/11/22 at 7:52 a.m. Surveyor asked CCM (Clinical Care Manager)-K why R12 only wears a pressure relieving boot on the left foot. CCM-K informed Surveyor because R12 complains there is pain in her heel/foot. Surveyor inquired how staff should off load R12's heels. CCM-K informed Surveyor staff uses pillows to offload. Surveyor informed CCM-K of the observations of R12's heels not being offloaded.
5. R71's diagnoses includes dementia, hypertension and diabetes mellitus.
The at risk for skin breakdown d/t (due to) diabetes, immobility, incontinence care plan initiated & revised 3/1/22 has the following approaches:
* Administer medications as ordered. Monitor/document for side effects and effectiveness. Initiated & revised 3/1/22.
* Administer treatments as ordered and monitor for effectiveness. Initiated & revised 3/1/22.
* Encourage me/assist me with repositioning routinely and PRN (as needed). Initiated & revised 3/1/22.
* Follow facility policies/protocols for the prevention/treatment of skin breakdown. Initiated & revised 3/1/22.
* I have a pressure reducing cushion in my chair. Initiated & revised 3/1/22.
* Inform me/family/caregivers of any new area of skin breakdown. Initiated & revised 3/1/22.
* Monitor/document/report to MD (medical doctor) PRN (as needed) changes in skin status: appearance, color, wound healing, s/sx (signs/symptoms) of infection, wound size (length x (times) width x depth), stage. Initiated & revised 3/1/22.
* Obtain and monitor lab/diagnostic work as ordered. Report results to MD and follow up as indicated. Initiated & revised 3/1/22.
* Pressure relieving mattress to bed. Initiated & revised 3/1/22.
Surveyor noted there are not approaches to prevent pressure injuries from developing on R71's heels.
The quarterly MDS with an assessment reference date of 7/16/22 documents a BIMS score of 7 which indicates severe impairment. R71 requires extensive assistance with one person physical assist for bed mobility, transfer & toilet use, ambulates in the room with limited assistance with one person physical assist, dependent with one person physical assist for ambulating in the corridor. R71 is at risk for pressure injury development and is coded as not having any pressure injuries.
On 8/7/22 at 9:28 a.m. Surveyor observed R71 in bed on her left side. Surveyor observed R71's heels are resting directly on the mattress and are not being offloaded.
On 8/7/22 at 9:59 a.m. Surveyor observed R71 continues to be on the left side. Surveyor observed R71's heels are resting directly on the mattress and are not being offloaded.
On 8/7/22 at 10:20 a.m. Surveyor observed R71 in bed on her back. There is a pillow under R71's calves with the right heel floating and the left heel resting directly on the pillow.
On 8/7/22 at 11:27 a.m. Surveyor observed R71 in bed on her back. Surveyor observed R71 has a pillow under her calves and R71's heels are being offloaded.
On 8/9/22 at 8:17 a.m. Surveyor observed R71 in bed on her left side. Surveyor observed R71's heels are not being offloaded.
On 8/9/22 at 2:11 p.m. Surveyor asked CCM (Clinical Care Manager)-K what the Facility is doing to prevent pressure injuries from developing on R71's heels. CCM-K informed Surveyor she thought R71 was wearing boots. Surveyor informed CCM-K Surveyor didn't note any interventions on R71's skin integrity care plan to prevent pressure injuries from developing on R71's heels. CCM-K looked at R71's electronic medical record and informed Surveyor there isn't an order for boots and then stated she would look a the care plan. After reviewing R71's care plan, CCM-K stated nope there isn't anything. Surveyor asked CCM-K if staff should be offloading R71's heels. CCM-K replied they should be. Surveyor informed CCM-K of the observations of R71's heels not being offloaded.
On 8/10/22 at 7:31 a.m. Surveyor observed R71 awake in bed leaning towards the right side. Surveyor observed R71 is wearing gripper socks, there is not a pillow under R71's calves and R71's heels are resting directly on the mattress.
On 8/11/22 at 8:29 a.m. Surveyor observed R71 in bed on her left side. R71's heels are not being offloaded.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility did not ensure residents were safe to self administer medications...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility did not ensure residents were safe to self administer medications for 2 of 2 (R34 and R42) residents who were observed to have medications left at bedside for self administration.
R34 had medications left at bedside, but did not have an assessment to determine if she was safe to self administer medications.
R42 had medications left at bedside, but did not have an assessment to determine if she was safe to self administer medications.
Findings include
The Facility policy titled Medication Administration Schedule revised November, 2020 documents (in part) .
.3. Scheduled medications are administered within one (1) hour of their prescribed time, unless otherwise specified.
The above policy was the only policy the facility provided upon request from Surveyor.
1. On 8/7/22 at 9:28 AM Surveyor observed R34 sitting in her wheelchair next to the bed. Surveyor observed 2 white pills lying on the mattress next to R34. Surveyor asked R34 if she knew what the pills were. R34 stated, those are my gas pills. Surveyor asked R34 if staff usually leave them for her to take, to which R34 stated Yes.
On 8/7/22 at 9:30 AM Surveyor asked Certified Medication Aide (CMA)-D what pills were on R34's bed. CMA-D stated, those are her gas pills, she takes them when she starts eating. Surveyor asked So you just leave them there for her? CMA-D stated, Yes. She doesn't want to eat right now, so she'll take them when she starts eating.
On 8/7/22 at 11:33 AM Surveyor observed the same 2 white pills remained on R34's bed. R34 was observed to be asleep in her wheelchair. Surveyor noted R34 did not eat her bacon, eggs and toast, but did consume all of the oatmeal.
On 8/7/22 at 2:09 PM Surveyor observed R34 in the bathroom with a staff member. Surveyor noted the 2 white pills were no longer on the bed.
R34's Medication Administration Record (MAR) documented: Simethicone tablet 80 mg (milligrams) give 2 tablets by mouth every 8 hours as needed for flatulence - signed out as having been administered at 8:51 AM. Surveyor noted the 2 gas pills were not taken and remained on her bed until after 11:33 AM.
R34's medical record revealed a Quarterly Minimum Data Set (MDS) dated [DATE] indicated a Brief Interview for Mental Status (BIMS) score of 14 indicating no cognitive impairment. Surveyor located no Physician's order to self administer medications and no evidence the facility completed an assessment to determine if R34 can safely self administer medications.
2. On 8/7/22 9:53 AM, during interview with R42, Surveyor observed 4 pills on the bedside table. Surveyor asked what the pills were. R42 stated, I don't know. I take 11 in the morning, these are what I have left to take. Surveyor asked if the nurse usually leaves her pills for her to take. R42 stated, Yes, but a couple times I fell asleep and forgot to take them.
R42's MAR documented the following medications scheduled at 8:00 AM and 9:00 AM: Allopurinol 100 mg, Aspirin chewable 81 mg, Cholecalciferol 125 mcg (micrograms), Claritin 5 mg, Clopidogrel Bisulfate 75 mg, Docusate Sodium 100 mg, Folic Acid 1 mg, Magnesium Oxide 400 mg, Ropinirole 0.5 mg and Metoprolol Tartrate 100 mg - all of which were signed out as having been administered.
R42's medical record revealed a Quarterly MDS dated [DATE] indicated a BIMS sore of 14 indicating no cognitive impairment. Surveyor located no Physician's order to self administer medications.
Surveyor located a Self-Med Evaluation dated 1/15/18 which documented: Can resident self administer medication? No.
If self-administration of medication is not granted, explain: Nurse to be outside room during treatment r/t (related to) residents change of condition.
There were no other self med evaluations in R42's medical record.
On 8/9/22 at 3:00 PM Surveyor advised Nursing Home Administrator (NHA)-A of the above concerns. No additional information was provided.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the Facility did not ensure that Resident representatives received notifications related to a change in condition for 1 (R19) of 18 Residents reviewed for notific...
Read full inspector narrative →
Based on interview and record review, the Facility did not ensure that Resident representatives received notifications related to a change in condition for 1 (R19) of 18 Residents reviewed for notification.
Findings include:
The Change in a Resident's Condition or Status policy 2001 MED-PASS, Inc (Revised February 2021) documents under policy statement, Our facility promptly notifies the resident, his or her attending physician, and the resident representative of changes in the resident's medical/mental condition and/or status (e.g., changes in level of care, billing/payments, resident rights, etc).
Under Policy Interpretation and Implementation documents
4. Unless otherwise instructed by the resident, the nurse will notify the resident's representative when:
a. the resident is involved in any accident or incident that results in an injury including injuries of an unknown source;
b. there is a significant change in the resident's physical, mental, or psychosocial status;
c. there is a need to change the resident's room assignment;
d. a decision has been made to discharge the resident from the facility; and/or
e. it is necessary to transfer the resident to a hospital/treatment center.
R19's diagnoses includes Alzheimer's Disease, dementia, and gastro-esophageal reflux. R19 has an activated power of attorney for healthcare.
The nurses note dated 7/27/22 documents Resident noted with dark colored stool and mild abdominal distention. Abdomen soft and non-tender. Bowel Sounds heard in 4 quadrants. Resident assessed by NP (nurse practitioner). New orders received for labs in AM and occult blood x (times) 1. Orders entered. Resident has Hx (history) of GI bleed. Writer updated POA (power of attorney) and in agreement with new orders. Writer also had a conversation with POA regarding hospice and the services that can benefit resident. POA in agreement with new order for Hospice to eval (evaluate) and treat if indicated. POA chose [name of] Hospice. Order provided to SW (Social Worker) who made referral to [name of hospice].
The nurses note dated 7/29/22 documents Resident had a large bowel movement this shift. Stool specimen to be tested for occult blood was collected and left at refrigerator to be picked up. KUB (kidney, ureter, bladder) results were notified to [name of] NP. No s/s (signs/symptoms) of pain.
The nurses note dated 7/30/22 documents Resident's fecal occult blood test was positive. On call NP was notified. Orders: pantoprazole 40 mg (milligrams), twice daily for 3 months and CBC (complete blood count) on 7/31/22.
The physician orders dated 7/31/22 documents Pantoprazole Sodium Tablet Delayed Release 40 MG Give 1 tablet by mouth two times a day for GERD for 3 Months. The end date for this medication is 10/31/22.
The nurses note dated 8/3/22 documents Resident is monitored for new order for pantoprazole. Resident tolerates med well. No s/s of pain.
Surveyor was unable to locate when R19's power of attorney was notified of the new medication and lab ordered for R19.
On 8/8/22 at 10:52 a.m. Surveyor spoke with RN (Registered Nurse)-L on the telephone. Surveyor read the 7/30/22 nurses note RN-L wrote regarding R19. Surveyor asked RN-L if she called anyone else regarding R19. RN-L replied No, called NP and put on 24 hour board so we can follow up. Surveyor asked RN-L if she knew who would have called the POA/Resident Representative. RN-L replied probably me, I didn't do it. Surveyor asked RN-L if she notified R19's representative of Pantoprazole and CBC ordered for 7/31/22 due to GI bleed. RN-L replied no and explained if she had notified R19's representative the documentation would have been in her notes.
On 8/9/22 at 4:20 p.m. Administrator-A and Corporate Consultant-M were informed of the above.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the Facility did not report alleged violations related to mistreatment, exploitation, negl...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the Facility did not report alleged violations related to mistreatment, exploitation, neglect, or abuse, including injuries of unknown source and misappropriation of resident property to the proper authorities, including the State Agency, within prescribed timeframe's for 2 of 2 (R237 and R12) residents reviewed for abuse.
* R237 and R12's allegation of abuse was not reported to the State Agency within prescribed timeframe.
Findings include:
The Facility policy titled: Abuse, Neglect and Exploitation revised 7/2022 documents (in part) .
.Policy:
It is the policy of this facility to provide protections for the health, welfare and rights of each resident by developing and implementing written policies and procedures that prohibit and prevent abuse, neglect, exploitation, and misappropriation of resident property.
Definitions:
Abuse means the willful infliction of injury, unreasonable confinement, intimidation, or punishment with resulting physical harm, pain or mental anguish. Abuse also includes the deprivation by an individual, including a caretaker, of goods or services that are necessary to attain or maintain physical, mental, and psychosocial well-being. Instances of abuse of all residents, irrespective of any mental or physical condition, cause physical harm, pain or mental anguish. It includes verbal abuse, sexual abuse, physical abuse and mental abuse including abuse facilitated or enabled through use of technology.
Willful means the individual must have acted deliberately, not that the individual must have intended to inflict injury or harm.
Sexual Abuse is non-consensual sexual contact of any type with a resident.
Physical Abuse includes, but is not limited to hitting, slapping, punching, biting and kicking. It also includes controlling behavior through corporal punishment.
Mental abuse includes, but is not limited to humiliation, harassment, threats of punishment or deprivation.
Neglect means failure of the facility, its employees or service providers to provide goods and services to a resident that are necessary to avoid physical harm, pain, mental anguish or emotional distress.
Mistreatment means inappropriate treatment or exploitation of a resident.
VII. Reporting/Response
1. Reporting of alleged violations to the Administrator, state agency, adult protective services, and to all other required agencies (e.g., law enforcement when applicable) within specified timeframe's:
a. Immediately, but not later than 2 hours after the allegation is made, if the events that cause the allegation involve abuse or result in serious bodily injury, or
b. Not later than 24 hours if the events that cause the allegation do not involve abuse and do not result in serious bodily injury.
2. Assuring that reporters are free from retaliation or reprisal;
4. Taking all necessary actions as a result if the investigation, which may include, but are not limited to, the following:
a. Analyzing the occurrence(s) to determine why abuse, neglect occurred and what changes are needed to prevent further occurrences;
b. Defining how care provision will be changed and/or improved to protect residents receiving services;
c. Training of staff on changes made and demonstration of staff competency after training is implemented;
d. Identification of staff responsible for implementation of corrective actions;
e. The expected date for implementation; and
f. Identification of staff responsible for monitoring the implementation of the plan.
1. R237 was admitted to the facility on [DATE] and discharged on 6/30/22.
Diagnoses included: Attention Deficit Hyperactivity Disorder, Dementia, Major Depressive Disorder and Rheumatoid Arthritis.
R237's BIMS (Brief Interview for Mental Status) dated 6/23/22 documented a score of 13 - indicating R237 as cognitively intact for daily decision making skills.
Surveyor reviewed a Facility Reported Incident dated 6/4/22.
Clinical Care Manager (CCM)-K statement dated 6/4/22 documents:
On 6/2/22 (R237) reported to me that a male resident kissed her on the cheek. R237 did not know who the resident was and reported it did not really bother her.
Surveyor noted CCM-K did not report the allegation to Nursing Home Administrator (NHA)-A or Director of Nursing (DON)-B.
On 6/3/22 when CCM-K was leaving the building, R237 informed CCM-K she knew who the resident was. CCM-K stated: OK, you could let me know when I return.
Surveyor noted although R237 informed CCM-K she could identify the resident involved in the alleged sexual abuse, on 6/3/22 CCM-K did not report the allegation to NHA-A or DON -B.
On 6/4/22 CCM-K received a call from the Registered Nurse (RN) stating that R237 is telling them that the man touched her nightgown that day (6/2/22) also. CCM-K interviewed R237 on the phone and R237 stated R41 came into her room, lifted her nightgown and pointed at her private area and gestured for her to move her leg. R237 reported he lifted up the night gown, pointed at her private area, smiled and said me and you like he wanted sex. He kissed her cheek and she told him no way and to go away.
