CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
Based on interview and record review, the facility failed to: 1. Provide supervision (refers to the ongoing monitoring and guidance provided by staff to ensure the safety and well-being of a resident)...
Read full inspector narrative →
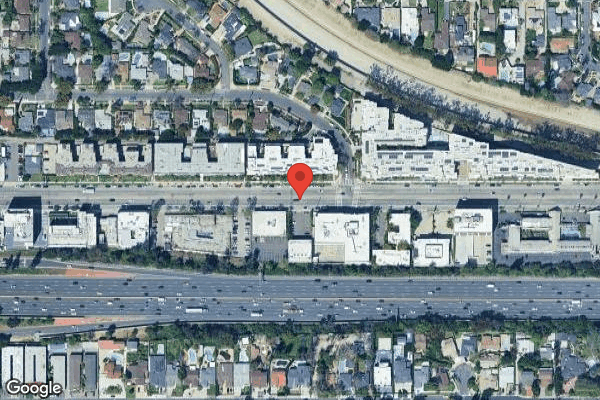
Based on interview and record review, the facility failed to: 1. Provide supervision (refers to the ongoing monitoring and guidance provided by staff to ensure the safety and well-being of a resident) to one of one sampled resident (Resident 97), who was cognitively impaired (refers to difficulties with thinking, learning, remembering, and using judgment, among other mental abilities), unable to verbalize needs due to aphasia (a disorder that makes it difficult to speak), had history of falls and elopement (the act of leaving a facility unsupervised and without prior authorization), and identified as at risk for elopement, by: A. Failing to monitor Resident 97's whereabouts on 7/25/2025 at 12:14 p.m. (date and time of Resident 97's elopement). The facility staff were not aware Resident 97 had left the facility until around 5 p.m. when CNA 2 was distributing the dinner trays and Resident 97 was not in his (Resident 97) room. Facility staff (Certified Nursing Assistant [CNA] 1, CNA 2, CNA 3, Licensed Vocational Nurse [LVN] 1, Registered Nurse [RN] 1, and RN 2) did not know Resident 97 was an elopement risk and did not know what interventions are in place to prevent Resident 97 from eloping. There were multiple missed opportunities for the facility staff to prevent Resident 97's elopement and to remain aware of Resident 97's whereabouts: a.1 On 7/25/2025 at 12:07 p.m., CNA 1 documented in Resident 97's Nutritional Amount Eaten Percentage (%) as 50% and set-up or clean-up assistance was provided to Resident 97 without directly observing Resident 97 eat his (Resident 97) lunch. Resident 97 had a physician's order to provide Resident 97 with supervision during meals which was not followed. a.2 On 7/25/2025 at 12:53 p.m., LVN 1 documented a blood pressure (BP - the pressure of circulating blood against the walls of blood vessels) reading of 110/62 millimeters of mercury (mmHg- unit of pressure, normal range is between 90/60 mmHg and 120/80 mmHg) for Resident 97, stating that he (LVN 1) used the BP reading previously obtained on 7/25/2025 at 8:00 a.m. Resident 97 had a physician's order to monitor Resident 97's BP every six hours (midnight - 6 a.m.-12 p.m.- 6 p.m. intervals). a.3 Resident 97 had physician's orders for monitoring every shift for falls and episodes of depression (a mental health condition that makes you feel persistently sad and lose interest in things you usually enjoy) manifested by crying which were not completed during the 7 a.m. to 3 p.m. shift on 7/25/2025. a.4. During the 3 p.m. hand off report (change of shift) on 7/25/2025, CNA 2 stated there was no mention of Resident 97. RN 2 stated that RN 1 did not provide any information regarding Resident 97. Both RN 1 and RN 2 were unaware that Resident 97 had an elopement incident on 1/29/2025 and had been identified as an elopement risk. B. Failing to implement the facility's Policy and Procedures (P&P) titled, Wandering and Elopements, last reviewed on 4/24/2025 indicating, . the resident's care plan will include strategies and interventions to maintain the resident's safety. Resident 97's care plan titled, Elopement Risk, initiated on 1/30/2025, was not person-centered (prioritizing the resident's needs, preferences, values and goals) and did not include interventions for monitoring and supervision to ensure Resident 97's safety. C. Failing to implement their P&P titled, Safety and Supervision of Residents, last reviewed on 4/24/2025 indicating, Resident safety and supervision and assistance to prevent accidents are facility-wide priorities The care team shall target interventions to reduce individual risks related to hazards in the environment including adequate supervision Resident supervision is a core component of the system's approach to safety. The type and frequency of resident supervision is determined by the individual resident's assessed needs This deficient practice resulted in Resident 97's elopement on 7/25/2025 at 12:14 p.m., placing Resident 97 at risk for vehicular accidents since the facility is located in a busy street with many cars passing by, negative outcome from not receiving Resident 97's medication, and exposure to environmental elements (hot weather), and possible physical attacks from strangers that could lead to serious injury, serious harm and death. On 7/25/2025, in the afternoon (exact time not indicated), Resident 97 was found on the ground in the street (not known) with a small contusion (known as bruise, an injury to the soft tissue often produced by a blunt force such as a kick, fall, or blow) to the right frontal scalp (area at the very front of your head where your hairline begins and the hair that frames your face, including the area around your temples). Resident 97 was admitted to General Acute Care Hospital (GACH) 1 on 7/25/2025 at 2:23 p.m. for trauma (a physical injury or wound caused by an external force, or a psychological or emotional upset resulting from severe mental or emotional stress or physical injury). On 7/29/2025, Resident 97's family visited Resident 97 at GACH 1 and upon seeing the family member, Resident 97 cried for 10 minutes. 2. Ensure Resident 7's bed was at the lowest position and the floor/fall mat (a cushioned floor pad designed to help prevent injury should a person fall) on the right side of the bed did not have a side table on top of them. 3. Ensure Residents 21 and 32 did not have any medications left at the bedside. 4. Ensure Resident 70's feeding pump pole was not placed on top of the left floor mat. 5. Ensure Resident 82's pathway to the restroom was unobstructed with the two roommate's bedside tables. These deficient practices increased the risk of accidents such as falls with injuries and accidental ingestion of chemicals/biologicals on residents. On 7/31/2025 at 2:30 p.m., while onsite at the facility, the State Survey Agency (SSA) called an Immediate Jeopardy (IJ - a situation in which the facility's non-compliance with one or more requirements of participations has caused, or is likely to cause, serious injury, harm, impairment, or death of a resident) in the presence of the Administrator (Adm) and the Director of Nursing (DON) due to the facility's failure to provide supervision to Resident 97 and to prevent the elopement of Resident 97 on 7/25/2025 at 12:14 p.m. On 8/1/2025 at 4:36 p.m., the DON provided an acceptable IJ removal plan (a detailed plan to address the IJ findings) for the facility's failure to provide supervision to Resident 97 and to prevent the elopement of Resident 97 on 7/25/2025 at 12:14 p.m. On 8/1/2025 at 5:19 p.m., while onsite at the facility, the SSA verified and confirmed the facility's full implementation of the IJ Removal Plan through observations, interviews, and record reviews, and determined the IJ situation regarding elopement due to lack of supervision was no longer present. The SSA removed the IJ on 8/1/2025 at 5:19 p.m., in the presence of the Adm and DON. The acceptable IJ Removal Plan included the following summarized actions: 1. On 7/29/2025, the facility marketer visited Resident 97 at GACH 1 and confirmed with the attending nurse that Resident 97 had been brought to GACH 1's emergency room by paramedics (emergency medical services [EMS], persons trained to give emergency medical care to people who are injured or ill, typically in a setting outside of a hospital) on 7/25/2025. 2. On 7/31/2025 and 8/1/2025 the Licensed Nurses and Social Services Director (SSD) completed a reassessment of all current residents for elopement risk evaluation utilizing the facility's Point Click Care (PCC - a software system used in healthcare facilities, especially those dealing with long-term care, to manage patient information and daily operations) Elopement Risk Assessment Tool and no current residents are at risk for elopement. The Elopement Risk Assessment Tool covers 12 questions, including but not limited to history of elopement, wandering behavior, verbal expressions of a desire to go home, etc. Effective 8/1/2025, the facility will utilize the previous Elopement Risk Assessment that addresses the residents' cognition (the mental action or process of acquiring knowledge and understanding through thought, experience, and the senses), Activities of Daily Living (ADLs - refers to the basic self-care tasks that a person performs regularly to maintain their health and well-being), ambulation, and elopement history. 3. As of 7/31/2025, the Quality Assurance (QA) Consultant provided one-on-one in-service (an individual employee receives instruction and guidance from a trainer or mentor) training regarding Wandering and Elopement policy and Safety and Supervision of Resident policy emphasizing importance of resident monitoring to CNA 1, CNA 2, CNA 3, LVN 1, RN 1, and RN 2. 4. On 7/31/2025, the QA Consultant conducted one-on-one in-service regarding accurate documentation to CNA 1 and LVN 1. 5. As of 8/1/2025, the DON/DSD completed the in-service training to staff members regarding Wandering and Elopement policy and Safety and Supervision of Resident policy emphasizing importance of resident monitoring and the following topics: a. Licensed nurses assigned to all facility nursing stations, including station 1, station 2, and subacute station (refers to designated area within a facility that provides subacute care to residents who require more intensive medical services than those typically offered in standard long term care) will conduct rounds every two hours and document and sign off resident's presence or non-presence in the Residents Whereabouts Monitoring Log and indicate any unusual behaviors noted during the shift and endorse to RN supervisor accordingly. b. RN supervisors will utilize the Midnight Census (a PCC generated census after midnight, stating resident status including occupied or empty, to check off and verify resident's presence during shift-change, endorsement, or rounds. This document is signed off by an outgoing and incoming RN supervisor after the shift-change, endorsement or rounds. c. Develop and implement a person-centered care plan for elopement risk, including but not limited to frequent supervision. 6. As of 8/1/2025, all current active employees have completed the in-service training, with the exception of one RN and two LVNs who were unable to complete the in-service training due to being on medical leave. The DON/Designee will complete their in-services upon their return. 7. On 8/1/2025, the DON provided a written warning to LVN 1 and CNA 1 for inaccurate documentation on Resident 97's clinical records. Findings: 1.During a review of Resident 97’s admission Record (AR), the AR indicated the facility originally admitted Resident 97 on 4/3/2024 and readmitted the resident on 5/10/2024 with diagnoses including aphasia, dysphagia (difficulty swallowing), history of falling, anxiety (a feeling of unease, worry, or fear), and depression.
During a review of Resident 97’s Minimum Data Set (MDS – a resident assessment tool), dated 5/17/2025, the MDS indicated that Resident 97 was sometimes able to understand others and was sometimes understood by others.
During a review of Resident 97’s History and Physical (H&P – comprehensive assessment conducted by a healthcare provider that includes gathering a thorough medical history from the resident and performing a physical examination to assess their overall health and identify any potential medical concern), dated 5/22/2025, the H&P indicated Resident 97 did not have the capacity to understand and make decisions.
During a review of Resident 97’s Care Plan for aspiration (when something swallowed enters the airways or lungs), initiated on 5/16/2024 and revised on 3/12/2025, the care plan indicated Resident 97 is at risk for aspiration of food and liquids secondary to dysphagia. The care plan interventions included monitoring signs and symptoms of aspiration (such as choking [refers to the inability to breathe due to a blockage in the airway, typically caused by a foreign object lodged in the throat], shortness of breath [SOB], respiration changes), and resident’s tolerance of prescribed diet and fluid intake.
During a review of Resident 97’s Care Plan for self-care deficits, initiated on 7/29/2024, the care plan indicated Resident 97 required total assistance from staff with eating. The care plan intervention indicated to provide Resident 97 with a safe environment.
During a review of Resident 97’s Change of Condition (COC – when there is a sudden change in a resident’s condition) Interaction Assessment form, dated 1/29/2025, timed at 9 p.m., the COC form indicated Resident 97 eloped and fell in front of the facility. The nursing notes indicated that on 1/29/2025 at 9 p.m., Resident 97 was walking on the sidewalk in front of the facility and attempted to cross the street. The CNA and LVN were able to bring Resident 97 back to the facility and as Resident 97 was walking up the stairs, Resident 97 lost his footing and fell.
During a review of Resident 97’s Care Plan for elopement, initiated on 1/29/2025, the care plan indicated Resident 97 leaves the facility at times without authorization and permission. The care plan interventions included administering medications as ordered, notifying the physician and responsible party of the COC, and assisting Resident 97 to resident’s activities of choice.
During a review of Resident 97’s Elopement Evaluation, dated 5/18/2025, the Elopement Evaluation indicated Resident 97 had an elopement score of one (score value of one or higher indicates risk for elopement).
During a review of Resident 97’s Fall Risk Evaluation, dated 5/18/2025, the Fall Risk Evaluation indicated Resident 97’s fall risk score was seven (total score of 10 or greater indicates the resident should be considered as high risk for potential falls). The Fall Risk Evaluation indicated Resident 97 had balance problems while walking.
During a review of Resident 97’s Physician Orders, dated 5/19/2025, the Physician’s Orders indicated implementation of the falling star program, frequent visual monitoring due to the resident’s increased risk for falls and injury. The Physician’s Orders indicated to document per shift, every shift.
During a review of Resident 97’s Care Plan for falling star program, initiated on 5/19/2025, the care plan indicated Resident 97 was at risk for falls related to antihypertensive medication (medications used to treat high blood pressure), auditory (hearing) deficits, balance deficits, cognitive impairment, decreased strength and endurance, history of falls, noncompliant with request for assistance on use of call lights, poor safety awareness and judgment, unsteady gait (manner of walking), difficulty in walking, and muscle weakness. The care plan interventions indicated to remind staff during huddles (a brief, structured meeting, often daily, among healthcare professionals to discuss the day's plan, identify potential problems, and ensure smooth workflow) of the resident’s high fall risk status, implementing frequent visual monitoring, and placing the resident near the nursing station for closer observation.
During a review of Resident 97’s Physician’s Orders, dated 5/30/2025, the Physician’s Orders indicated monitoring resident’s blood pressure every six hours.
During a review of Resident 97’s Medication Administration Record (MAR - a daily documentation record used by a licensed nurse to document medications and treatments given to a resident) for 7/2025, the MAR for 7/25/2025 indicated the following:
- the monitoring for episodes of depression manifested by crying spells and tally by hashmark, was left blank for the day shift (7 a.m. to 3 p.m.)
- the Falling Star Program frequent visual monitoring (due to higher risk for falls and injuries) document per shift was left blank for the day shift.
- the blood pressure monitoring every six hours indicated a blood pressure of 110/62 mmHg at 12:53 p.m.
During a review of Resident 97’s Physician Orders, dated 7/9/2025, the Physician Orders indicated Controlled Carbohydrates (CCHO- meal plan where individuals aim to eat roughly the same amount of carbohydrates at each meal, helping to stabilize blood sugar levels) no added salt (NAS) diet, dysphagia mechanical soft (a diet that involves eating foods that have been modified to be easy to chew and swallow) texture, nectar mildly thick consistency (means the liquid is thicker than regular water but still pourable), three meals, aspiration precautions, and supervision during meals.
During a review of Resident 97’s ADL eating task, dated 7/25/2025, at 12:07 p.m., the ADL eating task indicated Resident 97 was provided with setup or clean up assistance (helper sets up or cleans up resident completes activity helper assists only prior or following the activity).
During a review of Resident 97’s nutritional task amount eaten %, dated 7/25/2025, at 12:07 p.m., the nutritional task amount eaten % indicated Resident 97 ate 50 % of his (Resident 97) meal.
During a review of Resident 97’s COC form, dated 7/25/2025, timed at 5:20 p.m., the COC form indicated Resident 97 eloped. The nursing notes indicated that on 7/25/2025 at 5 p.m., while passing dinner trays, CNA 2 observed that Resident 97 was not in his (Resident 97’s) assigned room. CNA 2 informed RN 2, who immediately initiated a thorough search of the facility. A code green (missing resident) was activated to alert all facility staff and initiate a coordinated facility wide search. The COC indicated that at approximately 6:30 p.m., RN 2 contacted the DON to report the incident, provide a timeline, and updates of the search effort. The COC form indicated that RN 2 then notified the local police department and reported Resident 97 as missing and requested assistance with the search. RN 2 contacted Resident 97’s family members to inform them of the situation and to verify whether they had seen or heard from Resident 97, neither family members reported recent contact with Resident 97.
During a review of Resident 97’s GACH 1 record, dated 7/25/2025, at 2:23 p.m., the GACH 1 record indicated Resident 97’s admission type was for trauma. GACH 1’s Medicine H&P notes indicated that Resident 97 was brought in by EMS from the community for possible ground level fall (refers to a fall where a person falls from a standing position onto a flat surface, such as the floor or ground). GACH 1’s records indicated Resident 97 had a cervical collar (a medical device that supports the neck and limits its movement) and was tearful, crying, and pointing at the ceiling. GACH 1’s records indicated Resident 97 had a small right frontal scalp contusion. GACH ‘s 1 records further indicated Resident 97 had a fall and aspiration precaution orders started on 7/25/2025.
During a concurrent interview and observation on 7/29/2025, at 2:20 p.m., with the Adm, the facility provided Close Circuit Television (CCTV - video surveillance technology) video footage of the camera located in the facility lobby, dated 7/25/2025, at 12:14 p.m., was reviewed. The Adm stated that the video footage shows a visitor opening the door leading to the lobby, after which Resident 97 is seen entering the lobby and subsequently exiting through the facility’s front door.
During a concurrent interview and record review on 7/30/2025 at 11:48 a.m., with CNA 1, Resident 97’s nutritional task amount eaten %, dated 7/25/2025, timed at 12:07 p.m., was reviewed. CNA 1 stated she was not aware that Resident 97 had a Physician’s Order for supervision during all meals. CNA 1 stated that she (CNA 1) does not supervise Resident 97 during mealtimes and leaves the meal tray on Resident 97’s bedside table. CNA 1 stated that she was assigned to Resident 97 on 7/25/2025 and that the last time she (CNA 1) saw Resident 97 that day (7/25/2025) was between approximately 11:15 a.m. and 11:20 a.m. CNA 1 stated that prior to lunch, Resident 97 was in his (Resident 97) room. CNA 1 stated that she delivered Resident 97’s lunch tray and placed it on his (Resident 97) bedside table. CNA 1 stated Resident 97 was independent in using the bathroom. CNA 1 stated that she (CNA 1) observed that the bathroom door was closed and assumed Resident 97 was inside. CNA 1 stated that when she (CNA 1) returned sometime after 1:00 p.m. to retrieve the meal tray, CNA 1 observed the food had not been touched and the bathroom door remained closed. CNA 1 stated that she (CNA 1) did not knock on or open the bathroom door to verify Resident 97’s presence. CNA 1 reviewed Resident 97’s nutritional amount eaten % document and stated that she (CNA 1) documented a nutritional intake of 50% on 7/25/2025, despite knowing that Resident 97 had not eaten.
During a concurrent interview and record review on 7/30/2025, at 1:29 p.m., with LVN 1, Resident 97’s MAR dated 7/25/2025 was reviewed. LVN 1 stated that he was the nurse assigned to Resident 97 on 7/25/2025 during the 7 a.m. to 3 p.m. shift. LVN 1 stated he checked Resident 97’s blood sugar between 11 a.m. and 12 p.m., prior to lunch. LVN 1 stated that while he (LVN 1) checks on residents periodically, he did not check on Resident 97 again that day (7/25/2025) because Resident 97 is ambulatory (able to walk and move around) and typically seeks out staff when assistance is needed. LVN 1 also stated that Resident 97 becomes emotional when family visits, often crying and clinging to them, while expressing a desire to go home. LVN 1 stated that during shift-change, he (LVN 1) is informed about which residents are at risk for elopement. LVN 1 stated that Resident 97 is not considered an elopement risk and has never previously eloped. LVN 1 also stated that he (LVN 1) was not aware of Resident 97’s elopement incident on 1/29/2025. LVN 1 stated that the BP documented at 12:00 p.m. was taken at 8:00 a.m. LVN 1 stated that he did not check Resident 97’s BP every six hours as ordered. LVN 1 stated that failing to check Resident 97’s BP as ordered could result in unrecognized high or low BP readings potentially leading to delays in necessary interventions and treatment.
During an interview on 7/30/2025 at 2:13 p.m., with RN 1, RN 1 stated she (RN 1) was not initially aware that Resident 97 was an elopement risk but was later informed that Resident 97 had previously attempted to elope. RN 1 stated that the last time she (RN 1) saw Resident 97 on 7/25/2025 was around 12:00 p.m., when Resident 97 was observed walking near the nurses’ station by the intravenous (IV – within a vein) cart.
During an interview on 7/30/2025 at 3:00 p.m., with CNA 2, CNA 2 stated that upon starting her shift (3:00 p.m. to 11:00 p.m.), she (CNA 2) receives verbal hand off from the previous CNA 2 at the nurses’ station. CNA 2 stated that the hand off includes information about residents who are out on pass or have appointments. CNA 2 stated that she worked on 7/25/2025 at 3:00 p.m. CNA 2 further stated that during her (CNA 2) initial rounds, she (CNA 2) did not see Resident 97. CNA 2 stated that not seeing Resident 97 at that time did not raise concern, as Resident 97 frequently walks around and attends activities. CNA 2 stated that on 7/25/2025 at around 5:00 p.m., during dinner time, she (CNA 2) informed RN 2 that she (CNA 2) was unable to locate Resident 97. CNA 2 stated facility staff then conducted a search for Resident 97 inside the facility approximately 30 minutes but were unable to locate Resident 97. CNA 2 stated that facility staff searched for Resident 97 outside the facility, both on foot and by car, for approximately one hour. CNA 2 stated she (CNA 2) was not aware that Resident 97 was an elopement risk.
During an interview on 7/30/2025 at 4:18 p.m., with RN 2, RN 2 stated Resident 97 is alert and oriented to self with confusion and walks around the facility without assistive devices (tools, products, or equipment that can help an individual perform tasks and activities). RN 2 stated that Resident 97 had been crying and pointing at the door since the previous week, because he (Resident 97) wanted to go home. RN 2 stated he (RN 2) worked the 3 p.m. to 11 p.m. shift on 7/25/2025. RN 2 stated that during the hand off process, RNs begin by doing rounds, which involve standing outside residents’ rooms rather than entering. RN 2 stated that the hand off report includes any COC. RN 2 stated that during the 7/25/2025 report, RN 1 did not report any concerns regarding Resident 97. RN 2 stated that between 5 p.m. to 5:20 p.m., while CNAs were distributing dinner trays, CNA 2 informed RN 2 that she (CNA 2) had not seen Resident 97. RN 2 stated the facility staff conducted a search, and at 5:30 p.m., a “Code Green” was called to indicate a missing resident. RN 2 stated that he (RN 2) helped search the facility for approximately 20 minutes, then went outside around 6:00 p.m. to continue the search for about an hour. RN 2 stated he (RN 2) called the DON at approximately 6:30 p.m. to inform the DON that Resident 97 was missing. RN 2 also stated that another staff member contacted the local law enforcement (LLE). RN 2 stated that Resident 97 was not identified as an elopement risk, had never previously attempted to exit the facility, and that he (RN 2) was unaware Resident 97 had eloped back in 1/29/2025.
During an interview on 7/31/2025 at 8:34 a.m., with CNA 1, CNA 1 stated that Resident 97 had never previously attempted to leave the facility. CNA 1 stated that she (CNA 1) was not aware that Resident 97 had eloped on 1/29/2025. CNA 1 stated Resident 97 would often point toward the outside, and when CNA 1 asked if he (Resident 97) wanted to go with his (Resident 97) sister, Resident 97 would nod “yes”. CNA 1 stated that Resident 97 had attempted to open the lobby door, but was unable to open it, and that the activity personnel would catch him and redirect him at those times. CNA 1 stated that CNAs do not provide hand off reports to each other because the nurses on the oncoming shift inform the CNAs about any important updates regarding the residents. CNA 1 stated CNAs receive a generalized report at the nurses’ station rather than individualized information about each resident. CNA 1 stated that on 7/25/2025, she (CNA 1) did not remove the cover from Resident 97’s meal tray and assumed Resident 97 was in the bathroom at the time. CNA 1 stated that she did not supervise Resident 97 during lunch on that day (7/25/2025) and was unaware that Resident 97 had an order requiring supervision during meals. CNA 1 stated she usually documents breakfast intake around 11:00 a.m. and lunch intake at 2:00 p.m. CNA 1 stated that on 7/25/2025 she (CNA 1) documented Resident 97’s lunch intake at 12:07 p.m. because she had time and wanted to complete her documentation early. CNA 1 stated Resident 97 did not finish lunch, but she (CNA 1) had not visually checked Resident 97’s meal tray at 12:07 p.m. CNA 1 stated that because she (CNA 1) did not visually check the meal tray, she (CNA 1) did not catch that Resident 97 was missing. CNA 1 stated because she was not aware of the required supervision order during meals, she was unable to provide the necessary supervision for Resident 97. CNA 1 further stated that if she had been supervising Resident 97 during lunch, Resident 97 would not have been able to leave the facility.
During an interview on 7/31/2025 at 10:10 a.m., with Family Member (FM) 1, FM 1 stated that she visited GACH 1 on 7/29/2025 to see Resident 97. FM 1 stated that Resident 97 was traumatized, became emotional and restless, and was hysterical and crying for approximately 10 minutes. FM 1 stated that Resident 97 had a “bump” on his forehead and believed Resident 97 must have fallen. FM 1 stated that someone found Resident 97 on the floor and called 911.
During a concurrent interview and record review on 7/31/2025 at 12:19 p.m., with the DON, Resident 97’s care plan for elopement, initiated on 1/29/2025 and Physician’s Orders dated 5/19/2025 were reviewed. The DON stated that Resident 97 eloped on 7/25/2025. The DON stated staff became aware of Resident 97’s elopement on 7/25/2025 at around 5:00 p.m., she (DON) was informed around 6:00 p.m., and LLE was notified around 6:30 p.m. The DON stated Resident 97 was identified as an elopement risk and had a previous elopement incident on 1/29/2025, during which Resident 97 attempted to cross the street in front of the facility. The DON stated that the interventions for residents at risk for elopement included: visual checks, distraction techniques, contacting family members for support, psychiatric evaluations (a comprehensive assessment of an individual's mental health, conducted by a mental health professional to identify potential mental health disorders, determine the severity of symptoms, and develop appropriate treatment plans) if indicated and monitoring prescribed medications. The DON stated that the most critical intervention is direct visualization of the resident. The DON further stated that the elopement care plan initiated for Resident 97 on 1/29/2025 was not person-centered and did not include specific interventions tailored to Resident 97’s needs, such as visual checks and supervision. The DON stated that the care plan should be individualized, especially given the potential for re-elopement and the associated risk of harm. The DON further stated that Resident 97 was at risk for aspiration and required supervision while eating. The DON stated that if staff (CNA 1) had not simply left the meal tray on 7/25/2025 during lunchtime and had supervised Resident 97, CNA 1 would have noticed Resident 97 was missing at that time. The DON stated that Resident 97 had an order for Falling Star Program, which requires visualization of the resident at the end of each shift. The DON stated that if LVN 1 had completed the Falling Star visualization at 3:00 p.m., LVN 1 would have noticed the resident was missing. The DON stated that LVN 1 did not perform the required visual check on 7/25/2025 at 3:00 p.m., which contributed to a delay in identifying that Resident 97 was missing. The DON further stated that LVN 1 used the BP reading taken at 8:00 a.m. to document the 12:00 p.m. BP check rather than taking a new BP reading as ordered. The DON stated that if LVN 1 had taken Resident 97’s BP as scheduled at 12:00 p.m., LVN 1 would have discovered Resident 97 was missing at that time, allowing for an earlier response. The DON stated that the hand off report during shift change is conducted from RN to RN, and that the oncoming RN is expected to physically enter each resident’s room to visually check on the residents. The DON stated that RN 1 was assigned as Resident 97’s nurse during the 7:00 a.m. to 3:00 p.m. shift, while RN 2 was assigned to the medication cart for medication pass (the process of administering medications to residents in a facility, ensuring each dose is given correctly and safely). The DON stated no formal hand off report was given to RN 2 regarding Resident 97. The DON stated that CNAs do not conduct formal hand off reports. Instead, any special endorsements or important information are communicated to the licensed nurses, who are then responsible for endorsing the information to the oncoming CNAs. The DON further stated that if staff had conducted a proper
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to honor the resident's right to be informed in advance by the physici...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to honor the resident's right to be informed in advance by the physician or other practitioner or professional, of the risks and benefits of proposed care, treatment and treatment alternative or options for two of five sampled residents (Residents 100 and 112) reviewed for unnecessary medications by failing to ensure: 1. Resident 1's Depakote (it helps manage manic or mixed episodes [periods of high energy, irritability, or both] in adults with bipolar disorder) indicated the correct preparation/form on the consent form. This deficient practice violated the residents' right to make an informed decision regarding the use of psychoactive medications (substances that, when taken in or administered into one's system, affect mental processes, e.g. perception, consciousness, cognition or mood and emotions). 2. Resident 112's trazodone (a medication used to treat mental illness) and citalopram (a medication used to treat mental illness) had an informed consent (a process during which residents or caregivers are educated regarding the potential risks and benefits of medication therapy) from the resident or their responsible party (RP - a person delegated to make medical decisions for the resident in the event they are unable to do so) prior to treatment. The deficient practice had the potential to result in preventing Resident 112 or his RP from exercising their right to decline treatment with psychotropic medications. This increased the risk that Resident 112 could have experienced adverse effects (unwanted, uncomfortable, or dangerous effects that a drug may have) related to psychotropic medications leading to impairment or decline in his mental or physical condition or functional or psychosocial status. Findings: 1. During a review of Resident 100’s admission Record, the admission Record indicated the facility admitted the resident on 3/18/2023, with diagnoses including Alzheimer’s disease (a disease characterized by a progressive decline in mental abilities), dementia (a progressive state of decline in mental abilities), and mood disorder (a mental health condition that primarily affects the emotional state).
During a review of Resident 100’s Informed Consent, dated 3/18/2023, the Informed Consent indicated Depakene Oral Solution. Give 125 mg via gastrostomy tube (gt, a tube inserted through the abdomen directly into the stomach) three times a day (TID) for mood disorder monitor for behavior (m/b) uncontrollable extreme mood swing causing exhaustion.
During a review of Resident 100’s Order Summary Report, dated 5/30/2025, the Order Summary Report indicated an order for Depakote Oral Tablet Delayed Release 125 milligrams (mg, a unit of weight) (Divalproex Sodium). Give 1 tablet by mouth at bedtime for Mood disorder (Informed consent obtained from resident representative (RP) after explanation of risks and benefits and verified with MD).
During a review of Resident 100’s Minimum Data Set (MDS, a resident assessment tool), dated 7/2/2025, the MDS indicated the resident rarely to never had the ability to make self-understood and understand others and had severely impaired cognition (refers to a significant decline in a person's mental abilities that noticeably affects their daily life).
During a concurrent interview and record review on 7/30/2025, with Licensed Vocational Nurse (LVN) 5, Resident 100’s Depakene Informed Consent was reviewed. LVN 5 stated the consent written was different from the Physician’s Order. LVN 5 stated the order indicated a tablet preparation of the medication, but the consent was for oral solution. LVN 5 stated the staff should have obtained another consent as the preparation was not as ordered and the order was written after the 3/18/2023 consent in the chart.
During an interview on 7/30/2025, at 9 a.m., with LVN 6, LVN 6 stated he administered the medication Depakote to Resident 100 and he gave a tablet form this morning. LVN 6 stated he crushed the medications and administered them via gt. LVN 6 stated the consent was not accurate and they should have obtained a new consent from the family member or resident to honor their right to informed consent.
During an interview on 7/31/2025, at 12:43 p.m., with Registered Nurse (RN) 3, reviewed Resident 100’s Order Summary Report, Medication Administration Record (MAR), and Informed Consent. RN 3 stated they should have obtained a new informed consent for Depakote as it was reordered in a different form or preparation. RN 3 stated the failure of the staff to obtain a new consent has predisposed the resident to the adverse effect (an undesired effect of a drug or other type of treatment, such as surgery) of the medication that could lead to medication errors.
During a review of the facility's recent policy and procedure (P&P) titled, Administering Medications, last reviewed on 4/24/2025, the P&P indicated medications are administered in a safe and timely manner, and as prescribed.
During a review of the facility's recent P&P titled, Psychotropic Medication Use, last reviewed on 4/24/2025, the P&P indicated a psychotropic drug is any medication that affects brain activities associated with mental processes and behavior, which includes but is not limited to antipsychotics, anxiolytics, hypnotics and antidepressants. It is the responsibility of the attending health care practitioner to inform the resident and/or resident representative of the initiation, reason for use, and the risks associated with the use of psychotropic medications, per facility policy and applicable state regulation. The informed consent will be obtained by the Prescriber prior to initiation of the psychotropic medication. The Facility shall verify informed consent prior to the administration of a psychotropic medication for a resident.
During a review of the facility's recent P&P titled, Charting and Documentation, last reviewed on 4/24/205, the P&P indicated documentation in the medical record will be objective (not opinionated or speculative), complete, and accurate.
2. During a review of Resident 112’s admission Record (a record containing diagnostic and demographic resident information), the admission Record indicated he was admitted to the facility on [DATE] with diagnoses including insomnia (difficulty sleeping) and depression (a mental illness characterized by depressed mood, lack of energy, difficulty sleeping, and lack of interest in usually enjoyable activities.)
During a review of Resident 112’s History and Physical (a record of a physician’s comprehensive medical examination), dated 7/15/25, the History and Physical indicated the resident “has fluctuating capacity” to understand and make medical decisions and indicated Resident 112’s sister served as his RP.
During a review of Resident 112’s Order Summary Report (a summary of all active physician’s orders), dated 7/31/25, the order summary report indicated he was receiving the following psychotropic medications:
1. Citalopram 20 milligrams (mg – a unit of measure for mass) via gastrostomy tube (g-tube – a tube surgically implanted into the stomach for the administration of medication and nutrition) one time a day for depression to start on 7/16/25.
2. Trazodone 50 mg via g-tube at bedtime for insomnia to start on 7/16/25.
During a review of Resident 112’s available informed consent documentation for citalopram and trazodone, dated 7/22/25, and clinical record, the available informed consent documentation and clinical record indicated there was no documentation that Resident 112 or any responsible party received education from the prescriber regarding the risks and benefits of trazodone or citalopram prior to their administration.
During a telephone interview on 7/31/2025 at 10:49 AM with Resident 112's sister and RP (FM 2), FM 2 stated no one from the facility called to obtain permission to use trazodone or citalopram on 7/22/25 or any other date. FM 2 stated the only time she heard of these medications was when Resident 112 was still in the hospital prior to his admission to the facility. FM 2 stated no one from the facility called her to discuss risks or benefits of the medication or gave her the option to opt out prior to them being administered.
During an interview on 7/31/2025 at 11:03 AM with the Director of Nursing (DON), the DON stated informed consent for psychotropic medications must occur before the initiation of psychotropic medications. The DON stated the process of informed consent must be between the prescriber and the resident or the resident's representative to answer any questions or concerns related to the use of psychotropic medication and the risks versus benefits. The DON stated this is done to ensure the residents or their representatives can exercise their right to opt out of treatment prior to the medications being initiated. The DON stated the facility failed to obtain informed consent from Resident 112's RP prior to initiation of psychotropic therapy with citalopram and trazodone. The DON stated the informed consent documentation is incomplete and there is no other record that the prescriber provided education regarding the risks and benefits of these medications to the RP prior to their initiation. The DON stated this increased the risk that Resident 112 may experience adverse effects such as drowsiness or dizziness due to the adverse effects of the medication which could possibly lead to a decline in quality of life.
