BAY VIEW REHABILITATION HOSPITAL, LLC




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Bay View Rehabilitation Hospital, LLC has a Trust Grade of D, indicating below-average performance with some significant concerns. They rank #529 out of 1155 facilities in California, placing them in the top half, but at #48 of 69 in Alameda County, they have limited competition. The facility is improving, as the number of issues reported dropped from 11 in 2024 to just 1 in 2025, which is a positive sign. Staffing is a weakness, with a 2/5 star rating and an average turnover of 0%, suggesting stability but also possible staffing challenges. However, there are serious concerns, such as a critical incident where a staff member physically abused a resident and the facility's failure to promptly investigate. Other issues include improper food handling, which could lead to contamination and health risks for residents. Overall, while there are some strengths in terms of rankings and trends, the facility's serious deficiencies cannot be overlooked.
- Trust Score
- D
- In California
- #529/1155
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ✓ Good
- $46,726 in fines. Lower than most California facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 20 minutes of Registered Nurse (RN) attention daily — below average for California. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 33 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Near California average (3.1)
Meets federal standards, typical of most facilities
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 33 deficiencies on record
Jan 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the resident and/or responsible party (RP or le...
Read full inspector narrative →
Dec 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based observation, interview, and record review, the facility failed to provide a comfortable and safe room temperature for thre...
Read full inspector narrative →
Oct 2024
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
Based on interview, record review, and document review, the facility failed to ensure a significant change in status assessment (SCSA) Minimum Data Set (MDS) assessment was completed for one (Resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. An admission Record revealed the facility admitted Resident 13 on 06/17/2023. According to the admission Record, the resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on interview, record review, and facility policy review, the facility failed to ensure a comprehensive care plan was developed for one (Resident 148) of two sampled residents reviewed for mood/b...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected multiple residents
3. An admission Record indicated the facility admitted Resident 96 on 08/11/2021. According to the admission Record, the resident had a medical history that included a diagnosis of schizophrenia.
An a...
Read full inspector narrative →
Sept 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to prevent medical device related pressure injury (injury to the skin and underlying tissues that results from prolonged pressure on the skin)...
Read full inspector narrative →
Jul 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow its policy and procedure to immediately report alleged abuse allegations to the facility Administrator and to California Department ...
Read full inspector narrative →
May 2024
2 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Investigate Abuse
(Tag F0610)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to protect residents in the facility from physical abuse ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to keep one of three residents (Resident 1) free from ph...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a safe and functional environment for resident...
Read full inspector narrative →
Mar 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to follow its policy and procedure to immediately report an alleged abuse allegation to the California Department of Public Health (CDPH) with...
Read full inspector narrative →
Apr 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a licensed nurse (LVN) monitored one of three residents (Resident 1) to ensure all the resident ' s prescribed medicat...
Read full inspector narrative →
Jun 2021
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the privacy and dignity for two of five sample...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, facility failed to ensure one of 28 sampled residents (Resident 594) received nail care which resulted in Resident 594's nails on both hands being l...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based an interview and record review, the facility failed to provide restorative nursing services (nursing care used to improve or maintain physical function) to one of nine residents (Resident 1).
Th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide care for two (Resident 109 and 695) of two Residents that r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to follow doctor's orders for two (Resident 88 and Resident 91) of fiv...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to provide food that accommodated the preferences of three unsampled residents: Resident 95, Resident 127 and Resident seven who ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. During an observation on 6/21/21, at 12:56 p.m., all residents in facility were on contact and droplet precautions (measures ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure the walk-in refrigerator/freezer was maintained when there was grime, and ice build-up on the unit cooler (equipment wi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
The facility failed to ensure the competency of the Dietary Manager (DM) when:
1. the DM did not ensure the cleanliness and maintenence of equipment in the kitchen (Cross-reference F812 and F908); and...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected most or all residents
Based on observation, interview, and facility document review, the facility failed to ensure the competency of Food and Nutrition Services staff when:
1. Dietary [NAME] 1 (DC1) did not correctly date ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to store, prepare, and serve food safely when:
1. A dirty...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected most or all residents
Based on observation, interview, and facility document review, the facility failed to ensure nursing staff were knowledgeable about safely storing food for residents brought in by family and visitors....
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation, interview, and facility document review, the facility failed to store food-related garbage in a dumpster with a tight-fitting lid. This failure had the potential to attract pest ...
