Lompoc Valley Medical Center Comprehensive Care Ce




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Lompoc Valley Medical Center Comprehensive Care Center has earned a Trust Grade of B, which indicates it is a good choice but not among the very best facilities. It ranks #121 out of 1,155 nursing homes in California, placing it in the top half of the state, and #4 out of 14 in Santa Barbara County, meaning only three local options are better. The facility is improving, having reduced its issues from four in 2024 to two in 2025, and it has a strong staffing rating with a 0% turnover, indicating that staff members are committed to the residents. However, there are some concerns, including $6,500 in fines, which is average, and specific incidents such as failing to properly clean glucometers and reusing dirty personal protective equipment, both of which pose infection risks. Overall, while the facility has significant strengths, families should be aware of these weaknesses when considering care options.
- Trust Score
- B
- In California
- #121/1155
- Safety Record
- Low Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ✓ Good
- $6,500 in fines. Lower than most California facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 74 minutes of Registered Nurse (RN) attention daily — more than 97% of California nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 24 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, fire safety.
The Bad
Below median ($33,413)
Minor penalties assessed
The Ugly 24 deficiencies on record
Jul 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, facility failed to administer a prescribed medication (Bimatoprost - medicine to lower pre...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, interview, and facility policy review, the facility failed to follow professional food storage standards for labeling food in 1 of 1 walk-in freezer in the facility kitchen.
Find...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to implement abuse prevention policy when two residents (Resident 1 and 2) had an alleged abuse incident on 7/17/24 for which no interventions ...
Read full inspector narrative →
Jun 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure staff was available to answer a resident's cal...
Read full inspector narrative →
Jan 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, and facility policy and procedure (P/P), the facility failed to ensure the environment was fr...
Read full inspector narrative →
Jan 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide evidence that an allegation of abuse was thoroughly investigated for one of two residents (Resident 1).
This failure had the potent...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of 3 sampled residents (Resident 1), was free from physi...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a call light was within reach, for one of three sampled residents (Resident 1).
This facility failure had the potentia...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0563
(Tag F0563)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure when they posted the signage facility closed for visitation...
Read full inspector narrative →
Nov 2022
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected 1 resident
Based on interview, and record review, the facility failed to maintain an effective pest control program, when a termite infestation was discovered in one of two sampled residents (Resident 1) rooms.
...
Read full inspector narrative →
Nov 2022
3 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to offer the influenza (Flu- a highly contagious infectious disease) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to offer the COVID-19 (a highly contagious infectious disease) vaccin...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to maintain infection control practices when:
1. Glucometers (machine used to measure blood sugar) were not cleaned and disinfec...
Read full inspector narrative →
May 2022
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. According to Nursing Fundamentals by [NAME], [NAME] and [NAME], second edition, 2010 p. 322, Documentation is the professiona...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on observation and interview the facility failed to ensure a resident with impaired upper mobility was provided with other form of communication system or device to call for assistance for one o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure:
1. Hydration needs were met for Resident 61 wh...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
2) During a review of the clinical record for Resident 48 indicated diagnoses that included but not limited to unspecified dementia and major depressive disorder (feelings of worthlessness, no energy ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview the facility failed to ensure medications are not expired for one unsampled resident (Resident 19).
This failure had the potential for the resident t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to accommodate food preferences for two residents (Resident 76 and 30).
This failure had the potential not to meet residents' f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. During an observation and concurrent interview on 5/03/22 9:07 a.m., LN3 opened the second drawer of medication cart four (MC...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to store, prepare, distribute, and serve food and ice in accordance with professional standards when:
1. ambient room temperature...
Read full inspector narrative →
Feb 2020
3 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure an oxygen tank was full for one of one residents (Resident 9) dependent on oxygen.
This facility failure caused Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based upon observation, interview, and record review, the facility failed to ensure one of 18 residents (Resident 74 ) received pain medication based upon the level of pain experienced by the patient....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
3. The National Library of Medicine, National Institutes of Health (NCBI) Annex E Isolation rooms or areas retrieved 2/18/20 https://www.ncbi.nlm.nih.gov/books/NBK214341/ indicated in part, Stock the ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • 24 deficiencies on record. Higher than average. Multiple issues found across inspections.
About This Facility
What is Lompoc Valley Medical Center Comprehensive Care Ce's CMS Rating?