During a review of the facility’s P&P titled “Psychotropic Medication Use,” revised June 2021, the P&P indicated “It is the responsibility of the attending health care practitioner to inform the resident and/or resident representative of the initiation, reason for use, and the risk associated with the use of psychotropic medication, per facility policy or applicable state regulation. The informed consent will be obtained by the Prescriber prior to initiation of the psychotropic medication…”
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0574
(Tag F0574)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure that the residents were informed of their right to file a complaint with the State Survey Agency and certification age...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to ensure that the residents were informed of their right to file a complaint with the State Survey Agency and certification agency (a health and safety inspector for places that provide healthcare, like hospitals and nursing homes) and that the State Survey Agency name, address and telephone number was visible and readable for four of five sampled residents (Resident 21, 23, 51, and 90) reviewed under the Resident Council task. This deficient practice had the potential to deprive the residents of assistance from resident advocacy groups should unresolved issues arise in the facility. Findings: During a concurrent observation and interview during a Resident Council meeting on 7/30/2025 at 2:12 p.m. inside the resident activity room, observed there was no State Survey Agency contact information posted. Four of five residents (Resident 21, 23, 51, and 90) who attended the Resident Council meeting stated they did not know where the contact information for the State Survey Agency was posted and that they were not made aware of where they could find the information. During a concurrent observation and interview on 7/30/2025 at 2:55 p.m., in front of the facility information board on the hallway close to the activity room, with the Activity Director (AD), observed a standard-sized white printer paper was posted with the contact information for the Stated Survey Agency in standard-sized letters. The AD stated the State Survey Agency name, address, and telephone number were small and that the residents would not be able to read the letters easily. The AD stated the address and telephone number indicated in the paper was incorrect. The AD stated the contact information for the State Survey Agency should have been posted in a way that the residents and/or resident representatives can easily read to be able to contact the State Survey Agency if the residents and/or their representatives want to file a complaint directly. The AD stated the facility should have provided the State Survey Agency contact information during the monthly council meeting with the residents. The AD stated it was important for the residents to be aware of the contact information for the State Survey Agency so they can directly file a complaint to the State Survey Agency to address their issues or concerns regarding the care the residents are getting in the facility. During a concurrent observation and interview on 7/30/2025 at 3:05 p.m. in front of the facility information board on the hallway close to the activity room, with the Director of Nursing (DON), the DON stated the contact information for the State Survey Agency was not visible and easily readable for the residents and/or resident representatives. The DON stated the address and telephone number for the State Survey Agency were not updated. The DON stated that the State Survey Agency contact information, including address and telephone number, should be correct for the residents and/or their representatives to file a complaint with the State Survey Agency if they are not happy with the care the residents received in the facility. The DON stated the residents' right to file a complaint with the State was not honored. During a review of the facility's policy and procedure (P&P) titled, Resident's Rights, last reviewed 4/24/2025, the P&P indicated: - Federal and state laws guarantee certain basic rights to all residents in the facility. These rights include the residents' right to: j. Be informed about his or her rights and responsibilities x. Communicate with outside agencies (such as local, state, or federal officials, state and federal surveyors, state long-term care ombudsman, protection or advocacy organizations) regarding any matter.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide a safe and sanitary homelike environment for ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide a safe and sanitary homelike environment for two of seven sampled residents (Resident 1 and 36) reviewed under the Environment task area by failing to ensure the trashcan lid in the bathroom was clean and did not have brown stains and a yellow substance on the lid. This deficient practice had the potential to negatively affect the residents' physical and psychosocial wellbeing and make the residents feel uncomfortable in their living space. Cross Reference F880 Findings:a. During a review of Resident 1's admission Record (AR), the AR indicated the facility admitted the resident on 5/12/2022 and most recently admitted the resident on 2/15/2025 with diagnoses that included acute and chronic respiratory failure (a serious condition that occurs suddenly when the lungs cannot get enough oxygen), tracheostomy (opening surgically created through the front of the neck and into the trachea [windpipe]), dependence on respiratory ventilator (a medical device to help support or replace breathing), muscle weakness, and need for assistance with personal care. During a review of Resident 1's Minimum Data Set (MDS - resident assessment tool), dated 5/18/2025, the MDS indicated the resident was totally dependent on staff for mobility, dressing, bathing, toilet hygiene, and personal hygiene. During a review of Resident 1's History and Physical (H&P), dated 2/16/2025, the H&P indicated the resident was nonverbal but was awake, alert, able to respond yes/no appropriately to questions, and was able to move all extremities. The H&P further indicated the resident was able to understand and make decisions. During a review of Resident 1's Care Plan (CP) regarding risk for infection, last reviewed 6/6/2025, the CP indicated the resident was a high risk for infection with a goal to minimize and reduce the risks with interventions including cleaning and disinfection of equipment as needed. b. During a review of Resident 36's AR, the AR indicated the facility admitted the resident on 6/3/2015 and most recently admitted the resident on 7/15/2025 with diagnoses that included chronic respiratory failure, tracheostomy, dependence on respiratory ventilator, and urinary tract infection (UTI- an infection in the bladder/urinary tract). During a review of Resident 36's MDS, dated [DATE], the MDS indicated the resident was totally dependent on staff for mobility, dressing, bathing, toilet hygiene, and personal hygiene. During a review of Resident 36's H&P, dated 1/15/2024, the H&P indicated the resident did not have the capacity to understand and make decisions. During a review of Resident 36's CP regarding risk for infection, initiated 7/16/2025 and last reviewed 7/25/2025, the CP indicated the resident was at risk for infection due to the use of an indwelling catheter (a flexible tube placed in the bladder to drain urine) with a goal that the resident would be free from infection / UTI. During an observation on 7/29/2025 at 11:20 a.m., observed Residents 36 and 1 awake and lying in their beds in their shared room. Observed Family Member (FM) 1 of Resident 36 sitting at Resident 36's bedside. Observed in the shared restroom a beige colored trashcan with a lid that was covered in brown stains and a yellow substance. During an interview on 7/29/2025 at 11:40 a.m. with Certified Nursing Assistant (CNA) 5, CNA 5 stated CNA 5 was covering while CNA 6 was on break. CNA 5 entered Residents 36 and 1s' shared restroom and stated the trash can looked old and stained. CNA 5 stated that CNA 5 would not want a trash can like that in CNA 5's house. During an interview on 7/29/2025 at 11:59 a.m. with CNA 6, CNA 6 stated CNA 6 did not know what was on Residents 36 and 1s' trash can lid, but the lid did not always look brown. CNA 6 stated CNA 6 worked on 7/28/2025 and the trashcan lid was not brown. CNA 6 stated CNA 6 did not report to maintenance or housekeeping that the trash can lid was brown. During an interview on 7/29/2025 at 12:05 p.m. with FM 1, FM 1 stated Residents 36 and 1s' trash can lid had been brown since 7/28/2025, but the lid did not always look that way. FM 1 did not respond when the surveyor asked how FM 1 felt about the trash can lid. During an interview on 7/31/2025 at 2 p.m. with Housekeeper (HSK) 1, HSK 1 stated on 7/30/2025 the Housekeeping Director (HSKD) told HSK 1 to change Residents 36 and 1s' trash can, because it was no good. During an interview on 7/31/2025 at 2:10 p.m. with the HSKD, the HSKD stated Residents 36 and 1s' trash can looked dirty and it should not have been in the residents' bathroom. The HSKD stated it looked like somebody tried to clean the trash can lid, but they were not successful. The HSKD stated any staff that used the trash can should have reported that it looked dirty, but they did not. The HSKD stated a dirty trash can should not be in a resident's room because it looked dirty and is not nice for an inside environment. During a concurrent interview and record review on 8/1/2025 at 8:58 a.m. with the Infection Preventionist (IP), the IP reviewed the facility policy and procedure (P&P) regarding infection control, homelike environment, and reviewed a photo of Residents 36 and 1s' trash can lid from 7/29/2025. The IP stated the trashcan lid looked filthy and there were yellow areas that appeared to be feces. The IP stated any nurse, or housekeeper should have reported the trashcan, but they did not. The IP stated a dirty trashcan, with possible feces on it, should not be in a resident's room because there is a potential for cross contamination resulting in infection in the residents with e coli (a bacterium that is commonly found in the gut of humans that can cause infections). The IP stated the facility P&P regarding infection control and homelike environment was not followed because the trashcan was not sanitary. During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the Assistant Director of Nursing (ADON), the ADON reviewed the facility P&P regarding infection control, homelike environment, and reviewed a photo of Residents 36 and 1s' trashcan lid from 7/29/2025. The ADON stated the facility P&Ps were not followed when the trashcan did not look clean and could potentially lead to infections in residents. During a review of the untitled facility P&P regarding Housekeeping, last reviewed 4/24/2025, the P&P indicated in order to ensure the health and safety of residents, staff and visitors, it is critical that the facility be kept clean, sanitary, and in good repair at all times. Proper and safe methods for cleaning, disinfecting, and sterilizing all areas, surfaces, and equipment shall be employed in the facility as required by law. All rooms of the facility shall be kept clean and as free as possible of germs and other contaminating agents at all times, while maintaining a pleasant and home-like atmosphere for the residents. The facility shall acquire and properly maintain all necessary housekeeping equipment to ensure the proper cleaning of the facility. General duties of the housekeeping staff are to make sure that each room, area, piece of furniture, or equipment is cleaned properly and thoroughly with the correct equipment and cleaning product. During a review of the facility P&P titled, Homelike Environment, last reviewed 4/24/2025, the P&P indicated residents are provided with a safe, clean, comfortable and homelike environment and encouraged to use their personal belongings to the extent possible.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to report incidents of elopements (the act of leaving a facility unsupervised and without prior authorization) in a timely manner per the faci...
Read full inspector narrative →
Based on interview and record review, the facility failed to report incidents of elopements (the act of leaving a facility unsupervised and without prior authorization) in a timely manner per the facility's policy and procedure (P&P) for one of one sampled resident (Resident 97) when: 1.Resident 97 eloped on 1/29/2025 at 9 p.m. 2.Resident 97 eloped on 7/25/2025 at 5 p.m. This deficient practice resulted in a delay in an investigation by the State Agency (SA) and had the potential to negatively affect the safety of residents in the facility. Cross reference F689 Findings: During a review of Resident 97's admission Record (AR), the AR indicated the facility originally admitted Resident 97 on 4/3/2024 and readmitted the resident on 5/10/2024 with diagnoses including aphasia (difficulty speaking), dysphagia (difficulty swallowing), history of falling, anxiety (a feeling of unease, worry, or fear), and depression (a mental health condition that makes you feel persistently sad and lose interest in things you usually enjoy). During a review of Resident 97's Minimum Data Set (MDS - a resident assessment tool), dated 5/17/2025, the MDS indicated that Resident 97 was sometimes able to understand others and was sometimes understood by others. During a review of Resident 97's History and Physical (H&P - comprehensive assessment conducted by a healthcare provider that includes gathering a thorough medical history from the resident and performing a physical examination to assess their overall health and identify any potential medical concern), dated 5/22/2025, the H&P indicated Resident 97 did not have the capacity to understand and make decisions. During a review of Resident 97's Change of Condition (COC - when there is a sudden change in a resident's condition) Interaction Assessment form, dated 1/29/2025, timed at 9 p.m., the COC form indicated Resident 97 eloped and fell in front of the facility. The nursing notes indicated that on 1/29/2025 at 9 p.m., Resident 97 was walking on the sidewalk in front of the facility and attempted to cross the street. The Certified Nursing Assistant (CNA) and Licensed Vocational Nurse (LVN) were able to bring Resident 97 back to the facility and as Resident 97 was walking up the stairs, Resident 97 lost his footing and fell. During a review of Resident 97's COC form, dated 7/25/2025, timed at 5:20 p.m., the COC form indicated Resident 97 eloped. The nursing notes indicated that on 7/25/2025 at 5 p.m., while passing dinner trays, CNA 2 observed that Resident 97 was not in his (Resident 97's) assigned room. CNA 2 informed Registered Nurse (RN) 2, who immediately initiated a thorough search of the facility. A code green (missing resident) was activated to alert all facility staff and initiate a coordinated facility wide search. The COC indicated that at approximately 6:30 p.m., RN 2 contacted the Director of Nursing (DON) to report the incident, provide a timeline, and updates of the search effort. The COC form indicated that RN 2 then notified the local police department and reported Resident 97 as missing and requested assistance with the search. RN 2 contacted Resident 97's family members to inform them of the situation and to verify whether they had seen or heard from Resident 97, neither family members reported recent contact with Resident 97. During a review of the facility's Transmission Verification Report, the Transmission Verification Report indicated the report titled, RE: Report of a missing resident [Resident 97], was faxed over to the SA on 7/28/2025 at 5:42 a.m. During a concurrent interview and record review on 7/29/2025, at 2:20 p.m., with the Administrator (Adm), the facility provided Close Circuit Television (CCTV - video surveillance technology) video footage of the camera located in the facility lobby, dated 7/25/2025, at 12:14 p.m., was reviewed. The Adm stated that the video footage shows a visitor opening the door leading to the lobby, after which Resident 97 is seen entering the lobby and subsequently exiting through the facility's front door. The Adm stated he (Adm) was informed of Resident 97's elopement on 7/25/2025 at 6 p.m. by the DON. The Adm stated he (Adm) arrived at the facility at 7:30 p.m. and did another search for Resident 97 and called the local police around 8 p.m. The Adm stated he (Adm) was the one who reported Resident 97's elopement to the SA via fax on 7/28/2025. The Adm stated there were no calls made to the SA prior, and the initial reporting was via fax on 7/28/2025. During an interview on 7/31/2025 at 12:19 p.m. with the DON, the DON stated Resident 97 had an elopement on 1/29/2025 at 9 p.m. when Resident 97 was found at the sidewalk in front of the facility attempting to cross the street. The DON stated the facility did not report Resident 97's elopement on 1/29/2025 to the SA and based on the facility's unusual occurrence policy, the facility should have reported to the incident to the SA. The DON stated the incident should have been reported to the SA as soon as the DON and Adm were made aware. The DON stated unusual occurrences must be reported to SA within 24 hours. The DON stated Resident 97 eloped on 7/25/2025 and when she asked the Adm, the Adm informed the DON that he (Adm) reported the incident to the SA on Monday (7/28/2025). The DON stated there was a delay in reporting of three days. The DON stated the potential for not reporting elopement can be that there can be possible harm to the residents. During a review of the facility's policy and P&P titled, Unusual Occurrence Reporting, last reviewed on 4/24/2025, the P&P indicated as required by federal or state regulation, our facility reports unusual occurrences or other reportable events which affect the health, safety, or welfare of our residents, employees or visitors. h. other occurrences that interfere with facility operations and affect the welfare, safety, or health of residents, employees or visitors. 2. Unusual occurrences shall be reported via telephone to appropriate agencies as required by current law and or regulations within twenty-four (24) hours of such incident or as otherwise required by federal and state regulations. 3. A written report detailing the incident action taken by the facility after the event shall be sent or delivered to the state agency within forty-eight (48) hours of reporting the event or as required by federal and state regulations.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the comprehensive care plan is reviewed and re...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the comprehensive care plan is reviewed and revised by an interdisciplinary team for two of three sampled residents (Residents 5 and 103) reviewed for physical restraint (the use of a manual hold to restrict freedom of movement of all or part of a person's body, or to restrict normal access to the person's body, and that is used as a behavioral restraint) use by failing to update the care plan on the use of tab alarm (is a device designed to alert caregivers when a patient or resident is attempting to get out of bed or a chair, potentially preventing falls). The deficient practice had the potential for delay of necessary care and services to residents. Findings:1.During a review of Resident 5's admission Record, the admission Record indicated the facility admitted the resident on 12/31/2024, and readmitted the resident on 3/27/2025, with diagnoses including difficulty in walking, muscle weakness, and disorders of bone density (is how closely packed and full those spaces are within the bones) and structure. During a review of Resident 5's Minimum Data Set (MDS, a resident assessment tool), dated 7/10/2025, the MDS indicated the resident had the ability to make self-understood and understand others and had severe cognitive impairment (a significant decline in cognitive abilities, impacting daily life and independence). The MDS indicated that the resident required substantial assistance on mobility and activities of daily living (ADLs, activities such as bathing, dressing and toileting a person performs daily). The MDS indicated that the resident had a bed alarm (a pad with sensors that will alarm when a resident stands up unassisted to help prevent falls by alerting staff). During a review of Resident 5's Order Summary Report, dated 7/21/2025, the Order Summary Report indicated an order to apply tab alarm when in bed and wheelchair to alert/remind resident to ask for assistance when transferring or ambulating. Monitor for placement and functioning. (Informed consent obtained by MD from responsible party [RP] after explanation of risks and benefit verified with MD). Every shift. During a review of Resident 5's Fall Risk Evaluation, dated 7/10/2025, the Fall Risk Evaluation indicated the resident was at a moderate risk for fall. During a review of Resident 5's Care Plan (CP) Report titled Resident requires sensor pad alarm when in bed due to spontaneous act/behavior of trying to get up unassisted, last revised on 2/21/2025, the CP Report indicated an intervention to apply sensor pad alarm as ordered. During an observation and interview on 7/31/2025, at 9:41 a.m., with Certified Nursing Assistant (CNA) 9, inside Resident 5's room, observed Resident 5 in bed with a tab alarm on. CNA 9 stated they use the tab alarm to prevent the resident from falling out of bed because the resident does not ask for assistance when he gets out of bed. During an interview and record review on 7/31/2025, at 12:12 p.m., with Registered Nurse (RN) 3, reviewed Resident 5's Order Summary Report, Fall Risk Evaluation, and Care Plan. RN 3 stated Resident 5's tab alarm is a restraint because it prevents the resident from getting out of bed freely. RN 3 stated the care plan indicated the resident was using a pad alarm, however, the order from 7/21/2025 was a tab alarm. RN 3 stated the licensed staff should have updated the care plan to tab alarm and other interventions should have been reviewed and updated as needed. RN 3 stated the failure of the licensed staff to update the care plan had the potential for delay in care and services and miscommunication with healthcare providers providing direct care to the resident. During an interview on 8/1/2025, at 2:05 p.m., with the Assistant Director of Nursing (ADON), the ADON stated the staff should have updated the care plan on the use of tab alarm on Resident 5 to ensure the care and services were relevant and delivered timely. The ADON stated an updated care plan provides a standardized care to residents and helps healthcare providers provide high quality care to residents. 2.During a review of Resident 103's admission Record, the admission Record indicated the facility admitted the resident on 10/30/2024, with diagnoses including difficulty in walking, age-related nuclear cataract, bilateral (a type of cataract that develops in the center (nucleus) of the eye's lens, causing it to cloud over due to the natural aging process), and need for assistance with personal care. During a review of Resident 103's MDS, dated [DATE], the MDS indicated the resident sometimes had the ability to make self-understood and understand others and had short- and long-term memory problem. The MDS indicated the resident was dependent to requiring supervision on mobility and ADLs. The MDS indicated the resident had a bed alarm and chair alarm. During a review of Resident 103's Order Summary Report, dated 7/21/2025, the MDS indicated an order for tab alarm when in bed and wheelchair to alert/remind resident to ask for assistance when transferring or ambulating. Monitor for placement and functioning. (Informed consent obtained by MD from RP after explanation of risks and benefits verified with MD). Every shift. During a review of Resident 103's Fall Risk Evaluation, dated 5/24/2025, the Fall Risk Evaluation indicated the resident was high risk for falls. During a review of Resident 103's CP Report titled Sensor Pad Alarm. Resident requires sensor pad alarm when in wheel chair and bed due to spontaneous act/behavior of trying to get up unassisted, last revised on 12/3/2024, the CP Report indicated an intervention to apply sensor pad alarm as ordered. During an observation and interview on 7/31/2025, at 9:45 a.m., with CNA 9, inside Resident 103's room, observed Resident 103 in bed with a tab alarm on. CNA 9 stated they use the tab alarm to prevent the resident from falling because the resident does not ask for assistance when he gets out of bed. During an interview and record review on 7/31/2025, at 12:21 p.m., with RN 3, reviewed Resident 103's Order Summary Report, Fall Risk Evaluation, and Care Plan. RN 3 stated Resident 103's tab alarm is a restraint because it prevents the resident from getting out of bed freely. RN 3 stated the care plan indicated the resident was using a pad alarm, however, the order from 7/21/2025 was a tab alarm. RN 3 stated the licensed staff should have updated the care plan to tab alarm and other interventions should have been reviewed and updated as needed. RN 3 stated the failure of the licensed staff to update the care plan had the potential for delay in care and services and miscommunication with healthcare providers providing direct care to the resident. During an interview on 8/1/2025, at 2:05 p.m., with the ADON, the ADON stated the staff should have updated the care plan on the use of tab alarm on Resident 103 to ensure the care and services were relevant and delivered timely. The ADON stated an updated care plan provides a standardized care to residents and helps healthcare providers provide high quality care to residents. During a review of the facility's recent policy and procedure (P&P) titled Care Plans, Comprehensive Person-Centered, last reviewed on 4/24/2025, the P&P indicated a comprehensive, person-centered care plan that includes measurable objectives and timetables to meet the resident's physical, psychosocial and functional needs is developed and implemented for each resident. Policy Interpretation and Implementation 12. The interdisciplinary team reviews and updates the care plan: a. when there has been a significant change in the resident's condition; b. when the desired outcome is not met; c. when the resident has been readmitted to the facility from a hospital stay; and d. at least quarterly, in conjunction with the required quarterly MDS assessment.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the necessary care and services to maintain or improve a resident's ability to carry out the activities of daily livin...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to ensure the necessary care and services to maintain or improve a resident's ability to carry out the activities of daily living (ADLs, activities such as bathing, dressing and toileting a person performs daily) was provided for one of ten sampled residents (Resident 59) observed during dining observation task by failing to provide feeding assistance to the resident during lunch time on 7/29/2025. The deficient practice had the potential for the resident's inadequate intake and possible weight loss and contributed to feeling of helplessness of the resident. Findings: During a review of Resident 59's admission Record, the admission Record indicated the facility admitted the resident on 11/29/2023, and readmitted the resident on 5/27/2025, with diagnoses including Parkinson's disease (a progressive disease of the nervous system marked by tremor, muscular rigidity, and slow, imprecise movements), dysphagia (difficulty swallowing), and need for assistance with personal care. During a review of Resident 59's Minimum Data Set (MDS, a resident assessment tool), dated 6/8/2025, the MDS indicated the resident usually had the ability to make self-understood and understand others and had moderately impaired cognition (is a noticeable decline in mental abilities that significantly impacts daily activities). The MDS indicated the resident was dependent to needing substantial assistance on mobility and ADLs. The MDS indicated the resident was on a mechanically altered diet (require change in texture of food or liquids [e.g., pureed food, thickened liquids]) During a re view of Resident 59's Order Summary Report, the Order Summary Report indicated an order for: -7/23/2025 Regular diet. Mechanical soft texture, thin consistency, 2 margarines with meals. -6/17/2025 Ice cream with lunch and dinner. -7/23/2025 Continue skilled Speech Therapy (ST, a type of help for people who have trouble with talking, understanding language, or swallowing) services daily three times per week for four weeks (qd, 3x/wk, x 4 wks) for (r13.12) to continue oral (PO) trials, texture analysis, diet modification, safety education awareness, pharyngeal strengthening exercises and overall airway protection. One time only until 8/19/2025 7:44. During a review of Resident 59's Care Plan (CP) Report regarding the resident having an alteration in nutritional status, last revised on 5/30/2025, the CP Report indicated an intervention to set up meal tray, assist and give verbal cues if needed, allow enough time to eat, and observe for chewing or swallowing difficulties and report to the physician as indicated. During a concurrent observation, interview, and record review on 7/29/2025, at 12:35 p.m., with Restorative Nursing Assistant (RNA) 1, inside Resident 59's room, observed Resident 59 flat in bed with the lunch tray unopened, beverages still covered with saran wrap on top of a side table at the right side of the resident's bed. The resident already reached out for the ice cream on a carton and spilled the ice cream all over the resident's clothing. Reviewed the meal ticket on the tray of Resident 59 with RNA 1. RNA 1 stated the resident was on a mechanical soft, regular diet, thin fluids and had an alert indicating Feeding Assistance. RNA 1 stated it was the responsibility of the Certified Nursing Assistant (CNA) assigned to the resident to ensure that the resident can eat properly. RNA 1 stated the CNA should have pulled the resident up in bed, placed in an upright, sitting position, set the side table across the resident's bed, and opened the tray and remove the wraps from the beverages of the resident. RNA 1 stated the resident should have been assisted in feeding as the tray ticket was indicating an alert for feeding assistance. RNA 1 stated the resident should have been assisted with feeding to ensure the resident eats and to prevent aspiration (the accidental inhalation of food, liquid, or other foreign material into the lungs instead of the esophagus and stomach). During a concurrent interview and record review on 7/31/2025, at 12:51 p.m., with Registered Nurse (RN) 3, reviewed Resident 59's Order Summary Report, Tray Ticket, and Care Plan. RN 3 stated the resident was on a regular diet, mechanical soft texture, thin consistency liquids and the tray ticket indicated an alert feeding assistance. RN 3 also stated there was no care plan if the resident was refusing to be assisted on feeding. RN 3 stated the staff should have pulled the resident up in bed, placed in a sitting position, tray table should have been placed across the resident's bed, opened the tray for the resident. RN 3 stated the staff should have assisted the resident while eating due to the risk of aspiration. RN 3 stated the resident was on continued skilled ST services to continue PO trials, texture analysis, diet modification, safety education awareness, pharyngeal strengthening exercises and overall airway protection. During an interview on 8/1/2025, at 2:05 p.m., with the Assistant Director of Nursing (ADON), the ADON stated the licensed nurses were responsible for making sure residents with ADL needs, especially with feeding residents with swallowing issues were assisted. The ADON stated the staff should have pulled the patient up in bed, placed on an upright position to prevent aspiration to resident and placed the table across the resident's bed opened the contents and assisted the resident with feeding. The ADON stated the failure of the staff to assist the resident can contribute to the feeling of helplessness on the resident. During a review of the facility's recent policy and procedure (P&P) titled Feeding Residents, last reviewed on 4/24/2025, the P&P indicated to ensure proper and safe feeding of residents. Ensure that resident head of bed (HOB) is elevated/sitting up in bed. During a review of the facility's recent P&P titled Dignity, last reviewed on 4/24/2025, the P&P indicated each resident shall be cared for in a manner that promotes and enhances his or her sense of well-being, level of satisfaction with life, feelings of self-worth and self-esteem.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure residents maintained acceptable parameters of hydration status (amount of water intake needed for the body to function...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to ensure residents maintained acceptable parameters of hydration status (amount of water intake needed for the body to function) for one of one sampled resident (Resident 25) reviewed during the Hydration care area by failing to ensure the resident was offered sufficient fluid intake per the prescribed physician's orders to provide an adult handicap non-spill cup (adaptive drinking cup designed to assist adults with various physical limitations in drinking independently and safely) within reach of the resident. This deficient practice had the potential to result in dehydration (a condition that occurs when the body uses or loses more fluid than it takes in) placing residents at risk for electrolyte imbalances, organ failure and death. Findings: During a review of Resident 25's admission Record (AR), the AR indicated the facility admitted the resident on 9/13/2021 and most recently readmitted the resident on 2/15/2025 with diagnoses that included diabetes mellitus (DM-a disorder characterized by difficulty in blood sugar control and poor wound healing), dementia (a general term for loss of memory, language, problem-solving and other thinking abilities that interfere with daily life), and chronic obstructive pulmonary disease (COPD-a chronic lung disease causing difficulty in breathing). During a review of Resident 25's Minimum Data Set (MDS - resident assessment tool), dated 6/25/2025, the MDS indicated the resident was usually able to understand others and usually able to make themselves understood. The MDS further indicated the resident was dependent on staff for eating, bathing, toileting, and personal hygiene; and required substantial/maximal assistance with oral hygiene and dressing. During a review of Resident 25's Order Summary Report, the Order Summary Report indicated an order to use an adult handicap (non-spill) cup for drinking water during the day and at nighttime, place the cup within resident's reach, dated 7/9/2024. During a review of Resident 25's Dehydration Risk Evaluation, dated 6/8/2025, the Dehydration Risk Evaluation indicated the resident required feeding assistance and was at risk for dehydration. During a review of Resident 25's Nutritional Assessment Annual, dated 3/31/2025, the Nutritional Assessment Annual indicated the resident required 1800 to 2000 cubic centimeters (cc - a unit of liquid measurement) of fluids. During a review of Resident 25's Care Plan (CP) regarding risk for dehydration related to DM, cognitive impairment, kidney failure, and the use of laxatives (medication that helps have a bowel movement), last revised 4/9/2024; the CP indicated a goal to reduce the risk and or minimize the risk for dehydration with interventions that included to offer and encourage the resident to increase fluid intake and to provide fluids as ordered. During an observation on 7/29/2025 at 9:35 a.m., observed Resident 25 lying in bed. Observed a nightstand next to the bed, observed no adult handicap cup within reach of the resident. During an observation on 7/29/2025 at 9:45 a.m., observed Resident 25 lying in bed. Observed Licensed Vocation Nurse (LVN) 7 enter and exit the resident room. Observed LVN 7 did not place an adult handicap cup within reach of the resident. During an observation on 7/30/2025 at 1 p.m., observed Resident 25 sitting in a wheelchair in the Activities Room. Observed no adult handicap cup within reach of the resident. During an observation on 7/30/2025 at 4:22 p.m., observed Resident 25 sitting in a wheelchair at bedside. Observed no adult handicap cup within reach of the resident. Observed two adult handicap cups on a plastic bin against the wall across from the foot of the resident's bed. Observed Certified Nursing Assistant (CNA) 12 speaking with Resident 25, then CNA 12 exited the resident's room. During a concurrent observation and interview on 7/30/2025 at 4:30 p.m., with CNA 12, CNA 12 stated CNA 12 knows the resident well and the resident has a special no spill cup for water. CNA 12 confirmed two no spill cups were on the plastic bin against the wall. CNA 12 stated the cups were never within reach of the resident because the resident needs help and to be encouraged to drink. Observe CNA 12 walk into Resident 12's room and offer the no spill cup with water. Observed Resident 12 hold the cup independently and drink from the cup. During a concurrent interview and record review on 7/30/2025 at 4:30 p.m. with LVN 9, LVN 9 reviewed Resident 25's physician orders. LVN 9 stated Resident 25 had a physician's order to have the no spill cup within reach of the resident because the resident was at risk for dehydration. LVN 9 stated the cup should be within reach of the resident. LVN 9 stated when Resident 25 did not have the cup within reach there was a possible risk of dehydration. During a concurrent interview and record review on 7/31/2025 at 8:08 a.m. with Minimum Data Set Nurse (MDSN) 1 and MDSN 2, Resident 25's physician orders and Nutrition/Dietary Note dated 3/31/2025 at 2:22 p.m. were reviewed. MDSN 1 stated the Registered Dietician (RD) indicated that Resident 25 should have the non-spill cup for drinking and there was an order to have the cup within reach of the resident. MDSN 2 stated Resident 25 can't fully grasp a regular cup and should have the non-spill cup within reach to benefit the resident's hydration status and prevent dehydration that may result in a urinary tract infection. During an interview on 7/31/2025 at 10:18 a.m. with Registered Nurse (RN) 3, RN 3 stated Resident 25 was at risk of dehydration because the resident has dementia. RN 3 stated Resident 25 does not express when Resident 25 is thirsty, and the cup is a visual reminder to cue the resident to drink. RN 3 stated it was important to have the cup to prevent dehydration that may result in confusion, kidney issues, possible transfer to the hospital if the issue does not resolve. During a review of the facility Policy and Procedure (P&P) titled, Hydration - Clinal Protocol, last reviewed 4/24/2025, the P&P indicated the physician, and staff will help define the individual's current hydration status. The staff will provide supportive measures such as supplemental fluids and adjusting environmental temperature, where indicated.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure respiratory care provided to residents was consistent with professional standards of practice for one of one sampled r...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to ensure respiratory care provided to residents was consistent with professional standards of practice for one of one sampled resident (Resident 50) reviewed for respiratory care by failing to ensure Resident 50's oxygen via nasal cannula (NC - a simple, two-pronged device that delivers extra oxygen to the nose) was not touching the floor. The deficient practice had the potential for residents to develop complications such as shortness of breath and desaturation (low levels of oxygen in the blood) and respiratory infections. Findings: During a review of Resident 50's admission Record, the admission Record indicated the facility admitted the resident on 10/5/2024, and readmitted the resident on 4/30/2025, with diagnoses including sepsis (a life-threatening blood infection), pneumonitis (inflammation of the lungs), and chronic obstructive pulmonary disease (COPD, a chronic lung disease causing difficulty in breathing). During a review of Resident 50's History and Physical (H&P), dated 4/30/2025, the H&P indicated the resident was able to make decisions for activities of daily living. During a review of Resident 50's Minimum Data Set (MDS - a resident assessment tool), dated 5/7/2025, the MDS indicated the resident had the ability to make self-understood and understand others and had intact cognition (a participant who has sufficient judgment, planning, organization, self-control, and the persistence needed to manage the normal demands of the participant's environment). The MDS indicated the resident was on continuous oxygen therapy (a treatment that provides extra oxygen to a person, usually through a mask or nasal tubes, to help them breathe more easily, especially when their lungs are not working well enough on their own). During a review of Resident 50's Order Summary Report, the Order Summary Report indicated an order for: -5/1/2025 [Oxygen] Administer O2 at 2 liters per minute (L/min, a way to measure how much liquid or gas is flowing through something in one minute) via NC. May titrate (to carefully adjust or measure something, often a liquid, to achieve a specific outcome or find the right amount needed) up to 5 L/min for oxygen saturation (O2 sat, the amount of oxygen carried in the blood, specifically how much hemoglobin is carrying oxygen) less than 93%. -7/16/2025 [Oxygen] Change nasal cannula/mask as needed when soiled. During a review of Resident 50's Care Plan (CP) Report titled Resident is at risk for Coronavirus disease 2019 (COVID-19, a highly contagious respiratory disease caused by the SARS-CoV-2 virus. SARS-CoV-2 is thought to spread from person to person through droplets released when an infected person coughs, sneezes, or talks) infection, initiated on 7/4/2024, the CP Report indicated an intervention to continue infection control practices to prevent the spread of infection. During a concurrent observation and interview on 7/29/2025, at 10:52 a.m., with Certified Nursing Assistant (CNA) 7, inside Resident 50's room, observed Resident 50's oxygen via nasal cannula's tubing was touching the floor. CNA 7 stated the oxygen tubing should not be touching the floor and had no date on the tubing was placed was illegible. CNA 7 stated it was the responsibility of all staff working in the facility to ensure the oxygen via nasal cannula tubing should not be touching the floor to prevent respiratory infection and the tubing should be labeled with the date it was last changed and should be legible. CNA 7 stated the facility is labelling the tubing with the date it was last changed to help the staff determine on when to change the tubing again. During an interview on 7/31/2025, at 11:37 a.m., with Registered Nurse (RN) 3, RN 3 stated the nasal cannula tubing of Resident 50 should not be touching the floor due to infection control. RN 3 stated the resident can suffer from upper respiratory tract infection (URTI - a common cold or similar illness that affects the nose, throat, and sinuses) due to ascending infection. RN 3 stated the P&P regarding oxygen therapy is not followed because of the risk of URTI brought about by the tubing touching the floor. During an interview on 8/1/2025, at 2:05 p.m., with the Assistant Director of Nursing (ADON), the ADON stated the licensed staff should have kept the oxygen via nasal cannula from touching the floor due to the risk of respiratory infection to resident. The ADON stated microorganisms could creep into the tubing causing ascending infection to Resident 50. During a review of the facility's recent policy and procedure (P&P) titled Oxygen Administration, last reviewed on 4/24/2025, the P&P indicated the purpose of the procedure is to provide guidelines for safe oxygen administration. During a review of the facility's recent P&P titled Infection Control, last reviewed on 4/24/2025, the P&P indicated the facility must establish and maintain an Infection Control Program designed to provide a safe, sanitary and comfortable environment and to help prevent the development and transmission of disease and infection.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide pharmaceutical services (including procedures that assure accurate acquiring, receiving, dispensing, and administerin...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to provide pharmaceutical services (including procedures that assure accurate acquiring, receiving, dispensing, and administering of all drugs and biologicals) to meet the needs of each resident for: 1. One of three inspected medications carts (Sub-Acute Cart 2) by failing to accurately account for one dose of oxycodone (a controlled medication used to treat pain) 10 milligrams (mg - a unit of measure for mass) affecting Resident 27. This deficient practice increased the risk of diversion (any use other than that intended by the prescriber) of controlled mediations (medications with a high risk for diversion) and the risk that Resident 27 could have received too much or too little medication due to lack of documentation possibly resulting in serious health complications requiring hospitalization. 2. One of one sampled resident (Resident 97) by failing to ensure Licensed Vocational Nurse (LVN) 1 administered medications according to physicians' orders. This deficient practice had the potential to negatively affect Resident 97. Findings:1. 1.During an observation and concurrent interview of Sub-Acute Cart 2 on 7/30/25 at 2:25 p.m. with the Registered Nurse (RN) 4, the following discrepancy was found between the Controlled Drug Record (a log signed by the nurse with the date and time each time a controlled substance is given to a resident) and the medication card (a bubble pack from the dispensing pharmacy labeled with the resident’s information that contains the individual doses of the medication):
-Resident 27’s Controlled Drug Record for oxycodone 10 mg indicated there were two doses left; however, the medication card contained one dose.
During a concurrent interview, RN 4 stated she administered the missing dose of oxycodone to Resident 27 this morning but failed to sign for the dose at that time on the Controlled Drug Record. RN 4 stated she is the supervisor on this unit today so her attention has been divided in between several different tasks but understands that the doses must be signed out on the Controlled Drug Record immediately after they are removed from the resident's bubble pack. RN 4 stated this ensures accountability of the medication in order to prevent diversion of controlled substances and prevent accidental exposure to other residents which could possibly result in medical complications.
