CROWN BAY NURSING AND REHABILITATION CENTER
Over 2 years since last inspection. Current conditions may differ from available data.
Crown Bay Nursing and Rehabilitation Center has received a Trust Grade of D, indicating below-average performance with some notable concerns. It ranks #779 out of 1,155 facilities in California, placing it in the bottom half overall and #62 out of 69 in Alameda County, which means there are very few local options that perform better. The facility is trending towards improvement, as the number of reported issues decreased from 8 in 2024 to 7 in 2025. Staffing is rated average with a turnover rate of 39%, which is similar to the state average, suggesting stability among staff. Although the facility has not incurred any fines, two serious incidents were reported: one resident fell and fractured their arm and leg due to inadequate assistance during care, and there were multiple concerns about food safety that could put residents at risk for nutritional issues and foodborne illness. Overall, while there are some strengths, the facility does have significant areas needing improvement.
- Trust Score
- D
- In California
- #779/1155
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ○ Average
- 39% turnover. Near California's 48% average. Typical for the industry.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most California facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 24 minutes of Registered Nurse (RN) attention daily — below average for California. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 54 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (39%)
9 points below California average of 48%
Facility shows strength in fire safety.
The Bad
Below California average (3.1)
Below average - review inspection findings carefully
Near California avg (46%)
Typical for the industry
The Ugly 54 deficiencies on record
May 2025
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure one sampled resident (Resident 45), Minimum Data Set (MDS-Resident Assessment and Care Screening tool used to guide car...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the residents' medical records were updated to show document...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record review, the facility failed to maintain a safe, clean, comfortable and homelike environm...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, for one of three sampled residents (Resident 45), the facility failed to dev...
Read full inspector narrative →
Apr 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on observation , interview and record review, the facility failed to protect one of three sampled residents (Resident 2) the right to be free of physical abuse, when Resident 1 slapped Resident ...
Read full inspector narrative →
Apr 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure Resident 1 was free from physical abuse when:
...
Read full inspector narrative →
Feb 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure one of three sampled residents (Resident 1) had ...
Read full inspector narrative →
Oct 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of three sampled residents (Resident 1) or Resident Representative (RR), was provided written information that specified the dur...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0572
(Tag F0572)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide a written notice of rights and services prior to or upon ad...
Read full inspector narrative →
Aug 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of two sampled residents (Resident 2) received the corre...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide assistance for one (Resident 1) of two sampled residents wh...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the resident environment was safe and comfortable when the patio area had refrigerator parts, a circular concrete pad ...
Read full inspector narrative →
Jul 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the treatment for scabies (a contagious, itchy skin rash caused by a tiny burrowing mite called Sarcoptes scabiei.) for one of two s...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
The facility failed to ensure a Certified Nursing Assistant (CNA) 1 followed infection control protocols for one of one sampled Resident (Resident 1) when CNA 1 did not perform hand hygiene prior to f...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow infection prevention and control procedures when Certified Nursing Assistant (CNA) 1, did not wear Personal Protective...
Read full inspector narrative →
Aug 2023
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of three sampled residents (Resident 400) ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to thoroughly investigate an alleged abuse violation and submit the results of their complete investigation to the State Agency (...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to complete a performance review for two of three CNA's (Certified Nurse Assistant) at least once every 12 months.
This failure had the poten...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
Based on interview, and record review, the facility failed to complete and submit quarterly Minimum Data Set (MDS- an assessment tool used to plan care) assessments for nine of nine (9) sampled reside...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide nail care services to four of ten residents (...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to:
ensure the removal of expired biological supplies t...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to ensure the Registered Dietitian (RD) and/or Dietary Manager (DM) were competent to comprehensively evaluate and manage the foo...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to ensure staff were competent to meet professional standards for food safety for 118 of 118 residents when Dietary Aide (DA2):
1...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to store and prepare food in accordance with professional standards for safety when:
1. A resident food refrigerator contained i...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure the outside garbage storage area was maintained in a sanitary condition when refuse and dark liquid waste was found on...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure the following kitchen equipment was maintained in good repair when:
1. Reach-in refrigerator: the rubber gasket (a rub...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the pharmaceutical services were provided to assure accurate...
Read full inspector narrative →
Nov 2019
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview and document review, for one of three residents (Resident 80), the facility failed to provide a dignified dining experience when Certified Nursing Assistant (CNA) 1 rem...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, for one of two sampled residents (Resident 275), the facility failed to inve...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure comprehensive Minimum Data Set (MDS - an assessment tool use...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to transmit an Annual Minimum Data Set (MDS - an assessment tool used ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, for one of one sampled resident (Resident 276) who was on dialysis (process w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, for one of six residents (Resident 275) who were at risk of developing pressure ulcers, the facility failed to provide preventive skin treatment for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, for two of four sampled residents (Resident 81 and 175) who were investigated...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, for one (Resident 175) of two sampled residents who were observed receiving oxygen (O2), the facility failed to ensure Resident 175 received the nece...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure Residents 74 and 76 had their medication regimen reviewed monthly by the consulting pharmacist.
