Shepherd of the Valley SNF Operations LLC




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Shepherd of the Valley SNF Operations LLC has received a Trust Grade of F, indicating significant concerns about the quality of care provided. They rank #33 out of 33 nursing facilities in Wyoming, placing them in the bottom tier of all facilities in the state and #3 of 3 in Natrona County, suggesting there are no better local options available. Although the facility's trend is improving, with issues decreasing from 12 in 2024 to 4 in 2025, the overall inspection results remain troubling, with 37 issues found, including serious incidents that led to actual harm for some residents. Staffing is a relative strength, earning a 4/5 star rating, with a turnover rate of 46%, lower than the state average, but the facility has faced fines totaling $93,771, which is concerning as it is higher than 75% of similar facilities in Wyoming. Specific incidents include a failure to protect a resident from physical abuse by another resident, and not notifying physicians of significant changes in the condition of two residents, resulting in serious health complications for them. While staffing levels are good, the facility's overall performance raises red flags that families should carefully consider.
- Trust Score
- F
- In Wyoming
- #33/33
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 46% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $93,771 in fines. Higher than 56% of Wyoming facilities. Some compliance issues.
- Skilled Nurses ✓ Good
- Each resident gets 49 minutes of Registered Nurse (RN) attention daily — more than average for Wyoming. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 37 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, fire safety.
The Bad
Below Wyoming average (2.9)
Significant quality concerns identified by CMS
Near Wyoming avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 37 deficiencies on record
May 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, resident representative and staff interview, facility incident review, and performance improveme...
Read full inspector narrative →
Mar 2025
3 deficiencies
3 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Notification of Changes
(Tag F0580)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident representative and staff interview, medical record review, and policy review, the facility failed to notify re...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident representative and staff interview, medical record review, and policy review, the facility failed...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident representative and staff interview, and medical record review, the facility failed to ensure resi...
Read full inspector narrative →
Oct 2024
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident and staff interview, medical record review, and policy and procedure review, the facility failed to ensure res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, and policy review, the facility ensure infection control procedures were implemented for 1 of 2 sample residents (#77) reviewed for enhanced barrier precautions....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on resident and staff interview and medical record review, the facility failed to ensure activities meet the interest/nee...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on resident and staff interviews and medical record review, the facility failed to ensure sufficient staffing to attain or maintain the highest practicable physical, mental, and psychosocial wel...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of the 5-day Medicare MDS assessment dated [DATE] showed resident #120 had a BIMS score of 3 out of 15, which indicate...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, staff interview, and policy review, the facility failed to label and provide the date medications were opened in 2 of 6 medication storage areas (south hall medication cart #1, s...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on resident and staff interview, medical record review, bath schedule log review, and policy and procedure review, the facility failed to ensure medical records were accurately documented for 3 ...
Read full inspector narrative →
Sept 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Based on medical record review, staff interview, review of incident and facility documentation, and policy and procedure review, the facility failed to ensure residents were free from physical abuse b...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on medical record review, staff interview, and review of incident reports, the facility failed to develop an individualized, comprehensive care plan for 1 of 5 sample residents (#2). The finding...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident, resident representative, and staff interview, medical record review, facility policy review, and...
Read full inspector narrative →
Mar 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, family and staff interview, and the resident's family's written timeline, the facility failed to...
Read full inspector narrative →
Feb 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, resident and staff interview, and facility investigation review, the facility failed to protect ...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, the facility failed to develop and implement a comprehensive care plan for 2...
Read full inspector narrative →
Aug 2023
10 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, resident and staff interview, medical record and policy review, the facility failed to ensure residents who self-administered medications were assessed and determined safe to do ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review and staff interview, the facility failed to ensure the care plan was implemented for...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on medical record review, staff interview, and facility policy review, the facility failed to implement interventions to manage diabetes in accordance with physician orders and professional stan...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, medical record review, staff interview, and review of therapy and restorative documentation, the facility failed to provide services to maintain range of motion for 1 of 9 sample...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review and staff interview, the facility failed to provide adaptive equipment to prevent ac...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, medical record review, resident and staff interview, the facility failed to implement the necessary respiratory care for 1 of 8 sample residents (#130) reviewed for oxygen servic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
Based on observation, medical record review, staff interview, and review of menus, the facility failed to ensure the menu was followed during 1 of 2 meal observations. This failure affected resident #...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on observation, medical record review, and staff interview, the facility failed to adequately provide a call system to 2 of 44 sample residents (#13, #20) observed for resident call systems. The...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, staff interview, and review of the 2022 Food Code, the facility failed to ensure hand hygiene/gloving and hair restraint use was done in accordance with accepted standards to min...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, medical record review, staff interview, policy and procedure review, and professional reference review, the facility failed to ensure infection control procedures were followed f...
Read full inspector narrative →
May 2023
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on observation, medical record review and resident and staff interview, the facility failed to ensure staff were trained in the appropriate use of a mechanical lift for 1 of 5 sample residents (...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, the facility failed to ensure a chronic condition was addressed for 1 of 4 r...
