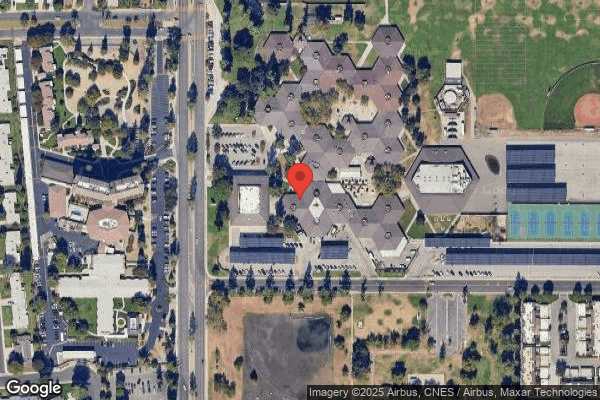
ROSEWOOD HEALTH FACILITY
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Rosewood Health Facility in Bakersfield, California has a Trust Grade of C, which means it is average and falls in the middle of the pack among nursing homes. It ranks #674 out of 1155 facilities statewide, placing it in the bottom half, but it is #2 out of 17 in Kern County, indicating that only one local option is better. The facility is improving, with issues decreasing from 15 in 2024 to just 1 in 2025. Staffing is a strong point, receiving 5 out of 5 stars with a turnover rate of 29%, which is below the state average, suggesting that staff are dedicated and familiar with residents. However, there are concerns, including $8,278 in fines, which is average, and serious incidents like failing to properly assess a resident's fall risk after discontinuing one-on-one monitoring, as well as inadequate responses to a Legionella bacteria issue in the water system, highlighting areas for improvement despite some strengths.
- Trust Score
- C
- In California
- #674/1155
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ✓ Good
- 29% annual turnover. Excellent stability, 19 points below California's 48% average. Staff who stay learn residents' needs.
- Penalties ○ Average
- $8,278 in fines. Higher than 60% of California facilities. Some compliance issues.
- Skilled Nurses ✓ Good
- Each resident gets 53 minutes of Registered Nurse (RN) attention daily — more than average for California. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 51 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Staffing Rating · Excellent nurse staffing levels
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Low Staff Turnover (29%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (29%)
19 points below California average of 48%
Facility shows strength in staffing levels, quality measures, staff retention, fire safety.
The Bad
Near California average (3.1)
Meets federal standards, typical of most facilities
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 51 deficiencies on record
Feb 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the Interdisciplinary team (IDT- a group of professionals fr...
Read full inspector narrative →
Dec 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow their policy and procedure on change of condition for one of three sampled residents (Resident 1). This failure result...
Read full inspector narrative →
Nov 2024
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
During a review of Resident 217's Order Review History Report (ORHR), dated 11/4/24, the ORHR indicated Resident 217 was receiving Temazepam 15 mg capsule, 1 capsule by mouth at bedtime and Mirtazapin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure physician ordered medication was available for one of six sampled residents (Resident 217). This failure resulted in Resident 217's ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow its policy and procedure (P&P) titled, Repositioning for one of three sampled residents (Resident 20). This failure re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Psychotropic Medication Use, for one of seven sampled residents (Resident 217), when the fa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Resident Food and Dining Preferences for two of six sampled residents (Resident 58 and Resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to update the care plan for for one of three sampled residents (Resident 20). This failure resulted in Resident 20 developing Mo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to follow their policy and procedure (P&P) titled Catheter Care, Urinary, for one of two sampled residents (Resident 49) when ti...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow its policy and procedure (P&P) titled, Medicat...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow its policy and procedure (P&P) titled, Water Management Prog...
Read full inspector narrative →
Oct 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0774
(Tag F0774)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide safe transportation for one of three sampled residents (Res...
Read full inspector narrative →
Sept 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of three sampled resident (Resident 1) was treated with dignity and respect. This failure had the potential for Resident 1 exper...
Read full inspector narrative →
Sept 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide ADL (Activities of Daily Living [tasks people do to manage one's basic needs, including personal hygiene or grooming,...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0790
(Tag F0790)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the facility's policy and procedure (P&P) on dental services was followed for one of four sampled residents (Resident 1). This failu...
Read full inspector narrative →
Jan 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to implement its policy and procedure for one of three sampled residents (Resident 1) when staff was not removed from resident care when an al...
Read full inspector narrative →
Oct 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to protect the privacy of two of four sampled residents (Resident 1 and Resident 2). This failure resulted in violation of Resident 1's rights...
Read full inspector narrative →
Sept 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of three sampled residents (Resident 1) received medicat...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure appropriate staff was available to provide medications intra...
Read full inspector narrative →
Aug 2023
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to notify one of four sampled residents (Resident 1) responsible party (RP) of a change in condition (COC). This failure had the potential for...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of four sampled residents (Resident 1) physician ' s orders were carried out and treatment was administered promptly. This failu...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide the fluid requirements for one of four sampled residents (Resident 1). This failure resulted in Resident 1 receiving inadequate flu...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0773
(Tag F0773)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to obtain physician order laboratory (labs), and report results to the physician timely for one of three sampled resident (Resident 1). These ...