This failure had the potential for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide a safe and sanitary environment when a bathroo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. Review of Resident 115's Annual Minimum Data Set (MDS-tool used to guide care), dated 10/25/19, indicated Resident 115 had mu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, for one of one sampled resident (Resident 114) who had difficulty hearing, the facility failed to provide treatment to maintain hearing abilities whe...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of Resident 23's Face Sheet, printed 12/5/19, indicated Resident 23 was admitted to the facility on [DATE].
Review of ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Social Worker
(Tag F0850)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to employ a qualified social worker on a full time basis.
This deficient practice resulted in the residents' inability to attain or maintain t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to maintain infection control practices when:
1. Manufacturer's directions were not followed for the disinfection of three of th...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Medical Records
(Tag F0842)
Minor procedural issue · This affected multiple residents
Based on interview and document review, the facility failed to ensure medical records for one of 27 residents (Residents 80) contained accurately documented records when Resident 80 had a medical docu...
Read full inspector narrative →
Oct 2018
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, for one (Resident 221) of 17 sampled residents, the facility failed to implement their Inf...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, for one of 17 sampled residents (Resident 116) the facility failed to provide an environment with comfortable sound levels when Resident 116 experien...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
2. Resident 56 was admitted to the facility with diagnoses that included adult failure to thrive and contractures (shortening and hardening of muscles, tendons, or other tissue, often leading to defor...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, for one of 17 sampled residents (Residents 38), the facility failed to provide personal hygiene assistance (combing hair, brushing, teeth, shaving, w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of seventeen sampled residents (Resident 31) with impaired hearing and vision received an individualized, ongoing activity progr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, for one of 17 sampled residents (Resident 220), the facility failed to provid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
3. Review of the Minimum Data Set (MDS - an assessment tool used to guide care), dated 4/13/18, indicated Resident 38 was admitted to the facility with diagnoses that included hemiplegia (paralysis on...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0790
(Tag F0790)
Could have caused harm · This affected 1 resident
2. Review of the face sheet, printed 10/11/18, indicated Resident 15 was admitted to the facility with diagnoses that included dysphagia (difficulty swallowing) and generalized muscle weakness.
Revie...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to implement their Employee Meals policy and procedure to store food under sanitary conditions when there was a dietary staff mem...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, for one of one randomly sampled resident (Resident 114), the facility failed to provide a sanitary environment when an air mattress that was heavily...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Assessment Accuracy
(Tag F0641)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, for one (Resident 39) of 17 sampled residents, the facility failed to ensure the Minimum D...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most California facilities.
- • 39% turnover. Below California's 48% average. Good staff retention means consistent care.
- • 54 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade D (45/100). Below average facility with significant concerns.
About This Facility
What is Crown Bay's CMS Rating?
CMS assigns CROWN BAY NURSING AND REHABILITATION CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Crown Bay Staffed?
CMS rates CROWN BAY NURSING AND REHABILITATION CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 39%, compared to the California average of 46%. This relatively stable workforce can support continuity of care. RN turnover specifically is 57%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Crown Bay?
State health inspectors documented 54 deficiencies at CROWN BAY NURSING AND REHABILITATION CENTER during 2018 to 2025. These included: 1 that caused actual resident harm, 51 with potential for harm, and 2 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
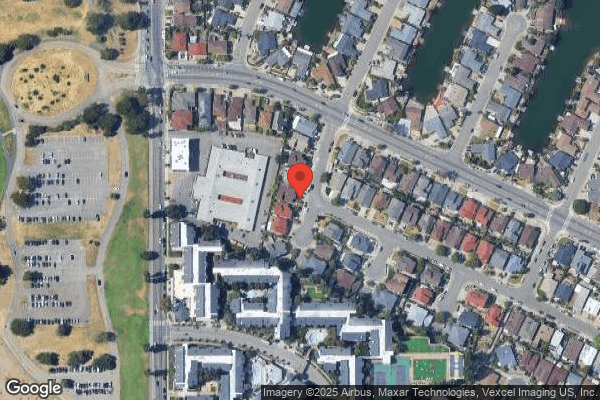
Who Owns and Operates Crown Bay?
CROWN BAY NURSING AND REHABILITATION CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 151 certified beds and approximately 119 residents (about 79% occupancy), it is a mid-sized facility located in ALAMEDA, California.
How Does Crown Bay Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, CROWN BAY NURSING AND REHABILITATION CENTER's overall rating (2 stars) is below the state average of 3.1, staff turnover (39%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Crown Bay?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Crown Bay Safe?
Based on CMS inspection data, CROWN BAY NURSING AND REHABILITATION CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Crown Bay Stick Around?
CROWN BAY NURSING AND REHABILITATION CENTER has a staff turnover rate of 39%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Crown Bay Ever Fined?
CROWN BAY NURSING AND REHABILITATION CENTER has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Crown Bay on Any Federal Watch List?
CROWN BAY NURSING AND REHABILITATION CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.