CCM-K's statement further documented DON-B was notified and she was directed to tell the RN to do the follow-up.
Surveyor's review of the Facility Self Report documented the report was submitted to the State Agency on 6/4/22 at 7:31 PM. R237 first reported the allegation of sexual abuse to CCM-K on 6/2/22 and again on 6/3/22, neither of which were reported to the State Agency.
On 6/10/11 Surveyor advised NHA-A of the concern R237 reported an allegation of abuse on 6/2/22 and 6/3/22 neither of which were reported to the State Agency until 6/4/22. No additional information was provided.
2. R12's quarterly MDS (Minimum Data Set) with an assessment reference date of 5/10/22 has a BIMS (brief interview mental status) score of 14 which indicates cognitively intact.
On 8/7/22 at 11:08 a.m. during the screening process Surveyor asked R12 how staff treated her and inquired if any staff have been rough, yelled, or swore at her. R12 informed Surveyor there was one girl but she doesn't come in R12's room anymore. R12 informed Surveyor with the CNA's (Certified Nursing Assistant) first name, CNA-T, and informed Surveyor she was rough when turning her so CCM (Clinical Care Manager)-K took her off from taking care of her. Surveyor asked R12 if she remembers when she spoke to CCM-K. R12 informed Surveyor it was four or five weeks ago. R12 informed Surveyor one time she spoke to the owner as CCM-K was not at the Facility. Surveyor inquired what she told the owner. R12 informed Surveyor she told the owner [name of CNA-T] said she (R12) looked like shit.
Surveyor asked R12 if she knew the name of the owner. R12 informed Surveyor the first name of DON (Director of Nursing)-B. Surveyor asked R12 when she spoke with owner. R12 informed Surveyor three weeks ago and he was true to his word she (CNA-T) hasn't been in her room.
On 8/7/22 at 1:37 p.m. Surveyor reviewed the Resident concern from May 1, 2022 to July 31, 2022. R12 was not on this concern log during this time period.
On 8/8/22 at 9:46 a.m. Surveyor reviewed the Facility's investigations which were reported to the State agency starting 5/1/22. Surveyor noted there is no self report investigation for R12.
On 8/8/22 at 1:30 p.m. Surveyor asked CCM-K if R12 ever voiced any concerns to her about staff treatment. CCM-K replied yes and explained there is one employee R12 complained about that she often says rude things. CCM-K informed Surveyor they talked to that employee and the employee is no longer allowed to take care of R12. Surveyor asked what the employee's name is. CCM-K informed Surveyor the first name of CNA-T. CCM-K informed Surveyor R12 said CNA-T was abrupt with everything and she wouldn't listen to R12. Surveyor asked CCM-K if R12 said CNA-T was rough with her. CCM-K informed Surveyor she didn't think she used rough, not sure if she used the word rough. Surveyor asked CCM-K when R12 spoke to her about CNA-T. CCM-K informed Surveyor she doesn't recall but thinks it was at least a month. Surveyor asked CCM-K if she reported R12's allegations to anyone. CCM-K informed Surveyor she spoke to DON-B and ADON (Assistant Director of Nursing)-H. CCM-K indicated they spoke with CNA-T to get her side of the story. CCM-K informed Surveyor CNA-T may have been misinterpreted and CNA-T said she was not abrupt or rough with R12 or forced her to turn. CCM-K informed Surveyor she did explain to CNA-T R12 didn't want her to be her caregiver and told CNA-T not to go into R12's room at all. Surveyor asked was CNA-T removed from resident care or suspended. CCM-K replied no. Just talked to her because they couldn't validate what R12 was saying.
On 8/8/22 at 1:53 p.m. Surveyor asked ADON-H if she was aware of any concerns with R12 and any staff. ADON-H informed Surveyor R12 has left her a few messages and she has spoken with R12. Surveyor asked when this was and what the concerns were. ADON-H informed Surveyor in the last 2 to 3 weeks. ADON-H indicated R12 expressed concerns regarding a certain staff member she didn't want going into her room. Surveyor inquired who the staff member was. ADON-H informed Surveyor the first name of CNA-T. ADON-H explained R12 felt CNA-T talked down to her. Surveyor asked ADON-H if R12 voiced a concern CNA-T told her she looked like shit. ADON-H informed Surveyor she was not aware of this. ADON-H informed Surveyor R12 didn't want CNA-T in her room and CNA-T went in the room to drop off a dinner tray. ADON-H informed Surveyor R12 called her again. ADON-H informed Surveyor she told R12 she would speak with CNA-T again. Surveyor asked ADON-H if R12 had any other concerns. ADON-H replied no just about CNA-T. ADON-H informed Surveyor CCM-K was on vacation, and all of CCM-K's calls were forwarded to her and this is why R12 called her.
On 8/8/22 at 2:12 p.m. Surveyor asked DON-B if R12 reported any staff concerns to him. DON-B informed Surveyor R12 complained one day but didn't make any allegation. Surveyor asked DON-B what the concern was about. DON-B informed Surveyor the staff member talked too loud. Surveyor asked who R12 was referring to. DON-B informed Surveyor the name of CNA-T, she was too fast that was R12's comment to him. DON-B informed Surveyor to avoid anything further he went to the unit manager and told her not to assign CNA-T to R12. Surveyor asked when this was. DON-B informed Surveyor he's going to say three or four weeks ago. Surveyor asked DON-B if R12 reported to him CNA-T said she looked like shit. DON-B replied no, started laughing and stated that would of been crossing the line there. DON-B then informed Surveyor you referring to the Surveyor need to dig further into the patient here, borderline, drug seeking, constantly demanding to go to the hospital. Surveyor asked if he has self reported any concerns with R12. DON-B replied I don't believe so then stated should I report abuse and neglect for talking to fast and loud. DON-B stated this is crossing the line of ridiculousness.
R12's allegation of mistreatment should have been reported to the State agency.
On 8/8/22 at 4:20 p.m. Administrator-A and Corporate Consultant-M were informed of the above.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. On 8/10/22 at 11:46 AM, Surveyor reviewed a facility self-report related to R56's elopement on 5/31/22.
On 8/10/22 at 10:20 A...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. On 8/10/22 at 11:46 AM, Surveyor reviewed a facility self-report related to R56's elopement on 5/31/22.
On 8/10/22 at 10:20 AM, Surveyor reviewed statements from 2 staff members related to R56's elopement on 5/31/22. Surveyor requested additional information from NHA-A related to the facility's investigation of R56's elopement, including additional staff statements and root cause analysis of R56's elopement.
On 8/11/22 at 1:02 PM, NHA-A informed Surveyor that there was no additional documentation related to R56's elopement investigation, including staff statements or root cause analysis of R56's elopement.
On 8/11/22 at 4:00 PM, Surveyor shared concerns with NHA-A that R56's elopement that occurred on 5/31/22 was not thoroughly investigated by the facility. No additional information was provided by the facility at this time.
Based on interview and record review the Facility did not thoroughly investigate allegations of abuse to prevent further abuse, neglect, exploitation and mistreatment from occurring for 4 of 4 (R237, R58, R12, and R56) residents reviewed for abuse.
R237 sexual abuse allegation was not thoroughly investigated.
R58's sustained sexual abuse that was not thoroughly investigated
R12's abuse allegation was not thoroughly investigated.
R56's elopement (neglect) was not thoroughly investigated.
Findings include:
The Facility policy titled: Abuse, Neglect and Exploitation revised 7/2022 documents (in part) .
.Policy:
It is the policy of this facility to provide protections for the health, welfare and rights of each resident by developing and implementing written policies and procedures that prohibit and prevent abuse, neglect exploitation and misappropriation of resident property.
Definitions:
Abuse means the willful infliction of injury, unreasonable confinement, intimidation, or punishment with resulting physical harm, pain or mental anguish. Abuse also includes the deprivation by an individual, including a caretaker, of goods or services that are necessary to attain or maintain physical, mental, and psychosocial well-being. Instances of abuse of all residents, irrespective of any mental or physical condition, cause physical harm, pain or mental anguish. It includes verbal abuse, sexual abuse, physical abuse and mental abuse including abuse facilitated or enabled through use of technology.
Willful means the individual must have acted deliberately, not that the individual must have intended to inflict injury or harm.
Sexual Abuse is non-consensual sexual contact of any type with a resident.
Physical Abuse includes, but is not limited to hitting, slapping, punching, biting and kicking. It also includes controlling behavior through corporal punishment.
Mental abuse includes, but is not limited to humiliation, harassment, threats of punishment or deprivation.
Neglect means failure of the facility, its employees or service providers to provide goods and services to a resident that are necessary to avoid physical harm, pain, mental anguish or emotional distress.
Mistreatment means inappropriate treatment or exploitation of a resident.
III. Prevention of Abuse, Neglect and Exploitation
The facility will implement policies and procedures to prevent and prohibit all types of abuse, neglect, misappropriation of resident property and exploitation that achieves:
A. Establishing a sage environment that supports, to the extent possible, a resident's consensual sexual relationship and by establishing policies and protocols for preventing sexual abuse, such as the identify when, how, and by whom determinations of capacity to consent to a sexual contact will be made and where this documentation will be recorded; and the resident's right to establish a relationship with another individual, which may include the development of or the presence of an ongoing sexually intimate relationship.
D. The identification, ongoing assessment, care planning for appropriate interventions, and monitoring of residents with needs and behaviors which might lead to conflict or neglect.
F. Providing residents, representatives and staff information on how and to whom they may report concerns, incidents and grievances without the fear of retribution; and providing feedback regarding the concerns that have been expressed.
V. Investigation of Alleged Abuse, Neglect and Exploitation
A. An immediate investigation is warranted when suspicion of abuse, neglect or exploitation, or reports of abuse neglect or exploitation occur.
B. Written procedures for investigations include:
1. Identifying staff responsible for the investigation;
3. Investigating different types of alleged violations;
4. Identifying and interviewing all involved persons, including the alleged victim, alleged perpetrator, witnesses, and others who might have knowledge of the allegations.
5. Focusing the investigation on determining if abuse, neglect, exploitation and/or mistreatment has occurred, the extent, and cause, and;
6. Providing complete and thorough documentation of the investigation.
VI. Protection of Resident
The facility will make efforts to ensure all residents are protected from physical and psychosocial harm during and after the investigation. Examples include but are not limited to:
A. Responding immediately to protect the alleged victim and integrity of the investigation.
B. Examining the alleged victim for any sign of injury, including a physical examination or psychosocial assessment if needed;
C. Increased supervision of the alleged victim and residents;
D. Room or staffing changes, if necessary, to protect the resident(s) from the alleged perpetrator;
E. Protection from retaliation;
F. Providing emotional support and counseling to the resident during during and after the investigation, as needed.
1. R237 admitted to the facility on [DATE] and discharged on 6/30/22. Diagnoses included: Attention Deficit Hyperactivity Disorder, Dementia, Major Depressive Disorder and Rheumatoid Arthritis.
R237's BIMS (Brief Interview for Mental Status) dated 6/23/22 documented a score of 13 - indicating R237 as cognitively intact.
Surveyor reviewed a Facility Self Report dated 6/4/22.
Clinical Care Manager (CCM)-K statement dated 6/4/22 documents:
On 6/2/22 (R237) reported to me that a male resident kissed her on the cheek. R237 did not know who the resident was and reported it did not really bother her.
Surveyor noted CCM-K did not follow up or investigate the allegation.
On 6/3/22 when CCM-K was leaving the building, R237 informed CCM-K she knew who the resident was. CCM-K stated: OK, you could let me know when I return.
Surveyor noted although R237 informed CCM-K she could identify the resident involved in the sexual abuse, CCM-K did not follow up or investigate the allegation, which placed other vulnerable residents at risk for sexual abuse.
On 6/4/22 CCM-K received a call from the Registered Nurse (RN) stating that R237 is telling them that the man touched her nightgown that day (6/2/22) also. CCM-K interviewed R237 on the phone and R237 stated R41 came into her room, lifted her nightgown and pointed at her private area and gestured for her to move her leg. R237 reported he lifted up the night gown, pointed at her private area, smiled and said me and you like he wanted sex. He kissed her cheek and she told him no way and to go away.
CCM-K's statement further documented DON-B was notified and she was directed to tell the RN to do the follow-up.
The facility was aware of the allegation of sexual abuse that occurred between R41 and R237 on 6/2/22. The facility did not complete a thorough investigation of the allegation.
There was no evidence an assessment was completed on R237 to determine her ability to consent, and no investigation of the perpetrator (R41) to determine the possible cause of the behavior. R41 did not have a care plan related to sexual behaviors, and no evidence of increased monitoring and intervention to keep other residents safe.
2. 9 days later, on 6/11/22, another incident of sexual abuse occurred between R41 and a different female resident (R58).
R58 was admitted to the facility on [DATE] and has diagnoses that include: Schizophrenia, Major Depressive Disorder and Anxiety Disorder.
R58's Quarterly MDS dated [DATE] documents a BIMS score of 15 - indicating no cognitive impairment.
Graduate Practical Nurse (GPN)-E's statement documented she was walking down the hall and noticed R58 sitting on the couch. R41 was sitting behind R58 with his hand in the back of her brief near her butt. GPN-E told R41 to take his hand out R58's pants. The residents were separated and went back to their rooms. R58 was asked if she was OK and she reported yes, he was just rubbing my back. GPN-E reported the incident to the Supervisor.
Surveyor was unable to locate evidence an interview was completed with R58 following the incident.
There was no assessment of R58 to determine her ability to consent and no investigation of R41 to determine the possible cause of the behavior. R41 did not have a care plan related to sexual behaviors, and no evidence of increased monitoring to keep other residents safe.
On 8/8/22 at 1:30 PM Surveyor asked DON-B if he had any additional information regarding the investigation and incident between R41 and R58. DON-B reported he did not have any additional information. Surveyor advised the investigation did not include an interview with R58, and asked if there were any other staff or resident interviews. DON-B stated, I guess there isn't.
On 8/9/22 NHA-A provided an interview with R58 dated 6/11/22.
Licensed Practical Nurse (LPN)-N's statement documented, On 6/11/22 at roughly 3 :00 PM, she interviewed R58 who was asked how she was feeling, which she reported fine. She was asked about the interaction with R41. R58 reported he started to rub her shoulders and back, she liked it and it felt good. She did not ask him to do this. She stated he was touching inside the front of her pants. She reported she was not sad, upset or scared. LPN-N reassured her she did nothing wrong, and she was safe.
Registered Nurse (RN)-O's statement dated 6/11/22 documented he spoke to DON-B and was informed to keep the residents separated and start 15 minute checks for R41. RN-O called R58's son and daughter- in- law. Family in agreement but added that resident (R58) has had similar issues in her past and they would like to have psychologist talk with resident during the next visit to the facility.
After reviewing the 6/11/22 Facility Reported Incident, Surveyor was unable to locate an interview with R41. Surveyor asked DON-B if R41 speaks English. DON-B reported he does speak English, but has some cognitive deficits. An interview was not provided.
The facility did not complete a thorough investigation of the alleged abuse between R41 and R58. The facility was aware of R58's history of sexual abuse, however this was not included in the investigation. R58 did not have a care plan related to her previous sexual abuse. There was no evidence R41 was interviewed following either incident. R41 did not have a care plan related to sexual behaviors, and no evidence of increased monitoring to keep other residents safe.
On 6/10/22 NHA-A was advised of the above concerns. No additional information was provided.