2.During a review of Resident 97 admission Record (AR), the AR indicated the facility admitted Resident 97 on 4/3/2024 and readmitted the resident on 5/10/2024, with diagnoses included aphasia ( a disorder that makes it difficult to speak), dysphagia (difficulty swallowing), history of falling, anxiety (a feeling of unease, worry, or fear), and depression (a mental health condition that makes you feel persistently sad and lose interest in things you usually enjoy).
During a review of Resident 97’s Physician Orders, dated 12/20/2024, the Physician Orders indicated:
- atenolol oral tablet 25 milligrams (mg- a unit of measurement) give one (1) tablet by mouth every 12 hours for hypertension (HTN-high blood pressure) hold for systolic blood pressure (SBP-systolic blood pressure reading is the measurement of this peak pressure in the arteries) less than (<) 110 or heart rate (HR-the number of times your heart beats per minute [BPM]) 60.
- Docusate sodium tablet 100 mg give one tablet by mouth one time a day for bowel management (hold for loose bowel movement).
During a review of Resident 97’s care plan for altered behavior patterns related to depression, initiated on 1/2/2025 and revised on 3/12/2025, the care plan indicated Resident 97 had depression manifested by crying spells and inability to sleep. The care plan interventions included assessing what may cause behavior and what may trigger behavior, attempt to reduce and eliminate those triggers if possible.
During a review of Resident 97’s Physician Orders, dated 1/29/2025, the Physician Orders indicated Zoloft oral tablet 50 mg give one (1) tablet by mouth one time a day for depression manifested by crying spells.
During a review of Resident 97’s Physician Orders, dated 3/12/2025, the Physician Orders indicated Keppra oral tablet 500 mg give one tablet by mouth two times a day for seizures (a sudden, uncontrolled electrical disturbance in the brain which can cause uncontrolled jerking, blank stares, and loss of consciousness).
During a review of Resident 97’s Minimum Data Set (MDS – a resident assessment tool), dated 5/17/2025, the MDS indicated Resident 97 sometimes understood and was sometimes able to be understood. The MDS indicated Resident 97 coughed and choked during meals or when swallowing medications.
During a review of Resident 97’s Physician Orders, dated 5/30/2025, the Physician Orders indicated clonazepam oral tablet 0.5 mg give one tablet by mouth two times a day for anxiety.
During a review of Resident 97’s History and Physical (H&P – comprehensive assessment conducted by a healthcare provider that includes gathering a thorough medical history from the resident and performing a physical examination to assess their overall health and identify any potential medical concern), dated 5/22/2025, the H&P indicated Resident 97 did not have the capacity to understand and make decisions.
During a review of Resident 97’s Medication Administration Audit Report dated 7/25/2025, the Medication Administration Audit Report indicated:
- Docusate Sodium tablet 100 mg one tablet by mouth a day for bowel management, indicated schedule date: 7/25/2025 at 9 a.m. and administration time as 12:52 p.m. (3 hours and 52 minutes delay in administration).
- atenolol oral tablet 25 mg- a unit of measurement give one tablet by mouth every 12 hours for HTN hold for SBP less than 110 or HR 60, indicated schedule date: 7/25/2025 at 9 a.m. and administration time as 12:52 p.m. (3 hours and 52 minutes delay in administration).
- Zoloft oral tablet 50 mg give one tablet by mouth one time a day for depression manifested by crying spells, indicated schedule date: 7/25/2025 at 9 a.m. and administration time as 12:52 p.m. (3 hours and 52 minutes delay in administration).
- Keppra oral tablet 500 mg give one tablet by mouth two times a day for seizures, indicated schedule date: 7/25/2025 at 9 a.m. and administration time as 12:52 p.m. (3 hours and 52 minutes delay in administration).
- Clonazepam oral tablet 0.5 mg give one tablet by mouth two times a day for anxiety, indicated schedule date: 7/25/2025 at 9 a.m. and administration time as 12:52 p.m. (3 hours and 52 minutes delay in administration).
During a concurrent interview and record review on 7/30/2025 at 1:29 p.m., with Licensed Vocational Nurse (LVN) 1, Resident 97’s Medication Administration Record (MAR - a daily documentation record used by a licensed nurse to document medications and treatments given to a resident) dated 7/25/2025 was reviewed. LVN 1 stated for administration of blood pressure medication, it is required to check the blood pressure prior administering medication. LVN 1 stated we verify the name, we check the administration parameters then we administer the medication. LVN 1 stated after administering medication, we document right away in the MAR. LVN 1 reviewed Resident 97`s MAR for 7/25/2025 and stated that the scheduled time to administer atenolol was at 9:00 a.m., and he (LVN 1) documented that he administered the medication at 12:52 p.m. LVN 1 stated he (LVN 1) documents on paper the time that he (LVN 1) gives medication, then he (LVN 1) documents in the MAR that he (LVN 1) administered the medication. LVN 1 stated the issue with late documentation is that it will consider late medication administration when the data entry is late. LVN 1 stated for atenolol it is a blood pressure medication looks like it was given late. LVN 1 stated atenolol administration was late for about four hours. LVN 1 stated late administration of atenolol can cause Resident 97’s blood pressure to go high. LVN 1 stated Keppra is for seizure, and the late administration of Keppra can cause Resident 97 to have seizure. LVN 1 stated Resident 97 can have agitation if he does not receive his clonazepam and Zoloft on time.
During a concurrent interview and record review on 7/31/2025 at 12:19 p.m. with the Director of Nursing (DON), Resident 97’s MAR was reviewed. The DON stated for medication administration staff are required to verify the right resident, right medication, right dose and right route. The DON stated if prior administering medication any monitoring is required, staff are required to perform pre and post monitoring. The DON stated staff are required to sign and document in MAR after administering medications. The DON reviewed Resident 97’s MAR and stated that on 7/25/2025, there was about four (4) hour delay in administering Resident 97’s medications. The DON stated based on audit form the medications were given late. The DON stated there is a potential for adverse reaction due to a delay in Resident 97`s medication administration.
During a review of the facility’s policy and P&P titled, “Administering Medication,” last reviewed on 4/24/2025, the P&P indicated Medications are administered in a safe and timely manner and as prescribed.
1. Medications are administered in accordance with prescriber orders, including any required time frames.
10. The following information is checked and verified for each resident prior to administering medications:
b. vital signs, if necessary
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide reasonable accommodation of resident needs an...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide reasonable accommodation of resident needs and preferences by failing to ensure: 1.The call light (CL, an alerting device for nurses or other nursing personnel to assist a resident when in need) was within reach for two (2) of five (5) residents (Resident 1 and 10) reviewed under the Environment task. 2. The pad call light (a specialty alerting device that have ultra-sensitive touch surface for patients with limited mobility for nurses or other nursing personnel to assist a patient when in need) was within reach for two (2) of four (4) sampled residents (Residents 8 and 71) reviewed under the Environment task. These deficient practices had the potential to result in a delay of care and services and possible injury to residents when they are unable to summon health care workers. Findings:a.During a review of Resident 1’s admission Record (AR), the AR indicated the facility admitted the resident on 5/12/2022 and most recently admitted the resident on 2/15/2025 with diagnoses that included acute and chronic respiratory failure (a serious condition that occurs suddenly when the lungs cannot get enough oxygen), tracheostomy (opening surgically created through the front of the neck and into the trachea [windpipe]), dependence on respiratory ventilator (a medical device to help support or replace breathing), muscle weakness, and need for assistance with personal care.
During a review of Resident 1’s Minimum Data Set (MDS – resident assessment tool), dated 5/18/2025, the MDS indicated the resident was totally dependent on staff for mobility, dressing, bathing, toileting, and personal hygiene.
During a review of Resident 1’s History and Physical (H&P), dated 2/16/2025, the H&P indicated the resident was nonverbal, awake, alert, able to respond yes/no appropriately to questions, and was able to move all extremities. The H&P further indicated that the resident was able to understand and make decisions.
During a review of Resident 1’s Care Plan (CP) regarding communication deficit, initiated 5/12/20218 and last reviewed 6/6/2025, the CP indicated a goal that the resident would have their needs met with an intervention to keep the CL within reach.
During an observation on 7/29/2025 at 11:20 a.m., observed Resident 1 awake in bed. Observed the call light cord was wrapped around the resident`s right bedside rail (SR - rigid plastic bars attached to the bed) and dangling toward the floor. Observed the CL was not within reach of the resident. Resident 1 did not respond to the surveyor.
During an interview on 7/29/2025 at 11:40 a.m. with Certified Nursing Assistant (CNA) 5, CNA 5 stated CNA 5 was covering while the assigned CNA, CNA 6, was on break. CNA 5 stated the CL should always be within reach for residents to use to get assistance when needed. CNA 5 stated Resident 1 is able to use his hands. CNA 5 entered Residents 1’s room and stated the CL was tied to the side rail and was not within reach of the resident. Observed CNA 5 untied the CL from the SR and placed the CL on Resident 1’s chest.
During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the Assistant Director of Nursing (ADON), the ADON reviewed the facility policy and procedure (P&P) regarding CLs. The ADON stated the CL should be within easy reach of all residents. The ADON stated when CLs are not within reach of residents, they may not be able to get assistance when needed. The ADON stated when the resident is not able to get assistance it may result in a delay of care and a potential resident fall if the resident attempts to get up. The ADON stated the facility P&P was not followed when Resident 1’s CL was not within reach.
During a review of the facility P&P titled, “Fall and Fall Risk, Managing,” last reviewed 4/24/2025, the P&P indicated the staff will identify interventions related to the resident's specific risks and causes to try to prevent the resident from falling and to try to minimize complications from falling.
During a review of the facility P&P titled, “Functioning Equipment: Call Lights,” last reviewed 4/24/2025, the P&P indicated the purpose of the P&P was to ensure residents will have a functioning Call light system. Staff shall ensure residents have a functioning call light for prompt assistance. Ascertain that a working call light is within residents reach when in his/her room.
b. During a review of Resident 10’s AR, the AR indicated the facility admitted the resident on 12/7/2024 and most recently admitted the resident on 12/23/2024 with diagnoses that included nontraumatic intracerebral hemorrhage (a type of stroke caused by bleeding in the brain), hemiplegia (total paralysis of the arm, leg, and trunk on the same side of the body) and hemiparesis (partial paralysis or weakness on one side of the body) affecting left non-dominant side, and need for assistance with personal care.
During a review of Resident 10’s MDS, dated [DATE], the MDS indicated the resident was sometimes able to understand others and was sometimes able to be understood. The MDS further indicated that the resident was totally dependent on staff for mobility, dressing, bathing, toileting, and personal hygiene.
During a review of Resident 10’s H&P, dated 12/24/2024, the H&P indicated the resident was able to understand and make decisions. The H&P further indicated the resident was able to move both the lower extremities and was able to move the right upper extremity.
During a review of Resident 10’s Order Summary Report, the Order Summary Report indicated a physician’s order for the following:
-Falling Star Program (a fall prevention initiative designed to identify and protect patients at high risk of falling) frequent visual monitoring due to high risk for fall and injury, dated 5/23/2025.
During a concurrent observation and interview on 7/30/2025 at 10:07 a.m., with Resident 10 and Restorative Nurse Aide (RNA) 1, observed Resident 10 lying in bed with the CL clipped to the sheet on the left side of the resident. Resident 10 stated Resident 10 had pain and would call the nurse. Observed Resident 10 moved the right arm in the direction of the CL at the left side of the resident’s body. Observed that Resident 10 was unable to move the left arm. Observed the CL was not within reach of Resident 10’s right hand. RNA 1 then exited from behind a closed curtain to Resident 10’s bedside. RNA 1 stated Resident 10’s CL was not within reach and the CL should not have been placed on the left side of the resident because the resident could not move the left arm. Observed RNA 1 unclip the CL from the sheet on the left side and re-clipped the CL to the sheet on the right side of the resident.
During an interview on 7/30/2025 at 10:15 a.m. with CNA 9, CNA 9 stated Resident 10 cannot move the left arm and the CL light should not have been clipped to the left side of the resident’s sheet. CNA 9 stated Resident 10’s CL should always be placed on the right side of the resident so the resident can call for assistance with any needs. CNA 9 stated CNA 9 was sorry.
During an interview on 7/31/2025 at 10:27 a.m. with Registered Nurse (RN) 3, RN 3 stated Resident 10 should have the CL on the resident’s right side, not the left. RN 3 stated the CL should be within reach to ensure the resident has access to call for assistance when help is needed. RN 3 stated when residents do not have access to the CL then a lot of things can happen like a delay in care and treatment of the resident, or the resident may fall when trying to do something on their own.
During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the ADON, the ADON reviewed the facility P&P regarding CLs. The ADON stated the CL should be within easy reach of all residents. The ADON stated when CLs are not within reach of residents, they may not be able to get assistance when needed. The ADON stated when the resident is not able to get assistance it may result in a delay of care and potentially a fall if the resident attempts to get up. The ADON stated the facility P&P was not followed when Resident 10’s CL was not within reach.
During a review of the facility P&P titled, “Fall and Fall Risk, Managing,” last reviewed 4/24/2025, the P&P indicated the staff will identify interventions related to the resident's specific risks and causes to try to prevent the resident from falling and to try to minimize complications from falling.
During a review of the facility P&P titled, “Functioning Equipment : Call Lights,” last reviewed 4/24/2025, the P&P indicated the purpose of the P&P was to ensure residents will have a functioning Call light system. Staff shall ensure residents have a functioning call light for prompt assistance. Ascertain that a working call light is within residents reach when in his/her room.
c. During a review of Resident 8’s AR, the AR indicated the facility originally admitted the resident on 5/4/2011 and readmitted in the facility on 5/12/2025, with diagnoses including dependence on respirator (also known as ventilator – a machine used to help a person breath when they are unable to do so on their own) status , contracture of muscle multiple sites, and type two diabetes mellitus (DM 2 - a disorder characterized by difficulty in blood sugar control and poor wound healing).
During a review of Resident 8’s History and Physical (H&P) dated 5/13/2025, the H&P indicated Resident 8 did not have the capacity to understand and make decisions.
During a review of Resident 8’s MDS, dated [DATE], the MDS indicated Resident 8 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make her needs known. The MDS further indicated Resident 8 had impairment of both upper extremities and required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive).
During a review of Resident 8’s fall risk assessments dated 1/2/2025, 4/3/2025, 5/13/2025, and 7/4/2025, the fall risk assessments indicated Resident 8 was a low risk for falls.
During a review of Resident 8’s care plan (CP) on risk for falls or injury initiated on 10/4/2016 and last revised on 4/16/2023, the CP indicated to keep call light within easy reach and encourage resident to use it to get assistance as one of the interventions to reduce the risk of falls and injury daily.
During a concurrent observation and interview on 7/29/2025 at 10:57 a.m. inside Resident 8’s room with LVN 4, LVN 4 stated Resident 8’s both upper extremities were contracted and that the call light was placed next to the left upper siderail away from Resident 8’s reach. LVN 4 stated staff are supposed to ensure the call light is within a resident’s reach, especially the resident with specialty call lights prior to leaving the room. LVN 4 stated Resident 8’s call light should have been placed on top of the chest or on either side of the face so Resident 8 would be able to alert the staff for assistance. LVN 4 stated if Resident 8’s call light was not within reach, the staff would not be able to know she needed assistance, and it could lead to a delay in assisting and meeting the resident needs.
During an interview on 7/29/2025 at 11:30 p.m. with Registered Nurse (RN) 4, RN 4 stated prior to leaving the room, all staff involved with the residents’ care should ensure that the call light is within reach to be able to alert staff for assistance even if they were unable to talk. RN 4 stated the pad call light is very sensitive with small movement and placed for residents who have limited mobility with their upper extremities. RN 4 stated Resident 8’s both upper extremities are severely contracted and that the call light should have been placed either on top of the chest or next to the face so the resident would be able to ask for assistance when needed by moving her face towards the pad call light. RN 4 stated if the call light was not placed within Resident 8’s reach, the resident would not be able to call for assistance, which could lead to a delay in assisting the resident and meeting her needs.
During an interview on 7/31/2025 at 4:13 p.m. with the Director of Nursing (DON), the DON stated the staff should ensure that the call light is placed within the residents’ reach prior to leaving the rooms. The DON stated that for residents with contractures of the upper extremities and unable to use a call light with push button, they are provided with the pad call light. The DON stated the staff did not place the call light within Resident 8’s reach. The DON stated Resident 8’s pad call light should have been placed on top of the chest area or on either side of the face to ensure the resident would be able to call for assistance even if Resident 8 was unable to communicate verbally with the staff. The DON stated if Resident 8’s call light was not within reach, the resident would be able to call which could lead to a delay in meeting the resident’s needs.
During a review of the facility’s recent P&P titled, “Functioning Equipment – Call Lights,” last reviewed on 4/24/2025, the P&P indicated the facility will ensure residents will have a functioning call light system and ascertain (make sure) that a working call light is within the resident’s easy reach when in his/her room or toilet.
d. During a review of Resident 71’s AR, the AR indicated the facility originally admitted the resident on 5/4/2011 and readmitted in the facility on 5/12/2025, with diagnoses including tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), dependence on respirator status, contracture of muscle multiple sites, and gastrostomy (a surgical opening fitted with a device to allow feedings to be administered directly to the stomach common for people with swallowing problems).
During a review of Resident 71’s H&P dated 6/24/2025, the H&P indicated Resident 71 did not have the capacity to understand and make decisions.
During a review of Resident 71’s MDS, dated [DATE], the MDS indicated Resident 71 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make her needs known. The MDS further indicated Resident 71 had impairment of both upper and lower extremities and required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive).
During a review of Resident 71’s fall risk assessments dated 12/26/2024, 4/2/2025, and 7/3/2025, the fall risk assessments indicated Resident 71 was a low risk for falls.
During a review of Resident 71’s CP on risk for falls or injury initiated on 2/16/2018 and last revised on 7/4/2025, the CP indicated to keep call light within easy reach as one of the interventions to reduce falls and injury daily.
During a concurrent observation and interview on 7/29/2025 at 10:59 a.m. inside Resident 71’s room with LVN 4, LVN 4 stated Resident 71’s both upper extremities were contracted and that the pad call light was hanging over the left siderail and was already close to touching the floor and was not within Resident 71’s reach. LVN 4 stated staff are supposed to ensure the call light is within the resident’s reach, especially the residents with specialty call lights, prior to leaving the room. LVN 4 stated Resident 71’s call light should have been placed on top of the chest or on either side of the face so Resident 71 would be able to alert the staff for assistance. LVN 4 stated if Resident 71’s call light was not within reach, the staff would not be able to know she needed assistance, and it could lead to a delay in assisting and meeting the resident needs.
During an interview on 7/29/2025 at 11:30 p.m. with RN 4, RN 4 stated prior to leaving the room, all staff involved with the residents’ care should ensure that the call light is within reach to be able to alert staff for assistance even if they were unable to talk. RN 4 stated the pad call light is very sensitive with small movement and placed for residents who have limited mobility with their upper extremities. RN 4 stated Resident 71’s both upper extremities are contracted and that the call light should have been placed either on top of the chest or next to the face so the resident would be able to ask for assistance when needed by moving her face towards the pad call light. RN 4 stated if the call light was not placed within Resident 71’s reach, the resident would not be able to call for assistance, which could lead to a delay in assisting the resident and meeting her needs.
During an interview on 7/31/2025 at 4:13 p.m. with the DON, the DON stated the staff should ensure that the call light is placed within the residents’ reach prior to leaving the rooms. The DON stated that for residents with contractures of the upper extremities and unable to use a call light with push button, they are provided with the pad call light. The DON stated the staff did not place the call light within Resident 71’s reach. The DON stated Resident 71’s pad call light should have been placed on top of the chest area or on either side of the face to ensure the resident would be able to call for assistance even if Resident 71 was unable to communicate verbally with the staff. The DON stated if Resident 71’s call light was not within reach, the resident would be able to call which could lead to a delay in meeting the resident’s needs.
During a review of the facility’s recent P&P titled, “Functioning Equipment – Call Lights,” last reviewed on 4/24/2025, the P&P indicated the facility will ensure residents will have a functioning call light system and ascertain (make sure) that a working call light is within the resident’s easy reach when in his/her room or toilet.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents were treated with respect and dignit...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents were treated with respect and dignity including the right to be free from physical restraints (any manual method, physical or mechanical device, material or equipment that is attached or adjacent to the resident's body that he or she cannot easily remove that restricts freedom of movement or normal access to one's body) for one of seven sampled residents (Resident 10, 44, ) reviewed during the Physical Restraints care area by failing to: 1. Ensure side rails (SR, adjustable rigid bars attached to the bed that may be positioned in various locations; upper or lower, either or both sides) were not placed in the raised (up) position on bilateral upper (area including the arms and head) and lower sides (area including the legs) without assessing for the need, assessing for safety, and obtaining informed consent (voluntary agreement to accept treatment and/or procedures after receiving education regarding the risks, benefits, and alternatives offered) prior to use for Resident 10. 2. Ensure two pillows and a folded blanket were not placed under the resident's fitted sheet while Resident 44 was lying in bed. 3. Ensure an entrapment risk assessment was completed on 2/2025 for the use of bilateral half upper SR for Resident 102. 4. Ensure an entrapment risk assessment was completed on 11/26/2024, 2/2025, 5/27/2025, and 7/26/2025 for the use of lower SR up for preference or family request for Resident 102. 5. Ensure a quarterly restraint assessment was completed on 5/2025 for the use of lower SR for Resident 102. 6. Ensure Residents 5 and Resident 103's tab alarm (a type of personal alarm used in healthcare settings, particularly in long-term care facilities and hospitals, to monitor patient movement and help prevent falls) was assessed initially and quarterly for safety of use. These deficient practices had the potential to result in the restriction of residents' freedom of movement, a decline in physical functioning, psychosocial harm, physical harm from entrapment (a state in which a person is trapped by the bed rail in a position that they cannot move from), and death of residents. Cross reference F700 Findings: a. During a review of Resident 10’s admission Record, the AR indicated the facility admitted the resident on 12/7/2024 and most recently admitted the resident on 12/23/2024 with diagnoses that included nontraumatic intracerebral hemorrhage (a type of stroke caused by bleeding in the brain), hemiplegia (total paralysis of the arm, leg, and trunk on the same side of the body) and hemiparesis (partial paralysis or weakness on one side of the body) affecting the left non-dominant side, and need for assistance with personal care.
During a review of Resident 10’s Care Plan (CP) titled, “Resident is on: lower bed, floor mat, and bilateral half upper SRs up and locked,” initiated 12/17/2024, the CP indicated a goal to prevent or reduce incidents of injury / fall as well as for comfort of getting in and out of bed. The CP indicated interventions including attempts to use the least restrictive devices on an ongoing basis.
During a review of Resident 10’s History and Physical (H&P), dated 12/24/2024, the H&P indicated the resident was able to understand and make decisions. The H&P further indicated the resident was able to move both the lower extremities and was able to move the right upper extremity.
During a review of Resident 10’s Order Summary Report, the Order Summary Report indicated a physician’s order for the following:
- [non-restraint] bilateral upper half side rails up and locked when in bed for safety, balance, activities of daily living, positioning, and as an enabler. Informed consent obtained from resident / responsible party after explanation of risk and benefits, and verified by medical doctor, dated 5/29/2025.
During a review of Resident 10’s Minimum Data Set (MDS – resident assessment tool), dated 6/16/2025, the MDS indicated the resident was sometimes able to understand others and was sometimes able to be understood. The MDS further indicated the resident was totally dependent on staff for dressing, bathing, toileting, and personal hygiene.
During a review of Resident 10’s SR Entrapment Assessment, dated 6/23/2025, the SR Entrapment Assessment indicated a recommendation for bilateral half upper SRs.
During an observation on 7/29/2025 at 3:45 p.m. Resident 10 was observed lying in bed with the bilateral lower and bilateral upper SRs in the raised position.
During a concurrent observation and interview on 7/30/2025 at 10:07 a.m., with Resident 10 and Restorative Nurse Aide (RNA) 1, Resident 10 was lying in bed with all four SRs in the raised position. RNA 1 walked to Resident 10’s bedside. RNA 1 stated Resident 10 had all four SRs in the raised position and RNA 1 did not know why all the SRs were up.
During an interview on 7/30/2025 at 10:15 a.m. with Certified Nursing Assistant (CNA) 9, CNA 9 stated CNA 9 was assigned to care for Resident 10. CNA 9 stated CNA 9 did not put Resident 10’s bilateral lower SRs in the raise position because that would be considered a restraint. CNA 9 stated CNA 9 did not know who placed all four of Resident 10’s SRs up.
During a concurrent interview and record review on 7/31/2025 at 10:27 a.m. with Registered Nurse (RN) 3, RN 3 reviewed Resident 10’s physician orders, SR Entrapment assessment dated [DATE], and Informed Consents. RN 3 stated the facility uses hospital beds that have bilateral lower and upper SRs attached to the bed. RN 3 stated sometimes the CNAs just put all four SRs up just because the SRs are there. RN 3 stated Resident 10 had an assessment and an order for only two upper SRs. RN 3 stated Resident 10 should not have all four SRs in the raised position because there was no need for all four SRs, there was no assessment for the safety of the bilateral lower SRs, no physician’s order for the use of bilateral lower SRs, and no informed consent for bilateral SRs. RN 3 stated the use of four SRs is considered a restraint because Resident 10 would not be able to lower the SRs and the SRs may prevent the resident from moving freely. RN 3 stated Resident 10 is able to move the legs and there was a potential for entrapment if the resident got caught between the bed and the lower SRs. RN 3 stated when a resident becomes caught it may result in an injury or even death of the resident if they are not found in time. RN 3 stated using the use of four SRs may also result in the resident feeling confined to the bed resulting in psychosocial issues.
During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the Assistant Director of Nursing (ADON), the ADON reviewed the facility P&P regarding SRs and Restraints. The ADON stated that when SRs are used, informed consent is obtained, and an initial safety assessment is completed to ensure entrapment and falls are prevented. The ADON stated in general residents may use bilateral upper sides rails for safety and repositioning. The ADON stated when all four SRs are up a resident is not able to remove the SRs and it confines the resident to one specific area and is considered a restraint. The ADON stated Resident 10 should not have had all four SRs raised and it was every staff member’s responsibility to ensure the lower SRs were not up. The ADON stated when Resident 10 had all four SRs in use, there was the potential to result in complications like injury to the resident if the resident tried to get over the SR to get out of the bed or psychosocial effects causing stress to the resident when they could not move out of the bed.
b. During a review of Resident 44’s admission Record, the admission Record indicated the facility originally admitted the resident on 4/12/2019 and readmitted on [DATE] with diagnoses including encephalopathy (a broad term describing any disorder or disease that affects the brain's structure or function, leading to impaired brain function), epilepsy (a condition that affects the brain and causes frequent seizures [sudden, uncontrolled body movements and changes in behavior that occurs because of abnormal electrical activity in the brain]), contracture (a stiffening/shortening at any joint, that reduces the joint's range of motion) of muscle on right upper arm, right lower leg, left lower leg, and left upper arm.
During a review of Resident 44’s CP Report titled at risk for falls/injury, dated 2/21/2023 and revised on 3/13/2025, the CP Report indicated a goal to reduce risks of falls and injury, which included interventions such as low bed with one left sided mattress against the wall when in bed, right side mattress on the floor next to the bed as landing mat to minimize risks of injury of fall.
During a review of Resident 44’s MDS, dated [DATE], the MDS indicated the resident had adequate hearing, no speech, was rarely/never makes self-understood and rarely/never had the ability to understand others. The MDS indicated the resident had impairment on both upper and lower extremities that interfered with daily functions or placed the resident at risk of injury. The MDS indicated the resident was dependent on staff for mobility which included rolling left and right, sitting to lying, lying to sitting on side of the bed, and chair/bed-to-chair transfer.
During an observation on 7/29/2025 at 9:32 a.m., while at Resident 44’s bedside, Resident 44 was lying in bed and the following was observed:
- Two pillows and a folded blanket tucked under the resident’s fitted sheet by the resident’s right hip and right leg.
- Bed placed against the wall with mattress in between, mattress on the floor at the right side of bed, and a mattress at the head of bed, and right-side rail up with padding.
- unknown number of pillows under the mattress the resident was lying on.
During a concurrent observation and interview on 7/29/2025 at 9:42 a.m. with the Assistant Director of Staff Development (ADSD), while at Resident 44’s bedside, the ADSD stated a total of six pillows were under the mattress of the resident and one pillow was underneath the fitted sheath. There was one pillow and a folded blanket on the floor on the right side of the resident’s bed. The ADSD stated she does not know why the pillow and blanket were on the floor. The ADSD stated the resident has a behavior of kicking.
During a concurrent interview and record review on 7/29/2025 at 9:45 a.m. with the ADSD, Resident 44’s Physician Orders were reviewed. The ADSD stated there was no order for the use of pillows under the fitted sheet. The ADSD stated there should be an order and care plan for the use of pillows under the fitted sheet. The ADSD stated if there is no order then they are not following the order. The ADSD stated that when the use of pillow underneath the fitted sheet has not been care planned the resident may get stuck between the bed and the mattress.
During an interview on 8/1/2025 at 3:13 p.m. with the ADON, the ADON stated when pillows are placed under the fitted sheet this is considered as a restraint. The ADON stated the resident could climb over it and could cause an injury and the psychosocial effects could cause stress to the residents when they cannot move out of bed. The ADON stated placing pillows under the fitted sheet is not an intervention here at the facility.
c. During a review of Resident 102’s AR, the AR indicated the facility admitted the resident on 5/14/2024 with diagnoses including tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), lack of coordination, and gastrostomy (GT - a surgical opening fitted with a device to allow feedings to be administered directly to the stomach common for people with swallowing problems).
During a review of Resident 102’s restraint assessment dated [DATE] and 2/26/2025, the restraint assessment indicated the use of lower SR for preference or family request as a precautionary measure and poor trunk control to decrease potential injuries.
During a review of Resident 102’s H&P, dated 5/14/2025, the H&P indicated Resident 102 was incapacitated (refers to a state in which an individual was unable to make sound decisions or manage their affairs).
During a review of Resident 102’s entrapment (when a resident gets trapped in the spaces in between or around the bed rails, mattress, or bed frame) risk assessment dated [DATE] and 5/27/2025, the entrapment risk assessment indicated a recommendation for the use of bilateral half upper SR due to generalized muscle weakness, poor trunk control, involuntary movement, and poor trunk control.
During a review of Resident 102’s MDS, dated [DATE], the MDS indicated Resident 102 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make his needs known. The MDS further indicated Resident 102 required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive).
During a review of Resident 102’s CP on use of lower SR up per family preference or request initiated on 7/29/2025 and the CP on use of bilateral half upper SR up and locked when in bed initiated on 6/6/2024, the CP indicated to attempt to use less restrictive devices on an ongoing basis as one of the interventions to prevent or reduce incidence of injury or fall.
During a review of Resident 102’s Order Summary Report dated 8/1/2025, the Order Summary Report indicated the following physician’s orders:
-10/8/2024 and last revised on 7/29/2025: may put lower SR up for preference or family request. Informed consent obtained from the responsible party (RP) by the physician (MD) after explanation of risks and benefits.
-5/18/2024 and last revised on 7/30/2025: bilateral upper half SR up and locked when in bed secondary to involuntary movement by gravity due to elevated head of bed.
During a concurrent observation and interview on 7/29/2025 at 11:53 a.m. while inside Resident 102’s room with Registered Nurse (RN) 7, RN 7 stated Resident 102’s both upper and lower SR were up. RN 7 stated that from her knowledge, Resident 102 is not supposed to have both upper and lower SR up. RN 7 stated that usually the CNAs put all 4 SR up while providing care for resident safety when turning but they must put down the lower SR after providing care. RN 7 stated Resident 102’s bilateral lower SR should have been lowered down as it was restricting the resident’s freedom of movement and can be considered a restraint. Resident 102 can get trapped in between the SR and get injured.
During a concurrent interview and record review on 7/31/2025 at 2:30 p.m., Resident 102’s physician orders, entrapment risk assessments, and restraint assessments were reviewed with Registered Nurse (RN) 3. RN 3 stated Resident 102 had a physician’s order for bilateral half upper SR and locked while in bed dated 5/18/2024 and was revised 7/30/2025 and may put lower SR up for preference or family request dated 10/8/2024 and was revised 7/26/2025. RN 3 stated the entrapment risk assessments for the use of bilateral half upper SR dated 2/2025 and the entrapment risk assessment for the use of lower SR up for preference or family request for 11/26/2024, 2/27/2025, 5/27/2025, and 7/26/2025 were not completed. RN 3 stated the quarterly restraint assessment was not completed for 5/2025 for the use of bilateral upper and lower SR. RN 3 stated entrapment risk assessments and restraint assessments are completed during admission, quarterly or as needed. RN 3 stated entrapment risk assessment are completed to ensure resident safety with the use of SR when in bed. RN 3 stated Resident 102’s entrapment risk assessments should have been completed for the use of both bilateral half upper for 2/2025 and the use of lower SR up for 11/26/2024, 2/2025, 5/27/2025, and 7/26/2025 to ensure that the use of SR was appropriate and Resident 102 was not at risk of getting trapped in between the SR and the bed mattress/frame which could to injuries. RN 3 stated Resident 102’s quarterly restraint assessment for the use of bilateral half upper and lower SR up should have been completed for 5/2025 to ensure the use of both upper and lower SR were still needed and the resident still meets the criteria for the use of all SR up while in bed as the use of all SR up was restricting Resident 102’s freedom of movement and is considered a restraint.
During a concurrent interview and record review on 7/31/2025 at 4:15 p.m., Resident 102’s physician orders, entrapment risk assessments, and restraint assessments were reviewed with the Director of Nursing (DON). The DON stated Resident 102 had a physician’s order for bilateral half upper SR and locked while in bed dated 5/18/2024 and was revised on 7/30/2025 and may put lower SR up for preference or family request dated 10/8/2024 and was revised on 7/26/2025. The DON stated the entrapment risk assessments for the use of bilateral half upper SR dated 2/2025 and the entrapment risk assessment for the use of lower SR up for preference or family request for 11/26/2024, 2/27/2025, 5/27/2025, and 7/26/2025 were not completed. The DON stated the quarterly restraint assessment was not completed on 5/2025 for the use of bilateral upper and lower SR. The DON stated entrapment risk assessments and restraint assessments are completed during admission by the admitting nurse if using bilateral half upper and/or lower SR up, then quarterly and as needed together with the MDS assessments. The DON stated entrapment risk assessments are completed quarterly to ensure the continued use of the side rails is still safe for the residents when in bed. The DON stated Resident 102’s entrapment risk assessments should have been completed for the use of both bilateral half upper for 2/2025 and the use of lower SR up for 11/26/2024, 2/2025, 5/27/2025, and 7/26/2025 to ensure that the use of SR was appropriate and Resident 102 was not at risk of getting trapped in between the SR and the bed mattress/frame which could to injuries and/or hospitalization. RN 3 stated Resident 102’s quarterly restraint assessment for the use of bilateral half upper and lower SR up should have been completed for 5/2025 to ensure the use of both upper and lower SR were still a necessity and the resident still meets the criteria for the use of all SR up while in bed as the use of all SR up was restricting Resident 102’s freedom of movement and can be considered a restraint.
d. During a review of Resident 5’s AR, the AR indicated the facility admitted the resident on 12/31/2024, and readmitted the resident on 3/27/2025, with diagnoses including cerebral infarction (occurs as a result of disrupted blood flow to the brain due to problems with the blood vessels that supply it), difficulty in walking, and muscle weakness.
During a review of Resident 5’s MDS, dated [DATE], the MDS indicated the resident had the ability to make self-understood and understand others and had severe cognitive impairment (a significant decline in a person's ability to think, learn, remember, and make decisions). The MDS indicated the resident was dependent on needing substantial assistance on mobility and activities of daily living (ADLs, activities such as bathing, dressing and toileting a person performs daily). The MDS indicated that the resident had a bed alarm (a pad with sensors that will alarm when a resident stands up unassisted to help prevent falls by alerting staff).
During a review of Resident 5’s Fall Risk Evaluation, dated 7/10/2025, the Fall Risk Evaluation indicated the resident was moderate risk for falls.
During a review of Resident 5’s Order Summary Report, dated 7/21/2025, the Order Summary Report indicated an order to apply a tab alarm when in bed and wheelchair to alert and remind the residents to ask for assistance when transferring or ambulating. Monitor for placement and functioning. (Informed consent obtained by MD from resident representative [RP] after explanation of risks and benefit and verified with MD). Every shift.
During a concurrent observation and interview on 7/31/2025, at 9:41 a.m., with CNA 9, while inside Resident 5’s room, Resident 5 was in bed with a tab alarm on. CNA 9 stated the resident had a tab alarm to prevent the resident from falling. CNA 9 stated the resident was at a high risk for falls and does not ask for assistance from staff when getting out of bed. CNA 9 stated the tab alarms alert healthcare providers when the residents attempts to get out of bed.