Read full inspector narrative →
Mar 2019
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to obtain a doctors order or determine if one of 38 sampled residents (Resident 160) was able to self-administer medications, when...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure three of 38 sampled residents (Residents 117, 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure residents had bedside curtains which assured full visual privacy in multiple occupancy rooms.
This deficient practice resulted in no v...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, for one (Resident 265) of one sampled resident, the facility failed to ensure the oxygen humidifier (a device to that helps the nose from drying out ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, expired medication and equipment was found in a medication room and expired a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record reviews, the staff failed to follow infection control practice when contrary to the facility policy, the treatment nurse brought back unused disposable tre...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s), $46,726 in fines. Review inspection reports carefully.
- • 33 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $46,726 in fines. Higher than 94% of California facilities, suggesting repeated compliance issues.
- • Grade D (43/100). Below average facility with significant concerns.
About This Facility
What is Bay View Rehabilitation Hospital, Llc's CMS Rating?
CMS assigns BAY VIEW REHABILITATION HOSPITAL, LLC an overall rating of 3 out of 5 stars, which is considered average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Bay View Rehabilitation Hospital, Llc Staffed?
CMS rates BAY VIEW REHABILITATION HOSPITAL, LLC's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes.
What Have Inspectors Found at Bay View Rehabilitation Hospital, Llc?
State health inspectors documented 33 deficiencies at BAY VIEW REHABILITATION HOSPITAL, LLC during 2019 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 32 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Bay View Rehabilitation Hospital, Llc?
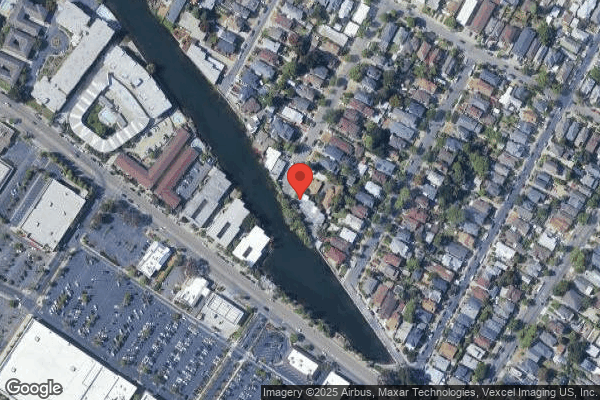
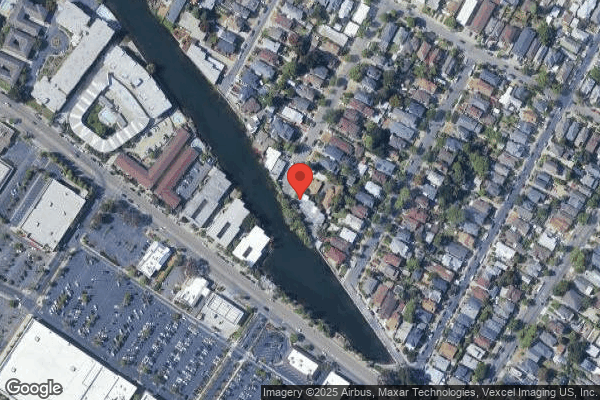
BAY VIEW REHABILITATION HOSPITAL, LLC is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by DAVID & FRANK JOHNSON, a chain that manages multiple nursing homes. With 180 certified beds and approximately 161 residents (about 89% occupancy), it is a mid-sized facility located in ALAMEDA, California.
How Does Bay View Rehabilitation Hospital, Llc Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, BAY VIEW REHABILITATION HOSPITAL, LLC's overall rating (3 stars) is below the state average of 3.1 and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Bay View Rehabilitation Hospital, Llc?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Bay View Rehabilitation Hospital, Llc Safe?
Based on CMS inspection data, BAY VIEW REHABILITATION HOSPITAL, LLC has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in California. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Bay View Rehabilitation Hospital, Llc Stick Around?
BAY VIEW REHABILITATION HOSPITAL, LLC has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Bay View Rehabilitation Hospital, Llc Ever Fined?
BAY VIEW REHABILITATION HOSPITAL, LLC has been fined $46,726 across 1 penalty action. The California average is $33,546. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Bay View Rehabilitation Hospital, Llc on Any Federal Watch List?
BAY VIEW REHABILITATION HOSPITAL, LLC is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.