3. R12's quarterly MDS (minimum data set) with an assessment reference date of 5/10/22 has a BIMS (brief interview mental status) score of 14 which indicates cognitively intact.
On 8/7/22 at 11:08 a.m. during the screening process Surveyor asked R12 how staff treated her and inquired if any staff have been rough, yelled, or swore at her. R12 informed Surveyor there was one girl but she doesn't come in R12's room anymore. R12 informed Surveyor with the CNA's (Certified Nursing Assistant) first name, CNA-T, and informed Surveyor she was rough when turning her so CCM (Clinical Care Manager)-K took her off from taking care of her. Surveyor asked R12 if she remembers when she spoke to CCM-K. R12 informed Surveyor it was four or five weeks ago. R12 informed Surveyor one time she spoke to the owner as CCM-K was not at the Facility. Surveyor inquired what she told the owner. R12 informed Surveyor she told the owner [name of CNA-T] said she (R12) looked like shit. Surveyor asked R12 if she knew the name of the owner. R12 informed Surveyor the first name of DON (Director of Nursing)-B. Surveyor asked R12 when she spoke with owner. R12 informed Surveyor three weeks ago and he was true to his word she hasn't been in her room.
On 8/7/22 at 1:37 p.m. Surveyor reviewed the Resident concern from from May 1, 2022 to July 31, 2022. R12 was not on this concern log during this time period.
On 8/8/22 at 9:46 a.m. Surveyor reviewed the Facility's investigations which were reported to the State agency starting 5/1/22. Surveyor noted there is not a self report investigation for R12.
On 8/8/22 at 1:30 p.m. Surveyor asked CCM-K if R12 ever voiced any concerns to her about staff treatment. CCM-K replied yes and explained there is one employee R12 complained about that she often says rude things. CCM-K informed Surveyor they talked to that employee and the employee is no longer allowed to take care of R12. Surveyor asked what the employee's name is. CCM-K informed Surveyor the first name of CNA-T. CCM-K informed Surveyor R12 said CNA-T was abrupt with everything and she wouldn't listen to R12. Surveyor asked CCM-K if R12 said CNA-T was rough with her. CCM-K informed Surveyor she didn't think she used rough, not sure if she used the word rough. Surveyor asked CCM-K when R12 spoke to her about CNA-T. CCM-K informed Surveyor she doesn't recall but thinks it was at least a month. Surveyor asked CCM-K if she reported R12's allegations to anyone. CCM-K informed Surveyor she spoke to DON-B and ADON (Assistant Director of Nursing)-H. CCM-K indicated they spoke with CNA-T to get her side of the story. CCM-K informed Surveyor CNA-T may have been misinterpreted and CNA-T said she was not abrupt or rough with R12 or forced her to turn. CCM-K informed Surveyor she did explain to CNA-T R12 didn't want her to be her caregiver and told CNA-T not to go into R12's room at all. Surveyor asked was CNA-T removed from resident care or suspended. CCM-K replied no. Just talked to her because they couldn't validate what R12 was saying. Surveyor asked if anything was written up for an investigation. CCM-K replied no. Surveyor asked CCM-K if other resident's were spoken to. CCM-K replied no.
On 8/8/22 at 1:53 p.m. Surveyor asked ADON-H if she was aware of any concerns with R12 and any staff. ADON-H informed Surveyor R12 has left her a few messages and she has spoken with R12. Surveyor asked when this was and what the concerns were. ADON-H informed Surveyor in the last 2 to 3 weeks. ADON-H indicated R12 expressed concerns regarding a certain staff member she didn't want going into her room. Surveyor inquired who the staff member was. ADON-H informed Surveyor the first name of CNA-T. ADON-H explained R12 felt CNA-T talked down to her. Surveyor asked ADON-H if R12 voiced a concern CNA-T told her she looked like shit. ADON-H informed Surveyor she was not aware of this. ADON-H informed Surveyor R12 didn't want CNA-T in her room and CNA-T went in the room to drop off a dinner tray. ADON-H informed Surveyor R12 called her again. ADON-H informed Surveyor she told R12 she would speak with CNA-T again. Surveyor asked ADON-H if R12 had any other concerns. ADON-H replied no just about CNA-T. ADON-H informed Surveyor while CCM-K was on vacation, all of CCM-K's calls were forwarded to her and this is why R12 called her.
On 8/8/22 at 2:12 p.m. Surveyor asked DON-B if R12 reported any staff concerns to him. DON-B informed Surveyor R12 complained one day but didn't make any allegation. Surveyor asked DON-B what the concern was about. DON-B informed Surveyor the staff member talked to loud. Surveyor asked who R12 was referring to. DON-B informed Surveyor the name of CNA-T, she was too fast that was R12's comment to him. DON-B informed Surveyor to avoid anything further he went to the unit manager and told her not to assign CNA-T to R12. Surveyor asked when this was. DON-B informed Surveyor he's going to say three or four weeks ago. Surveyor asked DON-B if R12 reported to him CNA-T said she looked like shit. DON-B replied no, started laughing and stated that would of been crossing the line there. DON-B then informed Surveyor you referring to the Surveyor need to dig further into the patient here, borderline, drug seeking, constantly demanding to go to the hospital. Surveyor asked DON-B if he has anything in writing regarding an investigation. DON-B informed Surveyor this is not going to happen because he can't investigate everything, that is unreasonable with 100 patients.
On 8/8/22 at 4:20 p.m. Administrator-A and Corporate Consultant-M were informed of the above.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. The Facility policy titled Catheter Care, Urinary revised September, 2014 documents (in part) .
.Purpose:
The purpose of th...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. The Facility policy titled Catheter Care, Urinary revised September, 2014 documents (in part) .
.Purpose:
The purpose of this procedure is to prevent catheter-associated urinary tract infections.
Preparation:
1. Review the resident's care plan to assess for any special needs of the resident.
Maintaining Unobstructed Urine Flow
3. The urinary drainage bag must be held or positioned lower than the bladder at all times to prevent the urine in the tubing and drainage bag from flowing back into the urinary bladder.
R34 admitted to the facility on [DATE]. Urology placed a suprapubic catheter on 7/8/22.
R34's Care Plan indicated she was incontinent of urine. R34 did not have a care plan for her suprapubic catheter.
On 8/7/22 at 9:22 AM Surveyor observed R34 sitting in the wheelchair in her room. Surveyor observed R34's catheter bag hanging on the right side of the wheelchair on the metal frame under the arm rest, uncovered and above the level of her bladder.
On 8/8/22 at 9:23 AM Surveyor observed R34 sitting in the wheelchair in the bathroom. Surveyor observed the catheter bag hanging on the right side of the wheelchair on the metal frame under the arm rest, uncovered and above the level of her bladder.
On 8/9/22 at 7:20 AM Surveyor observed R34 sitting in the wheelchair in her room. Surveyor observed the catheter bag hanging on the right side of the wheelchair on the metal frame under the arm rest, uncovered and above the level of her bladder.
On 8/10/22 at 9:51 AM Surveyor asked R34 if staff always hangs her catheter bag on the side of her wheelchair under the armrest. R34 stated: Yes. Surveyor asked if the bag is ever covered, to which R34 stated: No. Surveyor asked R34 if it bothers her the bag is not covered, to which she replied: Yes, I can smell the urine and it stinks.
On 8/9/22 at 3:00 PM Surveyor advised Nursing Home Administrator (NHA)-A of concern R34's Care Plan indicated urinary incontinence and there was not a Care Plan for her suprapubic catheter.
3. The Facility policy titled Smoking Policy - Residents revised July, 2017 documents (in part) .
.6. The resident will be evaluated on admission to determine if he or she is a smoker or non-smoker. If a smoker, the evaluation will include:
a. Current level of tobacco consumption;
b. method of tobacco consumption (traditional cigarettes, electronic cigarettes, pipe, etc.);
c. Desire to quit smoking, if a current smoker; and
d. Ability to smoke safely with or without supervision (per a completed Safe Smoking Evaluation).
R58 admitted to the facility on [DATE].
Surveyor reviewed a Facility Reported Incident related to R58 smoking. Surveyor identified no concerns related to the investigation or reporting of the incident. The Facility completed additional smoking assessment after the incident to determine if R58 is still safe to smoke independently. Smoking assessment deemed R58 safe for smoking.
Review of R58's care plan revealed she did not have a care plan for smoking.
On 8/7/22 at 1:41 PM Surveyor observed R58 sitting on a bench outside the facility entrance smoking with several other residents.
On 8/7/22 at 2:19 PM Surveyor spoke with R58 who reported the nurses keep her cigarettes and lighter and she asks for them when she wants to go out to smoke.
On 8/8/22 at 1:05 PM Surveyor observed R58 ask the nurse for a cigarette, which was provided.
Surveyor had multiple observations of R58 sitting outside on the bench smoking safely during survey.
On 8/9/22 at 3:00 PM Surveyor advised Nursing Home Administrator (NHA)-A of concern R58 did not have a care plan for smoking. No additional information was provided.
Based on staff interview and record review, the Facility did not ensure 3 (R12, R34 & R58) of 18 Residents who required a comprehensive care plan had a comprehensive person-centered care plan developed.
* A comprehensive care plan addressing R12's constipation and the use of splints was not developed for R12.
* A suprapubic catheter care plan was not developed for R34.
* A smoking care plan was not developed for R58.
Findings include:
1. R12's diagnoses includes hemiplegia and hemiparesis following non traumatic intracranial hemorrhage affecting left non dominate side, adjustment disorder, and depressive disorder.
The quarterly MDS (minimum data set) with an assessment reference date of 5/10/22 has a BIMS (brief interview mental status) score of 14 which indicates cognitively intact. R12 requires extensive assistance with two plus person physical assist for bed mobility, has transferred only once or twice with two plus person physical assist, doesn't ambulate and is dependent with two plus person physical assist for toilet use. R12 is coded as always being incontinent of bowel. Under functional range of motion indicates R12 has upper extremity impairment on one side.
Surveyor reviewed R12's comprehensive care plans and noted the following care plans:
* At risk for alteration in psychosocial well being initiated 7/30/21.
* At risk for infection related to COVID-19 initiated 7/30/21.
* Current Functional Performance initiated & revised on 8/9/21.
* Summary of Leisure/Social Lifestyle Preference initiated 8/9/21 & revised 2/10/22.
* At risk for injury related to falls initiated & revised 9/27/21.
* At risk for skin breakdown initiated & revised 7/30/21 and initiated & revised 9/27/21.
* ADL (activities daily living) Self Care Performance Deficit initiated & revised 9/27/21.
* I use psychotropic medications initiated & revised 12/2/21.
* I am on anticoagulant therapy initiated & revised 12/2/21.
* Increased risk for weight loss initiated 8/9/22.
The nurses note dated 8/3/22 documents Writer was called to resident's room for resident wanting to go to hospital. Writer asked what was going on and resident said she want Suboxone injection for her constipation. Explained to resident that it is not medication for constipation and offered Laclulose for her constipation. Resident refused. Offered Dulcolax suppository and prune juice but refused as well as all stool softeners. Informed NP [name]. NP [name] came to resident's room, spoke to resident but insist on going to the hospital.
The nurses note dated 8/3/22 documents Resident returned from hospital with the following orders: Stop taking Senna-S 50-8.6 mg and Miralax. New order for Miralax 17 g (grams) daily as needed for constipation.
The hospital after visit summary dated 8/3/22 under diagnoses documents Right lower quadrant abdominal pain & Constipation, unspecified constipation type.
On 8/7/22 at 11:12 a.m. Surveyor observed R12 in bed on her back with the head of the bed elevated. Surveyor observed R12's left hand is contacted and is resting on a pillow. R12 is not wearing any device in her left hand.
On 8/11/22 at 8:05 a.m. Surveyor informed CCM (Clinical Care Manager)-K Surveyor observed R12 has a left hand contracture and inquire what interventions are in place to prevent further decline in R12's range of motion. CCM-K informed Surveyor there is a splint that R12 had which went missing, was reordered and CCM-K believe it's missing again. CCM-K informed Surveyor R12 is suppose to wear the split at all times but she often ask staff to remove the splint. Surveyor asked CCM-K if she knows the status of replacing R12's splint. CCM-K informed Surveyor she did speak to therapy but she doesn't know about the new splint. Surveyor asked CCM-K if she remembers when she spoke to therapy about R12's left hand splint. CCM-K replied no I don't and explained she has spoken to therapy a couple of times but can't pin point the date. CCM-K informed Surveyor she does know at one point there was an order for the left hand splint but they discontinued the order until a new splint is obtained. Surveyor asked CCM-K if she remembers which therapist she spoke to. CCM-K informed Surveyor it may have been TD (Therapy Director)-S who she thinks is the Director. CCM-K indicated there are so many therapist that come & go and they are contracted staff.
On 8/11/22 at 8:16 a.m. Surveyor spoke to OTA (Occupational Therapist Assistant)-R regarding R12. Surveyor informed OTA-R R12 codes on the MDS (minimum data set) for upper extremity impairment on one side and Surveyor had observed R12's left hand to be contracted. Surveyor explained Surveyor had spoke to CCM-K who indicated she had spoken to therapy about a splint for R12 and Surveyor was wondering the status of the splint. OTA-R informed Surveyor she will get back to Surveyor.
On 8/11/22 at 8:48 a.m. OTA-R informed Surveyor she spoke to TD (Therapy Director)-S and TD-S will get back to Surveyor.
On 8/11/22 at 9:06 a.m. Surveyor spoke to TD-S who informed Surveyor they gave R12 a splint around May 6th but wasn't sure of the exact date. TD-S explained R12 was discharged from OT (occupational therapy) on May 6th and it would of been a few days after May 6th that a splint was provided to R12. Surveyor asked TD-S if she knew when R12 should be wearing the splint. TD-S explained she doesn't know the answer as R12 was admitted from another facility wearing the splint. Surveyor asked TD-S if anyone informed her R12's left hand splint is missing now. TD-S replied no not to my knowledge, nothing about a splint just leg pain.
On 8/11/22 at 7:40 a.m. Surveyor asked CCM (Clinical Care Manager)-K who develops or updates care plans. CCM-K informed Surveyor depends on the situation. They review care plans at morning meeting and DON (Director of Nursing)-B would direct who should do the care plans. CCM-K informed Surveyor since she's a LPN (Licensed Practical Nurse) she would review the care plans with DON-B or the care plans would be assigned to someone else such as the MDS nurse, ADON (Assistant Director of Nursing) or DON-B would tell her what to put in the care plan. Surveyor informed CCM-K Surveyor was unable to locate a constipation or splint care plan for R12.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. R75 was admitted to the facility 9/21/20 with diagnoses of juvenile arthritis, bilateral hand contractures and dementia. R75'...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. R75 was admitted to the facility 9/21/20 with diagnoses of juvenile arthritis, bilateral hand contractures and dementia. R75's Significant change Minimum Data Set (MDS) dated [DATE] indicates that R75 requires extensive assistance of 1 staff for bed mobility. R75 has range of motion limitations to their upper and lower extremities including bilateral hand contractures. R75's Braden assessment dated [DATE] indicates R75 has a score of 12, indicating R75 is at high risk for pressure injuries. R75 was enrolled in hospice/comfort care on 1/21/22 due to severe protein malnourishment and failure to thrive.
Surveyor reviewed R75's physician's orders. R75's physician's orders indicate R75 is to wear bilateral palm protectors at all times.