Read full inspector narrative →
Feb 2023
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of 29 sampled residents (Resident 8) was assessed and determined appropriate to self-administer medication. This f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to accurately assess the need for denture care for one of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0639
(Tag F0639)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure Social Services performed annual and quarterly resident asse...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to develop and implement a comprehensive care plan for one of 29 sampled residents (Resident 19). This failure resulted in Reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement its policy and procedure (P&P) on Repositioning when one ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure two of seven staff members (Certified Nursing Assistant (CNA) 3 and Housekeeper 1) were trained in fall prevention mea...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to:
1. Ensure poured medications temporarily held were appropriately labeled and secured for three of six sampled residents (Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0790
(Tag F0790)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide dental service for one of 29 sampled residents (Resident 19) promptly. This failure had the potential for the delay o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
During an interview on 2/7/23, at 10:03 AM, with admission Director (ADMD), ADMD stated, new residents or family should be offered assistance with AD upon admission. ADMD stated, We just started offer...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to follow its policy and procedure (P&P) on Departmental Policy (Respiratory Therapy) -Prevention of Infection when the water of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to maintain a medication error rate of less than five percent (%) when:
1. Diltiazem CD (medication to treat blood pressure and ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected most or all residents
During a concurrent interview and record review, on 2/9/23, at 3:25 PM, with MDSN, Resident 9's MRR, dated 1/24/23 was reviewed. The MRR indicated, MD reviewed, agreed, and signed the MRR on 2/5/23. T...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to implement its policy and procedure (P&P) on Preventing Foodborne Illness-Employee Hygiene and Sanitary Practices when one of ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure infection prevention and control practices were implemented when:
1. Occupational Therapist (OT) exited Resident 366's...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their abuse policy and procedure (P&P) for one of one sampled residents (Resident 1). This failure had the potential to place the re...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to prevent a staff member (Certified Nursing Assistant [CNA] 1) from verbally abusing one of three sampled residents (Resident 1). This failur...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to create measurable and objective (a statement describing results to be achieved) care plans for two of two sampled residents (...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of three sampled residents (Resident 1)'s responsible party (RP) was informed of the bed-hold policy when Resident 1 was transfe...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow its policy and procedure on change in resident ' s condition...
Read full inspector narrative →
Oct 2019
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow its policy and procedure on Advance Directives (living will or durable power of attorney for health care) for three of 39 sampled re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide a baseline care plan summary (the instructions needed to pr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During an interview with Licensed Vocational Nurse (LVN) 2 and review of the clinical record for Resident 31, on 10/31/19, at...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide resident centered activities for one of 39 sampled residents (Resident 150). This failure had the potential to negatively impact th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
2. During a review of the clinical record for Resident 11, the Physician's Order, dated 8/21/18, indicated Depakote (a mood stabilizer medication) 125 mg (milligram, a unit of measurement) one tablet ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
3. During an observation and interview with Resident 31, on 10/29/19, at 9:44 PM, in Resident 31's room, a CPAP machine was observed on the bedside table. Resident 31 stated he uses the CPAP machine n...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain the high temperature dishmachine conveyor (a dishwasher with booster heaters that raise the interior water temperatu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to have a complete and accurate log of discontinued controlled medications. This had the potential for diversion of controlled medications.
Find...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to provide and maintain safe and sanitary handling, storage, and distribution of food when:
1. The staff assisting and serving m...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 29% annual turnover. Excellent stability, 19 points below California's 48% average. Staff who stay learn residents' needs.
- • 51 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade C (56/100). Below average facility with significant concerns.
About This Facility
What is Rosewood Health Facility's CMS Rating?
CMS assigns ROSEWOOD HEALTH FACILITY an overall rating of 3 out of 5 stars, which is considered average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Rosewood Health Facility Staffed?
CMS rates ROSEWOOD HEALTH FACILITY's staffing level at 5 out of 5 stars, which is much above average compared to other nursing homes. Staff turnover is 29%, compared to the California average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Rosewood Health Facility?
State health inspectors documented 51 deficiencies at ROSEWOOD HEALTH FACILITY during 2019 to 2025. These included: 1 that caused actual resident harm and 50 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Rosewood Health Facility?
ROSEWOOD HEALTH FACILITY is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility is operated by HUMANGOOD, a chain that manages multiple nursing homes. With 79 certified beds and approximately 64 residents (about 81% occupancy), it is a smaller facility located in BAKERSFIELD, California.
How Does Rosewood Health Facility Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, ROSEWOOD HEALTH FACILITY's overall rating (3 stars) is below the state average of 3.1, staff turnover (29%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Rosewood Health Facility?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Rosewood Health Facility Safe?
Based on CMS inspection data, ROSEWOOD HEALTH FACILITY has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Rosewood Health Facility Stick Around?
Staff at ROSEWOOD HEALTH FACILITY tend to stick around. With a turnover rate of 29%, the facility is 17 percentage points below the California average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly.
Was Rosewood Health Facility Ever Fined?
ROSEWOOD HEALTH FACILITY has been fined $8,278 across 1 penalty action. This is below the California average of $33,162. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Rosewood Health Facility on Any Federal Watch List?
ROSEWOOD HEALTH FACILITY is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.