ALHAMBRA HEALTHCARE & WELLNESS CENTRE, LP




Inspected within the last 6 months. Data reflects current conditions.
Alhambra Healthcare & Wellness Centre has a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranking #520 out of 1,155 facilities in California places it in the top half, but its overall performance may still raise red flags for families. The facility is showing an improving trend, decreasing from 18 issues in 2024 to 15 in 2025, which is a positive sign. Staffing is a weakness here, with a rating of 2 out of 5 stars and a turnover rate of 46%, which is average but concerning for consistency of care. Serious incidents have occurred, including a failure to provide CPR to an unresponsive resident and not adhering to dietary restrictions for another, highlighting areas that need urgent attention despite some strengths in quality measures.
- Trust Score
- F
- In California
- #520/1155
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 46% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $17,388 in fines. Lower than most California facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 16 minutes of Registered Nurse (RN) attention daily — below average for California. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 55 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Near California average (3.1)
Meets federal standards, typical of most facilities
Near California avg (46%)
Higher turnover may affect care consistency
Below median ($33,413)
Minor penalties assessed
The Ugly 55 deficiencies on record
Jun 2025
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to accommodate the needs for one (1) of 21 sampled resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide a safe, sanitary, and homelike environment for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of two sampled residents (Resident 61), wa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow the fluid restriction (a dietary change that l...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to administer a scheduled medication on time for one (1)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0808
(Tag F0808)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review of the facility menu, the facility failed to ensure one (1) of two sampled re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement its policy by not checking the food brought...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure two (2) of two sampled residents (Resident 23 ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement proper gastrostomy tube (GT - a tube that i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During a review of Resident 61's admission Record, the admission Record indicated Resident 61 was admitted to the facility on...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to dispose of expired vegetables stored in the facility kitchen's refrigerator during a kitchen observation conducted on 6/23/202...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to dispose of garbage properly in the facility's garbage disposal area during kitchen observation conducted on 6/23/2025.
This de...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During a review of Resident 38's admission Record, the admission Record indicated the resident was admitted to the facility o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement its protocol for Antibiotic (medication used to kill bact...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0911
(Tag F0911)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one (1) of 47 rooms (map diagram labeled rooms...
Read full inspector narrative →
Jun 2024
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to have an appropriate call light (an alerting device for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to maintain a current copy of the resident's advanced directive (a leg...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** (Cross reference F686)
Based on interview and record review, the facility failed to ensure a comprehensive person-centered care ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure resident care plans were revised for one (1) o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure two (2) of 20 sampled residents (Residents 643 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** (Cross reference F656)
Based on interview and record review the facility failed to ensure one (1) of two (2) sampled residents (...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one (1) of 5 (five) sampled residents (Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to follow its Medication Storage policy by failing to:
1. Refrigerate Residents 48's unused Novolin R Flex Pen (form of insulin, ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. A review of Resident 82's admission Record indicated the resident was initially admitted to the facility on [DATE] and with d...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. A review of Resident 641's admission Record, indicated the resident was initially admitted to the facility on [DATE] with dia...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to follow proper food handling practices in accordance with its policy and procedure by failing to ensure:
1. A container of ric...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** During an interview on 6/28/2024 at 8:29 AM with Infection Preventionist (IP), IP stated, For the facility's water management pr...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0911
(Tag F0911)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one (1) of 47 rooms (map diagram labeled rooms...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to prevent fall () for one (1) of three (3) sampled residents (Resident 1), assessed as high risk for falls when Resident 1 was ...
Read full inspector narrative →
Apr 2024
2 deficiencies
2 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0678
(Tag F0678)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one (1) of 1 sampled resident (Resident 1) was provided with...
Read full inspector narrative →
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Menu Adequacy
(Tag F0803)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow the physician's order to give mechanical soft texture (food ...
Read full inspector narrative →
Apr 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify the doctor for one of one sampled resident (Resident 1), of ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of one sampled resident (Resident 1), had an active doct...
Read full inspector narrative →
Dec 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop a comprehensive person-centered care plan for one of two sa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of two sampled residents (Resident 1), who had a diagnos...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to follow their policy and procedure by failing to:
1. Sanitize and disinfect spaces in between visitors, after Coronavirus (COVI...
Read full inspector narrative →
Jun 2021
19 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of five residents (Resident 64) had an informed consent ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide printed activities material for one of 28 sam...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to accurately code the functional limitations (Section G...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of 19 sampled residents (Resident 27) was ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide appropriate treatments and services to preven...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to post a No Smoking sign for one of seven sampled residents (Resident 366) who was using oxygen.
This deficient practice had t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to develop a dementia (a general term for loss of memory...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure one resident (Resident 8), who was receiving psychotropic (a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide care and services for one of 19 sampled resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure two of two sampled residents (Residents 17 and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. A review of Resident 34's Face Sheet indicated the resident admitted to the facility on [DATE] with diagnoses that included c...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to document the administration of controlled medications...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility had 25 opportunities of medication administration observed and ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
2. During a medication cart inspection with LVN 3 on 6/10/21 at 10:55 am., in station 2, the following six medication bottles did not have the opened date labeled on the container and one suppository ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure proper food storage and preparation by failing to ensure the following:
1.