On 8/07/22 at 9:10 AM, R75 was observed laying on their right side wearing hospital gown and incontinence product in bed. R75's bilateral hands are noted without palm protectors in place.
On 8/07/22 at 11:30 AM, R75 was observed laying on their right side wearing hospital gown and incontinence product in bed. R75's bilateral hands are noted without palm protectors in place.
On 8/07/22 at 1:35 PM, R75 was observed laying on their right side wearing hospital gown and incontinence product in bed. R75's bilateral hands are noted without palm protectors in place.
On 8/07/22 at 3:05 PM, R75 was observed laying on their right side wearing hospital gown and incontinence product in bed. R75's bilateral hands are noted without palm protectors in place.
On 8/08/22 at 8:26 AM, R75 was observed laying on their right side wearing hospital gown and incontinence product in bed. R75's bilateral hands are noted without palm protectors in place.
On 8/08/22 at 10:36 AM, R75 was observed laying on their right side wearing a black and white striped sweater and incontinence product in bed. R75's bilateral hands are noted without palm protectors in place. Palm protectors are noted laying on top of R75's bedside table.
On 8/08/22 at 11:35 AM, R75 was observed laying on their right side wearing a black and white striped sweater and incontinence product in bed. R75's bilateral hands are noted without palm protectors in place. Palm protectors are noted laying on top of R75's bedside table.
On 8/08/22 at 1:38 PM, R75 was observed laying on their right side wearing a black and white striped sweater and incontinence product in bed. R75's bilateral hands are noted without palm protectors in place. Palm protectors are noted laying on top of R75's bedside table.
On 8/09/22 at 9:08 AM, R75 was observed laying on their right side wearing hospital gown and incontinence product in bed. R75's bilateral hands are noted without palm protectors in place. Palm protectors are noted laying on top of R75's bedside table.
On 8/10/22 at 9:30 AM, Surveyor conducted interview with Certified Nursing Assistant (CNA)-I. Surveyor asked CNA-I how they would know if a resident has contractures and if they would need specialty equipment such as splints or palm protectors. CNA-I told Surveyor that this information should be on the resident's [NAME].
On 8/10/22 at 9:52 AM, Surveyor conducted an interview with Clinical Care Manager-J. Clinical Care Manager-J stated residents with contractures should have splints or palm guards in place.
On 8/10/22 at 3:20 PM, Surveyor conducted interview with Assistant Director of Nursing (ADON)-H. Surveyor asked ADON-H if a resident has contractures to their extremities if they should have devices in place such as a splint or palm protectors. ADON-H responded that residents with mobility issues or contractures would have orders for splints or mobility devices.
On 8/10/22 at 4:00 PM, Surveyor shared concern with NHA-A related to observations of R75 not wearing bilateral palm protectors. No additional information was provided to Surveyor at this time.
3. R26 was admitted to the facility on [DATE] with diagnoses of vascular dementia with behavioral disturbance, cerebral vascular accident and hemiplegia to left upper and lower extremities. R26's Quarterly MDS (Minimum Data Set) assessment dated [DATE] indicates that R26 requires extensive assistance of 1 staff member with bed mobility. R26 has limited range of motion to their left upper and lower extremities.
On 8/07/22 at 9:10AM, R26 was observed in bed laying on right side wearing hospital gown and incontinence product in bed. R26 is unable to reposition self independently due to hemiplegia to their left upper and lower extremities. R26 requires assistance to move their extremities.
On 8/07/22 at 12:10 PM, R26 was observed in bed with heels directly on their mattress laying on right side wearing hospital gown and incontinence product in bed. R26 requires assistance to move their extremities.
On 8/07/22 at 2:30 PM, R26 was observed in a wheelchair. No splint is noted to R26's left upper extremity.
On 8/08/22 at 9:02 AM, R26 was observed in a wheelchair. A soft arm splint is noted to R26's left upper extremity.
On 8/08/22 at 11:22 AM, R26 was observed in a wheelchair. A soft arm splint is noted to R26's left upper extremity.
On 8/09/22 at 3:17 PM, Surveyor reviewed R26 CNA (Certified Nursing Assistant) care [NAME] form. R26's [NAME] indicates that soft arm splint should be applied while up during the day.
On 8/10/22 at 9:30 AM, Surveyor conducted interview with CNA-I. Surveyor asked CNA-I how they would know if a resident requires use of specialty equipment such splints or palm protectors. CNA-I told Surveyor that this information should be on the resident's [NAME].
On 8/10/22 at 9:52 AM, Surveyor conducted interview with Clinical Care Manager-J. Surveyor asked Clinical Care Manager-J how they would know if a resident requires use of specialty equipment such splints or palm protectors. Clinical Care Manager-J told Surveyor that this information should be on the resident's [NAME] and their physician orders.
On 8/10/22 at 3:20 PM, Surveyor conducted interview with ADON-H. Surveyor asked ADON-H how they would know if a resident requires use of specialty equipment such splints or palm protectors. ADON-H told Surveyor that this information should be on the resident's [NAME] and their physician orders.
On 8/10/22 at 4:00 PM, Surveyor shared serious concerns with NHA-A related to observations of R26 not wearing their left arm splint in accordance with their physicians orders. The facility provided no additional information to the Surveyor at this time.
Based on observation, record review and interview, the facility did not ensure 3 (R12, R75 & R26) of 4 Residents reviewed with limited range of motion received appropriate treatment and services to increase range of motion and/or to prevent further decrease in range of motion.
* R12's left hand splint was misplaced and was not replaced.
* R75 was observed without palm guards.
* R26 hand splint was not consistently on.
Findings include:
1. R12's diagnosis includes hemiplegia and hemiparesis following other non traumatic intracranial hemorrhage affecting left non dominant side.
The quarterly MDS (Minimum Data Set) with an assessment reference date of 5/10/22 under functional range of motion indicates R12 has upper extremity impairment on one side.
On 8/7/22 at 11:12 a.m. Surveyor observed R12 in bed on her back with the head of the bed elevated. Surveyor observed R12's left hand is contacted and is resting on a pillow. R12 is not wearing any device in her left hand.
On 8/7/22 at 1:49 p.m. Surveyor observed R12 asleep in bed on her back with the head of the bed elevated. R12 is not wearing any device in her left hand.
On 8/8/22 at 11:04 a.m. Surveyor observed R12 asleep in bed on her back it the head of the bed elevated. R12 is not wearing any device in her left hand.
On 8/10/22 at 7:37 a.m. Surveyor observed R12 in bed on her back with the head of the bed elevated. R12 is not wearing any device in her left hand.
On 8/11/22 at 8:05 a.m. Surveyor informed CCM (Clinical Care Manager)-K Surveyor observed R12 has a left hand contracture and inquire what interventions are in place to prevent further decline in R12's range of motion. CCM-K informed Surveyor there is a splint that R12 had which went missing, was reordered and CCM-K believe it's missing again. CCM-K informed Surveyor R12 is suppose to wear the split at all times but she often ask staff to remove the splint. Surveyor asked CCM-K if she knows the status of replacing R12's splint. CCM-K informed Surveyor she did speak to therapy but she doesn't know about the new splint. Surveyor asked CCM-K if she remembers when she spoke to therapy about R12's left hand splint. CCM-K replied no I don't and explained she has spoken to therapy a couple of times but can't pin point the date. CCM-K informed Surveyor she does know at one point there was an order for the left hand splint but they discontinued the order until a new splint is obtained. Surveyor asked CCM-K if she remembers which therapist she spoke to. CCM-K informed Surveyor it may have been TD (Therapy Director)-S who she thinks is the Director. CCM-K indicated there are so many therapist that come & go and they are contracted staff.
On 8/11/22 at 8:16 a.m. Surveyor spoke to OTA (Occupational Therapist Assistant)-R regarding R12. Surveyor informed OTA-R R12 codes on the MDS (Minimum Data Set) for upper extremity impairment on one side and Surveyor had observed R12's left hand to be contracted. Surveyor explained Surveyor had spoke to CCM-K who indicated she had spoken to therapy about a splint for R12 and Surveyor was wondering the status of the splint. OTA-R informed Surveyor she will get back to Surveyor.
On 8/11/22 at 8:48 a.m. OTA-R informed Surveyor she spoke to TD (Therapy Director)-S and TD-S will get back to Surveyor.
On 8/11/22 at 9:06 a.m. Surveyor spoke to TD-S who informed Surveyor they gave R12 a splint around May 6th but wasn't sure of the exact date. TD-S explained R12 was discharged from OT (occupational therapy) on May 6th and it would have been a few days after May 6th that a splint was provided to R12. Surveyor asked TD-S if she knew when R12 should be wearing the splint. TD-S explained she doesn't know the answer as R12 was admitted from another facility wearing the splint. Surveyor asked TD-S if anyone informed her R12's left hand splint is missing now. TD-S replied no not to my knowledge, nothing about a splint just leg pain.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility did not ensure that 3 (R66, R34 and R61) of 3 residents reviewed...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility did not ensure that 3 (R66, R34 and R61) of 3 residents reviewed received appropriate treatment and services related to catheter care.
* R66 was observed with their catheter bag not having a privacy cover or protective barrier on 8/7/22 and 8/8/22.
* R34's catheter bag was uncovered and hanging above the level of her bladder.
* R61's catheter collection bag was observed with no catheter bag cover hanging off bed rail.
Findings include:
The Facility policy titled, Catheter Care, Urinary revised September, 2014 documents (in part) .
.Purpose:
The purpose of this procedure is to prevent catheter-associated urinary tract infections.
Preparation:
1. Review the resident's care plan to assess for any special needs of the resident.
Maintaining Unobstructed Urine Flow
3. The urinary drainage bag must be held or positioned lower than the bladder at all times to prevent the urine in the tubing and drainage bag from flowing back into the urinary bladder.
1. R66 was admitted to the facility on [DATE] with paraplegia and neurogenic bladder. R66s Quarterly MDS (Minimum Data Set) assessment dated [DATE] indicates that R66 has a suprapubic catheter in place since 3/10/22.
On 8/7/22 at 9:52 AM, Surveyor conducted interview with R66. R66 shared with Surveyor that they have concerns of their catheter bag never getting emptied and that they are worried about the urine backing up into the catheter system. R66's catheter bag was noted without a privacy cover at this time and is noted laying on the floor next to R66's bed.
On 8/8/22 at 8:07 AM, Surveyor conducted observations of R66's catheter bag. R66's catheter bag was noted without a privacy cover at this time and noted laying on the floor next to R66's bed with approximately 200 cc of urine in bag.
On 8/10/22 at 3:20 PM, Surveyor conducted interview with ADON (Assistant Director of Nursing)-H. Surveyor asked ADON-H if residents with catheter bags should have privacy bags. ADON-H told Surveyor Yes. Surveyor asked ADON-H if resident catheter bags should be resting on the floor without a barrier in place. ADON-H responded No, they should not. On 8/10/22 at 4:00 PM, Surveyor informed NHA (Nursing Home Administrator)-A of the above findings. The facility did not provide any additional to the Surveyor at this time.
2. R34 was admitted to the facility on [DATE]. Urology placed a suprapubic catheter on 7/8/22.
On 8/7/22 at 9:22 AM Surveyor observed R34 sitting in the wheelchair in her room. Surveyor observed R34's catheter bag hanging on the right side of the wheelchair on the metal frame under the arm rest, uncovered and above the level of her bladder.
On 8/8/22 at 9:23 AM Surveyor observed R34 sitting in the wheelchair in the bathroom. Surveyor observed the catheter bag hanging on the right side of the wheelchair on the metal frame under the arm rest, uncovered and above the level of her bladder.
On 8/9/22 at 7:20 AM Surveyor observed R34 sitting in the wheelchair in her room. Surveyor observed the catheter bag hanging on the right side of the wheelchair on the metal frame under the arm rest, uncovered and above the level of her bladder.
On 8/10/22 at 9:51 AM Surveyor asked R34 if staff always hangs her catheter bag on the side of her wheelchair under the armrest. R34 stated: Yes. Surveyor asked if the bag is ever covered, to which R34 stated: No. Surveyor asked R34 if it bothers her the bag is not covered, to which she replied: Yes, I can smell the urine and it stinks.
On 8/9/22 at 3:00 PM Surveyor advised Nursing Home Administrator (NHA)-A of concern related to multiple observations of R34's catheter hanging uncovered, above the level of her bladder. No additional information was provided.
3. On 08/09/22 10:11 AM, Surveyor observed R61 from the hallway lying in bed.
R61's catheter collection bag was observed with no catheter bag cover hanging off bed rail.
R61 did not respond to Surveyor's attempts to interview her.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the Facility did not ensure the necessary care and services to provide respir...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the Facility did not ensure the necessary care and services to provide respiratory care for 1 (R19) of 1 Residents receiving oxygen care.
* R19 has a physician order for 2 liters of oxygen per minute. R19 was observed receiving oxygen at 3 liters.
Findings include:
The quarterly MDS (Minimum Data Set) with an assessment reference date of 5/20/22 documents a BIMS (brief interview mental status) score of 3 which indicates severely impaired. Oxygen therapy is checked for while a Resident.
The physician orders with an order date of 7/20/22 documents Administer oxygen at 2L (liters)/min (minute) per nasal cannula to keep oxygenation level above 92%.
The CNA (Certified Nursing Assistant) [NAME] as of 8/9/22 under the section monitoring documents Oxygen settings: I have O2 (oxygen) via nasal prongs @ (at) 2L continuously/min.
On 8/8/22 at 8:15 a.m. Surveyor observed R19 in bed on her back with the head of the bed elevated. R19 is receiving oxygen via nasal cannula at 3 liters per minute.
On 8/9/22 at 8:46 a.m. Surveyor observed R19 in bed on back with the head of the bed elevated. R19's oxygen is at 3 liters per minute. R19's oxygen is not in her nostrils and the tubing of the oxygen is in R19's mouth.
On 8/9/22 at 9:33 a.m. Surveyor observed R19 in bed on her back with the head of the bed elevated. Surveyor observed R19 is receiving oxygen via nasal cannula at 3 liters.
On 8/9/22 at 1:40 p.m. Surveyor observed R19 continues to be in bed on her back with the head of the bed elevated. R19 is receiving oxygen via nasal cannula at 3 liters and the oxygen tubing is dated 8/8.
On 8/9/22 at 2:19 p.m. Surveyor asked CCM (Clinical Care Manager)-K how many liters should R19's oxygen be set at. CCM-K informed Surveyor she will need to check but knows it's for comfort. CCM-K informed Surveyor R19 was signed on for hospice today and then informed Surveyor their orders say 2 liters. Surveyor informed CCM-K of the observations of R19 receiving oxygen at 3 liters.
On 8/9/22 at 4:20 p.m. Administrator-A and Corporate Consultant-M were informed of the above.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview the facility did not ensure that 2 (R46, R35) of 2 residents who required dia...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview the facility did not ensure that 2 (R46, R35) of 2 residents who required dialysis received such services consistent with the standards of practice, the comprehensive care plan and the resident's goals and preferences.
* R46 did not have a physician's order documenting the frequency of dialysis treatments, or the location of the dialysis center in the community. R46 also did not have a physician's order documenting the care, monitoring, and location of the dialysis access site. R46's care plan did not accurately document the days that R46 receives dialysis treatment nor document the location of the dialysis access site.
* The facility did not have orders for and was not monitoring of R35's dialysis port. R35's care plan was not updated to reflect R35's dialysis port was changed from her left upper extremity to her chest area.