Read full inspector narrative →
Aug 2022
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, staff interview, and review of the RAI manual, the facility failed to complete a significant cha...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, the facility failed to ensure care plans were updated and revised for 1 of 3...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
2. Review of the 7/11/22 admission MDS assessment showed resident #79 was cognitively intact (BIMS score of 15) and required extensive assistance with locomotion. Further review showed s/he had Occupa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0839
(Tag F0839)
Could have caused harm · This affected 1 resident
Based on employee file review, staff interview, and review of the Nursys QuickConfirm License Verification Report, the facility failed to ensure professional staff had credentials to practice in accor...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, and policy review the facility failed to ensure infection control procedures were followed during 1 random observation of wound care (#89). The finding were:
1. ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the CMS Resident Assessment Instrument (RAI) manual version 3.0, medical record review, and staff interview, ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident and staff interview, and medical record review, the facility failed to develop and/or implement a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, and policy and procedure review the facility failed to ensure medications were labeled wi...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, Special Focus Facility, 7 harm violation(s), $93,771 in fines. Review inspection reports carefully.
- • 37 deficiencies on record, including 7 serious (caused harm) violations. Ask about corrective actions taken.
- • $93,771 in fines. Extremely high, among the most fined facilities in Wyoming. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Shepherd Of The Valley Snf Operations Llc's CMS Rating?
CMS assigns Shepherd of the Valley SNF Operations LLC an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Wyoming, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Shepherd Of The Valley Snf Operations Llc Staffed?
CMS rates Shepherd of the Valley SNF Operations LLC's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 46%, compared to the Wyoming average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Shepherd Of The Valley Snf Operations Llc?
State health inspectors documented 37 deficiencies at Shepherd of the Valley SNF Operations LLC during 2022 to 2025. These included: 7 that caused actual resident harm and 30 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Shepherd Of The Valley Snf Operations Llc?
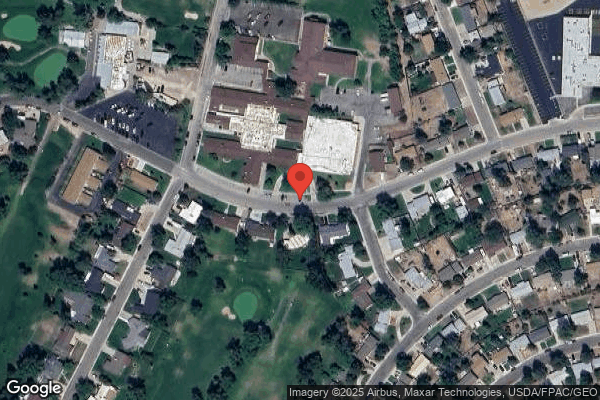
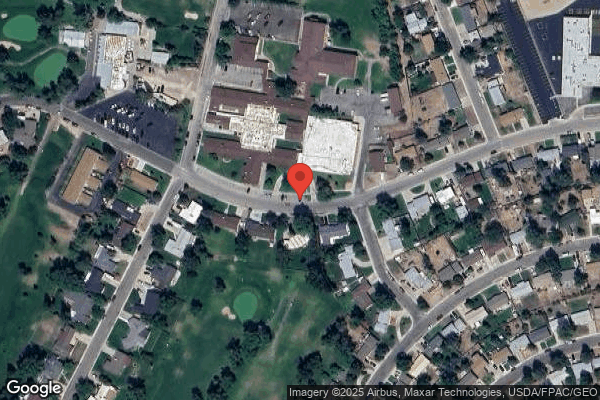
Shepherd of the Valley SNF Operations LLC is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by EMPRES OPERATED BY EVERGREEN, a chain that manages multiple nursing homes. With 192 certified beds and approximately 156 residents (about 81% occupancy), it is a mid-sized facility located in Casper, Wyoming.
How Does Shepherd Of The Valley Snf Operations Llc Compare to Other Wyoming Nursing Homes?
Compared to the 100 nursing homes in Wyoming, Shepherd of the Valley SNF Operations LLC's overall rating (1 stars) is below the state average of 2.9, staff turnover (46%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Shepherd Of The Valley Snf Operations Llc?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the substantiated abuse finding on record.
Is Shepherd Of The Valley Snf Operations Llc Safe?
Based on CMS inspection data, Shepherd of the Valley SNF Operations LLC has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility is currently on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes nationwide). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Wyoming. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Shepherd Of The Valley Snf Operations Llc Stick Around?
Shepherd of the Valley SNF Operations LLC has a staff turnover rate of 46%, which is about average for Wyoming nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Shepherd Of The Valley Snf Operations Llc Ever Fined?
Shepherd of the Valley SNF Operations LLC has been fined $93,771 across 5 penalty actions. This is above the Wyoming average of $34,017. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Shepherd Of The Valley Snf Operations Llc on Any Federal Watch List?
Shepherd of the Valley SNF Operations LLC is currently an SFF Candidate, meaning CMS has identified it as potentially qualifying for the Special Focus Facility watch list. SFF Candidates have a history of serious deficiencies but haven't yet reached the threshold for full SFF designation. The facility is being monitored more closely — if problems continue, it may be added to the official watch list. Families should ask what the facility is doing to address the issues that led to this status.