During a concurrent interview and record review on 7/31/2025, at 12:12 p.m., with Registered Nurse (RN) 3, Resident 5’s Order Summary Report, Informed Consent, Restraint Assessment, and Care Plan were reviewed. RN 3 stated the consent was not obtained prior to the use of tab alarm on the resident and the initial restraint assessment was not done. RN 3 stated it was important to obtain consent on the use of a restraint tab alarm to residents to ensure the risks and benefits were explained to the resident and/or representative. RN 3 also stated it was important to assess the restraint initially and quarterly for its safe use to prevent accidents such as the pull cord getting entangled on the resident.
During an interview on 8/1/2025, at 2:05 p.m., with the ADON, the ADON stated the restraint tab alarm on Resident 5 should have been assessed for appropriateness of use by licensed staff. The ADON also stated the licensed staff should have obtained a new consent for the tab alarm as the previous consent was for a pad alarm (is placed underneath the patient, and when pressure is released from the pad, an alert is sent to caregivers via a monitor or alarm). The ADON stated restraints should have a physician’s order, an informed consent, restraint assessment, and should have a care plan on its use prior to applying the restraint tab alarm.
During a review of the facility provided Tab Alarm 1 (TA) 1, copyright 2022, the information indicated TA 1 improves patient safety by alerting caregivers when a patient attempts to get out of a wheelchair or bed without assistance.
WARNING:
1. Long pull cord can entangle the patient and be potentially dangerous. Use care and supervision.
e. During a review of Resident 103’s AR, the AR indicated the facility admitted the resident on 10/30/2024, with diagnoses including difficulty in walking, age-related nuclear cataract (a type of cataract that develops in the center (nucleus) of the eye's lens, causing it to cloud over due to the natural aging process), and need for assistance with personal care.
During a review of Resident 103’s MDS, dated [DATE], the MDS indicated the resident sometimes had the ability to make self-understood and understand others and had short-term and long-term memory loss. The MDS indicated the resident was dependent and needed supervision on mobility and ADLs. The MDS indicated the resident had a bed and chair alarm.
During a review of Resident 103’s Fall Risk Evaluation, dated 5/24/2025, the Fall Risk Evaluation indicated the resident was high risk for falls.
During a review of Resident 103’s Order Summary Report, dated 7/21/2025, the Order Summary Report indicated an order to apply a tab alarm when in bed and wheelchair to alert/remind resident to ask for assistance when transferring or ambulating. Monitor for placement and functioning. (Informed consent obtained by MD from RP after explanation of risks and benefits and verified with MD. Every shift.
During a concurrent observation and interview on 7/31/2025, at 9:45 a.m., with CNA 9, while inside Resident 103’s room, Resident 103 was in bed with a tab alarm on. CNA 9 stated the resident had a tab alarm to prevent the resident from falls. CNA 9 stated the resident was a high risk for falls and does not ask for assistance from staff when getting out of bed. CNA 9 stated the tab alarms alert healthcare providers when the residents attempts to get out of the bed.
During a concurrent interview and record review on 7/31/2025, at 12:21 p.m., with RN 3, Resident 103’s Order Summary Report, Informed Consent, Restraint Assessment, and Care Plan were reviewed. RN 3 stated the consent was not obtained prior to the use of tab alarm on the resident and the initial restraint assessment was not done. RN 3 stated it was important to obtain a consent on the use of restraint tab alarm to residents to ensure the risks and benefits were explained to the resident and/or representative. RN 3 also stated it was important to assess the restraint initially and quarterly for its safe use to prevent accidents such as the pull cord getting entangled to the resident.
During an interview on 8/1/2025, at 2:05 p.m., with the ADON, the ADON stated the restraint tab alarm on Resident 103 should have been assessed for appropriateness of use by the licensed staff. The ADON also stated the licensed staff should have obtained a new consent for the tab alarm as the previous consent was for a pad alarm. The ADON stated restraints should have a physician’s order, an informed consent, restraint assessment, and should have a care plan on its use prior to applying the restraint tab alarm.
During a review of the facility policy and procedures (P&P) titled, “Use of Restraints,” last reviewed 4/24/2025, the P&P indicated restraints shall only be used for the safety and well-being of the resident(s) and only after other alternatives have been tried unsuccessfully. Restraints shall only be used to treat the resident's medical symptom(s) and never for discipline or staff convenience, or for the prevention of falls. Prior to placing a resident in restraints, there shall be an assessment and a review to determine the need for restraints. Restraints shall only be used upon the written order of a physician and after obtaining consent from the resident and/or representative.
During a review of the facility P&P titled, “Bed Safety and Bed Rails,” last reviewed 4/24/2025, the P&P indicated the use of bed rails is prohibited unless the criteria for use of bed rails have been met. The use of bed rails or side rails (including temporarily raising the side rails for episodic use during care) is prohibited unless the criteria for use of bed rails have been met, including attempts to use alternatives, interdisciplinary evaluation, resident assessment, and informed consent.
During a review of the facility P&P titled, “Resident Rights,” last reviewed 4/24/2025, the P&P indicated federal and state laws guarantee certain basic rights to all residents of this facility. These rights include the resident's right to be free from involuntary seclusion and physical or chemical restraints not required to treat the resident's symptoms.
During a review of the facility's recent P&P titled Use of Restraints, last reviewed on 4/24/2025, the P&P indicated physical restraints are defined as any manual method or physical or mechanical device, material or equipment attached or adjacent to the resident's body that the individual cannot remove easily, which restricts freedom of movement or restricts normal access to one's body.
Policy Interpretation and Implementation
5. Restraints may only be used if/when the resident has a specific medical symptom that cannot be addressed by another less restrictive intervention AND a restraint is required for:
a. Treat the medical symptom.
b. Protect the resident's safety; and
c. Help the resident attain the highest level of his/her physical or psychological well-being.
6. Prior to placing a resident in restraints, there shall be an assessment and a review to determine the need for restraints. The assessment shall be used to determine possible underlying causes of the problematic medical symptoms and to determine if there are less restrictive interventions (programs, devices, referrals, etc.) that may improve the symptoms.
9. Restrains shall only be used upon the written order of a physician and after obtaining consent from the resident and/or representative (sponsor). The order shall include the following:
a. The specific reason for the restraint (as it relates to the resident's medical symptom).
b. How restraint will be used to benefit the resident's medical symptom; and
c. The type of restraint, and period of time for the use of the restraint.
During a review of the facility provided Tab Alarm (TA) 1, copyright 2022, the information indicated TA 1 improves patient safety by alerting caregivers when a patient attempts to get out of a wheelchair or bed without assistance.
WARNING:
Long pull cord can entangle the patient and be potentially dangerous. Use care and supervision.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0605
(Tag F0605)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents were free from unnecessary psychotropic medication...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents were free from unnecessary psychotropic medication (medications that affect the mind, emotions, and behavior) and the use of chemical restraints (any drug that is used for discipline or staff convenience and not required to treat medical symptoms) for one of seven sampled resident (Residents 13) reviewed during the Accidents care area by failing to: 1. Provide ongoing re-evaluation of the need for psychotropic medication by ensuring as needed (PRN) lorazepam (a medication used to relieve symptoms of anxiety [a mental health condition that may result in restlessness, irritability, feelings of nervousness, panic, and fear]) was ordered with an end date (time at which a medication will no longer be dispensed and will be required to be re-prescribed) for Resident 13. 2. Ensure PRN lorazepam was prescribed and monitored for specific, measurable behavioral manifestation for Resident 13. 3. Provide ongoing re-evaluation of the need for psychotropic medication by failing to monitor for adverse effects (unwanted or dangerous medication-related side effects) of lorazepam for Resident 13. 4. Obtain informed consent (voluntary agreement to accept treatment and/or procedures after receiving education regarding the risks, benefits, and alternatives offered) prior to the administration of psychotropic medication for Resident 13. 5. Ensure the antipsychotic medication risperidone (a medication used to treat mental illness) was not used without a clear indication or diagnosis documented in the resident's clinical record for one of five residents sampled for unnecessary medications (Resident 15.) These deficient practices had the potential to result in an increased risk that Residents 13 and 15 could experience adverse effects related to psychotropic medication therapy, such as drowsiness, dizziness, constipation, or increased risk of fall, possibly leading to impairment or decline in their mental or physical condition or functional or psychosocial status. Findings: 1. During a review of Resident 13’s admission Record (AR), the AR indicated the facility admitted the resident on 6/25/2025 with diagnoses that included traumatic subarachnoid hemorrhage (bleeding in the area between the brain and the thin tissues that cover and protect it) with loss of consciousness (a state in which an individual lacks normal awareness of self and the surrounding environment), lack of coordination, muscle weakness, gastrostomy (GT - a surgical opening fitted with a device to allow feedings to be administered directly to the stomach common for people with swallowing problems), depression (persistent feelings of sadness and loss of interest that can interfere with daily living), and anxiety disorder.
During a review of Resident 13’s History and Physical (H&P), dated 6/27/2025, the H&P indicated the resident could not make their own decisions but was able to make needs known.
During a review of Resident 13’s Minimum Data Set (MDS – resident assessment tool) dated 7/2/2025, the MDS indicated the resident was sometimes able to understand others and was sometimes able to make themself understood. The MDS further indicated that the resident was dependent on staff for toileting, bathing, and lower body dressing; and required substantial/maximal assistance for upper body dressing, personal hygiene, and transferring from the bed to chair. The MDS indicated that the resident was administered the following high-risk medications (drugs that can cause significant patient harm if used incorrectly): antianxiety.
During a review of Resident 13’s Order Summary Report, the Order Summary Report indicated the following physician’s orders:
-Administer Lorazepam oral tablet five mg, one tablet via GT every 12 hours PRN for anxiety, dated 6/25/2025 and discontinue on 7/29/2025.
-Administer Lorazepam oral tablet five mg, one tablet by mouth every 12 hours PRN for anxiety, dated 7/29/2025.
-Monitor episodes of anxiety manifested by inability to relax and tally by hashmarks for lorazepam use, every shift, dated 7/7/2025.
- Monitor for potential side effects for anti-anxiety lorazepam: Sedation, drowsiness, morning hangover, ataxia, every shift, dated 7/7/2025.
1.a. During a concurrent interview and record review on 7/31/2025 at 8:32 a.m., with Minimum Data Set Nurse (MDSN) 1, MDSN 1 reviewed Resident 13’s physician orders and medication administration record (MAR- a record of all medications taken by a resident on a day-to-day basis) for 6/2025 and 7/2025. MDSN 1 stated psychotropic medications are high-risk medications that alter a resident’s mental status and can cause adverse effects resulting in resident falls. MDSN 1 stated medicating a resident for behavior issues should be a last resort and other methods should first be attempted. MDSN 1 stated that all PRN psychotropic medications should be ordered with a stop date when the physician then evaluates and determines if the resident still needs the medication. MDSN 1 stated Resident 13’s lorazepam order did not have a stop date and was ordered to continue indefinitely. MDSN 1 stated Resident 13 had been administered PRN lorazepam for over a month without a stop date.
During a concurrent interview and record review on 7/31/2025 at 8:53 a.m., with Registered Nurse (RN) 3, RN 3 reviewed Resident 13’s physician orders and MAR for 6/2025 and 7/2025. RN 3 stated psychotropic medications have side effects like increased confusion and increased risk for falls leading to injury. RN 3 stated the goal is to try to wean a resident off psychotropic medication because of the risk for side effects. RN 3 stated the benefits of psychotropic medication should outweigh the risks of taking the medication. RN 3 stated psychotropic medication administered PRN is ordered with a 14 day stop date. RN 3 stated PRN psychotropic medication will only be reordered after the physician re-evaluates the resident to determine if the behaviors continue and the resident has a need for the medication. RN 3 stated if a resident’s behavior is resolved, then the medication should not be reordered to prevent the medication from being administered unnecessarily. RN 3 further stated Resident 13 was not appropriately administered PRN lorazepam because there was no stop date for the order. RN 3 stated when psychotropic medication was not appropriately administered to Resident 13 there was the potential that the resident may be unnecessarily chemically restrained to control the resident behavior, without attempts to try alternative methods. RN 3 stated the unnecessary administration of lorazepam may potentially result in physical side effects leading to falls or psychosocial issues leading to the resident not participating in in activities of daily living.
During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the Assistant Director of Nursing (ADON), the ADON reviewed the facility policy and procedures regarding psychotropic medication. The ADON stated psychotropic medications affect how the resident’s brain works and can cause major side effects. The ADON stated the facility process for psychotropic medication is for the physician to obtain informed consent from the resident or resident representative, obtain an order that indicates specific behaviors to administer and monitor for, ensure PRN psychotropics are ordered for a specified time, and monitor the resident for side effects of the medication. The ADON stated it was important to follow the facility process to minimize the duration of administration of psychotropic medications due to side effects potentially resulting in tremors, sedation, drowsiness, and possible falls in residents. The ADON stated the facility P&P was not followed when Resident 13 was administered PRN lorazepam without an end date.
1.b. During a concurrent interview and record review on 7/31/2025 at 8:53 a.m., with RN 3, RN 3 reviewed Resident 13’s physician orders and MAR for 6/2025 and 7/2025. RN 3 stated psychotropic medications have side effects like increased confusion and increased risk for falls leading to injury. RN 3 stated the goal is to try to wean a resident off psychotropic medication because of the risk for side effects. RN 3 stated the benefits of psychotropic medication should outweigh the risks of taking the medication. RN 3 stated PRN psychotropic medications should be ordered and monitored for specific measurable behaviors to determine when to administer the medication. RN 3 reviewed Resident 13’s PRN lorazepam orders and noted the following:
-From 6/25/2025 to 7/6/2025, lorazepam was ordered to be administered for anxiety. RN 3 stated anxiety is not a specific measurable behavior because anxiety manifests differently in different residents. RN 3 stated Resident 13 has restlessness and is easily agitated. RN 3 stated Resident 13’s PRN Lorazepam should have been ordered, administered, and monitored for a specific measurable behavior, but it was not.
-From 7/6/2025 to 7/31/2025, lorazepam was ordered to be administered for anxiety manifested by an inability to relax. RN 3 stated the inability to relax may look different in different residents and is not a specific measurable behavior. RN 3 stated Resident 13’s PRN Lorazepam should have been ordered, administered, and monitored for a specific measurable behavior, but it was not.
RN 3 further stated Resident 13 was not appropriately administered PRN lorazepam because there was no clear behavioral manifestation to determine when to administer the medication.
During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the ADON, the ADON reviewed the facility policy and procedures regarding psychotropic medication. The ADON stated psychotropic medications affect how the resident’s brain works and can cause major side effects. The ADON stated the facility process for psychotropic medication is for the physician to obtain informed consent from the resident or resident representative, obtain an order that indicates specific behaviors to administer and monitor for, ensure PRN psychotropics are ordered for a specified time, and monitor the resident for side effects of the medication. The ADON stated it was important to follow the facility process to minimize the duration of administration of psychotropic medications due to side effects potentially resulting in tremors, sedation, drowsiness, and possible falls in residents. The ADON stated the facility P&P was not followed when Resident 13 was administered PRN lorazepam without specific measurable behavioral manifestations.
1.c. During a concurrent interview and record review on 7/31/2025 at 8:53 a.m., with RN 3, RN 3 reviewed Resident 13’s physician orders and MAR for 6/2025 and 7/2025. RN 3 stated psychotropic medications have side effects like increased confusion and increased risk for falls leading to injury. RN 3 stated the goal is to try to wean a resident off psychotropic medication because of the risk for side effects. RN 3 stated the benefits of psychotropic medication should outweigh the risks of taking the medication. RN 3 stated the facility process for monitoring is psychotropic medication side effects are monitored for and documented in the Medication Administration Record. RN 3 reviewed Resident 13’s MAR and noted the following:
-On 6/27/2025 at 7:20 p.m. lorazepam was administered and there was no documented evidence of monitoring for side effects.
On 6/28/2025 at 10:06 a.m. lorazepam was administered and there was no documented evidence of monitoring for side effects.
- On 6/28/2025 at 7:30 p.m. lorazepam was administered and there was no documented evidence of monitoring for side effects.
-On 6/29/2025 at 5:39 a.m. lorazepam was administered and there was no documented evidence of monitoring for side effects.
- On 6/30/2025 at 7:21 p.m. lorazepam was administered and there was no documented evidence of monitoring for side effects.
- On 7/1/2025 at 5:45 a.m. lorazepam was administered and there was no documented evidence of monitoring for side effects.
- On 7/3/2025 at 4:36 a.m. lorazepam was administered and there was no documented evidence of monitoring for side effects.
- On 7/5/2025 at 5:08 p.m. lorazepam was administered and there was no documented evidence of monitoring for side effects.
- On 7/6/2025 at 10:07 p.m. lorazepam was administered and there was no documented evidence of monitoring for side effects.
During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the ADON, the ADON reviewed the facility policy and procedures regarding psychotropic medication. The ADON stated psychotropic medications affect how the resident’s brain works and can cause major side effects. The ADON stated the facility process for psychotropic medication is for the physician to obtain informed consent from the resident or resident representative, obtain an order that indicates specific behaviors to administer and monitor for, ensure PRN psychotropics are ordered for a specified time, and monitor the resident for side effects of the medication. The ADON stated it was important to follow the facility process to minimize the duration of administration of psychotropic medications due to side effects potentially resulting in tremors, sedation, drowsiness, and possible falls in residents. The ADON stated the facility P&P was not followed when Resident 13 was administered PRN lorazepam without monitoring for side effects.
1.d. During a concurrent interview and record review on 7/31/2025 at 8:53 a.m., with RN 3, RN 3 reviewed Resident 13’s physician orders and Informed Consent form dated 7/7/2025. RN 3 stated psychotropic medications have side effects like increased confusion and increased risk for falls leading to injury. RN 3 stated the benefits of psychotropic medication should outweigh the risks of taking the medication. RN 3 stated prior to administering psychotropic medication, the physician must obtain written informed consent from the resident or resident representative after explaining the risk and benefits and side effects of the medication. RN 3 stated Resident 13’s written informed consent form for PRN lorazepam did not indicate who was informed of the risks and benefits of the medication and provided informed consent, and when informed consent was obtained. RN 3 stated all the nurses that administered PRN lorazepam to Resident 13 were responsible for ensuring that informed consent was obtained prior to the administration of the medication, but that was not done.
RN 3 further stated Resident 13 was not appropriately administered PRN lorazepam because there was no documented evidence of who provided consent for the psychotropic medication to be administered. RN 3 stated when psychotropic medication was not appropriately administered to Resident 13 there was the potential that the resident may be unnecessarily chemically restrained to control the resident behavior without family consent or attempts to try alternative methods. RN 3 stated the unnecessary administration of lorazepam may potentially result in physical side effects leading to falls or psychosocial issues leading to the residents not participating in activities of daily living.
During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the ADON, the ADON reviewed the facility policy and procedures regarding psychotropic medication. The ADON stated psychotropic medications affect how the resident’s brain works and can cause major side effects. The ADON stated the facility process for psychotropic medication is for the physician to obtain informed consent from the resident or resident representative, obtain an order that indicates specific behaviors to administer and monitor for, ensure PRN psychotropics are ordered for a specified time, and monitor the resident for side effects of the medication. The ADON stated the facility P&P was not followed when Resident 13 was administered PRN lorazepam without documented evidence of who gave informed consent. The ADON stated if the resident or family is not aware that psychotropic medication is administered to the resident then it could result be considered an unnecessary chemical restraint because the resident is potentially being sedated without their knowledge. The ADON stated chemically restraining a resident can affect the resident physically and emotionally causing a dignity issue.
2. A review of Resident 15’s AR, dated 7/31/25, indicated she was admitted to the facility on [DATE] with diagnoses including dementia (the loss of cognitive function, including memory, thinking, and reasoning, that interferes with daily life) and alcohol abuse. Further review of Resident 15’s admission Record indicated her brother was listed as her representative party (RP - a person delegated to make medical decisions for the resident in the event they are unable to do so.)
A review of Resident 15’s History and Physical (H&P – a record of a comprehensive physician’s assessment), dated 11/9/24, indicated Resident 15 likely has Wernicke-Korsakoff Syndrome (WKS – a medical condition causing confusion, disorientation, seeing and hearing things that are not there, and memory loss caused by a vitamin deficiency and usually associated with a history of alcohol abuse) and had “fluctuating capacity” to understand and make medical decisions. Further review of Resident 15’s H&P indicated she had “psychosis” (a mental condition characterized by a disconnection from reality in which someone may believe things that are untrue or see or hear things that are not there) and to follow up with psychiatry, but did not indicate any significant history of schizophrenia (a mental illness characterized by seeing or hearing things that are not there.)
A review of the psychiatry progress note (a record of a psychiatrist’s evaluation), dated 11/24/24, indicated Resident 15 had a “history of paranoid schizophrenia” and was “on risperidone.” Further review of the psychiatry note indicated there was no discussion of how it was determined that Resident 15 had a history of schizophrenia, how Resident 15 met the Diagnostic and Statistic Manual of Mental Disorders (DSM-5 – an objective tool used as a clinical guideline to diagnose mental illness) criteria for schizophrenia or how WKS or other medical conditions were ruled out as the cause of her psychotic symptoms.
A review of the psychiatry progress note, dated 3/6/25, indicated the “diagnosis of schizophrenia is questionable” due to “denied hallucinations.”
A review of Resident 15’s MDS, dated [DATE], Section I (active diagnoses) did not include schizophrenia as an active diagnosis.
A review of Resident 15’s available care plans, last reviewed 5/27/25, indicated there were no care plans that referenced a diagnosis of schizophrenia for which risperidone was listed as a targeted intervention.
A review of Resident 15’s Physician Order Summary (a monthly summary of all active physician orders), dated 7/31/25, indicated Resident 15 was prescribed risperidone 0.25 milligrams (mg – a unit of measure for mass) by mouth two times a day for “Schizophrenia manifested by extreme paranoid thoughts causing fear and stress.”
During a telephone interview on 7/31/2025 at 10:09 a.m. with Resident 15’s brother (FM 3), FM 3 stated he is not aware of Resident 15 having a history of schizophrenia prior to her admission to this facility. FM 3 stated her primary diagnosis is WKS and to his knowledge, she only started having psychosis-related behaviors (such as paranoid beliefs) since her initial diagnosis with WKS in November 2024.
During a concurrent observation and interview on 7/31/2025 at 10:23 a.m. of Resident 15, Resident 15 was observed lying in her bed using her cellular phone. Resident 15 was observed to be alert and oriented and able to respond to questions. Resident 15 adamantly stated she does not have schizophrenia and does not have a history of schizophrenia. Resident 15 stated no one from the facility has discussed a diagnosis of schizophrenia or medication related to treatment of schizophrenia with her.
During an interview on 7/31/2025 at 11:15 a.m. with the Director of Nursing (DON), the DON stated antipsychotic medications must have a clear indication for use which is diagnosed and documented in the resident’s clinical record. The DON stated Resident 15’s clinical record including diagnosis list, care plans, and MDS assessments do not contain a record of a diagnosis of schizophrenia. The DON stated the psychiatric progress note from 11/24/24 referenced a history of schizophrenia, but Resident 15's record contains no other documentation of a diagnosis or history of schizophrenia. The DON stated the psychiatric progress note on 3/6/25 appears to cast doubt on the validity of the diagnosis of schizophrenia. The DON stated that without a clear, confirmed diagnosis of schizophrenia, the use of risperidone may be questionable and would need to be reevaluated. The DON stated using antipsychotic medications without a clear indication may increase the risk that Resident 15 may experience adverse effects of risperidone including movement disorders, drowsiness, dizziness, actual falls, or dry mouth which could lead to a decline in her quality of life.
During a review of the facility P&P titled, “Psychotropic Medication Use,” last reviewed on 4/24/2025, the P&P indicated a psychotropic drug is any medication that affects brain activities associated with mental processes and behavior, which includes anxiolytics. The facility should not use psychotropic medications to address behaviors without first determining if there is a medical, physical, functional, psychological, social or environmental cause of the resident's behaviors. Facility staff should take a holistic approach to behavior management that involves a thorough assessment of underlying causes of behaviors and individualized person-centered non-drug and pharmaceutical interventions. Psychotropic medications may be used to address behaviors only if non-drug approaches and interventions were attempted prior to their use. Psychotropic medications to treat behaviors will be used appropriately to address specific underlying medical or psychiatric causes of behavioral symptoms. PRN orders for psychotropic drugs are limited to 14 days. For psychotropic PRN medications, if the attending physician or prescribing practitioner believes that it is appropriate for the PRN order to be extended beyond 14 days, he or she should document their rationale in the resident's medical record and indicate the duration for the PRN order.
A review of the facility’s policy “Psychotropic Medication Use,” revised March 2023, indicated “Residents who have not used psychotropic medications are not prescribed or given these medications unless the medication is determined to be necessary to treat a specific condition that is diagnosed and documented in the medical record…”
A review of the facility’s policy “Antipsychotic Medication Use, revised March 2023, indicated “Residents who are admitted from the community or transferred from a hospital and who are already receiving antipsychotic medications will be evaluated for the appropriateness and indications for use… Diagnosis of a specific condition for which antipsychotic medication are necessary to treat will be based on a comprehensive assessment of the resident… Resident diagnosis is based on a comprehensive assessment and evidence-based criteria and is consistent with professional standards, such as the Diagnostic and Statistical Manual of Mental Disorders (current edition.)…”
During a review of the facility P&P titled, “Psychotropic Medication Use,” last reviewed 4/24/2025, the P&P indicated the facility should not use psychotropic medications to address behaviors without first determining if there is a medical, physical, functional, psychological, social or environmental cause of the resident's behaviors. Psychotropic medications to treat behaviors will be used appropriately to address specific underlying medical or psychiatric causes of behavioral symptoms. Residents do not receive psychotropic drugs pursuant to a PRN order unless that medication is necessary to treat a diagnosed specific condition that is documented in the clinical record. All medications used to treat behaviors must have a clinical indication and be used in the lowest possible dose to achieve the desired therapeutic effect. All residents receiving medications used to treat behaviors should be monitored for:
a. Efficacy
b. Risks
c. Benefits
d. Harm or adverse consequences.
Facility staff should monitor resident's behavior pursuant to Facility policy using a behavioral monitoring chart or behavioral assessment record for residents receiving psychotropic medication. Facility staff should monitor behavioral triggers, episodes, and symptoms. Facility staff should document the number and/or intensity of symptoms.
During a review of the facility P&P titled, “Psychotropic Medication Use,” last reviewed 4/24/2025, the P&P indicated the facility should not use psychotropic medications to address behaviors without first determining if there is a medical, physical, functional, psychological, social or environmental cause of the resident's behaviors. It is the responsibility of the attending health care practitioner to inform the resident and/or resident representative of the initiation, reason for use, and the risks associated with the use of psychotropic medications, per facility policy or applicable state regulation. The informed consent will be obtained by the Prescriber prior to initiation of the psychotropic medication. The Facility shall verify informed consent prior to the administration of a psychotropic.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to develop and implement a comprehensive care plan (CP, ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to develop and implement a comprehensive care plan (CP, a plan that includes measurable objectives and timetables to meet the resident's physical, psychosocial and functional needs) for six of seven sampled residents (Resident 13, 102, 112, 70, 97, 82, and 2) by failing to: 1). Develop and implement a CP that included side effects and behavior monitoring for Resident 13's as needed (PRN) lorazepam (a medication used to relieve symptoms of anxiety [a mental health condition that may result in restlessness, irritability, feelings of nervousness, panic, and fear]) administration. 2). Ensure a care plan was developed in a timely manner for the use of lower side rails (SR - often metal rails that normally hang on the side of the resident's bed) for Resident 102. 3). Ensure a care plan was developed for the use of a low air loss mattress (LALM - a mattress that helps prevent and treat pressure injuries by circulating air and relieving pressure on the body) for Residents 112 and 70. 4). Ensure a care plan was developed and implemented for the use of anticoagulant (a type of medication that prevents the blood from clotting too easily) Eliquis (also known as apixaban) for Resident 2. 5). Implement Resident 82's CP for risk of falls to keep the resident's room safe and provide a clutter-free environment. These deficient practices had the potential to result in miscommunication among interdisciplinary staff, residents, and resident representatives resulting in a delay in the delivery of necessary care and services to residents. 6). Develop and implement a CP for Resident 97's risk for elopement (the act of leaving a facility unsupervised and without prior authorization). This deficient practice resulted in Resident 97 eloping on 7/25/2025 at 12:14 p.m. Cross Reference F686 Findings: a. During a review of Resident 13’s admission Record (AR), the AR indicated the facility admitted the resident on 6/25/2025 with diagnoses that included traumatic subarachnoid hemorrhage with loss of consciousness, lack of coordination, muscle weakness, gastrostomy, depression, and anxiety disorder.
During a review of Resident 13’s History and Physical (H&P), dated 6/27/2025, the H&P indicated the resident could not make their own decisions but was able to make needs known.
During a review of Resident 13’s Minimum Data Set (MDS – resident assessment tool) dated 7/2/2025, the MDS indicated the resident was sometimes able to understand others and was sometimes able to make themself understood. The MDS further indicated that the resident was dependent on staff for toileting, bathing, and lower body dressing; and required substantial/maximal assistance for upper body dressing, personal hygiene, and transferring from bed to chair. The MDS indicated the resident was administered the following high-risk medications (drugs that can cause significant patient harm if used incorrectly): antianxiety.
During a review of Resident 13’s Order Summary Report, the Order Summary Report indicated the following physician’s orders:
-Administer lorazepam oral tablet five milligrams (mg, a unit of measurement) one tablet via GT every 12 hours PRN for anxiety, dated 6/25/2025 and discontinued on 7/29/2025.
- Administer lorazepam oral tablet five mg, give tablet by mouth every 12 hours PRN for anxiety, dated 7/29/2025.
During a concurrent interview and record review on 7/31/2025 at 8:53 a.m., with Registered Nurse (RN) 3, RN 3 reviewed Resident 13’s physician orders and CPs. RN 3 stated psychotropic medications (medications that affect the mind, emotions, and behavior) have side effects (adverse effects - unwanted or dangerous medication-related side effects) like increased confusion and increased risk for falls leading to injury. RN 3 stated psychotropics should be monitored for specific measurable behaviors to determine when to administer the medication. RN 3 stated CPs are used by the interdisciplinary team (IDT) to guide the care of a resident and to assist the IDT to determine interventions to implement for a resident and time specific goals. RN 3 stated it is the facility’s process to create CPs for psychotropic medication like lorazepam to ensure resident specific behaviors and side effects are monitored while a resident is administered lorazepam. RN 3 stated Resident 13 had a CP for the use of lorazepam that indicated there was a black box warning (a serious warning given by the Federal Drug Administration for drugs or drug classes that may cause serious harm or death), but there was not a CP for monitoring for behaviors or side effects of the medication. RN 3 stated without a CP for monitoring, there is no plan or guide for how to properly care for the resident. RN 3 stated when Resident 13 did not have a CP for monitoring behaviors or side effects of PRN lorazepam there was a potential that the resident would not be monitored for behaviors or side effects of the medication potentially resulting in harm to the resident.
During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the Assistant Director of Nursing (ADON), the ADON reviewed the facility policy and procedures (P&P) regarding CPs. The ADON stated CPs are a communication tool that have resident specific goals and interventions and effects the care of the resident. The ADON stated a resident on PRN lorazepam must have a CP that includes monitoring behaviors and side effects of the medication. The ADON stated when Resident 13 did not have a CP for the monitoring of behaviors and side effects of PRN lorazepam the facility P&P was not followed.
b. During a review of Resident 102’s admission Record, the admission Record indicated the facility admitted the resident on 5/14/2024 with diagnoses including tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), lack of coordination, and gastrostomy (GT - a surgical opening fitted with a device to allow feedings to be administered directly to the stomach common for people with swallowing problems).
During a review of Resident 102’s History and Physical (H&P) dated 5/14/2025, the H&P indicated Resident 102 was incapacitated (refers to a state in which an individual was unable to make sound decisions or manage their affairs).
During a review of Resident 102’s MDS, dated [DATE], the MDS indicated Resident 102 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make his needs known. The MDS further indicated Resident 102 required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive).
During a review of Resident 102’s CP on the use of lower SR up per family preference or request initiated on 7/29/2025 and the use of bilateral half upper SR up and locked when in bed initiated on 6/6/2024, the CP indicated to attempt to use less restrictive devices on an ongoing basis as one of the interventions to prevent or reduce incidence of injury or fall.
During a review of Resident 102’s Order Summary Report dated 8/1/2025, the Order Summary Report indicated the following physician’s orders:
-10/8/2024 and last revised on 7/29/2025: The order indicated staff may put lower SR up for preference or family request. Informed consent obtained from the responsible party (RP) by the physician (MD) after explanation of risks and benefits.
-5/18/2024 and last revised on 7/30/2025: bilateral upper half SR up and locked when in bed secondary to involuntary movement by gravity due to elevated head of bed.
During a concurrent observation and interview on 7/29/2025 at 11:53 a.m. while inside Resident 102’s room with RN 7, RN 7 stated Resident 102’s both upper and lower SR were up. RN 7 stated that from her knowledge, Resident 102 is not supposed to have both upper and lower SR up. RN 7 stated usually the Certified Nursing Assistants (CNAs) put all 4 SR up while providing care for resident safety when turning but they must put down the lower SR after providing care. RN 7 stated Resident 102’s bilateral lower SR should have been lowered down as it was restricting the resident’s freedom of movement and can be considered a restraint. Resident 102 can get trapped in between the SR and get injured.
During a concurrent interview and record review on 7/31/2025 at 2:30 p.m., Resident 102’s physician’s order, and CP were reviewed with RN 3. RN 3 stated Resident 102 had a physician’s order for bilateral half upper SR and locked while in bed dated 5/18/2024 and revised 7/30/2025 and an order that staff may put lower SR up for preference or family request dated 10/8/2024 and was revised 7/26/2025. RN 3 stated the CP for the use of lower SR up was developed on 7/29/2025 and was not developed timely. RN 3 stated when an intervention is implemented on a resident, the care plan should be developed on the day the intervention was implemented such as the use of SR upon obtaining consent from the family. RN 3 stated Resident 102’s care plan for the use of lower SR up should have been developed timely on 7/26/2025 instead of 7/29/2025 as the care plan is important to establish goals and interventions appropriate for the residents and to ensure the staff are aware of the interventions for the resident’s safety and prevent delay in providing the care the resident needs.
During a concurrent interview and record review on 7/31/2025 at 4:15 p.m., Resident 102’s physician’s order, and CP were reviewed with the Director of Nursing (DON). The DON stated Resident 102 had a physician’s order for bilateral half upper SR and locked while in bed dated 5/18/2024 and was revised 7/30/2025 and may put lower SR up for preference or family request dated 10/8/2024 and was revised 7/26/2025. The DON stated the CP for the use of lower SR up was developed on 7/29/2025 and was not developed timely. The DON stated that when an intervention was implemented on a resident, the care plan should be developed on the day the intervention was implemented such as the use of SR upon obtaining consent from the family. The DON stated Resident 102’s care plan for the use of lower SR up should have been developed timely on 7/26/2025 instead of 7/29/2025 as the care plan is a guide for the staff to be aware of the interventions appropriate for the resident’s safety and prevent delay in providing the care the resident needs.
c. During a review of Resident 112’s admission Record, the admission Record indicated the facility admitted the resident on 7/15/2025 with diagnoses including Guillain-Barre Synromde (a condition in which the body's immune system [the body's defense against infections] attacks the nerves causing weakness, numbness or paralysis [occurs when a person is unable to make voluntary muscle movements]), tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), lack of coordination, and generalized muscle weakness.
During a review of Resident 112’s H&P dated 7/15/2025, the H&P indicated Resident 112 had fluctuating capacity to understand and make decisions.
During a review of Resident 112’s MDS, dated [DATE], the MDS indicated Resident 112 had some difficulty in new situations for cognition (mental action or process of acquiring knowledge and understanding) and was able to understand and make his needs known. The MDS further indicated Resident 112 required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive).
During a review of Resident 112’s Order Summary Report dated 8/1/2025, the Order Summary Report indicated a physician’s order dated 7/16/2025 for the use of a LALM for wound care and management.
During a review of Resident 112’s CP for risk for developing pressure sores (also known as bedsore - localized, pressure-related damage to the skin and/or underlying tissue usually over a bony prominence), and other types of skin breakdown initiated on 7/15/2025 and last revised on 7/28/2025, the CP did not indicate the LALM as an intervention to minimize the risk of skin breakdown or pressure sores.
During a review of Resident 112’s electronic health record (EHR), the EHR indicated that Resident 112’s current weight on 7/16/2025 was 123 lbs.
During an observation on 7/29/2025 at 11:12 a.m., while inside Resident 112’s room, Resident 112 was alert, responded by nodding or shaking his head and mouthing words, while lying on a LALM with the setting at 240 pounds (lbs. – a unit of measurement). Resident 112 stated he does not feel if the LALM was firm or soft as he was unable to feel anything.