Findings include:
1. R46 was admitted [DATE] with diagnoses that include End Stage Renal disease on hemodialysis, vascular dementia without behavioral disturbances, DM2 (Diabetes Mellitus type 2), and PVD (Peripheral Vascular Disease).
R46's dialysis care plan initiated on 10/14/2020 documents the following:
Dressing as ordered to access site. Monitor bruit and thrill, color, warmth, redness,
edema, drainage, bleeding. Report any abnormal findings to MD (Medical Doctor)
Date Initiated: 10/14/2020
Created on: 10/14/2020
Monitor/document/report to MD PRN (as needed) any s/sx (signs and symptoms) of infection to access site: Redness,
Swelling, warmth or drainage.
Date Initiated: 10/14/2020
Created on: 10/14/2020
I receive dialysis at [name of dialysis facility] on Tues/Thurs/Sat at 10:30. Their
phone number is [dialysis phone number]. Please call to notify them of any changes in my
condition or if I am unable to make my appointment.
Date Initiated: 06/23/2022
Created on: 06/23/2022
Surveyor noted R46's care plan did not document the type or location of R46's dialysis access site and R46's care plan has dialysis days as Tuesday, Thursday, and Saturday.
On Monday 08/08/2022, at 08:55 am, surveyor interviewed R46, who was observed in his room, sitting upright in his wheelchair. R46 informed surveyor he would eat breakfast prior to leaving the facility for dialysis. Surveyor noted a lamenated sheet of paper hung on a cabinet on R46's unit that documented residents' dialysis information. R46 had dialysis days of Mondays, Wednesdays, and Fridays listed on this documentation.
Surveyor reviewed R46's current physician's orders from August 2022 and noted there are no physician's orders documenting what days R46 goes to dialysis, the location of the dialysis clinic, where R46's dialysis access site is located or the type of assessment and monitoring the dialysis access site requires. Surveyor was unable to locate documentation that R46's dialysis access was being assessed and monitored on a routine basis.
On 08/11/2022 at 08:30 am surveyor interviewed clinical care manager LPN (licensed practical nurse)-K regarding R46's dialysis access site location and monitoring. LPN-K informed surveyor that the site should be monitored before and after R46 goes to dialysis and that staff should be checking it daily on night shift. LPN-K also said that there is no documentation regarding the access site, we were told it was a standard of practice. When surveyor asked LPN-K how staff would know to monitor the site, LPN-K stated you should have learned that in training. Surveyor asked LPN-K how would staff know where the dialysis access site is located? LPN-K stated someone should have told you. LPN-K also told surveyor it maybe in the care plan, but knows it is not on R46's regular (physician's) orders. LPN-K said there is the dialysis communication sheets and hopefully the nurse is checking the patient to say where the dialysis access site is. LPN-K reviewed R46's care plan with surveyor and could not locate access site information.
Surveyor asked LPN-K how staff would know when R46 goes to dialysis. LPN-K stated the care plan documents what days R46 goes to dialysis: Tuesdays, Thursdays, and Saturdays. LPN-K stated R46 had a time when R46 was going to dialysis Tuesdays, Thursdays, and Saturdays, but it was switched and apparently it was not updated in the care plan. LPN-K stated there is documentation at the nurse's station and showed surveyor a sheet of paper (the same paper that surveyor noted was hung on the cabinet on R46's unit) that had R46's name and the days of dialysis which where Mondays, Wednesdays, and Fridays.
Surveyor reviewed R46's dialysis communication between the nursing facility and the dialysis facility which is documented on a sheet of paper called Hemodialysis Communication. Surveyor noted starting on April 18, 2022, R46's Hemodialysis communication had dates of service that coincided with Mondays, Wednesdays, and Fridays. Prior to April 18, 2022, the dates of service were on Tuesdays, Thursdays, and Saturdays. Surveyor also noted the information that should be entered by the nursing facility is not consistently completed . On the Hemodialysis communication forms from 03/12/2022 and 07/25/2022, the facility did not document that R46's access site had been assessed.
Nursing Home Administrator (NHA)-A and the Corporate Consultant-M were advised of this concern on 08/10/2022.
2. R35's medical record was reviewed on 8/9/22. R35 was admitted into the facility on 6/7/22 and transferred to the hospital on 6/10/22 after falling and fracturing her arm. R35 was readmitted into the facility on 6/21/22. On 7/1/22, R35 was transferred to the hospital and readmitted into the facility on 7/30/22.
On 8/9/22 at 10:19 am, Surveyor spoke with R35 who stated on 6/10/ 2022 she fell here at the facility after coming back from dialysis. R35 stated she fell and broke her left arm. R35 stated she thought she stayed in the hospital for a couple of days. R35 reported since breaking her arm, she is not allowed to use her walker (with a seat) unless with therapist is in attendance. R35 stated she leaves for dialysis at 4:15 am, chair time from 5-8:30 am and is back by 9:30 am however they are using the catheter site (pointing to her chest area) which is quicker so starting to get home by 9:00 am.
R35 stated she is not able to have showers due to her catheter up in right chest area. Early in the morning on dialysis days the CNA washes me up. R35 stated she receives dialysis 3 times a week on Monday's, Wednesday's, and and Friday's.
On 8/9/22 at 2:16 PM Surveyor interviewed Assistant Director of Nursing (ADON) H who stated, on 8/8/22 a Surveyor from the survey team informed ADON H that R35's medical record did not have orders for the monitoring of R35's dialysis site.
ADON H reported she obtained the orders (last evening 8/8/22) and placed the orders for the monitoring onto R35's MAR with a start date of 8/8/22 of 2230 (10:30 pm).
ADON H also informed this surveyor that the facility has a dialysis communication book that is stored at the nurses station and is sent with R35 to dialysis. ADON H reported R35 left the book at dialysis yesterday (8/8/22) and will be bringing it back tomorrow 8/10/22. ADON H stated that yesterday dialysis faxed over the communication forms for 8/1, 8/3, 8/5 and 8/8/22.
Surveyor reviewed the MAR which indicated:
~ Hemodialysis pt. nrsing measure: Hemodialysis catherter marked clearly with tape at bed time for monitoring start 8/8/22 2000 (8:00 pm)
~ Hemodialysis pt nursing measure: ensure clamps are closed every shift for monitoring start 8/8/22 2230 (10:30pm)
~ Give am meds prior to dialysis on M-W-F. Dialysis M/W/F pick up 4am. Son transports. start 8/10/22 0300 (3:00 am)
Surveyor reviewed R35's care plan for dialysis which documents:
Problem: I have renal failure and require hemodialysis. Initiated on 6/22/22
Approaches initiated 6/22/22 include in part:
I receive dialysis . M-W-F. My son picks me up at 4:15 am .
My port/graft/fistuala sight is left UE (upper extremity).
Surveyor noted R35's care plan was not updated to reflect R35's hemodialysis catheter site is now located in her upper chest area as she is wearing a sling on her broken arm and her broken arm cannot be used as a dialysis port at this time.
On 8/9/22, Surveyor discussed with ADON H R35's dialysis care plan has not been updated since R35's dialysis port has been changed.
On 8/10/22, ADON H provided Surveyor with a revised dialysis care plan indicating to Monitor hemodialysis site to [NAME] chest. Monitor warmth, redness, edema, drainage, bleeding and to report any abnormal findings to MD. created on 8/9/22.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility did not always provide pharmaceutical services to meet the needs of 1 of 1 (R46) residents.
On 2/10/22 R46's Advanced Practice Nurse Practitioner (AP...
Read full inspector narrative →
Based on record review and interview the facility did not always provide pharmaceutical services to meet the needs of 1 of 1 (R46) residents.
On 2/10/22 R46's Advanced Practice Nurse Practitioner (APNP) wrote an order to hold Metoprolol prior to dialysis. This medication was not always held prior to dialysis. On 7/25/22 the dialysis communication form for the facility documented for the facility to make sure R46 was compliant with blood pressure medications. The facility did not follow up with R46's APNP/MD regarding dialysis' communication.
Findings include:
R46 's August physician orders documents:
Metoprolol Tartrate Tablet 25 MG
Give 0.5 tablet by mouth every 12 hours for HTN (Hypertension) Do not give before dialysis. Hold for SBP <100, HR <50
On 02/10/2022, R46's medical record documents R46 was seen by the APNP (advanced practice nurse practitioner) who documents, resident refuses meds (medications) before dialysis because they do not make him feel well. The APNP also wrote new Metoprolol instructions to hold prior to dialysis.
Review of the EMAR (Electronic Medical Record) from July 25, 2022 through August 8, 2022 documents that Metoprolol Tartrate 25mg 1/2 tab was given on the following dates prior to resident going to dialysis:
7/25/2022 at 0800 (8:00am)
7/29/2022 at 0846 (8:46am)
8/1/2022 at 0905 (9:05am)
8/3/2022 at 0932 (9:32am)
8/8/2022 at 0909 (9:09am)
During that time frame, Metoprolol Tartrate 25mg 1/2 tab was documented to be held 2 times: on 07/27/2022 and 08/05/2022.
On 7/25/2022, R46's dialysis communication form (to the facility) notes: ensure pt (patient) is compliant with blood pressure medications. Surveyor could not locate any documentation the facility followed up on this communication.
On 08/11/2022 at 8:30am, surveyor interviewed Clinical Care Manager, LPN (licensed practical nurse)-K. LPN-K told surveyor that R46 is supposed to get medications prior to dialysis; R46 refuses sometimes. Surveyor questioned why the Metoprolol was being given prior to dialysis when the order states to hold the medication. LPN-K stated the facility has been getting a call from dialysis regarding R46 having high blood pressure and the dialysis center would like R46 to take the Metoprolol prior to coming in. LPN-K stated there should have been a verbal order to give the Metoprolol prior to dialysis. LPN-K could not find any documentation related to this request from dialysis.
Surveyor asked if this communication would have been discussed with the facility's NP/MD, (nurse practitioner/medical doctor). LPN-K stated the NP here would be notified.
Surveyor then asked if the order from dialysis to give the Metoprolol prior to receiving dialysis was not transcribed, would it be the expectation that the nurses follow the current order? LPN-K said yes.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the Facility did not ensure each Resident's drug regimen was free from unnecessary drugs f...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the Facility did not ensure each Resident's drug regimen was free from unnecessary drugs for 2 (R19 & R71) of 2 Residents reviewed.
R19 & R71 received an antibiotic for UTI (urinary tract infection) without adequate indications for its use.
Findings include:
1. R19's quarterly MDS (minimum data set) with an assessment reference date of 5/20/22 documents a BIMS (brief interview mental status) score of 3 which indicates severe impairment. R19 is coded as always being incontinent of urine.
The nurses note dated 3/24/22 documents Stat KUB (kidney, ureter, bladder) and labs were notified to on call NP (nurse practitioner) for [name of physician]. KUB was negative for bowel obstruction. WBC (white blood count) of 12.2, BUN (blood, urea, nitrogen) of 38 and Creatinine of 1.41 were notified. Order for UA/C&S (urinalysis/culture & sensitivity) if indicated.
The nurses note dated 3/25/22 documents UA collected by writer via straight cath (catheter) and awaiting pickup from lab.
The nurses note dated 3/25/22 documents Writer called lab to let them know the UA is ready to be picked up. Per lab they will get the UA in the morning.
The nurses note dated 3/25/22 documents Pt (patient) is being followed for abdominal distention and needing a UA. Pt is alert and orientated per baseline. UA collected by writer via the straight cath and awaiting pick up in the fridge on [nursing unit]. Pt has no c/o (complaint of) pain or discomfort at this time. Pt is in bed sleeping. Changed and repositioned.
The nurses note dated 3/26/22 documents Pt is being followed for abdominal distention/pain and awaiting a C/S from the UA. Pt is alert and orientated per baseline. Pt has no c/o pain or discomfort at this time. Pt is in bed sleeping comfortably.
The nurses note dated 3/27/22 documents Pt is being followed for abdominal distention/pain and awaiting a C/S from the UA. Pt is alert and orientated per baseline. Pt has no c/o pain or discomfort at this time. Pt is in bed sleeping comfortably.
The nurses note dated 3/28/22 documents Residents urine c/s obtained and reviewed by n.p new orders received for bactrim ds one tab po (by mouth) q (every)12hr (hours) x 5 days. acidophilus 1 capsule po q12hr x 7 days.
The nurses note dated 3/29/22 documents Res. (Resident) alert and responsive, mentation at baseline. No adverse reaction noted to ABT (antibiotic) for UTI (urinary tract infection). Fluids offered and enc (encouraged). No verbalization of dysuria. T. (temperature) 97.3.
The nurses note dated 4/3/22 documents No adverse reaction noted to ABT for UTI which is now complete. Fluids offered and enc. No verbalization of dysuria. T.97.2.
Surveyor noted there is no documentation of urinary symptoms prior to R19 being placed on an antibiotic.
The einteract SBAR (situation background assessment recommendation) dated 4/13/22 indicates the change in condition is altered mental status. The outcomes of physical assessment for mental status evaluation is altered level of consciousness (hyperalert, drowsy but easily aroused, difficult to arouse). For functional status evaluation documents Needs more assistance with ADLs (activities daily living) other. The GU (genitourinary)/Urine status evaluation is blank as the instructions are to report positive findings. The nursing observations, evaluation, and recommendations are possible UTI (urinary tract infection). New orders for stat labs and stat UA for C/S straight cathed for urine specimen.
The nurses note dated 4/13/22 documents Labs drawn and UA given to phlebotomist at 2:10 p.m. [name of son] notified of change of condition at 3:45 p.m.
The nurses note dated 4/13/22 documents Resident monitored, notified MD (medical doctor) of lab results. UA and chest x-ray ordered.
The nurses note dated 4/15/22 documents Resident UA positive. C & S results obtained. NP aware of results and new orders obtained. Resident starting Cefuroximine 250 mg every 12 hours times 10 days for UTI. Probiotic ordered BID (twice daily) times 14 days. Order transcribed. Resident POA (power of attorney) [name] in agreement with new orders.
The nurses note dated 4/16/22 documents Sleeping well, no c/o (complaint of) dysuria, afebrile. Fluids encourged and offered.
Surveyor noted there is no documentation of urinary symptoms prior to R19 being placed on an antibiotic.
On 8/9/22 at 12:57 p.m. Surveyor asked Administrator-A what standard of practice the Facility uses for their definition of infections. Administrator-A informed Surveyor Mcgeers.
On 8/9/22 at 2:03 p.m. Surveyor asked CCM (Clinical Care Manager)-K if the Facility uses Mcgeers as the standard of practice for their definition of infections. CCM-K replied yes and explained she doesn't take care of infection control. CCM-K informed Surveyor DON (Director of Nursing)-B was the one responsible after their infection preventionist left. Surveyor inquired if the Facility uses a form which shows how a Resident meets the Facility's definition of infection. CCM-K informed Surveyor the person covering the infection control role would be responsible but she hasn't personally seen them use it. CCM-K informed Surveyor the NP would order the antibiotic.
On 8/9/22 at 4:20 p.m. during the end of the day meeting with Administrator-A and Corporate Consultant-M Surveyor informed Facility staff R19 was placed on an antibiotic on 3/28/22 & 4/15/22 for a UTI. Surveyor requested information on how R19 met the Facility's definition of infection for an UTI.
