GUARDIAN REHABILITATION HOSPITAL




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Guardian Rehabilitation Hospital has a Trust Grade of B, indicating it is a good choice, ranking in the top half of California facilities at #89 out of 1,155. Within Los Angeles County, it stands at #20 out of 369, showing it is one of the better local options. The facility is improving, with reported issues decreasing from 26 in 2024 to just 7 in 2025. Staffing is rated at 4 out of 5 stars, though turnover is average at 40%, which is similar to the state average. However, there are concerning aspects, including $32,040 in fines, which is higher than 75% of California facilities, suggesting ongoing compliance issues. Specific incidents include a serious case where a resident, who was at high risk for falls, fell from her bed and suffered significant injuries due to a lack of safety measures. Additionally, there were failures to ensure proper staffing hours were posted, preventing families from knowing who was available to care for their loved ones. Lastly, some residents did not receive the necessary services for maintaining their mobility, which could lead to further health complications. Overall, while there are notable strengths in care quality and improvement trends, these weaknesses highlight the need for ongoing attention to safety and compliance.
- Trust Score
- B
- In California
- #89/1155
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ○ Average
- 40% turnover. Near California's 48% average. Typical for the industry.
- Penalties ✓ Good
- $32,040 in fines. Lower than most California facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 38 minutes of Registered Nurse (RN) attention daily — about average for California. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 46 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (40%)
8 points below California average of 48%
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Near California avg (46%)
Typical for the industry
Below median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 46 deficiencies on record
Jan 2025
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement interventions to prevent accident risks and hazards for one of five sampled residents (Resident 77. Resident 77 was...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure one sampled resident (Resident 230) receiving o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain complete and accurate documentation for one ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure two of seven sampled residents (Residents 49 a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure annual competencies were completed for six of six sampled Restorative Nursing Aides, who perform RNA program tasks inc...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to maintain six of six electrical rehabilitation therapy (given to restore an individual back to their highest possible level of...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0912
(Tag F0912)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure two of 32 sampled resident rooms (room [ROOM NU...
Read full inspector narrative →
Aug 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of three sampled residents (Residents 1's) comprehensive...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of three sampled residents (Resident 1), w...
Read full inspector narrative →
Jul 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure for one of four sampled residents (Resident 1) who had a cha...
Read full inspector narrative →
Jun 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide care in a manner that promote or enhanced resident's dignit...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility staff failed to ensure physician (MD) notification and change of condition (C...
Read full inspector narrative →
May 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure documentation of grievances was completed for one of three s...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to document a medication intolerance for cephalexin (medication to tre...
Read full inspector narrative →
Mar 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop and implement a comprehensive care plan that met the care/s...
Read full inspector narrative →
Mar 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide reasonable accommodations for resident needs and preference...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement their policy regarding reporting of residents ' allegatio...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement its abuse prevention policy by failing to report an alleg...
Read full inspector narrative →
Feb 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Transfer
(Tag F0626)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to allow and readmit one of three sampled resident (Resident 1) to ret...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of three sampled resident (Resident 2) was...
Read full inspector narrative →
Feb 2024
13 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide reasonable accommodations for one of three sampled residents (Resident 25), by failing to ensure the resident's call ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a current copy of the resident's advance directive (a writte...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide assistance with activities of daily living (ADL) for one of six sampled residents (Resident 69). For Resident 69, who...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to monitor and record the intake and output for one of five sampled re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide services that promote the prevention of pressure ulcer injury (injury to the skin caused by pressure) for one of thre...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow its policy and procedure titled,Fall Risk and Prevention of ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide the care and services necessary to prevent urinary tract infections (UTI, infection in the urinary system) for one of...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide necessary respiratory care services for one of four sampled residents (Resident 132) by failing to ensure the residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of two sampled residents (Resident 15) who received dialysis (process of removing waste products and excess fluid from the body)...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to:
-Ensure all opened food items stored in one of one walk-in freezers were labeled with the name of the food item, open date, a...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed properly store and dispose of seven used Fentanyl (a medication classified as a narcotic which is a drug that produces pain reli...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to post daily actual hours worked by licensed and unlicensed staff providing direct care to the residents for 1/1/2023 to 2/10/20...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0912
(Tag F0912)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and record review, the facility failed to ensure two of 32 sampled resident rooms (rooms [ROOM NUMBERS]) me...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview, and record review, the facility failed to ensure one of three sampled residents (Resident 1) received treatment and care in accordance with physician's orders to maintain the highe...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to implement its' abuse prevention policy and procedures (P &P) for one...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on interview, and record review, the facility failed to maintain an effective infection prevention and control program (A system for preventing, identifying, reporting, investigating, and contro...
Read full inspector narrative →
Dec 2022
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of three sampled residents (Resident 1), w...