During a concurrent interview and record review on 7/31/2025 at 9 a.m., Resident 112’s CP was reviewed on risk for developing pressure sores with Licensed Vocational Nurse (LVN) 8. LVN 8 stated the use of a LALM or any pressure relieving devices was not included in the CP as an intervention to minimize the risk of developing pressure sores. LVN 8 stated CP such as risk for development of pressure sore should include pressure relieving devices such as the LALM as soon as the resident was placed on it, so the staff is aware of the current interventions in place to prevent skin breakdown. LVN 8 stated Resident 112’s CP should have included the use of LALM or any pressure relieving devices to ensure that the staff in charge of Resident 112 were implementing the proper interventions needed to prevent skin breakdown.
During an interview on 7/31/2025 at 4:30 p.m. with the DON, the DON stated CPs related to skin integrity and prevention of development of pressure sores should be developed as soon as possible to reflect or include the use of LALM or any pressure relieving devices so the staff would be aware of the plan of care and the current interventions in place to properly take care of the residents. The DON stated Resident 112’s CP should have indicated the use of a LALM or any pressure relieving devices as one of the interventions as it placed Resident 112 at risk for skin breakdowns if the staff are not aware of the interventions to provide the care the resident needs.
d. During a review of Resident 70’s admission Record, the admission Record indicated the facility originally admitted the resident on 6/30/2022 and readmitted the resident into the facility on 5/22/2023 with diagnoses including hemiplegia (total paralysis of the arm, leg, and trunk on the same side of the body) left non-dominant side, tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), and anxiety disorder (a mental health condition where excessive fear and worry interfere with daily life, and causing significant distress).
During a review of Resident 70’s CP on risk for developing pressure sore (also known as bedsore - localized, pressure-related damage to the skin and/or underlying tissue usually over a bony prominence), and other types of skin breakdown initiated on 7/18/2022, the CP did not indicate the LALM as an intervention to minimize the risk of skin breakdown or pressure sore.
During a review of Resident 70’s Order Summary Report dated 8/1/2025, the Order Summary Report indicated a physician’s order dated 11/7/2023 for the use of LALM for wound care and management.
During a review of Resident 70’s MDS, dated [DATE], the MDS indicated Resident 70 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make his needs known. The MDS further indicated Resident 70 required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive).
During a review of Resident 70’s H&P dated 7/15/2025, the H&P indicated Resident 70 was incapacitated (refers to a state in which an individual was unable to make sound decisions or manage their affairs).
During an observation on 7/29/2025 at 10:18 a.m., while inside Resident 70’s room, Resident 70 was lying on a LALM with the machine that was beeping with an orange blinking light indicating “low pressure.”
During a concurrent interview and record review on 7/31/2025 at 9 a.m., Resident 70’s CP regarding the risk for developing pressure sores was reviewed with LVN 8. LVN 8 stated the use of a LALM or any pressure relieving devices were not included in the CP as an intervention to minimize the risk of developing pressure sores. LVN 8 stated CP such as risk for development of pressure sore should include pressure relieving devices such as the LALM as soon as the resident was placed on it, so the staff are aware of the current interventions in place to prevent skin breakdown. LVN 8 stated Resident 70’s CP should have included the use of a LALM or any pressure relieving devices to ensure that the staff in charge of Resident 70 were implementing the proper interventions needed to prevent skin breakdown.
During an interview on 7/31/2025 at 4:30 p.m. with the DON, the DON stated CPs related to skin integrity and prevention of development of pressure sores should be developed as soon as possible to reflect or include the use of LALM or any pressure relieving devices, so the staff would be aware of the plan of care, and the current interventions in place to properly take care of the residents. The DON stated Resident 70’s CP should have indicated the use of LALM or any pressure relieving devices as one of the interventions as it placed Resident 70 at risk for skin breakdowns, if the staff are not aware of the interventions to provide the care the resident needs.
e. During a review of Resident 2’s admission Record, the admission Record indicated the facility admitted the resident on 6/27/2025 with diagnoses including pneumonia (an infection/inflammation in the lungs), tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), acute embolism and thrombosis (blockage in a blood vessel) of the deep veins of the left lower extremity, and long term use of anticoagulants.
During a review of Resident 2’s H&P dated 6/28/2025, the H&P indicated Resident 2 did not have the capacity to understand and make decisions.
During a review of Resident 2’s MDS, dated [DATE], the MDS indicated Resident 2 had an intact cognition (mental action or process of acquiring knowledge and understanding) and was able to understand and make his needs known. The MDS further indicated Resident 2 required partial/moderate assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive).
During a review of Resident 2’s Order Summary Report dated 8/1/2025, the Order Summary Report indicated the following physician’s orders dated 7/15/2025
-Administer Eliquis oral tablet five (5) milligrams (mg – a unit of measurement) one (1) tablet via GT every 12 hours for deep vein thrombosis prophylaxis (refers to measures taken to prevent diseases or infections before they occur).
-Monitor for discolored urine, black tarry stools, sudden severe headache, nausea and vomiting, diarrhea, muscle/joint pain, sleepiness, bruising, sudden changes in mental status and/or vital signs, shortness of breath, bleeding in any orifice (a hole or opening), abnormal laboratory results. Document: 'N' if monitored and none of the above observed. Document: 'Y' if monitored and any of the above observed, Notify physician and document in nurses' progress notes.
During a review of Resident 2’s CP, there was no CP developed and implemented for the use Eliquis.
During a concurrent interview and record review on 7/31/2025 at 4:30 p.m., Resident 2’s physician’s orders and CP for the use of Eliquis were reviewed with the DON. The DON stated there was no CP developed and implemented for Resident 2’s use of Eliquis that was ordered on 7/15/2025. The DON stated there was a CP developed for the use of Lovenox (also known as enoxaparin, another type of anticoagulant) but the CP was not developed for Eliquis when the Lovenox was discontinued and changed to Eliquis. The DON stated every time there is a change with the medication, a CP should be developed for the medication specially a high-risk medication such as Eliquis so the staff would be aware of the resident’s current plan of care and the current interventions in place to provide the care the residents need. The DON stated Resident 2’s CP should have been developed for the use of Eliquis to ensure the staff are aware of Resident 2’s current plan of care and interventions in place to properly care for the residents. The DON stated if the CP was not developed for Resident 2’s Eliquis, the staff would not know what interventions are in place to care for the residents which could lead to a delay in providing the care the resident needs.
f. During a review of Resident 82’s admission Record, the admission Record indicated the facility originally admitted the resident on 4/3/2024 and readmitted the resident on 4/3/2025 with diagnoses that included unspecified (unconfirmed) encephalopathy (a change in how the brain works due to an underlying condition), difficulty in walking, and generalized muscle weakness.
During a review of Resident 82’s H&P, dated 10/22/2024, the H&P indicated the resident has the capacity to understand and make decisions.
During a review of Resident 82’s Fall Risk Assessment (FRA), dated 4/11/2025, the FRA indicated the resident was a fall risk with history of fall in the last 12 months, continent in elimination status, and had adequate vision.
During a review of Resident 82’s IDT-Fall Risk/Compliance, dated 4/11/2025, the IDT-Fall Risk/Compliance indicated that the resident’s room be arranged to a position that will provide more space, free from clutter and adequate lighting to promote a safe environment and to modify resident’s environment to minimize exposure to items that could cause potential harm/injury.
During a review of Resident 82’s MDS, dated [DATE], the MDS indicated the resident had adequate hearing, clear speech, makes self-understood and had the ability to understand others. The MDS indicated that the resident has functional limitation in range of motion (extent of movement of a joint) on one side of his lower extremity that interfered with daily functions or placed the resident at risk of injury. The MDS indicated that the resident normally used a wheelchair as a mobility device (device designed to assist individuals with impaired movement). The MDS indicated that the resident maintained full continence for both urinary and bowel functions.
During a review of Resident 82’s Bowel and Bladder (B&B) Program Screener, dated 7/12/2025, the B&B Program Screener indicated that the resident was continent of both bowel and bladder.
During a concurrent observation and interview on 7/30/2025 at 9:03 a.m. with Resident 82, while at Resident 82’s bedside, Resident 82 stated he could not use the restroom right away because his two roommates’ overbed tables were obstructing his way going to the restroom. Resident 82 stated he could injure himself trying to move the tables himself. Resident 82 stated he would need to call and wait for the staff to come in and move the tables out of the way. Two overbed tables were observed at the foot of the residents’ beds and against the wall. Resident 82 stated he could injure himself trying to move the tables himself.
During a concurrent observation and interview on 7/31/2025 at 9:28 a.m. with CNA 4, while outside of Resident 82’s room, CNA 4 stated she is the assigned CNA to Resident 82. CNA 4 stated there are two overbed tables at the foot of the residents’ bed and by the wall. CNA 4 stated Resident 82 would need to ask her or another staff member to move the overbed tables out to pass to go to the restroom. CNA 4 stated Resident 82 could not move the tables out by himself, and she would need to move them for him. CNA 4 stated Resident 82’s two roommates do not like their overbed tables, so she placed them by the wall.
During an interview on 8/1/2025 at 3:13 p.m. with the ADON, the ADON stated that a safe and clutter-free environment in the resident’s room would be anything that could be in the way of the resident that can cause a hazard such as an obstructed pathway and a wet floor. The ADON stated the resident could potentially fall. The ADON stated the overbed tables obstructing the way of another resident is a hazard and should be moved. The ADON stated if the residents do not want their overbed tables then education should be provided by the residents, including why it would be dangerous for the other residents in that room. The ADON stated the purpose of the care plan is to have specific goals and have interventions, it is a communication tool. The ADON stated not implementing the care plan affects delivery of care provided and the place the residents at increased risk of falls.
g. During a review of Resident 97’s admission record (AR), the AR indicated the facility admitted Resident 97 on 4/3/2024 and readmitted the resident on 5/10/2024 with diagnoses that included aphasia, dysphagia, and depression (a mental health condition that makes you feel persistently sad and lose interest in things you usually enjoy).
During a review of Resident 97’s Change of Condition (COC– when there is a sudden change in a resident’s condition) interaction assessment form, dated 1/29/2025 at 9 p.m., the COC interaction assessment form indicated Resident 97 eloped and fell in front of the facility. The nursing notes indicated at 9 p.m. notified by CNA and LVN that Resident 97 was walking on Riverside past subacute and attempting to cross Riverside. CNA and LVN were able to bring Resident 97 back to the facility, as he was walking up the stairs, lost his footing and fell.
During a review of Resident 97’s care plan for elopement, initiated on 1/29/2025, the care plan indicated Resident 97 sometimes leaves the facility without authorization and permission. The care plan interventions included to administer medications as ordered, notify physician and responsible party of COC, and staff will assist with activities of residents’ choice.
During a review of Resident 97’s MDS, dated [DATE], the MDS indicated Resident 97 sometimes understood and was sometimes able to be understood. The MDS indicated Resident 97 coughed and choked during meals or when swallowing medications.
During a review of Resident 97’s Elopement Evaluation, dated 5/18/2025, the Elopement Evaluation indicated Resident 97 had an elopement score of 1 (score value of 1 or higher indicates risk for elopement).
During a review of Resident 97’s H&P, dated 5/22/2025, the H&P indicated Resident 97 did not have the capacity to understand and make decisions.
During a review of Resident 97’s COC interact assessment dated [DATE] at 5:20 p.m., the COC interact assessment indicated Resident 97 eloped. The nursing notes indicated at 5 p.m., while passing dinner trays, CNA 2 noted that Resident 97 was not in his assigned room. CNA 2 informed RN 2, who immediately initiated a thorough search of the facility. A code green (missing resident) was activated to alert all facility staff and initiate a coordinated facility wide search. At approximately 6:30 p.m. RN 2 contacted the DON to report the incident, provide a timeline and give an update of search effort. RN 2 then notified the local police department and reported Resident 97 as missing and requested assistance with the search. RN 2 contacted both Resident 97’s sisters to inform them of the situation and to verify whether they had seen or heard form Resident 97, neither reported recent contact with Resident 97.
During an interview on 7/30/2025 at 11:48 a.m. with CNA 1, CNA 1 stated she worked on 7/25/2025 and Resident 97 was her (CNA 1) resident that day. CNA 1 stated the last time she saw Resident 97 on 7/25/2025 was around 11:15 a.m. to 11:20 a.m. prior to lunch, he was in his (Resident 97) room. CNA 1 stated for lunch she passed Resident 97’s tray out and placed it by his bedside table, saw the bathroom door closed, CNA 1 stated Resident 97 was independent with bowel and bladder and assumed Resident 97 was in the bathroom. CNA 1 stated she went to pick up the tray sometime after 1p.m. and noted nothing had been eaten. The bathroom door was still closed. CNA 1 stated she did not knock on or open the door to check if Resident 97 was in the bathroom.
During an interview on 7/30/2025 at 1:29 p.m. with LVN 1, LVN 1 stated LVN 1 was the nurse for Resident 97 on 7/25/2025 for the 7 a.m. to 3 p.m. shift and checked Resident 97’s blood sugar around 11 a.m. to 12 p.m. LVN 1 stated Resident 97 does cry and gestures he wants to go home by clinging onto his family members when they show up. LVN 1 stated Resident 97 has never eloped and is not an elopement risk. LVN 1 stated was not aware of Resident 97 elopement in January. LVN 1 stated during shift change they are told which residents are elopement risk.
During an interview on 7/30/2025 at 2:13 p.m. with RN 1, RN 1 stated RN 1 on 7/25/2025. RN1 stated RN 1 was not aware Resident 97 was an elopement risk but was told later Resident 97 tried to elope prior. RN 1 stated last time she saw Resident 97 was around 12 p.m. and saw Resident 97 at the nurses’ station by the intravenous (IV-within a vein) cart and was walking around.
During an interview on 7/30/2025 at 3 p.m. with CNA 2, CNA 2 stated that when she (CNA 2) comes in she receives a verbal hand off and we do hand off at the nurses’ station. This is done by the nurse to the CNAs. The CNA that works the 7-3 does not give report but usually gets report on the basics such as the resident is out on pass or they have an appointment. CNA 2 stated CNA2 worked on 7/25/2025 around 3p.m. did her rounds and did not see Resident 97.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility's licensed nursing staff failed to provide care in accordance with profession...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility's licensed nursing staff failed to provide care in accordance with professional standards for: 1. Three of three sampled residents (Residents 21, 103, and 8) reviewed for insulin (a hormone that removes excess sugar from the blood, can be produced by the body or given artificially via medication) use by failing to rotate (a method to ensure repeated injections are not administered in the same area) subcutaneous (sq, beneath the skin) insulin administration sites. The deficient practice had the potential for adverse effect (unwanted, unintended result) of the same site subcutaneous administration of insulin such as excessive bruising, lipodystrophy (abnormal distribution of fat) and cutaneous amyloidosis (is a condition in which clumps of abnormal proteins called amyloids build up in the skin). 2. One of tour sampled Residents (Resident 97) reviewed for accidents by failing to: a. Develop a comprehensive person-centered care plan for Resident 97's risk for elopement (the act of leaving a facility unsupervised and without prior authorization). This deficient practice resulted in Resident 97 eloping on 7/25/2025 at 12:14 p.m. b. Provide supervision for Resident 97 during all meals as ordered. This deficient practice had the potential for Resident 97 to aspirate (food, liquid, or saliva accidentally enters the airway or lungs instead of going down the esophagus [food pipe] to the stomach). c. Monitor Resident 97 for Falling Star Program. This deficient practice had the potential for Resident 97 to have a fall. d. Monitor Resident 97 blood pressure (the pressure of circulating blood against the walls of blood vessels) as ordered. e. Provide monitoring to Resident 97 per facility policy and procedures (P&P) titled, Monitoring Residents, that indicated every two (2) hour monitoring from the nursing department. f. Perform shift change endorsement for Resident 97 per facility P&P titled, Shift-Change Endorsement Policy, that indicated to conduct endorsement at bedside. This deficient practice had the potential to negatively affect Resident 97. Cross reference F684, F689, and F760 Findings:
1.During a review of Resident 21’s admission Record, the admission Record indicated the facility admitted the resident on 12/3/2024, and readmitted the resident on 12/17/2024, with diagnoses including Type 2 diabetes mellitus (DM, a disorder characterized by difficulty in blood sugar control and poor wound healing) with diabetic neuropathy (disease or dysfunction of one or more nerves, typically causing numbness or weakness in the hands and feet), and diabetic chronic kidney disease (a condition where diabetes damages the kidneys, making them less effective at filtering waste from the blood).
During a review of Resident 21’s History and Physical (H&P), dated 12/18/2024, the H&P indicated the resident had the capacity to understand and make decisions.
During a review of Resident 21’s Minimum Data Set (MDS - a resident assessment tool), dated 6/26/2025, the MDS indicated the resident had the ability to make self-understood and understand others and had intact cognition (means that a person's mental abilities are working well and are not impaired). The MDS indicated the resident was on a high-risk drug class hypoglycemic medication (refers to drugs that helplowerhigh blood sugar levels).
During a review of Resident 21’s Order Summary Report, dated 3/14/2025, the Order Summary Report indicated an order for:
Insulin Glargine Subcutaneous Solution (Insulin Glargine). Inject 22 unit (is a way to measure the amount of insulin needed to help the body use blood sugar [glucose] properly) subcutaneously in the evening for DM 2 (Rotate injection site) hold for blood sugar (BS) less than (<) 100.
Insulin Aspart Injection Solution 100 units per milliliters (unit/ml, ow much insulin is packed into a given volume of liquid) (Insulin Aspart). Inject as per sliding scale (adjusting the amount of insulin a person takes based on their current blood sugar level): if 70 - 150 = 0 unit and follow hypoglycemia (low blood sugar) protocol and call MD; 151 - 200 = 2 unit; 201 - 250 = 4 unit; 251 - 300 = 6 unit; 301 - 350 = 8 unit; 351 - 400 = 10 unit call MD if BS greater than (>) 400, subcutaneously before meals for DM 2. Rotate injection site Give 8 ounces (oz, a unit of volume) of orange juice for BS < 70 and Inject 4 unit subcutaneously before meals for DM.
Insulin Aspart Injection Solution (Insulin Aspart). Inject as per sliding scale: if 70 - 150 = 0 unit and follow hypoglycemia protocol and call MD; 151 - 200 = 2 unit; 201 - 250 = 4 unit; 251 - 300 = 6 unit; 301 - 350 = 8 unit; 351 - 400 = 10 unit, call MD if BS >400, subcutaneously at bedtime for DM 2 (rotate injection site) Give 8 oz of orange juice for BS <70 and Inject 4 unit subcutaneously at bedtime for DM.
During a review of Resident 21’s Location of Administration Report of insulin for 5/2025 to 7/2025, the Location of Administration Report indicated:
-Insulin Aspart Injection Solution 100 unit/ml was administered on,
7/2/2025 at 11:26 a.m. on the Abdomen – Left Lower Quadrant (LLQ)
7/2/2025 at 11:30 a.m. on the Abdomen – LLQ
7/2/2025 at 5:28 p.m. on the Abdomen – Right Lower Quadrant (RLQ)
7/3/2025 at 12:31 p.m. on the Abdomen – RLQ
7/4/2025 at 4:49 p.m. on the Abdomen - LLQ
7/4/2025 at 4:50 p.m. on the Abdomen – LLQ
7/6/2025 at 2:29 p.m. on the Abdomen – Left Upper Quadrant (LUQ)
7/6/2025 at 6:24 p.m. on the Abdomen – LUQ
7/7/2025 at 4:47 p.m. on the Abdomen – Right Upper Quadrant (RUQ)
7/8/2025 at 8:03 a.m. on the Abdomen – RUQ
7/9/2025 at 5:13 p.m. on the Abdomen - RUQ
7/10/2025 at 6:31 a.m. on the Abdomen - RUQ
7/10/25 at 6:32 a.m. on the Abdomen – RUQ
7/10/2025 at 5:20 p.m. on the Abdomen - LLQ
7/10/2025 at 5:20 p.m. on the Abdomen – LLQ
7/12/2025 at 6:26 a.m. on the Abdomen - LLQ
7/12/2025 at 6:27 a.m. on the Abdomen - LLQ
7/12/2025 at 4:17 p.m. on the Abdomen – LLQ
7/13/2025 at 11:35 a.m. on the Abdomen - RLQ
7/13/2025 at 11:35 a.m. on the Abdomen - RLQ
7/13/2025 at 4:31 p.m. on the Abdomen - LLQ
7/13/2025 at 4:31 p.m. on the Abdomen – LLQ
7/13/2025 at 11:35 a.m. on the Abdomen - RLQ
7/13/2025 at 11:35 a.m. on the Abdomen - RLQ
7/13/2025 at 4:31 p.m. on the Abdomen - LLQ
7/13/2025 at 4:31 p.m. on the Abdomen – LLQ
7/16/2025 at 4:49 p.m. on the Abdomen - LLQ
7/16/2025 at 4:49 p.m. on the Abdomen - LLQ
7/17/2025 at 7:08 a.m. on the Abdomen - RLQ
7/17/2025 at 7:08 a.m. on the Abdomen - RLQ
7/17/2025 at 11:30 a.m. on the Abdomen - RLQ
7/17/2025 at 2:17 p.m. on the Abdomen – RLQ
7/18/2025 at 11:39 a.m. on the Abdomen - RLQ
7/18/2025 at 1:45 p.m. on the Abdomen – RLQ
7/19/2025 at 11:38 a.m. on the Abdomen - RLQ
7/19/2025 at 1:39 p.m. on the Abdomen – RLQ
7/21/2025 at 5:03 p.m. on the Abdomen - RUQ
7/21/2025 at 5:03 p.m. on the Abdomen - RUQ
7/22/25 at 11:31 a.m. on the Abdomen - LLQ
7/22/2025 at 11:31 a.m. on the Abdomen - LLQ
7/22/2025 at 4:44 p.m. on the Abdomen - RUQ
7/2220/25 at 4:44 p.m. on the Abdomen – RUQ
7/24/2025 at 5:46 a.m. on the Abdomen - LLQ
7/24/2025 at 5:47 a.m. on the Abdomen - LLQ
7/24/2025 at 11:30 a.m. on the Abdomen - RLQ
7/24/2025 at 2:47 p.m. on the Abdomen – RLQ
7/24/2025 at 4:16 p.m. on the Abdomen - LLQ
7/25/2025 at 4:33 p.m. on the Abdomen – LLQ
7/27/2025 at 5:45 p.m. on the Abdomen - RLQ
7/28/2025 at 7:16 a.m. on the Abdomen - RLQ
7/28/2025 at 7:16 a.m. on the Abdomen - RLQ
7/28/2025 at 11:27 a.m. on the Abdomen - LLQ
7/28/2025 at 11:28 a.m. on the Abdomen – LLQ
During a review of Resident 21’s Care Plan (CP) Report titled “Resident is at risk for hypoglycemia and hyperglycemia (high blood sugar) related to diabetes mellitus,” last revised on 1/3/2025, the CP Report indicated an intervention to administer medications as ordered.
During concurrent interview and record review on 7/31/2025, at 11:37 a.m., with Registered Nurse (RN) 3, reviewed Resident 21’s Medical Diagnosis, Order Summary Report, Location of Administration of insulin from 5/2025 to 7/2025, and Care Plan. RN 3 stated there were multiple instances where the licensed staff did not rotate the insulin administration sites of insulin on Resident 21. RN 3 stated the sites of insulin administration should be rotated to prevent irritation, pain and discomfort on the frequented sites of administration. RN 3 also stated the sites of administration of insulin was also rotated to prevent lipodystrophy on residents. RN 3 stated injecting insulin on the sites of lipodystrophy can render the insulin ineffective due to poor absorption that can lead to hyper or hypoglycemia on Resident 21. RN 3 stated their current electronic medication administration record had a capability of checking where the last site of administration of insulin and there was no reason for the licensed staff to repeat the site of insulin administration.
During an interview on 8/1/2025, at 2:05 p.m., with the Assistant Director of Nursing (ADON), the ADON stated the licensed staff should have rotated the insulin administration sites to Resident 21 to prevent skin irritation and lipodystrophy. The ADON stated that administering insulin on the same site can cause lipodystrophy that could affect the absorption of insulin leaving them ineffective to lower the blood sugar level of Resident 21.
During a review of the facility's recent policy and procedure (P&P) titled Insulin Administration, last reviewed on 4/24/2025, the P&P indicated to provide guidelines for the safe administration of insulin to residents with diabetes.
Steps in the Procedure (Insulin Injections via Syringe)
8. Select an injection site.
a. Insulin may be injected into the subcutaneous tissue of the upper arm, and the anterior or lateral areas of the thighs and abdomen. Avoid the area approximately 2 inches around the navel.
b. Injection sites should be rotated, preferably within the same general area (abdomen, thigh, upper arm).
During a review of the facility-provided Highlights of Prescribing Information on the use of Insulin Aspart injection, for subcutaneous or intravenous use, with initial U.S. approval in 2000, the Highlights of Prescribing Information indicated to rotate injection sites within the same region from one injection to the next to reduce risk of lipodystrophy and localized cutaneous amyloidosis.
During a review of the facility-provided Highlights of Prescribing Information on the use of Lantus (insulin glargine injection) for subcutaneous injection, with initial U.S. approval in 2000, the Highlights of Prescribing Information indicated to rotate injection sites to reduce the risk of lipodystrophy.
2. During a review of Resident 103’s admission Record, the admission Record indicated the facility admitted the resident on 10/30/2024, with diagnoses including type 2 diabetes mellitus, end stage renal disease (the final, permanent stage of chronic kidney disease, where kidney function has declined to the point that the kidneys can no longer function on their own), and metabolic encephalopathy (a condition where the brain's function is impaired due to chemical imbalances in the body, often caused by an underlying illness or organ dysfunction).
During a review of Resident 103’s MDS, dated [DATE], the MDS indicated the resident sometimes had the ability to make self-understood and sometimes had the ability to understand others and had short-term and long-term memory problem. The MDS indicated the resident was on a high-risk drug class hypoglycemic medication.
During a review of Resident 103’s Order Summary Report, dated 10/31/2024, the Order Summary Report indicated an order for:
Insulin Aspart Injection Solution 100 unit/ml (Insulin Aspart). Inject as per sliding scale: if 70 - 140 = 0 unit; 141 - 180 = 2 unit; 181 - 220 = 4 unit; 221 - 260 = 6 unit; 261 - 300 = 8 unit; 301 - 350 = 10 unit; 351 - 400 = 12 unit; call/notify MD for BS >400, subcutaneously before meals and at bedtime for DM 2 (Rotate injection site). Give 8 oz of orange juice for BS <70.
Insulin Glargine-yfgn Subcutaneous Solution 100 unit/ml (Insulin Glargine-yfgn). Inject 22 unit subcutaneously at bedtime for DM 2 hold for BS <100 Rotate injection site.
During a review of Resident 103’s Location of Administration Report of insulin for 5/2025 to 7/2025, the Location of Administration Report for insulin indicated:
Insulin Glargine-yfgn Subcutaneous Solution 100 unit/ml was administered on,
7/4/2025 at 9:49 p.m. on the Abdomen - RUQ
7/5/2025 at 10:45 p.m. on the Abdomen – RUQ
Insulin Aspart Injection Solution 100 unit/ml was administered on,
7/5/2025 at 11:20 a.m. on the Abdomen - LLQ
7/5/2025 at 4 p.m. on the Abdomen – LLQ
7/5/2025 at 8:06 p.m. on the Abdomen - RLQ
7/6/2025 at 7:23 a.m. on the Abdomen – RLQ
7/6/2025 at 4:09 p.m. on the Abdomen - LUQ
7/6/2025 at 8:45 p.m. on the Abdomen – LUQ
7/14/2025 at 4:55 p.m. on the Abdomen - RLQ
7/14/2025 at 9:08 p.m. on the Abdomen – RLQ
7/17/2025 at 9:34 p.m. on the Abdomen - RUQ
7/18/2025 at 7:34 a.m. on the Abdomen – RUQ
7/22/2025 at 9:41 p.m. on the Abdomen - RLQ
7/23/2025 at 7:13 a.m. on the Abdomen – RLQ
7/25/2025 at 7:27 a.m. on the Abdomen - RLQ
7/25/2025 at 11:38 a.m. on the Abdomen - RLQ
7/26/2025 at 4:03 p.m. on the Arm - left
7/26/2025 at 9:48 p.m. on the Arm – left
During a review of Resident 103’s CP Report titled “Resident is at risk for hypoglycemia and hyperglycemia related to diabetes mellitus,” last revised on 12/3/2024, the CP Report indicated an intervention to administer medications as ordered.
During a concurrent interview and record review on 7/31/2025, at 11:37 a.m., with RN 3, reviewed Resident 103’s Medical Diagnosis, Order Summary Report, Location of Administration of insulin from 5/2025 to 7/2025, and Care Plan. RN 3 stated there were multiple instances where the licensed staff did not rotate the insulin administration sites of insulin on Resident 103. RN 3 stated the sites of insulin administration should be rotated to prevent irritation, pain and discomfort on the frequented sites of administration. RN 3 also stated the sites of administration of insulin was also rotated to prevent lipodystrophy on residents. RN 3 stated injecting insulin on the sites of lipodystrophy can render the insulin ineffective due to poor absorption that can lead to hyper or hypoglycemia on Resident 103. RN 3 stated their current electronic medication administration record had a capability of checking where the last site of administration of insulin and there was no reason for the licensed staff to repeat the site of insulin administration.
During an interview on 8/1/2025, at 2:05 p.m., with the ADON, the ADON stated the licensed staff should have rotated the insulin administration sites to Resident 103 to prevent skin irritation and lipodystrophy. The ADON stated that administering insulin on the same site can cause lipodystrophy that could affect the absorption of insulin leaving them ineffective to lower the blood sugar level of Resident 103.
During a review of the facility's recent P&P titled Insulin Administration, last reviewed on 4/24/2025, the P&P indicated to provide guidelines for the safe administration of insulin to residents with diabetes.
Steps in the Procedure (Insulin Injections via Syringe)
8. Select an injection site.
a. Insulin may be injected into the subcutaneous tissue of the upper arm, and the anterior or lateral areas of the thighs and abdomen. Avoid the area approximately 2 inches around the navel.
b. Injection sites should be rotated, preferably within the same general area (abdomen, thigh, upper arm).
During a review of the facility-provided Highlights of Prescribing Information on the use of Insulin Aspart injection, for subcutaneous or intravenous use, with initial U.S. approval in 2000, the Highlights of Prescribing Information indicated to rotate injection sites within the same region from one injection to the next to reduce risk of lipodystrophy and localized cutaneous amyloidosis.
During a review of the facility-provided Highlights of Prescribing Information on the use of Lantus (insulin glargine injection) for subcutaneous injection, with initial U.S. approval in 2000, the Highlights of Prescribing Information indicated to rotate injection sites to reduce the risk of lipodystrophy.
3. During a review of Resident 8’s admission Record (front page of the chart that contains a summary of basic information about the resident), the admission Record indicated the facility originally admitted the resident on 5/4/2011 and readmitted in the facility on 5/12/2025, with diagnoses including dependence on respirator (also known as ventilator – a machine used to help a person breath when they are unable to do so on their own) status , contracture of muscle multiple sites, and type 2 diabetes mellitus (DM 2 - a disorder characterized by difficulty in blood sugar control and poor wound healing).
During a review of Resident 8’s History and Physical (H&P) dated 5/13/2025, the H&P indicated Resident 8 did not have the capacity to understand and make decisions.
During a review of Resident 8’s Minimum Data Set (MDS, a resident assessment tool), dated 6/1/2025, the MDS indicated Resident 8 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make her needs known. The MDS further indicated Resident 8 had impairment of both upper extremities and required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive). The MDS indicated Resident 8 received insulin.
During a review of Resident 8’s care plan (CP) on risk for hypoglycemia (low level of sugar in the blood) and hyperglycemia (high level of sugar in the blood) related to DM 2 initiated on 4/4/2014 and last revised on 4/16/2023, the CP indicated to administer insulin and medications as ordered as one of the interventions to prevent unrecognized signs and symptoms of hypoglycemia or hyperglycemia.
During a review of Resident 8’ Order Summary Report dated 8/1/2025, the Order Summary Report indicated the following physician’s orders:
-5/13/2025: Lantus (also known as insulin glargine, a long-acting insulin) subcutaneous solution 100 unit per milliliter (unit/ml – a unit of measurement. Inject ten (10) units subcutaneously at bedtime for DM2. Hold for blood sugar (BS) less than (< - a unit of measurement) 100. Rotate injection site.
-5/12/2025 and revised on 7/26/2025: Insulin aspart (a short acting insulin) flexpen subcutaneous solution pen-injector 100 unit/ml. Inject subcutaneously every 6 hours for DM2. Rotate injection site. Inject as per sliding scale: if 70 – 149, zero (0) and may give eight (8) ounces (oz – a unit of measurement) orange juice via gastrostomy (GT - a surgical opening fitted with a device to allow feedings to be administered directly to the stomach common for people with swallowing problems) if BS < 70. Recheck BS after 15 minutes and call physician (MD); for 150 - 199 = two (2) units; 200 - 249 = three (3) units; 250 - 299 = five (5) units; 300 - 349 = seven (7) units; 350 - 400 = 10 units; for BS more than (> - a unit of measurement) 350 notify or call MD; subcutaneously every 6 hours for DM2. Rotate injection site.
-7/26/2025: Insulin aspart (a short acting insulin) flexpen subcutaneous solution pen-injector 100 unit/ml. Inject subcutaneously every six (6) hours for DM2. Rotate injection site. Inject as per sliding scale: if 70 – 149, 0 and may give 8 oz orange juice via GT if BS < 70. Recheck BS after 15 minutes and call MD; for 150 - 199 = 2 units; 200 - 249 = 3 units; 250 - 299 = 5 units; 300 - 349 = 7 units; 350 - 400 = 10 units; for BS more than (> - a unit of measurement) 400 call MD; subcutaneously every 6 hours for DM2. Rotate injection site.
During a concurrent interview and record review on 7/30/2025 at 8:30 a.m. reviewed Resident 8’s physician’s orders, care plans, and location of administration sites for Lantus and insulin aspart from 6/2025 and 7/2025 with Registered Nurse (RN) 4. RN 4 stated Resident 8 had a physician’s order for Lantus and insulin aspart and were administered as follows:
-Lantus subcutaneous solution:
7/2/25 9:28p.m. subcutaneously Abdomen – right lower quadrant (RLQ)
7/3/25 9:05p.m. subcutaneously Abdomen – RLQ
7/5/25 8:07 p.m.subcutaneously Abdomen – left upper quadrant (LUQ)
7/6/25 8:07p.m. subcutaneously Abdomen – LUQ
7/19/25 9:06p.m. subcutaneously Abdomen – left lower quadrant (LLQ)
7/20/25 8:39 p.m. subcutaneously Abdomen – LLQ
Insulin aspart flexpen subcutaneous solution:
6/6/25 12:08 a.m. subcutaneously Abdomen – left upper quadrant (LUQ)
6/6/25 5:08 a.m. subcutaneously Abdomen – LUQ
6/13/25 11:33 p.m. subcutaneously Abdomen – LLQ
6/13/25 6:28 a.m. subcutaneously Abdomen – LLQ
RN 4 stated that the administration sites for insulin should be rotated per standards of practice, manufacturer’s guidelines, and per physician’s order to prevent hardening or lumps in the skin. RN 4 stated the location of administration sites for Resident 8’s Lantus and insulin aspart were not rotated. RN 4 stated there was a physician’s order to rotate administration sites. RN 4 stated Resident 8’s administration sites should have been rotated to prevent pain, redness, irritation, and lumps on the resident’s skin which can affect the absorption of the insulin.
During an interview on 8/1/2025 at 2:05 p.m. with the Assistant Director of Nursing (ADON), RN 4 stated that nurses are supposed to rotate the insulin administration sites as indicated in the physician’s order, manufacturer’s guideline, and according to professional standards of practice. The ADON stated Resident 8’s insulin administration sites should have been rotated as it placed Resident 8 at risk for development of lipodystrophy which may affect the absorption of the insulin and lead to hyperglycemia.
During a review of the facility’s policy and procedure (P&P) titled “Insulin Administration,” last reviewed on 4/24/2025, the P&P indicated a purpose to provide guidelines for the safe administration of insulin to residents with diabetes. The P&P further indicated:
-Select an injection site.
a. Insulin may be injected into the subcutaneous tissue of the upper arm, and the anterior or lateral areas of the thighs and abdomen. Avoid the area approximately 2 inches around the navel.
b. Injection sites should be rotated, preferrable within the same general area (abdomen, thigh, upper arm).
-Documentation.
4. Injection site (presence or absence of any bruise, pain, redness, swelling or unusual marks on or near the injection site.
During a review of the facility provided manufacturer’s guideline for Insulin Aspart Injection, last revised on 2/2023, the manufacturer’s guideline indicates to rotate injection sites within the same region from one injection to the next to reduce risk of lipodystrophy and localized cutaneous amyloidosis.
During a review of the facility provided manufacturer’s guideline on insulin glargine (Lantus) last revised 5/2019, the manufacturer’s guideline indicated to rotate injection sites to reduce the risk of lipodystrophy. The manufacturer’s guideline further indicated some of the adverse reactions commonly associated with Lantus include hypoglycemia, injection site reactions, lipodystrophy, rash, and edema.