On 8/10/22 at 2:31 p.m. Administrator-A informed Surveyor he does not have any information on how R19 met their definition of infection to be treated with an antibiotic for an UTI on 3/28/22 & 4/15/22. Corporate Consultant-M informed Surveyor that was a DON (Director of Nursing) role.
2. R71's quarterly MDS (minimum data set) with an assessment reference date of 7/16/22 has a BIMS (brief interview mental status) score of 7 which indicates severe impairment. R71 is coded as being occasionally incontinent of urine.
The eMar (electronic medication administration record) dated 7/26/22 documents Macrobid capsule 100 mg (milligrams) with directions to give one capsule by mouth two times a day for UTI (urinary tract infection) for 5 days.
Surveyor reviewed R71's July MAR and noted R71 starting receiving Macrobid 100 mg twice daily on 7/27/22 ending with one dose on 7/31/22.
Surveyor was unable to locate any nurses notes regarding urinary signs/symptoms prior to R71 receiving an antibiotic on 7/27/22 for UTI.
On 8/9/22 at 8:57 a.m. Surveyor reviewed the Facility's July 2022 monthly infection control log (line list) and noted for R71 documents under infection definition met is N which indicates no. For classification has a X for not infected.
On 8/9/22 at 12:57 p.m. Surveyor asked Administrator-A what standard of practice the Facility uses for their definition of infections. Administrator-A informed Surveyor Mcgeers.
On 8/9/22 at 2:03 p.m. Surveyor asked CCM (Clinical Care Manager)-K if the Facility uses Mcgeers as the standard of practice for their definition of infections. CCM-K replied yes and explained she doesn't take care of infection control. CCM-K informed Surveyor DON (Director of Nursing)-B was the one responsible after their infection preventionist left. Surveyor inquired if the Facility uses a form which shows how a Resident meets the Facility's definition of infection. CCM-K informed Surveyor the person covering the infection control role would be responsible but she hasn't personally seen them use it. CCM-K informed Surveyor the NP would order the antibiotic.
On 8/9/22 at 4:20 p.m. during the end of the day meeting with Administrator-A and Corporate Consultant-M Surveyor informed Facility staff R71 was placed on an antibiotic on 7/27/22 for an UTI. Surveyor requested information on how R71 met the Facility's definition of infection for an UTI.
On 8/10/22 at 2:31 p.m. Administrator-A informed Surveyor he does not have any information on how R71 met their definition of infection to be treated with an antibiotic for an UTI. Corporate Consultant-M informed Surveyor that was a DON (Director of Nursing) role.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the Facility did not ensure that 1 (R71) of 5 Resident's medications reviewed were free from unnecessary drugs.
* R71 had a PRN (as needed) order for an anti-anx...
Read full inspector narrative →
Based on interview and record review, the Facility did not ensure that 1 (R71) of 5 Resident's medications reviewed were free from unnecessary drugs.
* R71 had a PRN (as needed) order for an anti-anxiety medication, Lorazepam, that did not have a documented rationale in R71's medical record that indicated the duration for the PRN order beyond 14 days. The last AIMS (Abnormal Involuntary Movement Scale) is dated 3/8/21.
Findings include:
The Use of Psychotropic Medication Policy dated 7/2/2021 under Policy Explanation and Compliance Guidelines documents;
8. Residents who receive an antipsychotic medication will have an Abnormal Involuntary Movement Scale (AIMS) test performed on admission, quarterly, with a significant change in condition, change in antipsychotic medication, PRN (as needed) or as per facility policy. and 9. PRN orders for all psychotropic drugs shall be used only when the medication is necessary to treat a diagnosed specific condition that is documented in the clinical record, and for a limited duration (i.e. 14 days).
R71's diagnoses includes dementia with behavioral disturbance and anxiety disorder. R71 receives hospice services.
The quarterly MDS (minimum data set) with an assessment reference date of 7/16/22 documents a BIMS (brief interview mental status) score of 7 which indicates severe impairment. Section N- Medications for indicate the number of days the resident received the following medications during the last 7 days is coded 7 for antipsychotic and antianxiety.
R71 receives Quetiapine Fumarate (Seroquel) 50 mg (milligrams) every 8 hours related to anxiety disorder & panic disorder with a start date of 8/8/22. Surveyor noted R71 received Seroquel 25 mg every 8 hours prior to this new order.
Surveyor noted the last AIMS completed for R71 is dated 3/8/21.
On 8/11/22 at 7:49 a.m. Surveyor informed CCM (Clinical Care Manager)-K R71 receives Seroquel and inquired where Surveyor would be able to locate an AIMS for R71. CCM-K informed Surveyor the AIMS would be under the assessment uda (user defined assessment) if she has one. CCM-K looked at R71's electronic medical record and informed Surveyor her last one was done a year ago and indicated the date was 3/8/21. Surveyor asked CCM-K who is responsible for completing a Resident's AIMS. CCM-K informed Surveyor usually the nurse on the unit.
R71 also receives Lorazepam 0.5 mg with directions to give 0.5 mg by mouth every 4 hours as needed for anxiety and restlessness. The start date for this medication is 4/12/22 and there is no end date.
On 8/11/22 at 8:35 a.m. Surveyor reviewed R71's hospice binder and noted an order electronically signed on 6/24/22 by [name of] Facility physician and [name of] hospice physician with instructions of PO (by mouth) Lorazepam 0.5 mg every four hours as needed for anxiety and restlessness. There is a start date of 4/12/22 and does not have an end date.
R71 received Lorazepam 0.5 mg on 7/1/22, 7/2/22, 7/5/22, 7/6/22, 7/7/22, 7/8/22, 7/20/22, 7/29/22, 8/7/22 & 8/9/22.
On 8/11/22 at 7:49 a.m. Surveyor informed CCM-K Surveyor is unable to locate an end date for R71's PRN Lorazepam. CCM-K informed Surveyor there is no stop date because R71 is hospice and they ordered the medication for restlessness, anxiety, and any terminal restless.
On 8/11/22 at 8:46 a.m. Surveyor informed CCM-K even though R71 is on hospice a stop date is required for R71's PRN Lorazepam.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. R56 was admitted to the facility on [DATE] with diagnoses of subdural hemmorage, metabolic encephalopathy and dementia withou...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. R56 was admitted to the facility on [DATE] with diagnoses of subdural hemmorage, metabolic encephalopathy and dementia without behavioral disturbance. R56's admission MDS (Minimum Data Set) dated [DATE] documents BIMS (Brief Interview for Mental Status) score of 03, indicating R56 is severely cognitively impaired for daily decision making skills. R56's MDS indicates resident requires supervision to limited assistance with activities of daily living including transfers and ambulation. R56's MDS indicates R56 exhibits wandering behavior on a daily basis. An Elopement assessment dated [DATE] indicates resident is at risk for elopement. R56's care plan dated [DATE] indicates resident is at risk for falls and includes intervention of wearing proper footwear when out of bed. R56's care plan dated [DATE] indicates resident is at risk for elopement due to attempts to leave facility. Interventions include redirection of resident from exit doors, distract from wandering with pleasant diversions including offering activities and snacks, and placement of a wanderguard bracelet to the left ankle.
On [DATE], R56 eloped from the facility and was found approximately a mile from the facility not wearing shoes. Surveyor reviewed R56's medical record including care plans. R56's risk for elopement care plan dated [DATE] did not include revisions with new interventions after R56's elopement on [DATE].
On [DATE] at 4:00 PM, Surveyor shared concern with NHA-A related to R56's care plan being without revision and additional interventions after R56's elopement on [DATE]. NHA-A told Surveyor that they would look for additional information. On [DATE] at 8:00 AM, Surveyor noted R56's elopement care plan was updated on [DATE] to include 15 minute resident checks as a new intervention.
6. R75 was admitted to the facility [DATE] with diagnoses of juvenile arthritis, bilateral hand contractures and dementia. R75's Significant change MDS dated [DATE] indicates that R75 was enrolled into hospice services on [DATE]. Surveyor reviewed R75's medical record including care plans.
R75's Advanced Directive Care plan initiated [DATE] indicates that R75 code status is a Full code. Interventions dated [DATE] include that a resident's advanced directives wishes will be known and to review advanced directives on file if applicable.
Surveyor reviewed R75's physician's orders. Surveyor noted an order dated [DATE] for DNR and comfort care.
On [DATE] at 1:35 PM, Clinical Care Manager-K was interviewed by Surveyor. Surveyor asked Clinical Care Manager-K how nursing staff would know how to identify a resident's code status. Clinical Care Manager-K told Surveyor that if a resident had a No Code/DNR status that this would be reflected in the EMR (electronic medical record) and DNR documents would be a residents hard chart. Surveyor asked Clinical Care Manager-K if a resident's code status should be reflected on their care plan. Clinical Care Manager-K responded Yes.
On [DATE] at 4:00 PM, Surveyor shared concerns with NHA-A that R75's care plan indicates R75's code status to be a Full Code/CPR while their physician's orders in the EMR indicate the R75 is on Hospice with a DNR code status. The facility did not provide any additional information to Surveyor at this time.
3. R71 was admitted to the facility on [DATE] with diagnoses which includes dementia with behavioral disturbances, hypertension, anxiety disorder, panic disorder, and depressive disorder.
The nurses note dated [DATE] documents Observed res (resident) lying on her right side in fetal position in skylight south dining room area. Wheelchair was behind res. no c/o (complaint of) pain or discomfort. cervical collar in place. ROM WNL (range of motion within normal limits) RN (Registered Nurse) present. Called [name] and order to send out to [name of hospital] ER (emergency room). Contacted friend [name]. [Name of] ambulance contacted. Res remained on the floor. Pillow placed under her head. T (temperature) 97.6 P (pulse) 72 R (respirations) 18 B/P (blood pressure)125/71 Pox (pulse oximetry) 98 RA (room air).
The Facility did not revise R71's fall care plan after this fall.
The nurses note dated [DATE] documents Resident was in the dining room eating breakfast and somehow got up and walked away from her Broda chair. Found by staff on the floor. Writer was called to assess resident. Resident on the floor with her cervical collar in place. Resident denied pain when asked. Resident to be sent out to hospital for eval and treat for existing neck injury. Updated Guardian [name] and informed NP [name]. Called up [name of] Ambulance for transport and [name of hospital] nurse [name] for report.
The Facility did not revise R71's fall care plan after this fall.
The nurses note dated [DATE] documents Resident found on the floor @ 11:30 a.m. Found side lying on the floor next to Broda chair in dining room in lead unit. Resident is alert. Cervical collar in place. Informed NP [name]. Updated Guardian [name]. Called up [name] Ambulance to transport . Called up [hospital name] ER nurse [name] to give report. Sent resident to ER for further eval and treat. Left message to phone of Caseworker [name] to call facility for update.
The Facility did not revise R71's fall care plan after this fall.
The nurses note dated [DATE] documents Was notified by RN supervisor that my resident fell. The aides on that hall said they found her on the floor crawling to her bed, she was in her wheelchair the last they saw her. I notified the doctor on call as well as her #1 emergency contact. I called [name] but they told me to call 911 because they already had two pickups from this facility. Vital signs 116/68 Pulse 77 T 97.3 and R 18. No pain or injuries noted.
The Facility did not revise R71's fall care plan after this fall.
The nurses note dated [DATE] documents Patient noted to be lying on right side on dining room floor on Skylight South unit. UWF (unwitnessed fall) with abrasion noted to left knee. RN (Registered Nurse) [name] assessed with ROM (range of motion) intact. C/O pain to right hip. T 96.9; BP 132/88; P 96; R 16; PO2 94%. Patient transferred back to Broda chair with extensive assist/2 staff.
The Facility did not revise R71's fall care plan after this fall.
The nurses note dated [DATE] documents Resident crawled out of bed x2. Hit Left knee. Knee bleeding cleansed area and applied dressing. Unwitnessed fall. Did not hit head. Called Nurse Practitioner and 911. Called friend. Incident happened 515am. Ambulance came sent to [hospital name].
The Facility did not revise R71's fall care plan after this fall.
The nurses note dated [DATE] documents Informed by CNA (Certified Nursing Assistant) that resident slid self from Broda chair while dinner trays were being passed, no injury noted, assisted back into Broda chair with 2 assist and gait belt. Call placed to [name of] Hospice and spoke with [name] RN, will send out nurse to assess resident. Left voice mail for guardian [name] to call facility and voice mail left for CM (Case Manager) [name] to call facility.
The Facility did not revise R71's fall care plan after this fall.
The nurses note dated [DATE] documents Resident monitored for fall. Agitated this afternoon. Had an unwitnessed fall in hallway. Managed to get to her room and get into bed. Hospice and POA notified. Hospice nurse will be coming tomorrow morning to evaluate her.
The Facility did not revise R71's fall care plan after this fall.
4. R46's care plan was not revised to reflect current status of having bilateral above the knee amputations.
R46 was admitted on [DATE] with primary diagnosis of end stage renal disease on hemodialysis, diabetes mellitus type 2, and peripheral vascular disease.
Surveyor reviewed R46's medical record which documents that R46 had his left leg amputated above the knee on [DATE] and his right leg amputated above the knee on [DATE].
R46's current care plan, revision date of [DATE], documents: I have an ADL (activities of daily living) self care performance deficit d/t (due to) left above the knee amputation, motivation deficit. Interventions on the ADL (activities of daily living) care plan include: I need staff to set up my supplies for ADL care, initiated on [DATE]; Praise all efforts at self care and focus on my abilities, initiated on [DATE]; Encourage me to use call bell for assistance, initiated on [DATE]; Bed Mobility: Encourage me and assist with repositioning in bed routinely and prn (as needed), initiated on [DATE]; Transfer: I require assist of 1 and slide board set up for transfers, initiated [DATE] and revised on [DATE].
Surveyor could not locate any mention of the [DATE] right above the knee amputation in R46's current care plan.
On [DATE] at 0855, R46 gave surveyor permission to enter his room where R46 was sitting upright in his wheelchair. At this time surveyor observed that R46 had bilateral lower extremeties amputated above the knees.
On [DATE], at 1:46 PM, surveyor interviewed the Assistant Director of Nursing (ADON)-H, who stated that she started working at the facility in December of last year and she thought R46 had both legs amputated at that time. Surveyor asked ADON-H who is responsible for updating the care plans. ADON-H stated that the Minimum Data Set (MDS) nurse is responsible for updating the care plan when an MDS is completed and outside of that the Interdisciplinary Team (IDT) will meet in the morning to talk about updates that should be made. At that time, one of the IDT members should be updating the care plans.
Nursing Home Administrator (NHA)-A and the Corporate Consultant-M were advised on this concern on [DATE].
Surveyor noted that on [DATE], R46's care plan was updated to include the right above the knee amputation.
Based on observation, record review and interview, the facility did not ensure 6 of 18 (R35, R14, R71, R46, R56 and R75) resident's care plans reviewed were updated to reflect the current needs of the residents.
R35's care plan for dialysis was not updated to reflect a different dialysis port. R35's care plan is not specific as to what type of behaviors for depression are being monitored.
R14's care plan was not updated to reflect R14's use of Melatonin for sleep or interventions that may assist R14 with sleep. R14's care plan does not address R14's periodic refusals to wear heel boots.
R71's fall care plan was not updated after falls.
R46's care plan was not updated to reflect R46's bilateral knee amputation.
R56's care plan was not updated to address his elopement.
R75's care plan was not updated to reflect current code status.
