GOLDEN HARBOR HEALTHCARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Golden Harbor Healthcare Center has received an F Trust Grade, indicating significant concerns about the quality of care provided. Ranked #1027 out of 1155 facilities in California, they are in the bottom half, and #68 out of 69 in Alameda County, meaning there is only one local option that performs worse. Although the facility is improving, reducing issues from 7 in 2024 to 2 in 2025, it still faces challenges, including $43,554 in fines, which is higher than 79% of California facilities, signaling compliance problems. Staffing is a strength with a 0% turnover rate, but the facility struggled to provide adequate Registered Nurse coverage, failing to have RNs on duty for eight of twelve sampled days, which could jeopardize resident safety. Specific incidents of concern include a resident with a history of elopement leaving the facility unattended and another resident's room being searched by the sheriff after live bullets were found in their laundry, highlighting serious safety risks.
- Trust Score
- F
- In California
- #1027/1155
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ○ Average
- $43,554 in fines. Higher than 52% of California facilities. Some compliance issues.
- Skilled Nurses ○ Average
- RN staffing data not reported for this facility.
- Violations ⚠ Watch
- 39 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below California average (3.1)
Significant quality concerns identified by CMS
Above median ($33,413)
Moderate penalties - review what triggered them
The Ugly 39 deficiencies on record
Mar 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to provide treatment and care in accordance with professional standards of practice for one of one sampled resident (Resident 1) ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and record review, the facility failed to provide pharmaceutical services and procedures that assure accurate dispensing and administration when Resident 1's Inhaler ...
Read full inspector narrative →
Nov 2024
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to identify and address a potential accident hazard when Activity Assis...
Read full inspector narrative →
May 2024
6 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, record reviews, for two of three (Resident 53 and 43) sampled residents who were reviewed for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement a comprehensive person-centered care plan to address the ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure a system of records for controlled drugs (medications regulated by the government due to high risk for potential abuse and dependenc...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure three of 18 sampled residents (Residents 33, 23, and 28) res...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure medications were dated and stored under proper temperature controls in the medication refrigerator for one of two medi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure there was Registered Nurse (RN) coverage eight hours a day, seven days a week, when an RN was not on duty for eight of 12 days sampl...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to provide and ensure services to maintain personal hygiene for one (Resident 1) of three sampled residents. The certified nursing assistants...
Read full inspector narrative →
Jan 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the skilled nursing facility did not protect the right of a resident to make their own health care decisions for one of three sampled residents (Res...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility's licensed nursing staff did not accurately assess the health care status for one of three sampled residents (Resident 1). Resident 1 received hospic...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review, the skilled nursing facility did not maintain an accurate medical record for one of three sampled residents (Resident 1). Licensed nursing staff documented a tele...
Read full inspector narrative →
Nov 2022
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, for one of three sampled residents (Resident 1), that were discharged , the facility faile...
Read full inspector narrative →
Mar 2022
20 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to make reasonable effort to safeguard the resident's property for one (Resident 36) sampled resident when Resident 36 complained of missing ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, for one of three residents (Resident 49) reviewed for closed records, the facility failed to notify Resident 49's representative of the decision to transfer Resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interview and closed record review, for two of three sampled residents, (Residents 47 and 49), the facility failed to:
1. Notify in writing, Resident 47 and Resident's Representative 2 (RR 2)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on interview and closed record review, for one of three sampled residents (Resident 49), the facility did not provide Resident 49 and Resident Representative 1 (RR 1) written information about t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to ensure the Minimum Data Set (MDS-Resident Assessment and Care Screening tool used to guide care), was accurate for one ( Resident 24) samp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, for one of two sampled residents (Resident 27) reviewed for PASRR (Pre-admission Screening...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, for one of four sampled residents (Resident 14), the facility failed to implement a compre...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, for one (Resident 30) of one sampled resident reviewed for skin issues, the facility failed to ensure treatment and care were provided in accordance...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure nursing staff had the appropriate competencies and skills sets for providing care to residents when staff training for behavioral se...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to ensure two (Residents 27 and 36) sampled residents were free from unnecessary drugs when:
1. Resident 36 was administered trazodone (anti-...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to remove expired medication for one of 16 residents (Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
Based on interview and record review, for one of four sampled residents (Resident 14), the facility failed to obtain physician ordered laboratory tests.
This failure resulted in not monitoring and re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected 1 resident
Based on interviews and record review the facility failed to ensure the staff skills competency evaluations were completed for one [NAME] (CK 1). CK 1's competency evaluation was not completed before ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review, for one of three sampled residents (Resident 42) reviewed for advanced directives, the facility failed to ensure Resident 27's clinical record was complete when t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility's quality assessment and assurance committee did not meet quarterly as required.