4. During a review of Resident 97 admission Record (AR), the AR indicated the facility admitted Resident 97 on 4/3/2024, and readmitted the resident on 5/10/2024, with diagnoses included aphasia (a disorder that makes it difficult to speak), dysphagia (difficulty swallowing), history of falling, anxiety (a feeling of unease, worry, or fear), and depression (a mental health condition that makes you feel persistently sad and lose interest in things you usually enjoy).
During a review of Resident 97’s care plan for aspiration, initiated on 5/16/2024 and revised on 3/12/2025, the care plan indicated Resident 97 is at risk for aspiration of food and liquids secondary to dysphagia. The care plan interventions included monitor for sign and symptoms of aspiration (choking, shortness of breath [SOB], respiration changes, and to monitor tolerance of diet and fluids).
During a review of Resident 97’s care plan for self-care deficits, initiated on 7/29/2024, the care plan indicated Resident 97 eating assistance was total. The care plan intervention indicated to provide safe environment.
During a review of Resident 97’s Physician Orders, dated 10/29/2024, the Physician Orders indicated to monitor episodes of depression manifested by crying spells and tally by hashmarks for Zoloft (medication used to treat depression) every shift.
During a review of Resident 97’s Speech Therapy Discharge summary dated [DATE], the Speech Therapy Discharge Summary indicated Resident 97 will tolerate minced and moist (soft, moist, and easy to chew food) nectar thick liquids (liquids that have been thickened to a consistency slightly thicker than water but still pourable, similar to the consistency of fruit nectar or heavy syrup) three (3) meals a day with aspiration precautions. On 12/3/2024 Resident 97 was at severe risk for aspiration.
During a review of Resident 97’s Change of Condition (COC– when there is a sudden change in a resident’s condition) interaction assessment form, dated 1/29/2025 at 9 p.m., the COC interaction assessment form indicated Resident 97 eloped and fell in front of the facility. The nursing notes indicated at 9 p.m., Resident 97 was walking on the sidewalk in front of the facility and attempted to cross the street. The CNA and LVN were able to bring Resident 97 back to the facility and as Resident 97 was walking up the stairs, Resident 97 lost his footing and fell.
During a review of Resident 97’s care plan for elopement, initiated on 1/29/2025, the care plan indicated Resident 97 sometimes leaves the facility without authorization and permission. The care plan interventions included administer medications as ordered, notify physician and responsible party of COC, and staff will assist to activities of residents’ choice.
During a review of Resident 97’s [TRUNCATED]
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to provide the necessary care and services to attain or maintain the ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to provide the necessary care and services to attain or maintain the highest practicable physical well-being for one of four sampled residents (Resident 97) by failing to: 1. Develop a comprehensive person-centered care plan (a plan of care that summarizes a resident's health conditions, specific care and services facility staff need to provide a resident to promote healing and prevent a worsening of a condition, and current treatments) for Resident 97's risk for elopement (the act of leaving a facility unsupervised and without prior authorization). This deficient practice resulted in Resident 97 eloping on 7/25/2025 at 12:14 p.m. 2. Provide supervision for Resident 97 during all meals as ordered. This deficient practice had the potential for Resident 97 to aspirate (food, liquid, or saliva accidentally enters the airway or lungs instead of going down the esophagus [food pipe] to the stomach). 3. Monitor Resident 97 for Falling Star Program (assessing residents for their risk of falls and then identifying those at high risk with a visible symbol, usually a falling star graphic placed on the resident`s door). This deficient practice had the potential for Resident 97 to have a fall. 4. Monitor Resident 97 blood pressure (the pressure of circulating blood against the walls of blood vessels) as ordered. 5. Provide monitoring to Resident 97 per facility policy and procedures (P&P) titled, Monitoring Residents, that indicated every two (2) hour monitoring from the nursing department. 6. Perform shift change endorsement for Resident 97 per facility P&P titled, Shift-Change Endorsement Policy, that indicated to conduct endorsement at bedside. This deficient practice had the potential to negatively affect Resident 97. Cross reference F658 Findings: During a review of Resident 97 admission Record (AR), the AR indicated the facility admitted Resident 97 on 4/3/2024 and readmitted the resident on 5/10/2024 with diagnoses included aphasia (a disorder that makes it difficult to speak), dysphagia (difficulty swallowing), history of falling, anxiety (a feeling of unease, worry, or fear), and depression (a mental health condition that makes you feel persistently sad and lose interest in things you usually enjoy). During a review of Resident 97's care plan for aspiration, initiated on 5/16/2024 and revised on 3/12/2025, the care plan indicated Resident 97 is at risk for aspiration of food and liquids secondary to dysphagia. The care plan interventions included monitor for sign and symptoms of aspiration (choking, shortness of breath [SOB], respiration changes, and to monitor tolerance of diet and fluids). During a review of Resident 97's care plan for self-care deficits, initiated on 7/29/2024, the care plan indicated Resident 97 eating assistance was total. The care plan intervention indicated to provide safe environment. During a review of Resident 97's Physician Orders, dated 10/29/2024, the Physician Orders indicated to monitor episodes of depression manifested by crying spells and tally by hashmarks for Zoloft (medication used to treat depression) every shift. During a review of Resident 97's Speech Therapy Discharge summary dated [DATE], the Speech Therapy Discharge Summary indicated Resident 97 will tolerate minced and moist (soft, moist, and easy to chew food) nectar thick liquids (liquids that have been thickened to a consistency slightly thicker than water but still pourable, similar to the consistency of fruit nectar or heavy syrup) three (3) meals a day with aspiration precautions. On 12/3/2024 Resident was severe risk for aspiration. During a review of Resident 97's Change of Condition (COC- when there is a sudden change in a resident's condition) interaction assessment form, dated 1/29/2025 at 9 p.m., the COC interaction assessment form indicated Resident 97 eloped and fell in front of the facility. The nursing notes indicated at 9 p.m., Resident 97 was walking on the sidewalk in front of the facility and attempted to cross the street. The CNA and LVN were able to bring Resident 97 back to the facility and as Resident 97 was walking up the stairs, Resident 97 lost his footing and fell. During a review of Resident 97's care plan for elopement, initiated on 1/29/2025, the care plan indicated Resident 97 sometimes leaves the facility without authorization and permission. The care plan interventions included administer medications as ordered, notify physician and responsible party of COC, and staff will assist to activities of residents' choice. During a review of Resident 97's Minimum Data Set (MDS - a resident assessment tool), dated 5/17/2025, the MDS indicated Resident 97 sometimes understood and was sometimes able to be understood. The MDS indicated Resident 97 coughed and choked during meals or when swallowing medications. During a review of Resident 97's Elopement Evaluation, dated 5/18/2025, the Elopement Evaluation indicated Resident 97 had an elopement score of 1 (score value of 1 or higher indicates risk for elopement). During a review of Resident 97' Fall Risk Evaluation, dated 5/18/2025, the Fall Risk Evaluation indicated Resident 97 fall risk score was 7 (total score is 10 or greater, the resident should be considered at high risk for potential falls). The Fall risk Evaluation indicated Resident 97 had balance problems while walking. During a review of Resident 97's Physician Orders, dated 5/19/2025, the Physician Orders indicated falling star program, frequent visual monitoring due to higher risk for fall and injury, and document during every shift. During a review of Resident 97's care plan for falling star program, initiated on 5/19/2025, the care plan indicated Resident 97 was at risk for falls related to antihypertensive medication, auditory deficits (a type of hearing loss caused by something affecting the part of the brain that processes how you hear), balance deficits, cognitive impairment, decreased strength and endurance, history of falls, noncompliant with request for assistance nonuse of call lights, poor safety awareness and judgment, unsteady gait, difficulty in walking, and muscle weakness. The care plan intervention indicated to remind staff during huddle on resident high fall risk status, provide frequent visual monitoring, and place the resident close to nursing station for close observation. During a review of Resident 97's History and Physical (H&P - comprehensive assessment conducted by a healthcare provider that includes gathering a thorough medical history from the resident and performing a physical examination to assess their overall health and identify any potential medical concern), dated 5/22/2025, the H&P indicated Resident 97 did not have the capacity to understand and make decisions. During a review of Resident 97's Physician Orders, dated 5/30/2025, the Physician Orders indicated monitor blood pressure every six (6) hours. During a review of Resident 97's Medication Administration Record (MAR - a daily documentation record used by a licensed nurse to document medications and treatments given to a resident) for July 2025, the MAR indicated for 7/25/2025: - Falling star program frequent visual monitoring due to higher risk for falls and injuries document per shift, every shift, was left blank for the day shift. - Monitor blood pressure every six (6) hours, indicated a blood pressure of 110/62 mmHg millimeters of mercury (mmHg, unit of pressure, normal range is between 90/60 mmHg and 120/80 mmHg; low blood pressure is below 90/60 mmHg) During a review of Resident 97's Physician Orders, dated 7/9/2025, the Physician Orders indicated Controlled Carbohydrates (CCHO- meal plan where individuals aim to eat roughly the same amount of carbohydrates at each meal, helping to stabilize blood sugar levels) no added salt (NAS) diet, dysphagia mechanical soft texture (diet is used for people who have difficulty swallowing), nectar mild thick consistency, 3 meals, aspiration precautions, supervision during meals. During a review of Resident 97's Activities of Daily Living (ADLs- activities such as bathing, dressing and toileting a person performs daily) task for eating, the ADL task for eating for 7/25/2025 at 12:07 p.m. indicated Resident 97 was provided with setup or clean up assistance (helper sets up or cleans up resident completes activity helper assists only prior or following the activity). During a review of Resident 97's task nutritional amount eaten (%), the task nutritional amount eaten (%) for 7/25/2025 at 12:07 p.m. indicated Resident 97 ate 50% of his (Resident 97) meal. During a review of Resident 97's COC interact assessment dated [DATE] at 5:20 p.m., the COC interact assessment indicated Resident 97 eloped. The nursing notes indicated at 5 p.m., while passing dinner trays, CNA 2 noted that Resident 97 was not in his assigned room. CNA 2 informed Registered Nurse (RN) 2, who immediately initiated a thorough search of the facility. A code green (missing resident) was activated to alert all facility staff and initiate a coordinated facility wide search. At approximately 6:30 p.m., RN 2 contacted the Director of Nursing (DON) to report the incident, provide timeline and give update of search effort. RN 2 then notified the local police department and reported Resident 97 as missing and requested assistance with search. RN 2 contacted both Resident 97's sisters to inform them of the situation and to verify whether they had seen or heard form Resident 97, neither reported recent contact with Resident 97. During a concurrent interview and record review on 7/30/2025 at 11:48 a.m. with CNA, Resident 97's nutritional amount eaten (%) was reviewed. CNA 1 stated she (CNA 1) leaves Resident 97 meal tray on the bedside table. CNA 1 stated she (CNA1) was not aware Resident 97 had an order for supervision during all meals. CNA 1 stated she (CNA1) does not supervise Resident 97 during his meals; she just leaves the meal tray on the resident`s bedside table. During a concurrent interview and record review on 7/30/2025 at 1:29 p.m. with LVN 1, Resident 97's MAR was reviewed. LVN 1 stated he (LVN 1) was the assigned nurse for Resident 97 on 7/25/2025 for the 7a.m. to 3 p.m. shift. LVN 1 stated he checked Resident 97's blood sugar between 11 a.m. to 12 p.m. prior to lunch. LVN 1 stated he checks on residents from time to time but, for Resident 97, he did not check on him (Resident 97) anymore because Resident 97 is ambulatory and if Resident 97 needs anything he (Resident 97) will come and find staff. LVN 1 stated Resident 97 cries and gestures he wants to go home by clinging onto his family members when they show up. LVN 1 stated Resident 97 has never eloped and is not at elopement risk. LVN 1 stated he (LVN 1) was not aware of Resident 97 elopement in January. LVN 1 stated during shift change is told which residents are elopement risk. LVN 1 reviewed Resident 97's MAR and stated the blood pressure documented on 7/25/2025 at 12 p.m. was copied from the 8 a.m. blood pressure he (LVN 1) took. LVN 1 stated he (LVN 1) did not measure Resident 97`s blood pressure as ordered by the physician every six hours. LVN 1stated the potential outcome of not checking a Resident 97`s blood pressure is the inability to know if the resident`s blood pressure is high or low and can result in a delay in the interventions. During an interview on 7/30/2025 at 3 p.m. with CNA 2, CNA 2 stated that when she (CNA 2) comes in she gets verbal hand off, we do hand off at the nurses' station, this is done by the nurse to the CNAs the CNA that works the 7-3 does not give report, usually gets report on the basics like the resident is out on pass or they have an appointment. CNA 2 stated for eating Resident 97 eats by himself, CNA 2 stated we just need to assist if he drops something or needs help putting on shoes and showers in the morning. CNA 2 stated the only thing we do is uncover the top of the tray and uncover the drinks he is on puree diet, but he eats on own, CNA 2 stated not aware Resident 97 required supervision during meals. CNA 2 stated not aware Resident 97 was an elopement risk. During an interview on 7/30/2025 at 4:18 p.m. with RN 2, RN 2 stated Resident 97 is alert and oriented to self with confusion and walks around the facility without devices. RN 2 stated Resident 97 has been crying and pointing at the door since last week, cries because he wants to go home. RN 2 stated he worked on 7/25/2025 during the 3 p.m. to 11 p.m. shift for hand off report we will first do rounds go in the front of the residents room, outside not in the rooms, then we will do the narcotic count, hand off report is any COC, anything significant this is done at the medication cart not in the residents rooms. RN 2 stated on 7/25/2025 for Resident 97 nothing was reported for Resident 97 by RN 1. RN 2 stated Resident 97 was not an elopement risk, Resident 97 has never tried to go outside of the facility. RN 2 stated was not aware Resident 97 had eloped back in January. During an interview on 7/31/2025 at 8:34 a.m. with CNA 1 stated for Resident 97 he has depression someday he cries, CNA 1 stated for Resident 97 he was crying for like 3 days at that point. CNA1 stated would ask Resident 97 if he wanted to see his sister and Resident 97 would nod yes, CNA 1 stated R97 would cry when he would see staff or any person, Resident 97 would then start to cry. CNA 1 stated Resident 97 would cry for about 10 minutes, would ask if he was in pain and Resident 97 would say no then would ask if he was sad and Resident 97 would nod yes. CNA1 stated would tell RNs and LVN 1 that Resident 97 would be crying and they would go and see Resident 97. CNA 1 stated Resident 97 had never attempted to get out, CNA 1 stated not aware that Resident 97 eloped in January, CNA 1 stated Resident 97 would point outside, and CNA 1 would ask Resident 97 do you want to go with your sister and Resident 97 would nod yes. CNA 1 stated Resident 97 would try to open the lobby door, but he was not able to open it and usually activity personnel would catch him and redirect him. CNA 1 stated the truth is we do not give hand off report because we are not allowed overtime but the nurses on the next shift tell the CNAs what is going on with the residents. CNA 1 stated we get a generalized report on all residents not individualized; this is done at the nurses station. CNA 1 stated that day 7/25/2025 did not remove the top the food tray assumed Resident 97 was in the bathroom, did not supervise Resident 97 that day for lunch, CNA 1 stated if we are not supervising Resident 97 during the meals he can choke, one time Resident 97 actually took another resident tray and was eating another resident food that was regular but CNA 1 was able to catch Resident 97 prior to him eating the food. CNA 1 stated because she was not aware Resident 97 required supervision during meals, she was not able to supervise Resident 97. CNA 1 stated if she was supervising Resident 97 during meals, Resident 97 would not have gotten out. CNA 1 stated Resident 97 kept pointing to go outside, he was showing signs he wanted to leave but was unable to open the door, someone opened the door for Resident 97. During an interview on 7/31/2025 at 12:19 p.m. with the DON, the DON stated Resident 97 was at elopement risk. The DON stated Resident 97 had an elopement in January and had few previous incidents as well. The DON stated intervention for residents at elopement risk are visual checks, distraction, call families to help, psychiatric evaluations if needed and monitor if medication are prescribed. However, the most important intervention is visualization. The DON reviewed Resident 97's care plan for elopement and stated the care plan does not indicate visualization. The DON stated Resident 97`s care plan is not patient centered. The DON stated the care plan should include visualization and should be patient centered. The DON stated the potential can be that the resident can elope again and potential for harm to the resident. The DON stated the care plan is a guide for the care or specifics activities for the residents, the DON stated staff review care plans as a reference on how care should be done for the residents. The DON stated Resident 97 required supervision while eating meaning staff are required to watch Resident 97. The DON stated Resident 97 would eat either in his room or in the dining room. The DON stated Resident 97 required supervision while eating because he had hemiplegia, and his diet is dysphagia mechanical soft. The DON stated Resident 97 was at risk for aspiration. The DON stated if staff did not just leave the tray during lunch time and would have supervised Resident 97, the staff would have noted that Resident 97 was missing. The DON stated Resident 97 had an order for falling star program to be done per shift this is done at the end of the shift. The DON stated if LVN 1 had done the falling star program visualization at 3 p.m., he (LVN 1) would have noted Resident 97 was missing. The DON stated that because of lack of monitoring, there was a delay in noticing Resident 97 was missing. The DON stated LVN 1 using the blood pressure he (LVN 1) took at 8 a.m. for the blood pressure check scheduled at 12 p.m. is inaccurate documentation. LVN 1 did not check Resident 97`s vital signs as ordered by the physician every six (6) hours. The DON stated that the potential outcome is a possibility for Resident 97 blood pressure to be elevated and resulting in late intervention and risk for harm. The DON stated if LVN 1 had taken Resident 97's blood pressure on time, LVN 1 would have noticed that Resident 97 was gone sooner. The DON stated hand off report during change of shift is done by RN to RN. The DON stated that the oncoming RN is physically going into each resident room and visually checking on the residents. The DON stated RN 1 was Resident 97's RN during the 7 a.m. to 3 p.m. shift. The DON stated RN 2 was supposed to be the supervisor for the 7/25/2025 3 p.m. to 11 p.m. shift but was placed at the cart instead. The DON stated no hand off was given to RN 2. The DON stated CNAs do not do a hand off report if there is any special endorsement it is reported to nursing to endorse to the oncoming CNAs. The DON stated if the staff performed room to room hand off, the staff would have been able to notice Resident 97 was missing sooner. The DON stated for Resident 97 safety needs to be individualized, intervention would be visual monitoring, monitoring of behavior, and that is the major, the facility did not do this and that is what lead to the reason Resident 97 eloped. The DON stated facility staff did not implement the safety precaution for Resident 97, and did not do visual assessment on Resident 97. During an interview on 7/31/2025 at 3:22 p.m. with Speech Therapist (ST) 1, ST 1 stated Resident 97 required supervision. ST 1 stated she (ST 1) recommended that Resident 97 be up in chair in dining room he was confused and needed to be supervised due to risk for aspiration, if not being monitored a risk for aspiration because he had impaired cognition. During an interview on 8/1/2025 at 12:39 p.m. with LVN 1, LVN 1 stated was unaware Resident 97 was an elopement risk prior to Resident 97 elopement (7/25/2025). LVN 1 stated blood pressure should be taken prior to administering any blood pressure medications, if it is indicated in the MAR, and if there is an order. LVN 1 stated Resident 97 had an order for blood pressure checks every six (6) hours. LVN 1 stated on 7/25/2025, he (LVN1) did not take Resident 97 blood pressure at 12 p.m. scheduled time. LVN1 stated instead, he (LVN 1) used the 8 a.m. vitals he (LVN 1) took. LVN 1 stated if he had gotten Resident 97's blood pressure would have been able to see that Resident 97 was missing at 12:54 p.m. and would have started the search sooner. LVN 1 stated we do round, it is constant, we administer medications, then vitals, it is a back and forth, after 1 p.m. does charting then will do a last round prior to end of the shift before 3 p.m. LVN 1 stated for falling star program it should be at the end of shift, it should be done physically by visualizing the resident. LVN 1 stated the MAR was left blank because LVN 1 did not do it on 7/25/2025. LVN 1 stated if he had done this at 3 p.m., he (LVN 1) would have known Resident 97 was missing at that time. During a concurrent interview and record review on 8/1/2025 at 3:23 p.m. of the facility P&P titled Shift-Change Endorsement Policy, with the Assistant Director of Nursing (ADON), the ADON stated the hand off report will talk about any COC, change in medications, will count narcotics, then do rounds, the staff are physically looking at the residents while getting report. The ADON stated is aware Resident 97 went missing, the ADON stated if staff had been doing room round during hand off would have caught Resident 97 missing sooner. The ADON reviewed facility P&P titled, Shift-Change Endorsement Policy, and stated rounds need to be made at bedside to be accurate it is not as indicated, should always be at bedside or near the resident. The ADON stated our standard of practice is that residents should all be checked on every two (2) hours, this is for all residents. The ADON stated if staff are not checking on residents every two (2) hours anything can happen a fall, an injury, and elopement like Resident 97. During a review of the facility's P&P titled, Monitoring Residents, last reviewed on 4/24/2025, the P&P indicated staff members will provide adequate supervision to all residents in accordance with their plans of care. Additionally, to the every two (2) hour monitoring from the nursing department, the facility will provide supervision and monitoring form the following duties, which include but not limited to: 1. Daily rounds 2. Medication Pass 3. Nourishment Pass 4. Toileting Program 5. Activity Program 6. RNA Program 7. Therapy Program 8. Meal Pass 9. Ice Pass and Water Pass 10. Incontinent Care Rounds 11. Daily care by Nursing Staff 12. May provide one-to-one monitoring if indicated. During a review of the facility's P&P titled, Shift-Change Endorsement Policy, last reviewed on 4/24/2025, the P&P indicated the nursing staff will conduct changing of shift report to ensure patient related information is communicated during shift-change. Make rounds and conduct endorsements at bedside if indicate, to ensure accuracy. During a review of the facility's P&P titled, Safety and Supervision of Residents, last reviewed on 4/24/2025, the P&P indicated the care team shall target interventions to reduce individual risks related to hazards in the environment, including adequate supervision and assistive devices. Resident supervision is a core component of the system approach to safety. The type and frequency of resident supervision is determined by the individual resident's assessed needs and identified hazards in the environment. During a review of the facility's P&P titled, Wandering and Elopements, last reviewed on 4/24/2025, the P&P indicated the facility will identify residents who are at risk of unsafe wandering and strive to prevent harm while maintaining the least restrictive environment for residents. If identified as at risk for wandering, elopement, or other safety issues, the resident's care plan will include strategies and interventions to maintain the resident's safety. During a review of the facility's P&P titled, Falling Star Program, last reviewed on 4/24/2025, the P&P indicated residents will be assessed for fall risk, utilizing the fall risk assessment form and appropriate intervention will be provided. During a review of the facility's P&P titled, Care Plans, Comprehensive Person-Centered, last reviewed on 4/24/2025, the P&P indicated a comprehensive, person-centered care plan that includes measurable objective and timetables to meet the resident's physical, psychosocial and functional needs is developed and implemented for each resident. During a review of the facility's P&P titled, Administering Medication, last reviewed on 4/24/2025, the P&P indicated Medications are administered in a safe and timely manner and as prescribed. 1. Medications are administered in accordance with prescriber orders, including any required time frames. 10. The following information is checked and verified for each resident prior to administering medications: b. vital signs, if necessary During a review of the facility's P&P titled, Charting and Documentation, last reviewed on 4/24/2025, the P&P indicated documentation in the medical record will be objective, complete and accurate.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents received care consistent with profes...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents received care consistent with professional standards of practice to prevent pressure injury (also called pressure ulcer, localized damage to the skin and/or underlying tissue usually over a bony prominence) for four (4) of four (4) sampled residents (Residents 112, 70, and 102) investigated under pressure injury by: 1. Failing to ensure Resident 112's and 92's low air loss mattress (LALM - a mattress that helps prevent and treat pressure injuries by circulating air and relieving pressure on the body) was set according to residents` weight or comfort. 2. Failing to ensure Resident 70's and 102's LALM was replaced timely when the LALM was beeping indicating low pressure and the resident's appeared sunk in the bed. Findings: a. During a review of Resident 112’s admission Record (front page of the chart that contains a summary of basic information about the resident), the admission Record indicated the facility admitted the resident on 7/15/2025 with diagnoses including Guillain-Barre Syndrome (a condition in which the body's immune system [the body's defense against infections] attacks the nerves causing weakness, numbness or paralysis [occurs when a person is unable to make voluntary muscle movements]), tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), lack of coordination, and generalized muscle weakness.
During a review of Resident 112’s History and Physical (H&P) dated 7/15/2025, the H&P indicated Resident 112 had fluctuating capacity to understand and make decisions.
During a review of Resident 112’s Minimum Data Set (MDS, a resident assessment tool), dated 7/22/2025, the MDS indicated Resident 112 had some difficulty in new situations for cognition (mental action or process of acquiring knowledge and understanding) and was able to understand and make his needs known. The MDS further indicated Resident 112 required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive). The MDS indicated Resident 112 had a pressure-reducing device for bed.
During a review of Resident 112’s Order Summary Report dated 8/1/2025, the Order Summary Report indicated a physician’s order dated 7/16/2025 for the use of LALM for wound care and management.
During a review of Resident 112’s electronic health record (EHR), the EHR indicated that Resident 112’s current weight dated 7/16/2025 indicated 123 pounds (lbs. – a unit pf measurement).
During a review of Resident 112’s Braden Scale for Predicting Pressure Sore Risk form dated 7/15/2025, 7/22/2025, and 7/29/2025, the Braden Scale for Predicting Pressure Sore Risk form indicated that Resident 112 was very high risk for developing pressure injuries.
During an observation on 7/29/2025 at 11:12 a.m., inside Resident 112’s room, observed Resident 112 alert, responds by nodding or shaking head and mouthing words, lying on a LALM with setting at 240 lbs. and a sticker on top of the pump panel indicated 120. Resident 112 stated he was not able to feel if the LALM was firm or soft as he was unable to feel anything.
During a concurrent observation and interview on 7/29/2025 at 12:30 p.m. inside Resident 112’s room with Licensed Vocational Nurse (LVN) 8, LVN 8 stated that Resident 112’s LALM setting was placed on 240 lbs., and the sticker on top of pump panel means that the setting should be at 120 lbs. LVN 8 stated the 240 lbs. setting is on the firm side for Resident 112 as the resident current weight is 120 lbs. LVN 8 stated she makes rounds every day and ensures that the LALM are in the correct setting. LVN 8 stated that when staff are providing ADL care to the residents or turning and repositioning, the setting can be adjusted to the firm setting and should be returned to the appropriate setting after as indicated on the sticker or upon checking the chart for the current weight. LVN 8 stated the staff should have ensured Resident 112’s LALM was set at 120 lbs. and not maintain at 240 lbs. as it placed Resident 112 at risk for development of pressure injury and discomfort.
During an interview on 7/31/2025 at 4:30 p.m. with the Director of Nursing (DON), the DON stated LALM are set according to the resident’s weight or comfort. The DON stated All LALM are set according to weight and the treatment nurse assigned to the unit makes rounds every day in the morning and as needed to ensure the LALM was set accordingly and correct it as she observes it. The DON stated the LALM pump has a sticker that indicates the residents’ current weight to make the staff aware of what setting the LALM should be. The DON stated during ADL care or turning and repositioning, the LALM setting should be at the firm setting for resident safety during the care and returned to appropriate setting after the care is finished. The DON stated Resident 112’s LALM should have been placed at 120 lbs. setting instead of 240 lbs. as the setting might be firm for the resident and can affect his comfort and placed Resident 112 at risk for development of pressure injuries.
During a review of the facility's recent policy and procedure (P&P) titled Prevention of pressure Injuries, last reviewed on 4/24/2025, the P&P indicated the purpose of this procedure is to provide information regarding identification of pressure injury risk factors and interventions for specific risk factors.
- Support Surfaces and Pressure Redistribution
1. Select appropriate support surfaces based on the resident's risk factors, in accordance with current clinical practice.
During a review of the facility's recent P&P titled Pressure-Reducing Mattresses, last reviewed on 4/24/2025, the P&P indicated to provide mattresses that will prevent and/or minimize pressure on the skin, and to provide comfort if resident prefers.
- STEPS:
May adjust air mattress to a desired firmness according to patient's weight and/or using hand check by sliding one hand between the air mattress and bed frame to feel the patient's buttock (able to feel the space in between, and the acceptable range is 1-1.5 inches).
During a review of the facility provided manufacturer’s guideline for Low Air Loss Mattress 1 (LALM 1), undated, the manufacturer’s guideline indicated:
- LALM 1 is designed for prevention, treatment, and management of pressure ulcers.
- LALM 1 is intended to reduce the incidence of pressure ulcers while optimizing patient comfort.
- Press up and down buttons to select the correct patient weight.
- Users can adjust the air mattress according to a desired firmness according to patient’s weight or the suggestion from a healthcare professional.
b. During a review of Resident 70’s admission Record, the admission Record indicated the facility originally admitted the resident on 6/30/2022 and readmitted in the facility on 5/22/2023, with diagnoses including hemiplegia (total paralysis of the arm, leg, and trunk on the same side of the body) left non-dominant side, tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), and anxiety disorder (a mental health condition where excessive fear and worry interfere with daily life, causing significant distress).
During a review of Resident 70’s History and Physical (H&P) dated 7/15/2025, the H&P indicated Resident 70 was incapacitated (refers to a state in which an individual was unable to make sound decisions or manage their affairs).
During a review of Resident 70’s MDS, dated [DATE], the MDS indicated Resident 70 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make his needs known. The MDS further indicated Resident 70 required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive). The MDS indicated Resident 70 had a pressure-reducing device for bed.
During a review of Resident 70’s Order Summary Report dated 8/1/2025, the Order Summary Report indicated a physician’s order dated 11/7/2023 for the use of LALM for wound care and management.
During a review of Resident 70’s Braden Scale for Predicting Pressure Sore Risk form dated 11/19/2024, 2/6/2025, and 5/9/2025, the Braden Scale for Predicting Pressure Sore Risk form indicated that Resident 70 was at moderate risk for developing pressure injuries.
During a concurrent observation and interview on 7/29/2025 at 10:18 a.m., inside Resident 70’s room with LVN 8, observed Resident 70 lying on a LALM with the pump unit making a beeping sound with an orange blinking light on the panel indicating “low pressure” and Resident 70 appeared sunk in the bed. LVN 8 stated that if the “low pressure” indicator light is flashing or blinking and the pump unit is beeping, it means that the LALM is getting softer or deflating and there must be a leak in the unit. LVN 8 stated the staff should check if the LALM is getting deflated or softer, if the connections are secure and correctly installed and also check for air leaks around the mattress. LVN 8 stated Resident 70’s LALM was observed with beeping sound and flashing “low pressure” indicator light since 8 a.m. and the maintenance department was already notified and that the LALM and pump unit needed to be replaced. LVN 8 stated the facility was awaiting delivery of the new mattresses. LVN 8 stated that it had been more than two (2) hours that the LALM had the “low pressure” indicted light on and Resident 70’s buttock was almost touching the bed frame which could lead to Resident 70 developing pressure injury the longer he stays on the deflated mattress. LVN 8 stated the facility should have extra LALM readily available in the event one of the mattresses malfunctions. LVN 8 stated Resident 70’s LALM should have been replaced immediately as it had the potential for Resident 70 to have a skin breakdown especially on the bony prominences if Resident 70’s buttock was touching the bed.
During an interview on 7/29/2025 at 10:30 a.m. with the DON, the DON she was made aware of the issue with the LALM continuously beeping and flashing the “low pressure” indicator light and the facility had ordered extra LAL mattresses to replace the malfunctioning mattresses. The DON stated the staff are supposed to check the connections, for any leakage or if the tubing was not corrected correctly or loose then notify the maintenance department to replace the LALM. The DON stated if a resident had been laying on a deflated mattress, the bottom almost touching the bed frame, and appeared sunk in the mattress for an undetermined period of time, it placed the resident at risk for developing or worsening of pressure injury. The DON stated the facility should have extra LALM available to replace the malfunctioning LALM. The DON stated Resident 70’s LALM should have been replaced as soon as possible and not lay on the deflated mattress for an undetermined amount of time as it placed Resident 70 at risk for development of pressure injury.
During a review of the facility's recent P&P titled Pressure-Reducing Mattresses, last reviewed on 4/24/2025, the P&P indicated a purpose to provide mattresses that will prevent and/or minimize pressure on the skin, and to provide comfort if resident prefers.
- STEPS:
May adjust air mattress to a desired firmness according to patient's weight and/or using hand check by sliding one hand between the air mattress and bed frame to feel the patient's buttock (able to feel the space in between, and the acceptable range is 1-1.5 inches).
During a review of the facility provided manufacturer’s guideline for Low Air Loss Mattress 1 (LALM 1), undated, the manufacturer’s guideline indicated:
- LALM 1 is designed for prevention, treatment, and management of pressure ulcers.
- LALM 1 is intended to reduce the incidence of pressure ulcers while optimizing patient comfort.
- Press up and down buttons to select the correct patient weight.
- Users can adjust the air mattress according to a desired firmness according to patient’s weight or the suggestion from a healthcare professional.
- Pump unit:
The audible alarm turns on when the mattress pressure is low.
- System Installation
e. Perform a “bottom out” test to ensure that patient is properly suspended. Slide your hand under the top cover along a deflated cell in the sacral (bottom) area.
- Hand check:
Check if pressure is properly adjusted by sliding one hand between the air mattress and bed frame to feel the patient’s buttock.
Users should be able to feel the space in between, and the acceptable range is approximately 25 to 40 millimeters (mm – a unit of measurement) or one (1) inch (in – a unit pf measurement) to 1.5 in.
- Low pressure warning:
When abnormal pressure occurs, the “low pressure” indicator will come on and the alarm will be activated to alert for a low-pressure condition. Check if the connections are secure and correctly installed according to the relevant instructions.
If the pressure is consistently low, open the zipper and confirm that all the hoses are properly connected. Then check for any noticeable leakage in any of the tubes. If necessary, contact your local dealer to replace any damaged tube or hoses.
c. During a review of Resident 102’s admission Record (front page of the chart that contains a summary of basic information about the resident), the admission Record indicated the facility admitted the resident on 5/14/2024 with diagnoses including tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), lack of coordination, and gastrostomy (GT - a surgical opening fitted with a device to allow feedings to be administered directly to the stomach common for people with swallowing problems).
During a review of Resident 102’s History and Physical (H&P) dated 5/14/2025, the H&P indicated Resident 102 was incapacitated (refers to a state in which an individual was unable to make sound decisions or manage their affairs).
During a review of Resident 102’s Minimum Data Set (MDS, a resident assessment tool), dated 7/22/2025, the MDS indicated Resident 102 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make his needs known. The MDS further indicated Resident 102 required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive). The MDS indicated Resident 70 had a pressure-reduced device for bed.
During a review of Resident 102’s Order Summary Report dated 8/1/2025, the Order Summary Report indicated a physician’s order dated 5/15/2024 for the use of LALM for wound care and management.
During a review of Resident 102’s Braden Scale for Predicting Pressure Sore Risk form dated 11/26/2024, 2/26/2025, and 5/27/2025, the Braden Scale for Predicting Pressure Sore Risk form indicated that Resident 102 had a moderate to high-risk score for developing pressure injuries.
During a concurrent observation and interview on 7/29/2025 at 10:01 a.m., inside Resident 102’s room with RN 7, observed Resident 102 lying on a LALM with the pump unit making a beeping sound with an orange blinking light on the panel indicating “low pressure” and Resident 102 appeared sunk in the bed. RN 7 stated if the “low pressure” indicator light is flashing or blinking and the pump unit beeping, it means that the LALM is getting softer or deflating and there must be a leak in the unit. RN 7 stated when the LALM is making a beeping sound and the “low pressure” indicator light, the staff should check if the LALM is getting deflated or softer, check if the connections are secure and correctly installed and also check for air leaks around the mattress. RN 7 stated Resident 102’s LALM was observed with beeping sound and flashing “low pressure” indicator light since 8 a.m. RN 7 stated that the maintenance department was already notified and that the LALM and pump unit needed to be replaced. RN 7 stated she was waiting for the LALM replacement. RN 7 stated that it had been two hours that the LALM had the “low pressure” indicator light on and Resident 102 appeared sunk in the bed which could lead to Resident 102 developing pressure injury the longer he stays on the deflated mattress. RN 7 stated Resident 102’s LALM should have been replaced immediately as it placed the resident at risk for developing pressure injury the longer, he stays on the deflated LALM.