Read full inspector narrative →
Oct 2021
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement care plan interventions to meet one of one ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to verify the time to apply Lidoderm (a medication used to treat pain) 5% (percent) patch with the ordering physician for one sa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement the smoking policy and procedure to safely ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to report food dislikes and provide food alternatives for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, facility failed to dispose of two expired (should not be used because it mayb...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0800
(Tag F0800)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to store, prepare, distribute, and serve food in accordance with professional standards for food service safety when:
1) Dietary ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure cooling of multiple potentially hazardous foods (e.g. roast beef, chicken, and beef broth) were completed and logged i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure two of three sampled residents (Residents 26 and 67) did not share and smoke the same cigarette.
This deficient practi...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0912
(Tag F0912)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure two of 32 resident rooms (Rooms 102 an 125) me...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 40% turnover. Below California's 48% average. Good staff retention means consistent care.
- • 46 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $32,040 in fines. Higher than 94% of California facilities, suggesting repeated compliance issues.
About This Facility
What is Guardian Rehabilitation Hospital's CMS Rating?
CMS assigns GUARDIAN REHABILITATION HOSPITAL an overall rating of 5 out of 5 stars, which is considered much above average nationally. Within California, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Guardian Rehabilitation Hospital Staffed?
CMS rates GUARDIAN REHABILITATION HOSPITAL's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 40%, compared to the California average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Guardian Rehabilitation Hospital?
State health inspectors documented 46 deficiencies at GUARDIAN REHABILITATION HOSPITAL during 2021 to 2025. These included: 1 that caused actual resident harm, 42 with potential for harm, and 3 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
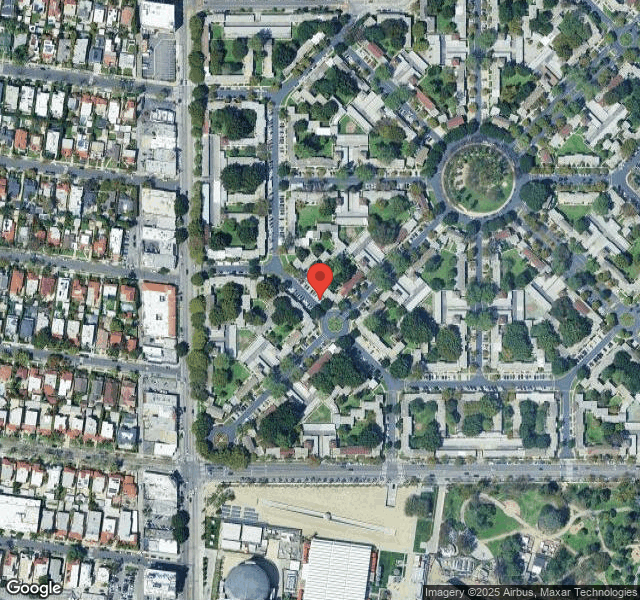
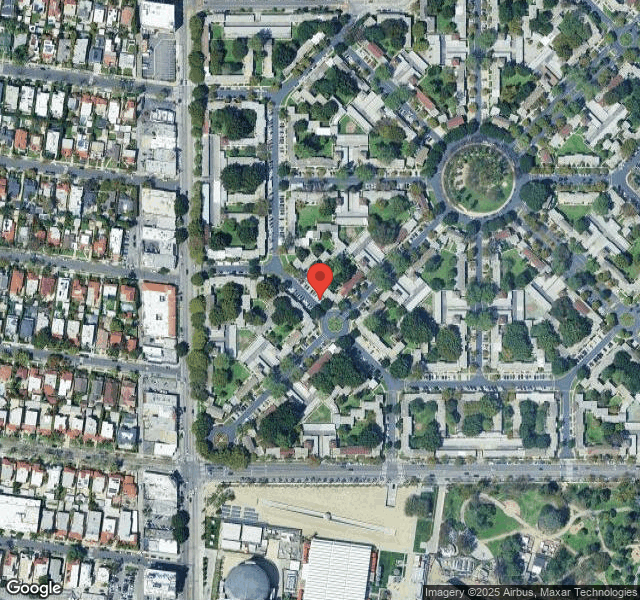
Who Owns and Operates Guardian Rehabilitation Hospital?
GUARDIAN REHABILITATION HOSPITAL is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by THE MANDELBAUM FAMILY, a chain that manages multiple nursing homes. With 93 certified beds and approximately 85 residents (about 91% occupancy), it is a smaller facility located in LOS ANGELES, California.
How Does Guardian Rehabilitation Hospital Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, GUARDIAN REHABILITATION HOSPITAL's overall rating (5 stars) is above the state average of 3.2, staff turnover (40%) is near the state average of 46%, and health inspection rating (4 stars) is above the national benchmark.
What Should Families Ask When Visiting Guardian Rehabilitation Hospital?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Guardian Rehabilitation Hospital Safe?
Based on CMS inspection data, GUARDIAN REHABILITATION HOSPITAL has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 5-star overall rating and ranks #1 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Guardian Rehabilitation Hospital Stick Around?
GUARDIAN REHABILITATION HOSPITAL has a staff turnover rate of 40%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Guardian Rehabilitation Hospital Ever Fined?
GUARDIAN REHABILITATION HOSPITAL has been fined $32,040 across 1 penalty action. This is below the California average of $33,399. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Guardian Rehabilitation Hospital on Any Federal Watch List?
GUARDIAN REHABILITATION HOSPITAL is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.