CMS assigns Lompoc Valley Medical Center Comprehensive Care Ce an overall rating of 5 out of 5 stars, which is considered much above average nationally. Within California, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Lompoc Valley Medical Center Comprehensive Care Ce Staffed?
CMS rates Lompoc Valley Medical Center Comprehensive Care Ce's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes.
What Have Inspectors Found at Lompoc Valley Medical Center Comprehensive Care Ce?
State health inspectors documented 24 deficiencies at Lompoc Valley Medical Center Comprehensive Care Ce during 2020 to 2025. These included: 24 with potential for harm.
Who Owns and Operates Lompoc Valley Medical Center Comprehensive Care Ce?
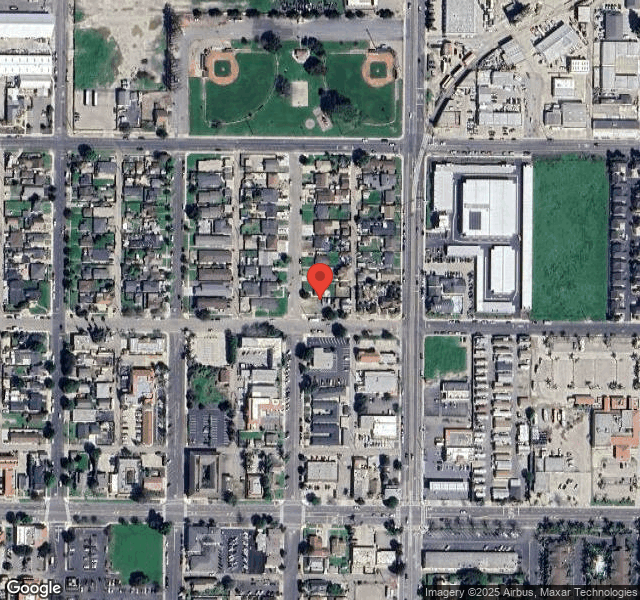
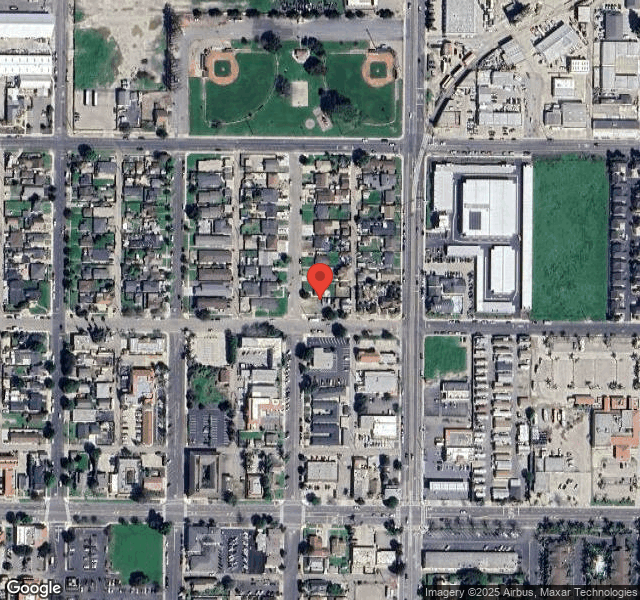
Lompoc Valley Medical Center Comprehensive Care Ce is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 110 certified beds and approximately 96 residents (about 87% occupancy), it is a mid-sized facility located in Lompoc, California.
How Does Lompoc Valley Medical Center Comprehensive Care Ce Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, Lompoc Valley Medical Center Comprehensive Care Ce's overall rating (5 stars) is above the state average of 3.2 and health inspection rating (5 stars) is much above the national benchmark.
What Should Families Ask When Visiting Lompoc Valley Medical Center Comprehensive Care Ce?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Lompoc Valley Medical Center Comprehensive Care Ce Safe?
Based on CMS inspection data, Lompoc Valley Medical Center Comprehensive Care Ce has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 5-star overall rating and ranks #1 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Lompoc Valley Medical Center Comprehensive Care Ce Stick Around?
Lompoc Valley Medical Center Comprehensive Care Ce has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Lompoc Valley Medical Center Comprehensive Care Ce Ever Fined?
Lompoc Valley Medical Center Comprehensive Care Ce has been fined $6,500 across 1 penalty action. This is below the California average of $33,144. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Lompoc Valley Medical Center Comprehensive Care Ce on Any Federal Watch List?
Lompoc Valley Medical Center Comprehensive Care Ce is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.