During a concurrent observation and interview on 7/29/2025 at 10:18 a.m., inside Resident 102’s room with LVN 8, observed Resident 102 lying on a LALM with the pump unit making a beeping sound with an orange blinking light on the panel indicating “low pressure” and Resident 102 appeared sunk in the bed. LVN 8 stated if the “low pressure” indicator light is flashing or blinking and the pump unit beeping, it means that the LALM is getting softer or deflating and there must be a leak in the unit. LVN 8 stated the staff should check if the LALM is getting deflated or softer, if the connections are secure and correctly installed and check for air leaks around the mattress. LVN 8 stated Resident 102’s LALM was observed with beeping sound and flashing “low pressure” indicator light since 8 a.m. and the maintenance department was already notified and that the LALM and pump unit needed to be replaced. LVN 8 stated the facility was awaiting delivery of the new mattresses. LVN 8 stated that it had been more than two hours that the LALM had the “low pressure” indicator light on and Resident 102’s buttock was almost touching the bed frame which could lead to Resident 102 developing pressure injury the longer he stays on the deflated mattress. LVN 8 stated the facility should have extra LALM readily available in the event one of the mattresses malfunctions. LVN 8 stated Resident 102’s LALM should have been replaced immediately as it had the potential for Resident 102 to have a skin breakdown especially on the bony prominences if Resident 102’s buttock was touching the bed.
During an interview on 7/29/2025 at 10:30 a.m. with the DON, the DON stated that she was made aware of the issue with the LALM continuously beeping and flashing the “low pressure” indicator light and the facility had ordered extra LAL mattresses to replace the malfunctioning mattresses. The DON stated the staff are required to check the connections for any leakage or if the tubing was not connected correctly or loose then notify the maintenance department to replace the LALM. The DON stated if a resident had been laying on a deflated mattress, the bottom almost touching the bed frame, and appeared sunk in the mattress for an undetermined period, it placed the resident at risk for developing or worsening of pressure injury. The DON stated the facility should have extra LALM available to replace the malfunctioning LALM. The DON stated Resident 102’s LALM should have been replaced as soon as possible. The DON stated Resident 102 should not lay on the deflated mattress for an undetermined period of time as it placed Resident 102 at risk for development of pressure injury.
During a review of the facility's recent P&P titled Pressure-Reducing Mattresses, last reviewed on 4/24/2025, the P&P indicated a purpose to provide mattresses that will prevent and/or minimize pressure on the skin, and to provide comfort if resident prefers.
- STEPS:
May adjust air mattress to a desired firmness according to patient's weight and/or using hand check by sliding one hand between the air mattress and bed frame to feel the patient's buttock (able to feel the space in between, and the acceptable range is 1-1.5 inches).
During a review of the facility provided manufacturer’s guideline for Low Air Loss Mattress 1 (LALM 1), undated, the manufacturer’s guideline indicated:
- LALM 1 is designed for prevention, treatment, and management of pressure ulcers.
- LALM 1 is intended to reduce the incidence of pressure ulcers while optimizing patient comfort.
- Press up and down buttons to select the correct patient weight.
- Users can adjust the air mattress according to a desired firmness according to patient’s weight or the suggestion from a healthcare professional.
- Pump unit:
The audible alarm turns on when the mattress pressure is low.
- System Installation
e. Perform a “bottom out” test to ensure that patient is properly suspended. Slide your hand under the top cover along a deflated cell in the sacral (bottom) area.
- Hand check:
Check if pressure is properly adjusted by sliding one hand between the air mattress and bed frame to feel the patient’s buttock.
Users should be able to feel the space in between, and the acceptable range is approximately 25 to 40 millimeters (mm – a unit of measurement) or one (1) inch (in – a unit pf measurement) to 1.5 in.
- Low pressure warning:
When abnormal pressure occurs, the “low pressure” indicator will come on and the alarm will be activated to alert for a low-pressure condition. Check if the connections are secure and correctly installed according to the relevant instructions.
If the pressure is consistently low, open the zipper and confirm that all the hoses are properly connected. Then check for any noticeable leakage in any of the tubes. If necessary, contact your local dealer to replace any damaged tube or hoses.
d. During a review of Resident 92’s admission Record, the admission Record indicated the facility admitted the resident on 11/16/2021, and readmitted the resident on 3/24/2025, with diagnoses including hemiplegia (total paralysis of the arm, leg, and trunk on the same side of the body) and hemiparesis (is a medical condition where you experience weakness or a decreased ability to move one entire side of your body), muscle weakness, and cerebral infarction (occurs as a result of disrupted blood flow to the brain due to problems with the blood vessels that supply it).
During a review of Resident 92’s MDS, dated [DATE], the MDS indicated the resident usually had the ability to make self-understood and understand others and had moderate cognitive impairment (a condition in which people have more memory or thinking problems than other people their age). The MDS indicated the resident was dependent to needing moderate assistance on mobility and activities of daily living (ADLs, activities such as bathing, dressing and toileting a person performs daily). The MDS also indicated the resident was incontinent of urine and stool (feces) and the resident was at risk for developing pressure ulcers/injuries. The MDS indicated the resident was on a pressure-reducing device for bed.
During a review of Resident 92’s Order Summary Report, dated 3/25/2025, the Order Summary Report indicated an order for [Treatment] Low Air Loss Mattress for wound care and management.
During a review of Resident 92’s Braden Scale for Predicting Pressure Sore Risk, dated 5/28/2025, the Braden Scale for Predicting Pressure Score Risk indicated the resident was at moderate risk for developing pressure injuries.
During a concurrent observation and interview on 7/29/2025, at 10:44 a.m., with Registered Nurse (RN) 6, inside Resident 92’s room, observed Resident 92’s LALM was set at 160, the sticker attached to the LALM machine was 200. RN 6 stated the LALM should be set according to the resident’s weight and the sticker that was attached to the LALM machine should be the setting on the machine. RN 6 stated not setting the LALM according to the resident’s weight had the potential for developing or worsening of pressure injury of Resident 92.
During a concurrent interview and record review on 7/31/2025, at 12:38 p.m., with RN 3, reviewed Resident 92’s Weight and Vitals log. RN 3 stated Resident 92’s latest weight was 185. RN 3 stated the LALM should be placed on setting 200. RN 3 stated not setting the LALM according to the resident’s weight had the potential for developing or worsening of pressure injury to Resident 92.
During an interview on 8/1/2025, at 2:05 p.m., with the Assistant Director of Nursing (ADON), the ADON stated the LALM should be set according to Resident 92’s weight. The ADON stated if Resident 92’s weight is 185, it should be set to 200 to provide maximum therapeutic effect of the LALM. The ADON stated the failure of the staff of setting the LALM according to the resident’s weight had predisposed the resident to development or worsening of the pressure injury of the resident.
During a review of the facility's recent policy and procedure (P&P) titled Prevention of pressure Injuries, last reviewed on 4/24/2025, the P&P indicated the purpose of this procedure is to provide information regarding identification of pressure injury risk factors and interventions for specific risk factors.
Support Surfaces and Pressure Redistribution
1. Select appropriate support surfaces based on the resident's risk factors, in accordance with current clinical practice.
During a review of the facility's recent P&P titled Pressure-Reducing Mattresses, last reviewed on 4/24/2025, the P&P indicated to provide mattresses that will prevent and/or minimize pressure on the skin, and to provide comfort if resident prefers.
STEPS:
-May adjust air mattress to a desired firmness according to patient's weight and/or using hand check by sliding one hand between the air mattress and bed frame to feel the patient's buttock (able to feel the space in between, and the acceptable range is 1-1.5 inches).
During a review of the facility-provided Operation Manual for Low Air Loss Mattress (LALM) 1, undated, indicated on product function to press up and down buttons to select the correct patient weight.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents who were incontinent of urine receiv...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents who were incontinent of urine received appropriate treatment and services to prevent urinary tract infections (UTI, an infection in the bladder/urinary tract) for four of four randomly sampled residents (Resident 36, 1, 5, and 55) by failing to: 1. Ensure the urinal bottle (a container used to collect urine and is made for either male or female anatomy) was labeled with a resident identifier for Residents 36, 1, and 55. 2. Anchor the urinary catheter (a hollow tube inserted into the bladder to drain or collect urine) tubing in the stat lock (a strap-free device which secures a Foley catheter [a hollow tube inserted into the bladder to drain or collect urine] in place, stabilizes the catheter and reduces the likelihood of a sudden pull) of Resident 5. These deficient practices had the potential for cross-contamination (the physical movement or transfer of harmful bacteria from one person, object or place to another) and urinary tract infection (UTI, an infection of the urinary system, which includes the kidneys, ureters, bladder, and urethra) due to switching of urinals and torn urinary meatus (the opening in the penis where the urine [pee] comes out) due to constant tugging and pulling of the catheter tubing as portal of entry for infection. Findings:1.a. During a review of Resident 1’s admission Record (AR), the AR indicated the facility admitted the resident on 5/12/2022 and most recently readmitted the resident on 2/15/2025 with diagnoses that included acute and chronic respiratory failure (a serious condition that occurs suddenly when the lungs cannot get enough oxygen), tracheostomy (opening surgically created through the front of the neck and into the trachea [windpipe]), dependence on respiratory ventilator (a medical device to help support or replace breathing), muscle weakness, and need for assistance with personal care.
During a review of Resident 1’s Minimum Data Set (MDS – resident assessment tool), dated 5/18/2025, the MDS indicated the resident was totally dependent on staff for mobility, dressing, bathing, toilet hygiene, and personal hygiene.
During a review of Resident 1’s History and Physical (H&P), dated 2/16/2025, the H&P indicated the resident was nonverbal but was awake, alert, able to respond yes/no appropriately to questions, and was able to move all extremities. The H&P further indicated the resident was able to understand and make decisions.
During a review of Resident 1’s Care Plan (CP) regarding potential for recurrent urinary tract infections, initiated 9/3/2023 and last reviewed 6/6/2025, the CP indicated a goal to reduce the risk of urinary tract infections (UTI- an infection in the bladder/urinary tract)
1.b. During a review of Resident 36’s AR, the AR indicated the facility admitted the resident on 6/3/2025 and most recently readmitted the resident on 7/15/2025 with diagnoses that included chronic respiratory failure, tracheostomy, dependence on respiratory ventilator, and UTI.
During a review of Resident 36’s MDS, dated [DATE], the MDS indicated the resident was totally dependent on staff for mobility, dressing, bathing, toilet hygiene, and personal hygiene.
During a review of Resident 36’s H&P, dated 1/15/2024, the H&P indicated the resident did not have the capacity to understand and make decisions.
During a review of Resident 36’s Order Summary Report, the Order Summary Report indicated a physician’s order for an indwelling catheter (a flexible tube placed in the bladder to drain urine) attached to bedside drainage bag due to neuromuscular dysfunction of the bladder (a person lacks bladder control due to brain, spinal cord or nerve problems), every shift, dated 7/16/2025.
During a review of Resident 36’s CP regarding risk for infection, initiated 7/16/2025 and last reviewed 7/25/2025, the CP indicated the resident was at risk for infection due to the use of an indwelling catheter (a flexible tube placed in the bladder to drain urine) with a goal that the resident would be free from infection / UTI.
During an observation on 7/29/2025 at 11:20 a.m., observed Residents 36 and 1 awake and lying in their beds in their shared room. Observed in the shared restroom an unlabeled urinal hanging from the mobility assistance bar.
During an interview on 7/29/2025 at 11:40 a.m. with Certified Nursing Assistant (CNA) 5, CNA 5 stated CNA 5 was covering while CNA 6 was on break. CNA 5 entered Residents 36 and 1s’ shared restroom and stated there was an unlabeled urinal in the restroom. CNA 5 stated that Resident 36 had an indwelling catheter, and the urinal was used to empty the urine from the drainage bag. CNA 5 stated Resident 1 was incontinent. CNA 5 stated all urinals should be labeled with the resident’s first and last name and a date, but the urinal was not labeled.
During an interview on 7/29/2025 at 11:59 a.m. with CNA 6, CNA 6 stated urinals should be labeled because every resident should have a specific urinal to prevent infections. CNA 6 stated CNA 6 was assigned to care for Residents 36 and 1 and CNA 6 did not check to ensure the urinal in the shared restroom was labeled.
During an interview on 8/1/2025 at 8:58 a.m. with the Infection Preventionist (IP), the IP stated every resident should have a designated urinal to prevent cross contamination (the process by which bacteria or other microorganisms are unintentionally transferred from one substance or object to another, with harmful effect) between residents. The IP stated the residents’ rooms and bathrooms are communal areas and urinals need to be labeled. The IP stated all the staff are provided with markers to ensure the urinals are labeled. The IP stated even when one resident is not currently using a urinal, the urinals should be labeled because there was a possibility that the urinal may be used on the wrong resident. The IP stated when the urinal in Residents 36 and 1s’ shared restroom was not labeled there was a potential to result in infections in the residents.
During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the Assistant Director of Nursing (ADON), the ADON reviewed the facility P&P regarding infection control and urinals. The ADON stated urinals should be labeled so they do not get mixed up and used on the wrong resident resulting in UTIs in residents. The ADON stated the facility P&P was not followed when the urinal was not labeled in the shared restroom of Residents 36 and 1.
During a review of the facility policy and procedure (P&P) titled, “Giving and Removing Urinal,” last reviewed 4/24/2025, the Procedure indicated to provide resident with a container for urine. Label as indicated.
During a review of the facility P&P titled, “Infection Prevention and Control Program,” last reviewed 4/24/2025, the policy indicated an infection prevention and control program is established and maintained to provide a safe and sanitary and comfortable environment and to help prevent the development and transmission of communicable diseases and infections.
2.During a review of Resident 55’s admission Record, the admission Record indicated the facility admitted the resident on 4/18/2025, with diagnoses including injury at C5 level of cervical spinal cord (means that the damage occurred at the level of the fifth cervical vertebra [C5] in the neck), type two diabetes mellitus (DM, a disorder characterized by difficulty in blood sugar control and poor wound healing), and need for assistance with personal care.
During a review of Resident 55’s H&P, dated 4/19/2025, the H&P indicated the resident had the capacity to understand and make decisions.
During a review of Resident 55’s MDS, dated [DATE], the MDS indicated the resident had the ability to make self-understood and understand others and had intact cognition (a participant who has sufficient judgment, planning, organization, self-control, and the persistence needed to manage the normal demands of the participant's environment). The MDS indicated the resident was dependent to needing setup assistance on mobility and activities of daily living (ADLs, activities such as bathing, dressing and toileting a person performs daily). The MDS indicated the resident was incontinent of urine and stool (feces).
During a concurrent observation and interview on 7/29/2025, at 9:34 a.m., with CNA 8, inside Resident 55’s room, observed Resident 55’s urinal hanging at the left side rail of the bed without any label. CNA 8 stated the staff should have labeled the urinal with the name and room number of the resident to prevent switching of urinals that can cause cross-contamination of infections among residents such as urinary tract infection (UTI, a bacterial infection that affects any part of the urinary system, including the bladder, urethra, ureters, and kidneys).
During an interview on 7/31/2025, at 11:51 a.m., with Registered Nurse (RN) 3, RN 3 stated the urinal bottle of Resident 55 should have been labeled with the name and room number of the resident to prevent cross-contamination. RN 3 stated using contaminated urinals can cause UTI to residents.
During an interview on 8/1/2025, at 2:05 p.m., with the ADON, the ADON stated the staff should have labeled the urinal bottle with the name and room number of the resident. The ADON stated the failure of the staff to label the urinal bottle of Resident 55 can predispose the resident to developing UTI.
During a review of the facility's recent P&P titled Policy: UTI- Preventive Measures, last reviewed on 4/24/2025, the P&P indicated this facility will utilize measures in order to help prevent urinary tract infections.
During a review of the facility's recent P&P titled Giving and Removing Urinal, last reviewed on 4/24/2025, the P&P indicated to provide resident with a container for urine.
For A Dependent Resident
STEPS:
13. Label as indicated.
3.During a review of Resident 5’s admission Record, the admission Record indicated the facility admitted the resident on 12/31/2024, and readmitted the resident on 3/27/2025, with diagnoses including methicillin resistant staphylococcus aureus (MRSA, a bacteria that does not respond to antibiotics) infection, pressure ulcer of sacral region, stage 4 (a very deep wound that extends into the muscle, bone, and sometimes tendons or other supporting structures like ligaments), benign prostatic hyperplasia (an enlarged prostate) with lower urinary tract symptoms.
During a review of Resident 5’s MDS, dated [DATE], the MDS indicated the resident had the ability to make self-understood and understand others and had severe cognitive impairment (a significant decline in a person's ability to think, learn, remember, and make decisions). The MDS indicated the resident required substantial assistance on mobility and ADLs. The MDS also indicated the resident had indwelling catheter (is essentially a soft, flexible tube inserted into the bladder to help drain urine continuously).
During a review of Resident 5’s Order Summary Report, the Order Summary Report indicated an order for:
-2/5/2025 [Catheter} Secure foley catheter tubing with anchor every day shift (To minimize dislodging of catheter).
-[Catheter] Foley catheter French scale (Fr, the size of an indwelling catheter is essentially the thickness or diameter of that straw) (18/10) milliliters (ml, a unit of volume) attached to bedside drainage bag due to urinary retention (a condition in which you cannot empty all the urine from your bladder) every shift.
During a concurrent observation and interview on 7/29/2025, at 9:41 a.m., with CNA 8, observed Resident 5’s indwelling catheter not anchored in the stat lock. CNA 8 stated the indwelling catheter tubing should be anchored in a stat lock to prevent tugging and pulling of the tubing that can dislodge the tube.
During an interview on 7/31/2025, at 11:48 a.m., with RN 3, RN 3 stated the resident was placed with the indwelling catheter due to urinary retention. RN 3 stated the indwelling catheter tubing should be anchored in a stat lock to prevent dislodging the tubing and to prevent trauma to the urinary meatus that can cause meatal tear acting as portal of entry for infection.
During an interview on 8/1/2025, at 2:05 p.m., with the ADON, the ADON stated the indwelling catheter of Resident 5 should have been anchored with stat lock to prevent the tubing from getting yanked accidentally causing trauma to the meatus that can lead to infection. The ADON stated the treatment nurses are responsible for ensuring the indwelling catheters are anchored and secured to prevent UTI to residents.
During a review of the facility's recent P&P titled Indwelling (Foley) Catheter Insertion, Male Resident, last reviewed on 4/24/2025, the P&P indicated the purpose is to provide guidelines for the aseptic insertion of an indwelling (Foley) urinary catheter in a male resident.
Steps in the Procedure
13. Insert the catheter:
f. Secure catheter tubing and/or bag to resident with approved catheter securement device.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility: 1. Failed to ensure residents receiving enteral feeding (EF - a...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility: 1. Failed to ensure residents receiving enteral feeding (EF - also known as tube feeding, a method of supplying nutrients directly into the stomach) received appropriate care and services to prevent complications of EF for three (3) of six (6) sampled resident (Residents 71, 89, and 81) reviewed for tube feeding when: 1.1. Resident 71's and 89's water flush bag label did not indicate the residents' name, room number, and administration rate. 1.2. Resident 81's EF bottle was not labeled accurately with the administration rate and matches with the administration rate on the gastrostomy (GT - a surgical opening fitted with a device to allow feedings to be administered directly to the stomach common for people with swallowing problems) feeding pump and the water flush bag indicated the resident's name and running rate. These deficient practices had the potential to result in altered nutritional status such as dehydration and malnutrition and complications associated with enteral feeding such as gastrointestinal (GI) (relating to stomach and intestines) problems such as abdominal pain and diarrhea which may lead to weight loss. 2. Failed to ensure the staff providing care and services to the resident who has a feeding tube (are soft plastic tubes through which liquid nutrition travels through the gastrointestinal tract [the series of organs that food and liquids pass through as they are digested, absorbed, and leave the body as feces]) are aware of, competent in, and utilize facility protocols regarding feeding tube nutrition and care for three of six sampled residents (Residents 28, 68, and 100) reviewed for tube feeding when: 2.1. Resident 28's formula feeding bottle and water flush bag for gastrostomy tube (GT, a tube inserted through the abdomen directly into the stomach) feeding was not labeled with the name, room number, the date and time it was hung, the rate of infusion, and initialed by the licensed nurse. 2.2. Resident 68 and 100's formula feeding bottle was labeled with the infusion rate and the water flush bag for GT feeding was labeled with the name, room number, the date and time it was hung, the rate of infusion, and initialed by the licensed nurse. These deficient practices had the potential to result in altered nutritional status that can lead to over or under hydration, gastrointestinal (GI, relating to stomach and intestines) infection to the resident. Findings:a. During a review of Resident 71’s admission Record (front page of the chart that contains a summary of basic information about the resident), the admission Record indicated the facility originally admitted the resident on 5/4/2011 and readmitted in the facility on 5/12/2025, with diagnoses including tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), dependence on respirator (also known as ventilator – a machine used to help a person breath when they are unable to do so on their own) status, contracture of muscle multiple sites, and gastrostomy.
During a review of Resident 71’s History and Physical (H&P) dated 6/24/2025, the H&P indicated Resident 71 did not have the capacity to understand and make decisions.
During a review of Resident 71’s Minimum Data Set (MDS, a resident assessment tool), dated 7/3/2025, the MDS indicated Resident 71 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make her needs known. The MDS further indicated Resident 71 received GT feeding and required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive).
During a review of Resident 71’s care plan (CP) on gastrostomy at risk for aspiration (a condition when something that’s supposed to be in the stomach gets into the airways to the lungs), dehydration (lack of water in the body necessary to perform its functions), and feeding intolerance initiated on 12/28/2022 and last revised on 7/2/2025, the CP indicated to administer enteral feedings as ordered and flush GT with water as ordered as a few of the interventions to minimize risk of dehydration, aspiration, and feeding intolerance.
During a review of Resident 71’s Order Summary Report dated 8/1/2025, the Order Summary Report indicated the following physician’s orders:
- 6/18/2024:
Turn pump on at 12 p.m. and turn off at 8 a.m. or until dose is completed.
Change Spike set and pump tubing when hanging a new formula bag.
- 6/28/2024: Flush enteral tube with 45 milliliters (ml – a unit of measurement) of water every one (1) hour for 20 hours to provide 900 ml per day.
- 12/10/2024: Tube Feeding (TF) 1 at 55 ml per hour for 20 hours via pump to provide 1100 ml per 1320 kilocalories (kcal – _a unit of measurement for measuring food energy) per day.
During a concurrent observation and interview on 7/29/2025 at 10:59 a.m., inside Resident 71’s room with Licensed Vocational Nurse (LVN) 4, LVN 4 stated Resident 71’s water flush bag did not indicate the resident’s name, room number, and the infusion rate. LVN 4 stated TF bottles and water flush bags are changed at 12 p.m. and both TF and water flush should be labeled with the resident name, room number, start date and time, initials of the nurse, and the infusion rate. LVN 4 stated Resident 71’s water flush bag should have been labeled completely to include Resident 71’s name, room number, and the infusion rate so the staff would be aware that the bag belongs to the resident and the infusion rate matches with rate in the feeding pump. LVN 4 stated the staff, or everyone involved in the resident’s care, would not know if Resident 71 was getting the correct amount of water flush which could lead to dehydration.
During a concurrent interview record review on 7/29/2025 at 11:30 a.m., reviewed a photograph of Resident 71’s water flush bag with Registered Nurse (RN) 4. RN 4 stated Resident 71’s water flush bag indicated a start date of 7/28/2025 at 12 p.m. but did not indicate Resident 71’s name, room number, and the infusion rate. RN 4 stated TF bottles and water flush bags are changed by the licensed nurse (LN) in charge of the residents every day and are hung at 12 p.m. RN 4 stated the LN should write in the label the resident name, room number, start date and time, initials of the LN, and the infusion rate. RN 4 stated the LN in charge of Resident 71 on 7/28/2025 should have indicated Resident 71’s name, room number, and TF infusion rate on the water flush bag label so the staff would be aware that the bag that was hanging belongs to the correct resident and the TF infusion rate matches with the rate in the feeding pump. RN 4 stated that if the bag was not labeled correctly, the staff or everyone involved in the resident’s care would not know if Resident 71 was getting the correct amount of water flush which could lead to dehydration.
During a review of the facility’s recent policy and procedure (P&P) titled, “Enteral Feedings – Safety Precautions,” last reviewed on 4/24/2025m the P&P indicated the facility ensures the safe administration of enteral nutrition. The P&P further indicated:
- The facility will remain current in and follow accepted best practices in enteral nutrition.
To prevent errors in administration:
1. Check the enteral nutrition label against the order before administration. Check the following information:
a. Resident name, ID, and room number
b. Type of formula
c. Date and time the formula was prepared
d. Route of delivery
e. Access site
f. Method (pump, gravity, syringe), and
g. Rate of administration
2. On the formula label document initials, date and time the formula was hung, and initial that the label was checked against the order.
b. During a review of Resident 89’s admission Record, the admission Record indicated the facility originally admitted the resident on 2/20/2022, and readmitted in the facility on 10/27/2023, with diagnoses including tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), dependence on respirator (also known as ventilator – a machine used to help a person breath when they are unable to do so on their own) status, contracture of muscle multiple sites, and gastrostomy (GT - a surgical opening fitted with a device to allow feedings to be administered directly to the stomach common for people with swallowing problems).
During a review of Resident 89’s History and Physical (H&P) dated 10/27/2024, the H&P indicated Resident 89 was incapacitated (refers to a state in which an individual was unable to make sound decisions or manage their affairs).
During a review of Resident 89’s MDS, dated [DATE], the MDS indicated Resident 89 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make her needs known. The MDS further indicated Resident 89 received GT feeding and required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive).
During a review of Resident 89’s care plan (CP) on GT feeding at risk for aspiration (a condition when something that’s supposed to be in the stomach gets into the airways to the lungs), dehydration (lack of water in the body necessary to perform its functions), and feeding intolerance initiated on 3/3/2022 and last revised on 6/13/2025, the CP indicated to administer enteral feedings as ordered and flush GT with water as ordered as a few of the interventions to minimize risk of dehydration, aspiration, and feeding intolerance.
During a review of Resident 89’s Order Summary Report dated 8/1/2025, the Order Summary Report indicated the following physician’s orders:
- 10/28/2023:
Turn pump on at 12 p.m. and turn off at 8 a.m. or until dose is completed.
Change Spike set and pump tubing when hanging a new formula bag.
- 10/31/2023: Flush enteral tube with 60 milliliters (ml – a unit of measurement) of water every one (1) hour for 20 hours to provide 1200 ml of water.
- 2/17/2025: Tube Feeding (TF) 2 at 55 ml per hour for 20 hours via pump to provide 1100 ml per 1650 kilocalories (kcal – _a unit of measurement for measuring food energy) per day.
During a concurrent observation and interview on 7/29/2025 at 10:59 a.m., inside Resident 89’s room with Licensed Vocational Nurse (LVN) 4, LVN 4 stated Resident 89’s water flush bag did not indicate the resident’s name, room number, and the infusion rate. LVN 4 stated TF bottles and water flush bags are changed every 12 p.m. and both TF and water flush should be labeled with the resident name, room number, date and time hung, initials of the nurse, and the running rate. LVN 4 stated Resident 89’s water flush bag should have been labeled completely to include Resident 89’s name, room number, and the running rate so the staff would be aware that the bag belongs to the resident and the running rate matches with rate in the feeding pump. LVN 4 stated the staff, or everyone involved in the resident’s care would not know if Resident 71 was getting the correct amount of water flush which could lead to dehydration.
During a concurrent interview record review on 7/29/2025 at 11:30 a.m., reviewed a photograph of Resident 89’s water flush bag with Registered Nurse (RN) 4. RN 4 stated Resident 89’s water flush bag indicated a start date of 7/28/2025 at 12 p.m. but did not indicate Resident 89’s name, room number, and the TF infusion rate. RN 4 stated TF bottles and water flush bags are changed by the licensed nurse (LN) in charge of the residents every day and are hung at 12 p.m. RN 4 stated the LN should write the resident name, room number, start date and time, initials of the LN, and the TF infusion rate on the label. RN 4 stated the LN in charge of Resident 89 on 7/28/2025 should have indicated in the water flush bag label Resident 89’s name, room number, and the infusion rate so the staff would be aware that the bag that was hanging belongs to the correct resident and the TB infusion rate matches with the rate in the feeding pump. RN 4 stated that if the bag was not labeled correctly, the staff or everyone involved in the resident’s care would not know if Resident 89 was getting the correct amount of water flush which could lead to dehydration.
During a review of the facility’s recent policy and procedure (P&P) titled, “Enteral Feedings – Safety Precautions,” last reviewed on 4/24/2025m the P&P indicated the facility ensures the safe administration of enteral nutrition. The P&P further indicated:
- The facility will remain current in and follow accepted best practices in enteral nutrition.
- To prevent errors in administration:
1. Check the enteral nutrition label against the order before administration. Check the following information:
a. Resident name, ID, and room number
b. Type of formula
c. Date and time the formula was prepared
d. Route of delivery
e. Access site
f. Method (pump, gravity, syringe), and
g. Rate of administration
2. On the formula label document initials, date and time the formula was hung, and initial that the label was checked against the order.
c. During a review of Resident 81’s admission Record, the admission Record indicated the facility originally admitted the resident on 8/20/2016 and readmitted in the facility on 7/5/2025, with diagnoses including tracheostomy, dependence on respirator status, and gastrostomy.
During a review of Resident 81’s History and Physical (H&P) dated 7/2/2025, the H&P indicated Resident 81 did not have the capacity to understand and make decisions.
During a review of Resident 81’s MDS, dated [DATE], the MDS indicated Resident 81 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make his needs known. The MDS further indicated Resident 81 received GT feeding and required total assistance from staff with all ADLs.
During a review of Resident 81’s care plan (CP) on GT feeding at risk for aspiration dehydration, and feeding intolerance initiated on 12/28/2022 and last revised on 7/2/2025, the CP indicated to administer enteral feedings as ordered and flush GT with water as ordered as a few of the interventions to minimize risk of dehydration, aspiration, and feeding intolerance.
During a review of Resident 81’s Order Summary Report dated 8/1/2025, the Order Summary Report indicated the following physician’s orders
- 7/5/2025:
Turn pump on at 12 p.m. and turn off at 8 a.m. or until the dose is completed
Change Spike set and pump tubing when hanging a new formula bag.
- 7/9/2025: Flush enteral tube with water at 80 ml per hour for 20 hours via pump to provide 1000 ml per day.
During an observation on 7/29/2025 at 12:28 p.m. inside Resident 81’s room, observed Resident 81’s GT feeding pump was turned on with Tube Feeding (TF) 2 bottle labeled with an administration rate of 85 ml per hour, and the GT feeding pump indicated a rate of 80 ml per hour. Upon further observation, Resident 81’s water flush bag did not indicate Resident 81’s name, room number, and the administration rate.
During a concurrent observation, interview, and record review on 7/29/2025 at 12:35 p.m., inside Resident 81’s room with LVN 2, LVN 2 stated the label on Resident 81’s TF 2 indicated an administration rate of 85 ml per hour and did not match the administration rate of 80 ml per hour in the GT feeding pump and the water flush bag did not indicate the resident’s name, room number, and administration rate. Reviewed Resident 81’s physician’s order with LVN 2 and the physician’s order indicated an order for TF 2 at 80 ml per hour. LVN 2 stated she must have overlooked the administration rate and mislabeled the formula bottle. LVN 2 stated prior to starting GT feeding, the licensed nurses (LN) were supposed to check the current physician’s order and the label in the formula bottle and GT feeding pump should match the accurate administration rate. LVN 2 stated both the GT feeding pump and formula bottle should be labeled with the resident name, room number, date and time hung, LN initials, and the administration rate. LVN 2 stated Resident 81’s TF 2 bottle and GT feeding pump should both indicate the current physician’s order for the administration rate and the water flush bag should have been labeled to include Resident 81’s name, room number, and administration rate so all staff involved with the resident’s care would be aware that Resident 81 was receiving the accurate amount of feeding and water flush hourly which may lead to dehydration and weight loss.
During a concurrent interview record review on 7/29/2025 at 1:30 p.m., reviewed photographs of Resident 81’s water flush bag, TF 2 bottle, and GT feeding pump with Registered Nurse (RN) 4. RN 4 stated Resident 81’s water flush bag indicated a start date of 7/29/2025 at 12 p.m. but did not indicate Resident 81’s name, room number, and the TB administration rate. RN 4 stated Resident 81’s TB administration rate written on the TF 2 bottle and the GT feeding pump screen did not match together. RN 4 stated TF bottles and water flush bags are changed by the licensed nurse (LN) in charge of the residents every day and are hung at 12 p.m. RN 4 stated the LN should write the resident name, room number, start date and time, initials of the LN, and the administration rate on the label. RN 4 stated the LN was required to ensure the running rate indicated on the TF bottles and the GT feeding pump match. RN 4 stated the LN in charge of Resident 81 should have indicated in the water flush bag label Resident 81’s name, room number so the staff would be aware that the bag that was hanging belongs to the correct resident. RN 4 stated the LN should have ensured the running rate written on Resident 81’s TF bottle and GT feeding should match according to current physician’s orders to ensure that Resident 81 was receiving the accurate amount of feeding and water flush hourly which may lead to dehydration and weight loss.
During a review of the facility’s recent policy and procedure (P&P) titled, “Enteral Feedings – Safety Precautions,” last reviewed on 4/24/2025m the P&P indicated the facility ensures the safe administration of enteral nutrition. The P&P further indicated:
- The facility will remain current in and follow accepted best practices in enteral nutrition.
- To prevent errors in administration:
1. Check the enteral nutrition label against the order before administration. Check the following information:
a. Resident name, ID, and room number
b. Type of formula
c. Date and time the formula was prepared
d. Route of delivery
e. Access site
f. Method (pump, gravity, syringe), and
g. Rate of administration
2. On the formula label document initials, date and time the formula was hung, and initial that the label was checked against the order.
d. During a review of Resident 28’s admission Record, the admission Record indicated the facility admitted the resident on 3/12/2025, and readmitted the resident on 5/5/2025, with diagnoses including dysphagia (difficulty swallowing), protein-calorie malnutrition (a condition where a person's diet does not provide enough protein and calories [energy] for their body to function properly), and type two diabetes mellitus (DM, a disorder characterized by difficulty in blood sugar control and poor wound healing).
During a review of Resident 28’s History and Physical (H&P), dated 5/6/2025, the H&P indicated the resident did not have the capacity to understand and make decisions.
During a review of Resident 28’s MDS, dated [DATE], the MDS indicated the resident rarely to never had the ability to make self-understood and understand others and had severe cognitive impairment (a significant decline in a person's ability to think, learn, remember, and make decisions). The MDS indicated the resident had a feeding tube (a thin, flexible tube used to deliver liquid nutrition directly into the stomach or small intestine when a person is unable to eat or drink adequately on their own).
During a review of Resident 28’s Order Summary Report, the Order Summary Report indicated an order for:
-5/29/2025 Enteral Feed (a way of sending nutrition right to the stomach or small intestine) Order: Glucerna 1.2 at 80 cubic centimeters (cc, a unit of volume) per hour for 20 hours via pump to provide 1600 cc/1920 kilocalorie (kcal, a unit of energy)/day.
-5/15/2025 Enteral Feed Order: Every four hours for hydration [Enteral} Water Bolus Flush 200 milliliters (ml, a unit of volume) every four hours to provide 1200 cc/day.
During a concurrent observation and interview on 7/29/2025, at 11:05 a.m., with RN 6, inside Resident 28’s room, observed Resident 28’s formula feeding bottle and water flush bag for GT feeding were not labeled with the name, room number, the date and time it was hung, the rate of infusion, and the initial of the licensed nurse. RN 6 stated the licensed staff should label the formula feeding bag and the water flush bag with the name, room number, the date and time it was hung, the rate of infusion, and initialed by the licensed nurse to ensure the enteral feeding is accurately set and to prevent medication error to resident. RN 6 also stated that not labeling the bags will also predispose the resident from getting expired formula, with inaccurate rate of infusion the resident can suffer from nutritional imbalance.
During a concurrent interview and record review on 7/31/2025, at 11:47 a.m., with RN 3, reviewed Resident 28’s Order Summary Report and Policies and Procedure (P&Ps) for GT feeding. RN 3 stated there was an order for GT feeding and water flush on the resident. RN 3 stated the P&P titled Enteral Feedings- Safety Precautions, was not followed and the steps for preventing errors in administration was missed.
During an interview on 8/1/2025, at 2:05 p.m., with the Assistant Director of Nursing (ADON), the ADON stated the licensed staff hanging the feeding formula and the water flush for Resident 28 should have labeled the feeding formula and the water flush bag with the name, room number, the date and time it was hung, the rate of infusion, and initialed to prevent errors in administration. The ADON stated by the licensed nurse initialing the feeding formula bottle and the water flush bag, they are attesting that they double checked the formula feeding and the water flush bag with the physician’s order.
During a review of the facility's recent P&P titled Enteral Feedings- Safety Precautions, last reviewed on 4/24/2025, the P&P indicated to ensure the safe administration of enteral nutrition.
Preparation
2. The facility will remain current in and follow accepted best practices in enteral nutrition.
Preventing errors in administration
1. Check the enteral nutrition label against the order before administration. Check the following information:
a. Resident name, ID and room number;
b. Type of formula;
c. Date and time formula was prepared;
d. Route of delivery;
e. Access site;
f. Method (pump, gravity, syringe); and
g. Rate of administration (mL/hour)
2. On the formula label document initials, date and time the formula was hung, and initial that the label was checked against the order.
e. During a review of Resident 68’s admission Record, the admission Record indicated the facility admitted the resident on 1/24/2020, and readmitted the resident on 4/29/2025, with diagnoses including protein-calorie malnutrition, gastrostomy, and dysphagia.