Dietary staff did not perform handwashing ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure medical records were kept safe and secured from unauthorized use. During an observation, the facility stored their res...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. During a medication pass observation in room [ROOM NUMBER], which was occupied by two residents, on 6/9/21 at 9:40 a.m., the ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to have a functioning call light system for two out of 47 resident bedro...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0911
(Tag F0911)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one out of 47 rooms (map diagram labeled rooms...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 2 life-threatening violation(s). Review inspection reports carefully.
- • 55 deficiencies on record, including 2 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $17,388 in fines. Above average for California. Some compliance problems on record.
- • Grade F (34/100). Below average facility with significant concerns.
About This Facility
What is Alhambra Healthcare & Wellness Centre, Lp's CMS Rating?
CMS assigns ALHAMBRA HEALTHCARE & WELLNESS CENTRE, LP an overall rating of 3 out of 5 stars, which is considered average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Alhambra Healthcare & Wellness Centre, Lp Staffed?
CMS rates ALHAMBRA HEALTHCARE & WELLNESS CENTRE, LP's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 46%, compared to the California average of 46%. This relatively stable workforce can support continuity of care. RN turnover specifically is 69%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Alhambra Healthcare & Wellness Centre, Lp?
State health inspectors documented 55 deficiencies at ALHAMBRA HEALTHCARE & WELLNESS CENTRE, LP during 2021 to 2025. These included: 2 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 50 with potential for harm, and 3 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Alhambra Healthcare & Wellness Centre, Lp?
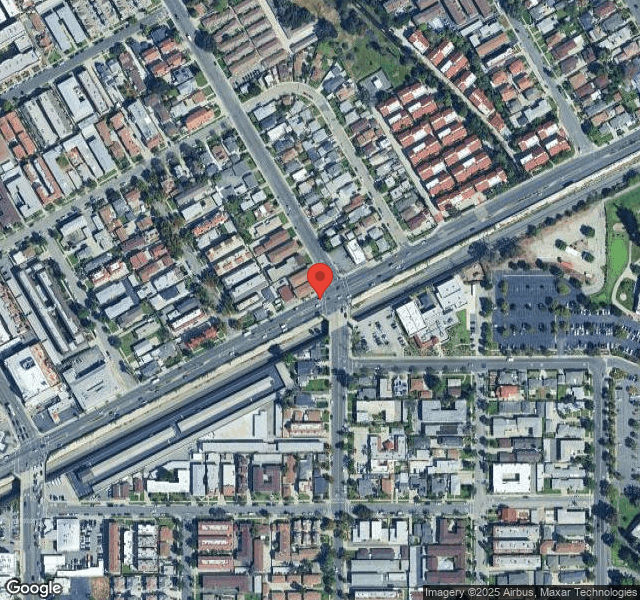
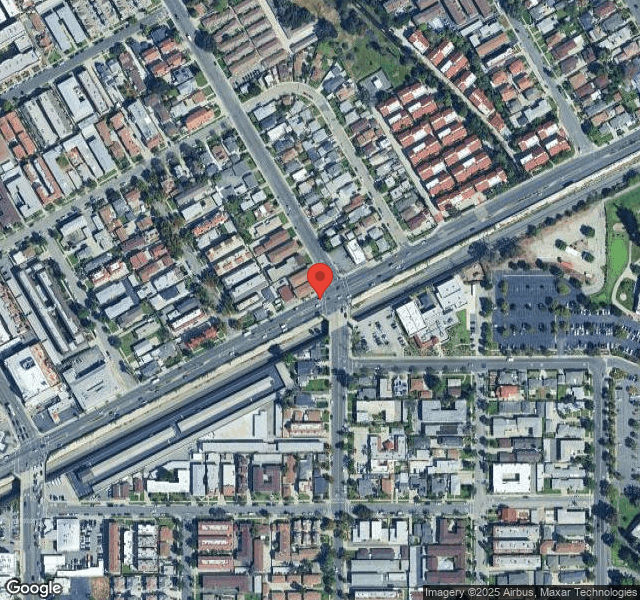
ALHAMBRA HEALTHCARE & WELLNESS CENTRE, LP is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 97 certified beds and approximately 93 residents (about 96% occupancy), it is a smaller facility located in ALHAMBRA, California.
How Does Alhambra Healthcare & Wellness Centre, Lp Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, ALHAMBRA HEALTHCARE & WELLNESS CENTRE, LP's overall rating (3 stars) is below the state average of 3.1, staff turnover (46%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Alhambra Healthcare & Wellness Centre, Lp?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Alhambra Healthcare & Wellness Centre, Lp Safe?
Based on CMS inspection data, ALHAMBRA HEALTHCARE & WELLNESS CENTRE, LP has documented safety concerns. Inspectors have issued 2 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in California. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Alhambra Healthcare & Wellness Centre, Lp Stick Around?
ALHAMBRA HEALTHCARE & WELLNESS CENTRE, LP has a staff turnover rate of 46%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Alhambra Healthcare & Wellness Centre, Lp Ever Fined?
ALHAMBRA HEALTHCARE & WELLNESS CENTRE, LP has been fined $17,388 across 1 penalty action. This is below the California average of $33,253. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Alhambra Healthcare & Wellness Centre, Lp on Any Federal Watch List?
ALHAMBRA HEALTHCARE & WELLNESS CENTRE, LP is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.