Findings include:
1. R35's medical record was reviewed on [DATE]. On [DATE] at 10:19 am, Surveyor spoke with R35 who stated on [DATE] she fell here at the facility after coming back from dialysis. R35 stated she fell and broke her left arm. R35 reported since breaking her arm, she is not allowed to her walker (with seat) unless with therapist in attendance. R35 stated she leaves for dialysis at 4:15 am, chair time from 5-8:30 am and is back by 9:30 am however they are using the catheter site (pointing to her chest area) which is quicker so she is starting to get home by 9:00 am.
Surveyor reviewed R35's care plan for dialysis which documents:
Problem: I have renal failure and require hemodialysis. Initiated on [DATE]
Approaches initiated [DATE] include in part:
I receive dialysis . M-W-F. My son picks me up at 4:15 am .
My port/graft/fistuala sight is left UE (upper extremity).
Surveyor noted R35's care plan was not updated to reflect R35's hemodialysis catheter site is now located in her upper chest area as she is wearing a sling on her broken arm and cannot be used as a dialysis port at this time.
On [DATE], Surveyor discussed with Assistant Director of Nursing (ADON) H R35's dialysis care plan has not been updated since R35's dialysis port has been changed.
On [DATE], ADON H provided Surveyor with a revised dialysis care plan indicating to Monitor hemodialysis site to [NAME] chest. Monitor warmth, redness, edema, drainage, bleeding and to report any abnormal findings to MD. created on [DATE].
R35's [DATE] Medication Administration Record (MAR) indicates R35 receives Cymbalta Capsule 20 mg daily for depression, and Duloxetine HCI 20 mg daily related to depression.
R35's care plan includes a problem of:
I use psychoactive medications r/t Bipolar, Anxiety, Depression, visual hallucination at times. initiated [DATE]
Goal: I will reduce the use of psychoactive medication through the review date.
Approaches dated [DATE] include in part:
Nursing to do Aims at times and intervals and PRN
Psych Consult
Referral to psych services for med management
On [DATE] 10:58 AM Surveyor interviewed RN-F as to what depressive behaviors the facility is monitoring R35 for. RN F stated R35 tends to to spend time alone in room and that R35 came in with this medication.
R35's care plan is not specific in regards as to what depressive behaviors R35 should be monitored for.
2. Surveyor reviewed R14's medical record on [DATE].
According to the July and [DATE] Medication Administration Record (MAR), R14 has physician's orders dated [DATE] for Melatonin Capsule 3 MG give 1 capsule by mouth at bedtime for sleep with 5mg for a total of 8 mg. R14 has been receiving the Melatonin capsules at HS daily.
R14's care plan does not address R14's use of Melatonin for sleep or interventions that may assist R14 with sleep.
On [DATE] at 2:45 pm, Surveyor shared with Administrator A and Corporate Consultant M, that R14's care plan does not address R14's issue involving sleep.
Surveyor also noted R14 has a care plans pertaining to R14 having pressure injuries.
One care plan documents, I having a pressure ulcer to his right proximal lateral foot-unstagable deep tissue injury wound now a stage 3. Approaches dated [DATE] include in part;
Assess/record/monitor wound healing (FREQ). Measure length, width and depth . heel boots at all times, seen by [NAME] wound.
Another care plan documents,I have a pressure ulcer/stasis ulcer unstagable wound to right medial heel, per wound MD right medial heel is now unstagable necrosis, right medial heel now a stage 4 per wound MD.
Approaches in part dated [DATE] include:
Heel boots at all times, pressure relieving cushion to chair, pressure relieving mattress to bed .etc.
On [DATE] 07:31 AM Surveyor interviewed wound nurse J who stated a lot of times [R14] does not want to wear heel boots with education provided. He has always had heel boots on even prior to the development of the pressure injury and at one time he preferred to stay in bed all the time. Over the time he has had this pressure injury it has improved and then deteriorated. Presently it is improving.
R14's care plan does not address R14 not always wanting to wear heel boots nor interventions to be implemented when R14 chooses not to do so.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and resident and staff interviews, 4 (R26, R66, R75 and R71) did not receive required assist...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and resident and staff interviews, 4 (R26, R66, R75 and R71) did not receive required assistance with Activities of Daily Living.
* R26, R66 and R75 did not receive assistance with bathing in accordance with facility protocol.
*On 8/7/22, R71 was noted with severe incontinence which had soaked their clothing, bedlinens and mattress.
Findings include:
1. R26 was admitted to the facility on [DATE] with diagnoses of vascular dementia with behavioral disturbance, cerebral vascular accident and hemiplegia to left upper and lower extremities. R26's Quarterly MDS (Minimum Data Set) assessment dated [DATE] indicates that R26 requires total assistance of 2 staff with showers/bathing. Per R26's medical record, R26 is to receive showers every Monday and Thursday.
On 8/7/22, Surveyor observed R26. R26's hair appeared matted to the back of their scalp and was noted with very dry, flaky skin to their extremities.
Surveyor reviewed R26's shower documentation for the previous 30 days. Facility's documentation indicated that R26 received Bed baths on 7/11/22, 7/14/22, 7/25/22, 7/28/22, 8/4/22 and 8/8/22. Surveyor could not identify that R26 had received a shower in the last 30 days.
On 8/10/22 at 1:30 PM, Surveyor conducted interview with Clinical Care Manager-K. Surveyor asked how often a resident should receive a shower or bath. Clinical Care Manager-K told Surveyor that residents should receive baths or showers at least once a week but many receive twice weekly baths/showers.
On 8/10/22 at 3:20 PM, Surveyor conducted interview with ADON (Assistant Director of Nursing)-H. Surveyor asked ADON-H how often residents should receive a bath or shower. ADON-H responded that residents should receive baths or showers at least once a week.
On 8/10/22 at 4:00 PM, Surveyor shared concerns with NHA (Nursing Home Administrator)-A that R26 has not been receiving twice weekly showers but only bed baths in the last month. The facility did not provide any additional information to Surveyor at this time.
2. R66 was admitted to the facility on [DATE] with paraplegia and neurogenic bladder. R66s Quarterly MDS assessment dated [DATE] indicates that R66 requires extensive assistance by 1 staff with showers/bathing. Per R66's medical record, R66 is to receive showers weekly.
On 8/7/22 at 9:52 AM, Surveyor conducted an interview with R66. R66 shared with Surveyor that they have not had their hair washed in a month and that it is very discouraging to not get help with bathing when needed. R66's hair appears long, greasy and unkempt.
Surveyor reviewed R66's shower documentation for the previous 30 days. Facility's documentation indicated that R66 refused showers/bathing on 7/13/22 and 8/3/22. Surveyor could not identify further offerings by staff to assist R66 with showers/bathing.
On 8/10/22 at 1:30 PM, Surveyor conducted interview with Clinical Care Manager-K. Surveyor asked how often a resident should receive a shower or bath. Clinical Care Manager-K told Surveyor that residents should receive baths or showers at least once a week but many receive twice weekly baths/showers.
On 8/10/22 at 3:20 PM, Surveyor conducted interview with ADON (Assistant Director of Nursing)-H. Surveyor asked ADON-H how often residents should receive a bath or shower. ADON-H responded that residents should receive baths or showers at least once a week.
On 8/10/22 at 4:00 PM, Surveyor shared concerns with NHA (Nursing Home Administrator)-A that R66 has not been receiving weekly showers. The facility did not provide any additional information to Surveyor at this time.
3. R75 was admitted to the facility 9/21/20 with diagnoses of juvenile arthritis, bilateral hand contractures and dementia. R75's Significant change MDS dated [DATE] indicates that R75 requires total assistance of 1 staff with bathing/showers.
Surveyor made observations of R75 on 8/7/22. R75 remained in bed wearing a hospital gown and brief throughout the day. Surveyor noted R75's hair as unkempt and greasy.
Surveyor reviewed R75's shower documentation for the previous 30 days. Facility's documentation indicated that R75 received bed baths on 7/22/22 and 8/2/22. Surveyor could not identify further offerings by staff to assist R75 with showers/bathing.
On 8/10/22 at 1:30 PM, Surveyor conducted interview with Clinical Care Manager-K. Surveyor asked how often a resident should receive a shower or bath. Clinical Care Manager-K told Surveyor that residents should receive baths or showers at least once a week but many receive twice weekly baths/showers.
On 8/10/22 at 3:20 PM, Surveyor conducted interview with ADON (Assistant Director of Nursing)-H. Surveyor asked ADON-H how often residents should receive a bath or shower. ADON-H responded that residents should receive baths or showers at least once a week.
On 8/10/22 at 4:00 PM, Surveyor shared concerns with NHA (Nursing Home Administrator)-A that R75 has not been receiving weekly showers. The facility did not provide any additional information to Surveyor at this time.
4. R71's diagnoses includes dementia with behavioral disturbances, anxiety disorder and depressive disorder.
The ADL (activities daily living) Self Care Performance Deficit care plan initiated & revised 3/1/22 includes approaches of TOILETING SCHEDULE: Upon waking, before meals and at bed time. Initiated & revised 3/1/22 and TOILETING SCHEDULE: Ask me routinely and PRN (as needed) if I need to use the restroom to prevent soiling myself. Assist me with incontinence care PRN. Initiated & revised 3/1/22.
The quarterly MDS (Minimum Data Set) with an assessment reference date of 7/16/22 documents a BIMS (brief interview mental status) score of 7 which indicates severe impairment. R71 requires extensive assistance with one person physical assist for bed mobility, transfer, and toilet use. R71 is coded as being occasionally incontinent of bowel and bladder.
On 8/7/22 at 9:28 a.m. Surveyor observed R71 in bed on her left side. R71 was wearing a gown with an incontinence product. Surveyor observed the sheet under R71 is saturated with a large urine stain. Surveyor who was wearing a N95 mask could smell a strong odor of urine.
On 8/7/22 at 9:53 a.m. Surveyor observed CNA (Certified Nursing Assistant)-Q and CCM (Clinical Care Manager)-K enter R71's room. CCM-K asked R71 if she was having any pain and if R71 wants medication for pain. R71 replied yes. CCM-K then informed R71 CNA-Q is going to wash her as she needs to be washed, is kind of messy and needs to be cleaned up. CNA-Q and CCM-K then left R71's room.
On 8/7/22 at 9:59 a.m. Surveyor observed R71 continues to be on the left side. There continues to be a strong urine smell and Surveyor observed there continues to be a large area of urine under R71.
On 8/7/22 at 10:00 a.m. Surveyor observed CNA-Q enter R71's room with towels, stated she needs a table and left R71's room. GPN (Graduate Practical Nurse)-E entered R71's room, raised the height of R71's bed up and informed R71 she has something for her pain & nausea, and administered medication to R71.
At 10:03 a.m., CNA-Q was back in R71's room and GPN-E informed CNA-Q let me get some gloves and I'll help you. GPN-E then washed her hands and placed gloves on. Surveyor asked CNA-Q what time she starts working. CNA-Q informed Surveyor she started at 6:30 a.m. CNA-Q with gloves on moved R71's bed away from the wall, removed pillows from under R71's head and removed the fitted sheet from the head & foot of the mattress. CNA-Q informed R71 she was going to wash her face and then washed R71's face. CNA-Q informed R71 she was going to remove her gown because the gown is wet and dirty, removed R71's gown and unfastened the incontinence product. Surveyor observed the incontinence product is saturated with urine. CNA-Q informed GPN-E you do the top, I'll do the bottom. CNA-Q washed R71's frontal perineal area from front to back while GPN-E washed R71's upper body. After washing R71's frontal perineal area, CNA-Q removed her gloves, cleansed her hands, and placed gloves on. GPN-E informed R71 she was going to turn her towards her, a clean gown was placed on R71 and R71 was positioned on the left side. Surveyor again observe a large yellow stain of urine under R71 on the sheet. GPN-E removed R71's incontinence product which was saturated with urine, and CNA-Q washed R71's buttocks.
At 10:12 a.m. Surveyor asked CNA-Q if this is the first time she provided cares for R71 today. CNA-Q replied yes. CNA-Q removed her gloves, cleansed her hands, and placed gloves on. CNA-Q then placed a fitted sheet on R71's bed, a draw sheet and product was placed under R71 and the incontinence product was fastened.
At 10:17 a.m. CNA-Q removed her gloves, cleansed her hands, raised the head of the bed, the bed was placed against the wall, lowered down and mat placed floor on the left side. CNA-Q placed a pillow under R71's head & calves, placed the call light in reach and left R71's room.
On 8/7/22 at 2:37 p.m. Surveyor reviewed the bowel & bladder entries under the task tab. Surveyor noted R71 is checked yes for being incontinent at 10:21 a.m. & 10:29 p.m. There is no documentation for the night tour on 8/7/22.
On 8/8/22 at 7:50 a.m. Surveyor observed CMA (Certified Medication Aide)-X and GPN-E with gloves on place a gait belt around R71 who was sitting on the edge of the bed and transfer R71 into a Broda chair & wheel R71 into the bathroom. GPN-E stated to R71 need you to grab the bar to go to the toilet, CMA-X & GPN-E stood R71 up, GPN-E pulled down R71's incontinence product and R71 was seated on the toilet. At 7:52 a.m. Surveyor checked R71's bed and observed the sheets are not soaked or even wet as they were on the previous day.
On 8/8/22 at 7:55 a.m. Surveyor informed GPN-E Surveyor had noted R71's linen on the bed is not wet today but yesterday it was soaked with a strong urine odor. GPN-E informed Surveyor that was shocking to her. GPN-E explained R71 always goes to the bathroom, she's continent and that was different to her also. GPN-E explained every morning she asks R71 if she wants to go to the bathroom and have breakfast. GPN-E informed Surveyor yesterday was the first time she had seen R71 like that. Surveyor asked GPN-E when CNA's check & change or toilet Residents should they document this. GPN-E replied yes in point click care.
On 8/9/22 at 2:14 p.m. Surveyor asked CCM (Clinical Care Manager)-K regarding R71's continence cares. CCM-K informed Surveyor staff takes R71 into the bathroom for the toilet. Surveyor inquired about the night shift. CCM-K informed Surveyor it should be the same thing. Surveyor asked how often staff should be checking R71. CCM-K informed Surveyor she believes when R71 is awake at night and in the morning CCM-K explained R71 is one of the first ones staff gets up if she is awake. Surveyor inquired what should staff do if R71's incontinence product & bed is saturated with urine and there is a strong urine odor. CCM-K informed Surveyor she would expect R71 to be cleaned up, change her brief and linen. Surveyor asked CCM-K if staff provides continence cares should this be documented. CCM-K informed Surveyor this should be documented in PCC. Surveyor informed CCM-K of Surveyor's observation on 8/7/22 and not finding any documentation for the night shift continence care was provided to R71. CCM-K informed Surveyor her assumption is night shift did not provide any cares.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility did not ensure the drug regimen of each resident was reviewed at least once a...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility did not ensure the drug regimen of each resident was reviewed at least once a month by a licensed pharmacist and that irregularities identified by the the pharmacist were reviewed, and action was taken to address them, for 4 (R10, R71, R14 & R31 ) of 4 Residents reviewed who required drug regimen reviews.
The pharmacist consultant did not conduct at least monthly pharmacy reviews for R10, R71, R14 and R31.