This failure had the potential to result in not identifying quality...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, the facility failed to update and revise four of 16 sampled resident (residents 10, 23, 29 an...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review, the facility failed to ensure five (Residents 19, 23, 24, 36, and 39) sample...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure three sampled residents (Resident 19, 24 and 36) received b...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to follow the policy and procedure to conduct infection control surveillance when they did not track, analyze, and create infection control da...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to follow the policy and procedure to implement antibiotic stewardship when they did not monitor appropriate use of antibiotics and improved o...
Read full inspector narrative →
Jul 2019
5 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to monitor and modify interventions for one (Resident 10) of one sampled resident who was assessed to be at risk for impaired nu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement their policy for safe and sanitary storage, handling and consumption of food brought in by family members for one (...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure that services were provided in a dignified and respectful manner for four (Residents 6, 19, 41, and 58) of four sampled residents wh...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0568
(Tag F0568)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to provide 17 of 17 sampled residents (Resident 4, 11, 14, 16, 17, 18, 21, 25, 27, 29, 30, 35, 38, 41,42, 45, 49), who's funds were managed by...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations, interview, and record review, the facility failed to ensure there was an air gap in the kitchen in order to prevent backflow of contaminates from the water supply outlet.
This f...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s), $43,554 in fines. Review inspection reports carefully.
- • 39 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $43,554 in fines. Higher than 94% of California facilities, suggesting repeated compliance issues.
- • Grade F (23/100). Below average facility with significant concerns.
About This Facility
What is Golden Harbor Healthcare Center's CMS Rating?
CMS assigns GOLDEN HARBOR HEALTHCARE CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Golden Harbor Healthcare Center Staffed?
CMS rates GOLDEN HARBOR HEALTHCARE CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes.
What Have Inspectors Found at Golden Harbor Healthcare Center?
State health inspectors documented 39 deficiencies at GOLDEN HARBOR HEALTHCARE CENTER during 2019 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 38 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
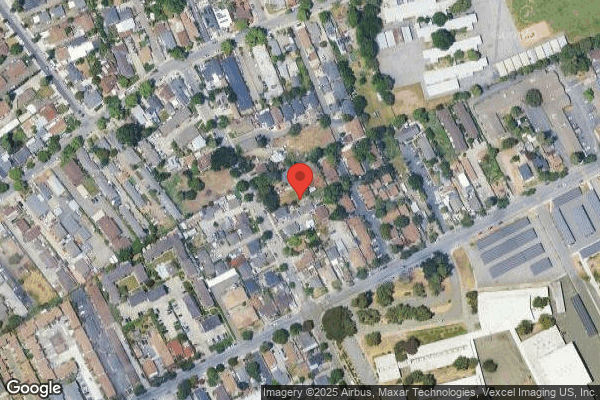
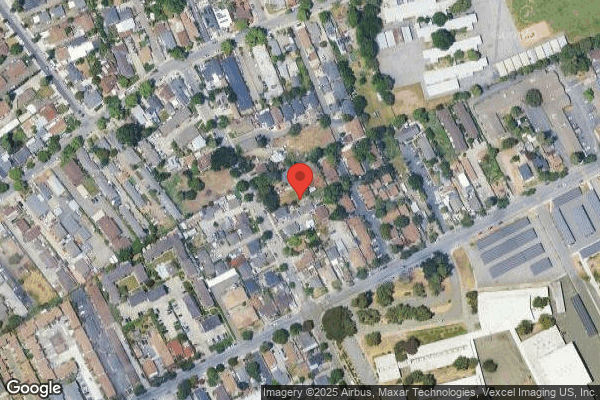
Who Owns and Operates Golden Harbor Healthcare Center?
GOLDEN HARBOR HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 99 certified beds and approximately 91 residents (about 92% occupancy), it is a smaller facility located in HAYWARD, California.
How Does Golden Harbor Healthcare Center Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, GOLDEN HARBOR HEALTHCARE CENTER's overall rating (1 stars) is below the state average of 3.1 and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Golden Harbor Healthcare Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Golden Harbor Healthcare Center Safe?
Based on CMS inspection data, GOLDEN HARBOR HEALTHCARE CENTER has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in California. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Golden Harbor Healthcare Center Stick Around?
GOLDEN HARBOR HEALTHCARE CENTER has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Golden Harbor Healthcare Center Ever Fined?
GOLDEN HARBOR HEALTHCARE CENTER has been fined $43,554 across 4 penalty actions. The California average is $33,514. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Golden Harbor Healthcare Center on Any Federal Watch List?
GOLDEN HARBOR HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.