Findings include:
1. R10 was admitted to the facility on [DATE].
On 8/9/22 Surveyor reviewed R10's medication which included Fluoxetine HCl 20 mg (milligrams), Memantine HCl 10 mg, Depakote Delayed Release Sprinkles 125 mg, Mirtazapine 7.5 mg, Tylenol Extra Strength Tablet 1000 MG, Metoprolol Succinate ER (extended release) 50 mg, Amlodipine Besylate 5 mg, Losartan Potassium 100 mg, Aspirin EC (enteric coated) Tablet Delayed Release 81 mg, Potassium Chloride ER 20 meq (millequivalent), & Furosemide 20 mg.
Surveyor reviewed R10's medical record and was unable to locate a drug regimen by a licensed pharmacist.
On 8/9/22 at 4:10 p.m. during end of the day meeting with Administrator-A and Corporate Consultant-M Surveyor inquired where monthly pharmacy reviews would be located. Administrator-A indicated they would look into this and get back to Surveyors.
On 8/10/22 at 1:01 p.m. Surveyor reviewed a list of Residents who had a July 2022 drug regimen conducted by a licensed pharmacist. Surveyor noted R10's name listed on the July list with no recommendations.
On 8/10/22 at 3:17 p.m. during the end of the day meeting with Administrator-A and Corporate Consultant-M Surveyor informed Facility staff Surveyors received the July 2022 pharmacist drug regimen reviews but still needs prior pharmacy reviews.
On 8/11/22 at 9:25 a.m. Surveyor was informed by another team member the Facility does not have any other pharmacy reviews and the Facility will provide them if they are able to locate them.
Surveyor was only provided with July 2022 pharmacy review for R10.
2. R71 was admitted to the facility on [DATE].
On 8/9/22 Surveyor reviewed R71's medication which included Seroquel 50 mg (milligrams), Morphine Sulfate 10 mg, Lorazepam 0.5 mg, Cymbalta 40 mg, Mirtazapine 7.5 mg, Celebrex 100 mg, Acetaminophen-Codeine 300-30 mg, Pantoprazole 40 mg, Tylenol 650 mg, Timpotic Solution 0.25%, Senna Plus 8.6-50 mg, Latanoprost Solution 0.005%, and Clonazepam 1 mg.
During R71's record review Surveyor noted a pharmacy medication review note dated 4/30/22. Surveyor was unable to locate any other pharmacy medication review for R71.
On 8/9/22 at 4:10 p.m. during end of the day meeting with Administrator-A and Corporate Consultant-M Surveyor inquired where monthly pharmacy reviews would be located. Administrator-A indicated they would look into this and get back to Surveyors.
On 8/10/22 at 1:01 p.m. Surveyor reviewed a list of Residents who had a July 2022 drug regimen conducted by a licensed pharmacist. Surveyor noted R71's name on this July list with no recommendations.
On 8/10/22 at 3:17 p.m. during the end of the day meeting with Administrator-A and Corporate Consultant-M Surveyor informed Facility staff Surveyors received the July 2022 pharmacist drug regimen reviews but still needs prior pharmacy reviews.
On 8/11/22 at 9:25 a.m. Surveyor was informed by another team member the Facility does not have any other pharmacy reviews and the Facility will provide them if they are able to locate them.
There is no evidence a pharmacy review were conducted for March, May, & June 2022.
4. R31 was admitted to the facility on [DATE] with diagnoses of depression and insomnia. The quarterly MDS (Minimum Data Set) assessment dated [DATE] indicates R31 is cognitively impaired needs extensive assistance with bed mobility, dressing, hygiene and transfers.
R31 was receiving trazadone 100 mg at night for insomnia, duloxetine 30 mg daily for depression and Methadone 2.5 mg every 8 hours for pain.
On 8/10/22 Surveyor reviewed R31 medical record observed a pharmacy medication review for July 2022 with no irregularities. Surveyor was unable to find previous months of pharmacy medication review.
On 8/10/22 at 2:30 p.m. during the daily exit meeting with Nursing Home Administrator A and Corporate Consultant M, Surveyor asked to see previous months of pharmacy medication review.
On 8/11/22 at 9:25 AM, Assistant Director of Nursing H informed Surveyor that they are unable to locate any other pharmacy medication reviews.
3. On 8/9/22 during the end of the day meeting with Administrator A and Corporate Consultant M, Surveyors requested to review the monthly pharmacist drug regimen reviews.
Administrator A informed Surveyors that the facility started with a new pharmacy in early June 2022. Corporate Consultant M reported the pharmacy reviews are not in the paper chart and that they may be in the portal. Administrator A and Corporate Consultant M indicated they would look for the pharmacist's monthly drug regimen reviews.
On 8/14/22, Surveyor was provided with the only monthly drug regimen the facility could find for R14 dated 7/9/22, even though R14 was admitted into the facility on [DATE].
Although, the physician/prescriber did not document a response to the pharmacist's recommendations on the Note to Attending Physician/Prescriber form Surveyor did locate a Nurse Practitioner's note dated 7/27/22 documenting GERD stable continue Pantoprazole as ordered.
The facility was not able to provide evidence of any previous monthly drug regimen being reviewed for R14 prior to this 7/9/2022 review.
On 8/11/22 at 9:20 am, Assistant Director of Nursing (ADON) H stated she was aware there were no other pharmacy reviews that could be located at this time. Surveyor informed ADON to send to Surveyor and additional pharmacy reviews if found after Surveyors left the facility.
As of 8/26/22, no additional pharmacy reviews were received.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
3. On 8/7/22 at 2:20 p.m. Surveyor observed GPN (Graduate Practical Nurse)-E wheeling R71. Surveyor observed GPN-E's face mask was not covering her nose.
4. On 8/8/22 from 8:16 a.m. to 8:40 a.m. Surve...
Read full inspector narrative →
3. On 8/7/22 at 2:20 p.m. Surveyor observed GPN (Graduate Practical Nurse)-E wheeling R71. Surveyor observed GPN-E's face mask was not covering her nose.
4. On 8/8/22 from 8:16 a.m. to 8:40 a.m. Surveyor observed morning cares for R19 with CMA (Certified Medication Aide)- X. During this observation CMA-X was not wearing eye protection.
On 8/8/22 at 8:51 a.m. Surveyor observed CMA-X walking down the hall with a breakfast tray. CMA-X was not wearing any eye protection.
On 8/8/22 at 9:01 a.m. Surveyor observed CMA-X exiting R10's room stating enjoy your breakfast. CMA-X was not wearing any eye protection.
5. On 8/8/22 at 8:50 a.m. Surveyor observed CNA-T enter R46's room with a breakfast tray. CNA-T was not wearing any eye protection.
6. On 8/8/22 at 8:54 a.m. Surveyor observed R71 sitting in a Broda chair in the dining room with a breakfast tray in front of R71. Surveyor observed the hospice aide next to R71 was not wearing any eye protection.
Based on interview and record review the Facility did not have an effective infection prevention and control program to prevent and control the spread of infections such as COVID-19.
The Facility did not ensure their outbreak policy was implemented which had possibility to affect all 84 residents.
* On 12/23/21 the facility had one staff who was symptomatic and tested positive for Covid 19. The facility has no evidence measures were put into place to prevent and contain the spread of the infection. The facilitiy had a Covid-19 outbreak from 12/23/22 through 1/21/22 affecting 26 staff members and 30 residents. There was no documentation regarding the implementation of their outbreak policy for this Covid 19 outbreak. There is no outbreak investigation into this outbreak.
* On 8/1/22 the facility Outbreak investigation Summary form indicated 2 staff who tested positive for Covid 19. The summary indicates two staff tested positive for Covid 19 on 7/19/22.
There is no evidence all staff were tested during this outbreak.
An infection line list for staff was not completed. The Covid 19 testing form indicates residents were not tested for Covid 19 until 7/21/22. The next testing perform for residents was on 7/28/22 and 7/29/22. It also indicates no residents tested positive for Covid 19. No other information was in the outbreak summary. It indicates the health department was not notified.
* Graduate Practical Nurse (GPN) E was not wearing her face mask so that it was covering her nose, Certified Medication Aide (CMS) X , Certified Nursing Assistant (CNA) T and Hospice Aide were not wearing eye protection.
Findings include:
The facility infection surveillance policy dated 11/2017 with revised date of 5/31/22 indicates:
1. The (designated infection preventionist) serves as the leader in surveillance activities, maintains documentation of incidents, findings, and any corrective actions made by the facility and reports surveillance findings to the facility's Quality Assessment and Assurance Committee, and public health authorities when required.
7. All resident infections will be tracked. Separate, site specific measures may be tracked as prioritized from the infection control risk assessment. Outbreaks will be investigated.
8. Employee, volunteer, and contract employee infections will be tracked, as appropriate, such as influenza or gastrointestinal infection outbreaks.
9. Data to be used in the surveillance activities may include, but are not limited to:
a. 24 hour shift reports
b. lab reports
c. Antibiograms obtained from lab
d. Antibiotics use reports from pharmacy
e. Skills validations for hand hygiene, PPE, and/or high risk procedures
f. Rounding observation data
g. Resident and employee immunization data
h. Documentation of signs and symptoms in clinical record.
The facility policy regarding Covid 19 antigen testing dated 1/20/22 indicates:
Interpretation of Antigen results: .
ii. If the resident or staff is the first positive test for Covid 19 within the facility, an outbreak response should be initiated immediately.
1. On 8/9/22 Surveyor reviewed the facility infection control binder. Surveyor noticed an outbreak line list for staff and residents with infections starting on 12/23/21. The line list and testing list indicate the infection was Covid 19. The line list indicated on 12/23/21 Staff Z had a sore throat and tested positive for Covid 19. R436 had respiratory symptoms on 12/24/21 and tested positive on 12/24/21. The line list indicates 26 staff tested positive and/or had respiratory symptoms from 12/23/21 through 1/21/22. The resident line list indicates 30 residents tested positive from 5 out of 6 different units. The infections began on 12/24/21 through 1/14/22. There is no documentation regarding the implementation of their outbreak policy for this Covid 19 outbreak. There is no outbreak investigation into this outbreak.
2. Surveyor reviewed the facility outbreak investigation summary dated 8/1/22. The summary indicates RN (registered nurse) W and MDS LPN (minimum data set Licensed Practical Nurse) V tested positive for Covid 19 on 7/19/22. There is no evidence all staff were tested during this outbreak. An infection line list for staff was not completed.
The Covid 19 testing form indicates residents were not tested for Covid 19 until 7/21/22. The next testing perform for residents was on 7/28/22 and 7/29/22.
It indicates the health department was not notified.
DON (Director of Nursing) B, who was the infection preventionist, no longer worked at the facility during the review of the infection line list on 8/9/22. On 8/11/22 at 9:47 a.m. Surveyor interviewed ADON H regarding infection control. ADON (assistant director of nursing) H stated DON B was responsible for the infection control. ADON H stated she is not sure who is responsible for it at this time. Surveyor was unable to interview anyone that would have knowledge or be responsible for infection control.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility did not ensure Covid 19 testing was being consistently performed according to the county positivity rate of infection.
The county positivity rate of ...
Read full inspector narrative →
Based on interview and record review the facility did not ensure Covid 19 testing was being consistently performed according to the county positivity rate of infection.
The county positivity rate of infection is high, which would indicate the facility would need to test all appropriate staff for Covid 19 twice a week and this was not done.
On 8/10/22 Surveyor reviewed the Covid testing of staff and identified the facility was not consistently testing staff. The only evidence of testing of staff for Covid 19 was for 7/21/22.
No other dates were identified for testing.
This deficient practice has the possibility to affect all 84 residents.
Findings include:
The facility policy regarding Employee Covid 19 vaccination exemption with revised date of 6/20/22 indicate:
Compliance guidelines:
.
6. The exempt employee will be masking, social distancing, and participating in periodic testing, in accordance with CDC (Centers for Disease Control and Prevention) updated regulations and county positivity rates.
The facility policy regarding Covid 19 Antigen testing with date of 1/20/22 indicates:
Policy explanation and compliance guidelines:
1. The facility will conduct testing through the use of rapid point of care (POC) diagnostic testing devices as per manufacturer's instructions.
2. Antigen testing will be used in the following circumstances:
a. testing of symptomatic residents and staff;
b. testing of asymptomatic residents and staff in facilities as part of a Covid 19 outbreak response or testing of asymptomatic residents or staff who are known close contacts of persons with Covid 19, and;
c. Testing of asymptomatic staff in facilities without a Covid 19 outbreak as part of expanded screen testing.
Surveyor reviewed the list of staff and their vaccination status. There are nine staff that have religious exemptions for the Covid 19 vaccine.
Surveyor reviewed the documentation the facility had regarding staff testing for Covid 19.
There is evidence of staff testing during the facility Covid 19 outbreak in January 2022. The last date of testing was 1/31/22.
The next time there is any evidence of staff testing was on 7/19/22 when LPN (licensed practical nurse) V and RN (registered nurse) W became symptomatic and tested positive for Covid 19. There is no evidence other staff were tested at that time.
During the survey, DON (Director of Nursing) B who was the infection preventionist, no longer was an employee at the facility.
On 8/10/22 during the daily exit meeting with NHA (Nursing Home Administrator) A, Surveyor explained the concern there is no evidence staff are being consistently tested for Covid 19. Surveyor explained the county positivity rate has been high since May 2022 and before it was in the medium level. NHA A understood the concern and had no additional information.
On 8/11/22 at 9:47a.m. Surveyor interviewed ADON (Assistant Director of Nursing) H. Surveyor asked ADON H who is responsible for infection control and staff testing. ADON H stated there has not been a decision as to who will be taking over those responsibilities.
MINOR
(C)
Minor Issue - procedural, no safety impact
Transfer Notice
(Tag F0623)
Minor procedural issue · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 8/8/22 at 8:31 AM, Surveyor reviewed R75's medical record. Surveyor noted that R75 was hospitalized on [DATE] hospitalizat...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 8/8/22 at 8:31 AM, Surveyor reviewed R75's medical record. Surveyor noted that R75 was hospitalized on [DATE] hospitalization.
On 8/9/22 at 8:42 AM Surveyor requested to review R75's transfer notice for R75's hospitalization on 7/17/22. NHA-A told Surveyor they were unsure if facility staff is currently providing transfer notices to residents and their representatives and that they would look into this matter.
On 8/9/22 at 1:32 PM, NHA-A told Surveyor that they could not provide a transfer notice for R75's 7/17/22 hospitalization. NHA-A added that the facility had missed the mark on providing transfer notices from the facility.
On 8/11/22 at 4:00 PM, Surveyor shared concern with NHA-A related to R75's representative not being provided a transfer notice for R75's 7/17/22 Hospitalization. No additional information was provided by the facility at this time.
Based on record review and interview, the facility did not provide a transfer/discharge notice to the resident and the resident representative for 2 of 2 residents (R35 and R75) reviewed for facility initiated discharges. This deficient practice has the potential affect all residents who may have a facility initiated transfers to the hospital.
Findings include:
1. R35 was transferred to the hospital on 6/10/22 and was readmitted into the facility on 6/21/22. There was no indication in R35's medical record of R35 and her responsible party of being provided with the transfer/discharge notice which includes appeal rights, for this hospitalization.
On 7/1/22 R35 was transferred to the hospital and was readmitted into the facility on 7/30/22. There was no indication in R35's medical record of R35 and her responsible party of being provided with the transfer/discharge notice which includes appeal rights, for this hospitalization.
On 8/08/22 at 8:38 am Administrator A informed Surveyor the facility has not been sending transfer/discharge notices with the resident to the hospital nor sending them to the resident's representative.