During a review of Resident 68’s MDS, dated [DATE], the MDS indicated the resident sometimes had the ability to make self-understood and understand others and had impaired cognition. The MDS indicated the resident had a tube feeding.
During a review of Resident 68’s Order Summary Report, dated 7/13/2025, the Order Summary Report indicated an order for Nepro 1.8 at 90 cc per hour for 12 hours via pump to provide 1080 cc/1994 kcal/day.
During a concurrent observation and interview on 7/29/2025, at 9:45 a.m., with RN 6, inside Resident 68’s room, observed Resident 68’s feeding formula bottle with no rate of infusion on the label and the water flush bag was not labeled with the name, room number, date and time it was hung, the rate of infusion, and the initial of the staff who hung the water flush bag. RN 6 stated they should place the rate of the infusion on the feeding bottle and label the water flush bag with the name, room number, date and time it was hung, and the initial of the licensed nurse who hang the formula and the water flush to ensure they are infusing the correct formula and hydration to residents to prevent weight loss and other complications.
During an interview on 8/1/2025, at 2:05 p.m., with the ADON, the ADON stated the licensed staff hanging the feeding formula and the water flush for Resident 68 should label the feeding formula and the water flush bag with the name, room number, the date and time it was hung, the rate of infusion, and the licensed nurse initial to prevent errors in administration. The ADON stated by the licensed nurse initialing the feeding formula bottle and the water flush bag, they are attesting that they double checked the formula feeding and the water flush bag with the physician’s order.
During a review of the facility's recent P&P titled Enteral Feedings- Safety Precautions, last reviewed on 4/24/2025, the P&P indicated to ensure the safe administration of enteral nutrition.
Preparation
2. The facility will remain current in and follow accepted best practices in enteral nutrition.
Preventing errors in administration
1. Check the enteral nutrition label against the order before administration. Check the following information:
a. Resident name, ID and room number;
b. Type of formula;
c. Date and time formula was prepared;
d. Route of delivery;
e. Access site;
f. Method (pump, gravity, syringe); and
g. Rate of administration (mL/hour)
2. On the formula label document initials, date and time the formula was hung, and initial that the label was checked against the order.
f. During a review of Resident 100’s admission Record, the admission Record indicated the facility admitted the resident on 3/18/2023, with diagnoses including dysphagia, gastrostomy, and gastroesophageal reflux disease (GERD, a condition where stomach acid frequently flows back into the esophagus, causing irritation and heartburn).
During a review of Resident 100’s MDS, dated [DATE], the MDS indicated the resident rarely to never had the ability to make self-understood and understand others and had severely impaired cognition. The MDS indicated the resident had a feeding tube.
During a review of Resident 100’s Order Summary Report, the Order Summary Report indicated an order for:
-7/16/2025 Jevity 1.2 at 80 cc per hour for 20 hours via pump to provide 1200 cc/1440 kcal per day.
-3/18/2023 Flush enteral tube with 50 cc of water continuously x 20 hours (Total of 1000 cc/day).
During a concurrent observation and interview on 7/29/2025, at 11:14 a.m., with RN 6, inside Resident 100’s room, observed Resident 100’s feeding formula bottle with no rate of infusion on the label and the water flush bag was not labeled with the name, room number, date and time it was hung, the rate of infusion, and the initial of the staff who hung t
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility: 1.Failed to ensure the resident was reassessed for the use of b...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility: 1.Failed to ensure the resident was reassessed for the use of bed rails (SR - also known as side rails, adjustable rigid plastic or metal bars attached to the bed that may be positioned in various locations on the bed; upper or lower, either or both sides), which includes a review of risks including entrapment (when a resident is trapped in the spaces in between or around the bed rails, mattress, or bed frame) for one of four sampled residents (Resident 102) reviewed under bedrails by failing: 1.1 To ensure an entrapment risk assessment was completed on 2/2025 for the use of bilateral half upper SR. 1.2 To ensure an entrapment risk assessment was completed on 11/26/2024, 2/2025, 5/27/2025, and 7/26/2025 for the use of lower SR up for preference or family request. 1.3 To ensure a quarterly restraint assessment was completed for 5/2025 for the use of lower SR. These deficient practices placed the resident at risk for potential accidents such as a body part being caught between the rails, falls if a resident attempts to climb over, around, between, or through the rails. 2. Failed to assess the risk of entrapment from bed rails/side rails prior to installation for two out of four sampled residents (Residents 50 and 55) reviewed for physical restraints (any action or procedure that prevents a person's free body movement to a position of choice and/or normal access to the body by the use of any method, attached or adjacent to a person's body that the person cannot control or remove easily) by failing to assess the resident for risk of entrapment from bed rails prior to installation. This deficient practice predisposed residents to bed entrapment. 3. Failed to ensure the safe and appropriate use of side rails for one of four sampled residents (Resident 10) reviewed under the Physical Restraints care area by failing to: 3.1 Ensure SR were not placed in the raised (up) position on bilateral upper (area including the arms and head) and lower sides (area including the legs) without assessing for the need, assessing for safety, and obtaining informed consent (voluntary agreement to accept treatment and/or procedures after receiving education regarding the risks, benefits, and alternatives offered) prior to use for Resident 10. This deficient practice had the potential to result in the restriction of residents' freedom of movement, a decline in physical functioning, psychosocial harm, physical harm from entrapment, and death of residents. Cross reference F604 Findings:
a. During a review of Resident 102’s admission Record (front page of the chart that contains a summary of basic information about the resident), the admission Record indicated the facility admitted the resident on 5/14/2024 with diagnoses including tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), lack of coordination, and gastrostomy (GT - a surgical opening fitted with a device to allow feedings to be administered directly to the stomach common for people with swallowing problems).
During a review of Resident 102’s History and Physical (H&P), dated 5/14/2025, the H&P indicated Resident 102 was incapacitated (refers to a state in which an individual was unable to make sound decisions or manage their affairs).
During a review of Resident 102’s Minimum Data Set (MDS - a resident assessment tool), dated 7/22/2025, the MDS indicated Resident 102 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make his needs known. The MDS further indicated Resident 102 required total assistance from staff with all activities of daily living (ADLs - activities such as bathing, dressing and toileting a person performs daily).
During a review of Resident 102’s care plan (CP) on use of lower SR up per family preference or request, initiated on 7/29/2025, and the use of bilateral half upper SR up and locked when in bed, initiated on 6/6/2024, the CP indicated to attempt to use less restrictive devices on an ongoing basis as one of the interventions to prevent or reduce incidence of injury or fall.
During a review of Resident 102’s Order Summary Report, dated 8/1/2025, the Order Summary Report indicated the following physician’s orders:
-10/8/2024 and last revised on 7/29/2025: may put lower SR up for preference or family request. Informed consent obtained from the responsible party (RP) by the physician (MD) after explanation of risks and benefits.
-5/18/2024 and last revised on 7/30/2025: bilateral upper half SR up and locked when in bed secondary to involuntary movement by gravity due to elevated head of bed.
During a review of Resident 102’s Entrapment Risk Assessment, dated 11/26/2024 and 5/27/2025, the entrapment risk assessment indicated a recommendation for the use of bilateral half upper SR due to generalized muscle weakness, poor trunk control, involuntary movement, and poor trunk control.
During a review of Resident 102’s Restraint Assessment, dated 11/26/2024 and 2/26/2025, the restraint assessment indicated the use of lower SR for preference or family request as a precautionary measure and poor trunk control to decrease potential injuries.
During a concurrent observation and interview on 7/29/2025 at 11:53 a.m. inside Resident 102’s room with Registered Nurse (RN) 7, RN 7 stated Resident 102’s both upper and lower SR were up. RN 7 stated that from her knowledge, Resident 102 is not supposed to have both upper and lower SR up. RN 7 stated the Certified Nursing Assistants (CNAs) usually put all four SR up while providing care for resident safety when turning but they must put down the lower SR after providing care. RN 7 stated Resident 102’s bilateral lower SR should have been lowered down as it was restricting the resident’s freedom of movement and can be considered a restraint. Resident 102 can get trapped in between the SR and get injured.
During a concurrent interview and record review on 7/31/2025 at 2:30 p.m. with RN 3, Resident 102’s physician orders, entrapment risk assessments, and restraint assessments were reviewed. RN 3 stated Resident 102 had a physician’s order for bilateral half upper SR and locked while in bed, dated 5/18/2024 and was revised 7/30/2025, and may put lower SR up for preference or family request, dated 10/8/2024 and was revised 7/26/2025. RN 3 stated the entrapment risk assessments for the use of bilateral half upper SR, dated 2/2025, and the entrapment risk assessment for the use of lower SR up for preference or family request for 11/26/2024, 2/2025, 5/27/2025, and 7/26/2025 were not completed. RN 3 stated the quarterly restraint assessment was not completed for 5/2025 for the use of bilateral upper and lower SR. RN 3 stated entrapment risk assessments and restraint assessments are completed during admission, quarterly, or as needed. RN 3 stated entrapment risk assessment are completed to ensure resident safety with the use of SR when in bed. RN 3 stated Resident 102’s entrapment risk assessments should have been completed for the use of both bilateral half upper for 2/2025 and the use of lower SR up for 11/26/2024, 2/2025, 5/27/2025, and 7/26/2025 to ensure that the use of SR was appropriate and Resident 102 was not at risk of getting trapped in between the SR and the bed mattress/frame which could to injuries. RN 3 stated Resident 102’s quarterly restraint assessment for the use of bilateral half upper and lower SR up should have been completed for 5/2025 to ensure the use of both upper and lower SR were still needed and the resident still meets the criteria for the use of all SR up while in bed as the use of all SR up was restricting Resident 102’s freedom of movement and is considered a restraint.
During a concurrent interview and record review on 7/31/2025 at 4:15 p.m. with the Director of Nursing (DON), Resident 102’s physician orders, entrapment risk assessments, and restraint assessments were reviewed. The DON stated Resident 102 had a physician’s order for bilateral half upper SR and locked while in bed, dated 5/18/2024 and was revised on 7/30/2025, and may put lower SR up for preference or family request, dated 10/8/2024 and was revised on 7/26/2025. The DON stated the entrapment risk assessments for the use of bilateral half upper SR, dated 2/2025, and the entrapment risk assessment for the use of lower SR up for preference or family request for 11/26/2024, 2/2025, 5/27/2025, and 7/26/2025 were not completed. The DON stated the quarterly restraint assessment was not completed on 5/2025 for the use of bilateral upper and lower SR. The DON stated entrapment risk assessments and restraint assessments are completed during admission by the admitting nurse if using bilateral half upper and/or lower SR up, then quarterly and as needed together with the MDS assessments. The DON stated entrapment risk assessments are completed quarterly to ensure the continued use of the side rails are still safe for the residents when in bed. The DON stated Resident 102’s entrapment risk assessments should have been completed for the use of both bilateral half upper for 2/2025 and the use of lower SR up for 11/26/2024, 2/2025, 5/27/2025, and 7/26/2025 to ensure that the use of SR was appropriate and Resident 102 was not at risk of getting trapped in between the SR and the bed mattress/frame which could to injuries and/or hospitalization. RN 3 stated Resident 102’s quarterly restraint assessment for the use of bilateral half upper and lower SR up should have been completed for 5/2025 to ensure the use of both upper and lower SR were still a necessity and the resident still meets the criteria for the use of all SR up while in bed as the use of all SR up was restricting Resident 102’s freedom of movement and can be considered a restraint.
b. During a review of Resident 50’s admission Record, the admission Record indicated the facility admitted the resident on 10/5/2014, and readmitted the resident on 4/30/2025, with diagnoses including hemiplegia (total paralysis of the arm, leg, and trunk on the same side of the body) and hemiparesis (is muscle weakness on one side of the body, making everyday activities like walking or using a fork difficult), lack of coordination, and muscle weakness.
During a review of Resident 50’s H&P, dated 4/30/2025, the H&P indicated the resident was able to make decisions for activities of daily living.
During a review of Resident 50’s MDS, dated [DATE], the MDS indicated the resident was able to make self-understood and understand others and had intact cognition (having normal or unimpaired cognitive abilities, including thinking, learning, memory, and decision-making). The MDS indicated the resident had upper and lower extremity impairment and was dependent to requiring substantial assistance on mobility and ADLs.
During a review of Resident 50’s Order Summary Report, dated 5/29/2025, the Order Summary Report indicated an order for bilateral half side rails up and locked when in bed for safety, balance, ADLs, changes, positioning, and as an enabler every shift. The Order Summary Report indicated an informed consent was obtained from resident/responsible party after explanation of risks and benefits and verified with MD.
During a review of Resident 50’s Fall Risk Evaluation, dated 8/4/2025, the Fall Risk Evaluation indicated the resident was high risk for falls.
During a review of Resident 50’s Care Plan (CP) Report titled “Resident is at risk for falls/injury related to history of falls, CVA,” last revised on 7/4/2025, the CP Report indicated an intervention of bilateral ¼ rails up as enabler for bed mobility and transfer.
During a concurrent observation and interview on 7/31/2025 at 9:31 a.m. with Licensed Vocational Nurse (LVN) 6 inside Resident 50’s room, Resident 50 had both upper side rails up and the left lower side rails up. LVN 6 stated the bed rails were used as an enabler and to prevent falls on resident. LVN 6 stated before applying a bedrail to a resident, they should have a physician’s order, informed consent, assessment for entrapment, and care plan on its use. LVN 6 stated it is important to have a physician’s order, informed consent, assessment for entrapment and a comprehensive care plan on its use to ensure the bedrails were safe to use.
During a concurrent interview and record review on 7/31/2025 at 11:55 a.m. with RN 3, reviewed Resident 50’s Order Summary Report, Informed Consent, Side Rails Assessment, and Care Plan. RN 3 stated the resident’s side rails did not have any assessment for entrapment prior to its use. RN 3 also stated the resident’s care plan resident is at risk for falls/ injury indicated the side rails as an intervention to prevent falls. RN 3 stated it was important to assess the use of bedrails prior to its use and quarterly to ensure it is still needed and it is safe to use.
During an interview on 8/1/2025 at 2:05 p.m. with the Assistant Director of Nursing (ADON), the ADON stated before applying side rails/bedrails on Resident 50, the licensed staff should have obtained a physician’s order, informed consent, side rails assessment for entrapment, and a care plan. The ADON stated the use of bedrails/siderails can be a restraint if the primary use was to prevent the resident from getting out of the bed easily such as for fall prevention. The ADON stated they are very cautious on the use of side rails because the residents can climb up from the side rails and sustain a higher elevation of fall causing injuries. The ADON also stated the bedrails/side rails should be assessed upon use and quarterly to ensure its safe use.
c. During a review of Resident 55’s admission Record, the admission Record indicated the facility admitted the resident on 4/18/2025, with diagnoses including injury at C5 (a bone in the neck area) level of cervical spinal cord (damage to the spinal cord in the neck area), intervertebral disc degeneration of lumbar region (a common condition where the cushioning discs between the vertebrae in your spine wear down over time), and need for assistance with personal care.
During a review of Resident 55’s H&P, dated 4/19/2025, the H&P indicated the resident had the capacity to understand and make decisions.
During a review of Resident 55’s MDS, dated [DATE], the MDS indicated the resident had the ability to make self-understood and understand others and had intact cognition. The MDS indicated the resident was dependent to requiring set up assistance on mobility and ADLs.
During a review of Resident 55’s Order Summary Report, dated 5/28/2025, the Order Summary Report indicated an order for bilateral upper half side rails up and locked when in bed for safety, balance, ADLs, changes, positioning, and as an enabler. Informed consent obtained from RP after explanation of risks and benefits, and verified with MD every shift.
During a review of Resident 55’s Fall Risk Evaluation, dated 8/1/2025, the Fall Risk Evaluation indicated the resident was moderate risk for falls.
During a concurrent observation and interview on 7/31/2025 at 9:37 a.m. with Certified Nursing Assistant (CNA) 11, Resident 55 bed had both upper side rails up. CNA 11 stated the resident is high risk for falls and they put up the upper side rails up to prevent the resident from falling out of the bed.
During a concurrent interview and record review on 7/31/2025 at 11:51 a.m. with RN 3, Resident 55’s Order Summary Report, Informed Consent, Side Rails Assessment, and Care Plan were reviewed. RN 3 stated the resident’s side rails did not have any assessment for entrapment prior to its use. RN 3 also stated the resident’s care plan resident is at risk for falls/ injury indicated the side rails as an intervention to prevent falls. RN 3 stated the licensed staff should have assessed the use of bedrails/side rails prior to its use to prevent the risk of entrapment to residents.
During an interview on 8/1/2025 at 2:05 p.m. with the ADON, the ADON stated before applying side rails on Resident 55, the licensed staff should have obtained for a physician’s order, informed consent, side rails assessment for entrapment, and a care plan. The ADON stated the use of bedrails/siderails can be a restraint if the primary use was to prevent the resident from getting out of the bed easily such as for fall prevention. The ADON stated they are very cautious on the use of side rails because the residents can climb up from the side rails and sustain a higher elevation of fall causing injuries. The ADON stated prior to application of the bedrail/side rail on Resident 55, the licensed staff should have assessed the resident for entrapment to ensure its safe use.
d. During a review of Resident 10’s admission Record (AR), the AR indicated the facility admitted the resident on 12/7/2024 and most recently admitted the resident on 12/23/2024 with diagnoses that included nontraumatic intracerebral hemorrhage (a type of stroke caused by bleeding in the brain), hemiplegia (total paralysis of the arm, leg, and trunk on the same side of the body) and hemiparesis (partial paralysis or weakness on one side of the body) affecting left non-dominant side, and need for assistance with personal care.
During a review of Resident 10’s MDS, dated [DATE], the MDS indicated the resident was sometimes able to understand others and was sometimes able to be understood. The MDS further indicated the resident was totally dependent on staff for dressing, bathing, toileting, and personal hygiene.
During a review of Resident 10’s H&P, dated 12/24/2024, the H&P indicated the resident was able to understand and make decisions. The H&P further indicated the resident was able to move both the lower extremities and was able to move the right upper extremity.
During a review of Resident 10’s CP titled, “Resident is on: lower bed, floor mat, and bilateral half upper SRs up and locked,” initiated 12/17/2024, the CP indicated a goal to prevent or reduce incidents of injury / fall as well as for comfort of getting in and out of bed. The CP indicated interventions including attempt to use the least restrictive devices on an ongoing basis.
During a review of Resident 10’s Order Summary Report, the Order Summary Report indicated a physician’s order for the following:
- [non-restraint] bilateral upper half side rails up and locked when in bed for safety, balance, activities of daily living, positioning, and as an enabler. Informed consent obtained from resident / responsible party after explanation of risk and benefits, and verified by medical doctor, dated 5/29/2025.
During a review of Resident 10’s SR Entrapment Assessment, dated 6/23/2025, the SR Entrapment Assessment indicated a recommendation of bilateral half upper SRs.
During an observation on 7/29/2025 at 3:45 p.m. with Resident 10, observed Resident 10 lying in bed with the bilateral lower and bilateral upper SRs in the raised position.
During a concurrent observation and interview on 7/30/2025 at 10:07 a.m. with Resident 10 and Restorative Nurse Aide (RNA) 1, Resident 10 laid in bed with all four SRs in the raised position. RNA 1 walked to Resident 10’s bedside. RNA 1 stated Resident 10 had all four SRs in the raised position and RNA 1 did not know why all the SRs were up.
During an interview on 7/30/2025 at 10:15 a.m. with CNA 9, CNA 9 stated CNA 9 was assigned to care for Resident 10. CNA 9 stated CNA 9 did not put Resident 10’s bilateral lower SRs in the raise position because that would be considered a restraint. CNA 9 stated CNA 9 did not know who placed all four of Resident 10’s SRs up.
During a concurrent interview and record review on 7/31/2025 at 10:27 a.m. with RN 3, Resident 10’s physician orders, SR Entrapment Assessment, dated 6/23/2025, and Informed Consents were reviewed. RN 3 stated the facility uses hospital beds that have bilateral lower and upper SRs attached to the bed. RN 3 stated sometimes the CNAs just put all four SRs up just because the SRs are there. RN 3 stated Resident 10 had an assessment and order for only two upper SRs. RN 3 stated Resident 10 should not have all four SRs in the raised position because there was no need for all four SRs, there was no assessment for the safety of the bilateral lower SRs, no physician’s order for the use of bilateral lower SRs, and no informed consent for bilateral SRs. RN 3 stated the use of four SRs is considered a restraint because Resident 10 would not be able to lower the SRs and the SRs may prevent the resident from moving freely. RN 3 stated Resident 10 is able to move the legs and there was a potential for entrapment if the resident got caught between the bed and the lower SRs. RN 3 stated when a resident becomes caught it may result in an injury or even death of the resident if they are not found in time. RN 3 stated using the use of four SRs may also result in the resident feeling confined to the bed resulting in psychosocial issues.
During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the ADON, the facility’s P&P regarding SRs and Restraints were reviewed. The ADON stated that when SRs are used, informed consent is obtained and an initial safety assessment is completed to ensure entrapment and falls are prevented. The ADON stated in general residents may use bilateral upper sides rails for safety and repositioning. The ADON stated when all four SRs are up a resident is not able to remove the SRs and it confines the resident to one specific area and is considered a restraint. The ADON stated Resident 10 should not have had all four SRs raised and it was every staff members responsibility to ensure the lower SRs were not up. The ADON stated when Resident 10 had all four SRs in use, there was the potential to result in complications like injury to the resident if the resident tried to get over the SR to get out of the bed or psychosocial effects causing stress to the resident when they could not move out of the bed.
During a review of the facility’s policy and procedure (P&P) titled, “Bed Safety and Bed Rails,” last reviewed on 4/24/2025, the P&P indicated the use of bed rails is prohibited unless the criteria for use of bed rails have been met. The P&P further indicated:
-Use of bed rails:
1. Bed rails are adjustable metal or rigid plastic bars that attach to the bed. They are available in a variety of types, shapes, and sizes ranging from full to one-half, one-quarter, or one-eight lengths. For the purpose of this policy “bed rails” include:
a. Side rails
b. Safety rails
c. Grab/assist bars
2. The use of bed rails or SR (including temporarily raising the SR for episodic use during care) is prohibited unless the criteria for use bed rails have been met, including attempts to use alternatives, interdisciplinary evaluation, resident assessment, and informed consent.
3. If attempted alternatives do not adequately meet the resident’s needs the resident may be evaluated for the use of bed rails. The interdisciplinary evaluation includes:
a. An evaluation of the alternatives to bed rails that were attempted and how these alternatives failed to meet the residents’ needs
b. The resident’s risk associated with the use of bed rails.
c. Input from the resident and/or representative
d. Consultation with the attending physician.
During a review of the facility’s P&P titled, “Use of Restraints,” last reviewed on 4/24/2025, the P&P indicated when the use of restraints is indicated, the least restrictive alternatives will be used for the least amount of time necessary, and the ongoing re-evaluation for the need for restraints will be documented. The P&P further indicated:
-“Physical Restraints” are any manual method, or physical or mechanical device, material, or equipment attached or adjacent to the resident’s body that the individual cannot remove easily, which restricts freedom of movement or restricts normal access to one’s body.
-The definition of restraint is based on the functional status of the resident and not the device. If the resident cannot remove a device in the same way the staff applied it, given that resident’s physical condition (i.e. side rails are put back down, rather than climbed over), and this restricts his or her typical ability to change position or place, that device is considered a restraint.
-Prior to placing a resident in restraints, there shall be an assessment and a review to determine the need for restraints. The assessment shall be used to determine possible underlying causes of the problematic medical symptoms and to determine if there are less restrictive interventions that may improve the symptoms.
-Restraints individuals shall be reviewed regularly (at least quarterly) to determine whether they are candidates for restraint reduction, less restrictive methods of restraints, or total restraint elimination.
During a review of the facility P&P titled, “Resident Rights,” last reviewed 4/24/2025, the P&P indicated federal and state laws guarantee certain basic rights to all residents of this facility. These rights include the resident's right to be free from involuntary seclusion and physical or chemical restraints not required to treat the resident's symptoms.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure Registered Nurse (RN) 1, RN 2, Licensed Vocational Nurse (LV...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure Registered Nurse (RN) 1, RN 2, Licensed Vocational Nurse (LVN) 1, Certified Nursing Assistant (CNA) 1, CNA 2, and CNA 3 had the skills and knowledge to identify and prevent one of one sampled resident (Resident 97) who was an identified as an elopement (the act of leaving a facility unsupervised and without prior authorization) risk, from eloping. This deficient practice resulted in Resident 97 eloping from the facility on 7/25/2025 at 12:14 p.m. Findings:During a review of Resident 97 admission Record (AR), the AR indicated the facility admitted Resident 97 on 4/3/2024 and readmitted the resident on 5/10/2024 with diagnoses included aphasia (a disorder that makes it difficult to speak), dysphagia (difficulty swallowing), history of falling, anxiety (a feeling of unease, worry, or fear), and depression (a mental health condition that makes you feel persistently sad and lose interest in things you usually enjoy). During a review of Resident 97's Change of Condition (COC- when there is a sudden change in a resident's condition) interaction assessment form, dated 1/29/2025 at 9 p.m., the COC interaction assessment form indicated Resident 97 eloped and fell in front of the facility. The nursing notes indicated at 9 p.m. notified by CNA and LVN that Resident 97 was walking on Riverside past subacute and attempting to cross Riverside. CNA and LVN were able to bring Resident 97 back to the facility, as he was walking up the stairs, lost his footing and fell. During a review of Resident 97's care plan (a document outlining a detailed approach to care customized to an individual resident's need) for elopement, initiated on 1/29/2025, the care plan indicated Resident 97 sometimes leaves the facility without authorization and permission. The care plan interventions included administer medications as ordered, notify physician and responsible party of COC, and staff will assist to activities of residents' choice. During a review of Resident 97's Minimum Data Set (MDS - a resident assessment tool), dated 5/17/2025, the MDS indicated Resident 97 sometimes understood and was sometimes able to be understood. The MDS indicated Resident 97 coughed and choked during meals or when swallowing medications. During a review of Resident 97's Elopement Evaluation, dated 5/18/2025, the Elopement Evaluation indicated Resident 97 had an elopement score of 1 (score value of 1 or higher indicates risk for elopement). During a review of Resident 97' Fall Risk Evaluation, dated 5/18/2025, the Fall Risk Evaluation indicated Resident 97 fall risk score was 7 (total score is 10 or greater, the resident should be considered at high risk for potential falls). The Fall risk Evaluation indicated Resident 97 had balance problems while walking. During a review of Resident 97's Physician Orders, dated 5/19/2025, the Physician Orders indicated falling star program, frequent visual monitoring due to higher risk for fall and injury. Document per shift, every shift. During a review of Resident 97's care plan for falling star program, initiated on 5/19/2025, the care plan indicated Resident 97 was at risk for falls related to antihypertensive medication, auditory deficits (a type of hearing loss caused by something affecting the part of the brain that processes how you hear), balance deficits, cognitive impairment, decreased strength and endurance, history of falls, noncompliant with request for assistance nonuse of call lights, poor safety awareness and judgment, unsteady gait, difficulty in walking, and muscle weakness. The care plan intervention indicated to remind staff during huddle on resident high fall risk status, frequent visual monitoring, and place resident close to nursing station for close observation. During a review of Resident 97's History and Physical (H&P - comprehensive assessment conducted by a healthcare provider that includes gathering a thorough medical history from the resident and performing a physical examination to assess their overall health and identify any potential medical concern), dated 5/22/2025, the H&P indicated Resident 97 did not have the capacity to understand and make decisions. During a review of Resident 97's COC interact assessment dated [DATE] at 5:20 p.m., the COC interact assessment indicated Resident 97 eloped. The nursing notes indicated at 5 p.m., while passing dinner trays, CNA 2 noted that Resident 97 was not in his assigned room. CNA 2 informed RN 2, who immediately initiated a thorough search of the facility. A code green (missing resident) was activated to alert all facility staff and initiate a coordinated facility wide search. At approximately 6:30 p.m. RN 2 contacted the DON to report incident, provide timeline and give update of search effort. RN 2 then notified the local police department and reported Resident 97 as missing and requested assistance with search. RN 2 contacted both Resident 97's sisters to inform them of the situation and to verify whether they had seen or heard form Resident 97, neither reported recent contact with Resident 97. During a review of Resident 97's General Acute Care Hospital (GACH) 1 record dated 7/25/2025 at 2:23 p.m., the GACH 1 records indicated Resident 97 was admitted due to trauma. The GACH 1's Medicine H&P notes indicated Resident 97 was brought in by Emergency Medical Services (EMS) from community for possible ground level fall. The GACH 1's Medicine H&P notes indicated Resident 97 had a cervical collar (a medical device that supports the neck and limits its movement) was tearful, crying, and pointing at the ceiling. Resident 97 noted for small right frontal scalp contusion. The GACH 1 records further indicated that Resident 97`s precaution orders were started on 7/29/2025 for fall and aspiration precautions. During a review of the facility provided Close Circuit Television (CCTV - video surveillance technology) video footage of the camera located in the facility lobby, on 7/29/2025 at 2:20 p.m. with the Administrator (Adm), the Adm stated Resident 97 is observed in the lobby camera with a dated of 7/25/2025 at 12:14 p.m. observed a visitor open the door that lead to the lobby, Resident 97 is observed entering the lobby and then exiting the front door of the facility. During an interview on 7/30/2025 at 11:48 a.m. with CNA 1, CNA 1 stated Resident 97 will communicate with gestures and or grab the staff by the hand and show them what he wants when he wants a shower will indicate with gestures he wants a shower, not verbal at all. CNA 1 stated she (CNA 1) worked on 7/25/2025 and Resident 97 was assigned to her. CNA 1 stated the last time she saw Resident 97 on 7/25/2025 was around 11:15 a.m. to 11:20 a.m. prior to lunch when the resident was in his (Resident 97) room. CNA 1 stated for lunch she (CNA 1) placed Resident 97's tray on his bedside table, and observed that the bathroom door was closed. CNA 1 stated Resident 97 was independent with bowel and bladder, and she (CNA 1) assumed Resident 97 was in the bathroom. CNA 1 stated she returned to pick up Resident 97`s tray sometime after 1p.m., she (CNA 1) noted that Resident 97`s food tray was untouched and nothing was consumed, and the resident`s bathroom door was still closed. CNA 1 stated she (CNA 1) did not knock or open the bathroom door to check if Resident 97 was in the bathroom. During an interview on 7/30/2025 at 1:29 p.m. with LVN 1, LVN 1 stated he (LVN1) was the nurse for Resident 97 on 7/25/2025 for the 7a.m. to 3 p.m. shift checked Resident 97's blood sugar 11 a.m. to 12 p.m. prior to lunch. LVN 1 stated checks on residents from time to time but for Resident 97 did not check on him anymore because Resident 97 is ambulatory and if Resident 97 needs anything he will come and find staff. LVN 1 stated Resident 97 does cry and gestures he wants to go home by clinging onto his family members when they show up. LVN 1 stated Resident 97 has never eloped, LVN 1 stated during shift change he is told which resident are elopement risk, all doors have an alarm, and we monitor the doors constantly, LVN 1 stated the front door to the lobby does not have an alarm. LVN 1 Resident 97 is not elopement risk and has never eloped, LVN 1 stated was not aware of the elopement in January. LVN 1 stated not aware of Resident 97 showing signs of elopement. During an interview on 7/30/2025 at 2:13 p.m. with RN 1, RN 1 stated she (RN 1) worked on 7/25/2025. RN1 stated she (RN 1) was not aware Resident 97 was an elopement risk but was told later Resident 97 tried to elope previously. RN 1 stated last time she saw Resident 97 was around 12 p.m. at nurses' station by intravenous (IV-within a vein) cart while he was walking around. During an interview on 7/30/2025 at 3 p.m. with CNA 2, CNA 2 stated she (CNA 2) worked on 7/25/2025 around 3p.m. CNA3 stated she (CNA 2) did her rounds and did not see Resident 97 which was not strange because Resident 97 likes to ambulate and likes to attend activity. CNA 2 thought Resident 97 was in either place. CNA 2 stated during the dinner time at 5 p.m. she (CNA 2) told RN 2 that she (CNA 2) could not find Resident 97. CNA 2 stated all staff started looking for Resident 97 inside the facility for maybe 30 minutes, then staff went outside the facility, walked around the block. CNA 2 stated some staff went in cars looking through the street. CNA 2 stated staff looked for Resident 97 for about an hour. CNA 2 stated she (CNA 2) was not aware Resident 97 was an elopement risk. During an interview on 7/30/2025 at 4:18 p.m. with RN 2, RN 2 stated Resident 97 is alert and oriented to self with confusion, walks in the facility without assistive devices. RN 2 stated Resident 97 has been crying and pointing at the door since last week. RN2 stated Resident 97 cries because he wants to go home. RN 2 stated that he (RN 2) worked on 7/25/2025 from 3 p.m. to 11 p.m. shift. RN 2 stated that on 7/25/2025 for Resident 97, RN1 did not report anything to him (RN 2). RN 2 stated that at around 5 p.m. to 5:20 p.m., CNAs were passing out dinner trays and CNA 2 reported RN 2 that she had not seen Resident 97. RN2 stated he looked for Resident 97 and at 5:30 p.m. he (RN 2) called Code Green, meaning missing resident. RN 2 started he continued Resident 97`s search in the facility for about 20 minutes then he (RN 2) went outside the facility at around 6p.m. for an hour. RN 2 stated he (RN 2) called the DON at around 6:30 p.m. and informed the DON Resident 97 was missing. RN 2 stated another staff called the local police. RN 2 stated Resident 97 was not an elopement risk; Resident 97 has never tried to go outside of the facility. RN 2 stated was not aware Resident 97 had eloped back in January. During an interview on 7/31/2025 at 8:34 a.m. with CNA 1, CNA1 stated Resident 97 has depression and someday he cries. CNA 1 stated Resident 97 he was crying for like 3 days at that point. CNA1 stated she (CNA 1) would ask Resident 97 if he wanted to see his sister and Resident 97 would nod yes. CNA 1 stated Resident 97 would cry when he saw staff or any person. CNA 1 stated Resident 97 would cry for about 10 minutes, would ask if he was in pain and Resident 97 would say no then would ask if he was sad and Resident 97 would nod yes. CNA1 stated she (CNA 1) would tell RNs and LVN 1 that Resident 97 would be crying and they would go and see Resident 97. CNA 1 stated Resident 97 had never attempted to get out. CNA 1 stated she (CNA 1) was not aware that Resident 97 eloped in January. CNA 1 stated Resident 97 would point outside, and CNA 1 would ask Resident 97 do you want to go with your sister and Resident 97 would nod yes. CNA 1 stated Resident 97 would attempt to open the lobby door, but he was not able to open it and usually activity personnel would catch him and redirect him. CNA 1 stated Resident 97 kept pointing to go outside, he (Resident 97) was showing signs he wanted to leave but was unable to open the door. CNA 1 stated someone opened the door for Resident 97. During an interview on 7/31/2025 at 12:19 p.m. with the DON, the DON stated Resident 97 had prior elopement on 1/29/2025, attempted to cross the street. The DON stated Resident 97 eloped on 7/25/2025, staff were made aware around 5 p.m., she (DON) was informed around 6 p.m. and the police was notified around 6:30 p.m. The DON stated Resident 97 was an elopement risk, Resident 97 had an elopement in January and had a few incidents. The DON stated intervention for residents with elopement residents are visual checks, distraction, calling families to help, psychiatric evaluations if needed, monitor if medication are prescribed, but the most important intervention is visualization. The DON reviewed Resident 97's care plan for elopement did not indicate visualization. The DON stated the care plan is not patient centered. The DON stated the care plan should include visualization and should be patient centered. The DON stated the potential can be that the resident can elope again and potential for harm to the resident. The DON stated the care plan is a guide for care or specifics activities for the residents. The DON stated staff review care plans as a reference on how care should be done for the residents. During an interview on 8/1/2025 at 12:39 p.m. with LVN 1, LVN 1 stated was unaware Resident 97 was an elopement risk prior to Resident 97 elopement (7/25/2025). During a review of the facility's policy and procedures (P&P) titled, Wandering and Elopements, last reviewed on 4/24/2025, the P&P indicated the facility will identify residents who are at risk of unsafe wandering and strive to prevent harm while maintaining the least restrictive environment for residents. If identified as at risk for wandering, elopement, or other safety issues, the resident's care plan will include strategies and interventions to maintain the resident's safety. During a review of the facility's P&P titled, Staffing, Sufficient and Competent Nursing, last reviewed on 4/24/2025, the P&P indicated the facility provides sufficient numbers of nursing staff with the appropriate skills and competency necessary to provide nursing and related care and services for all residents in accordance with resident care plans and the facility assessment.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents were free of any significant medication errors (th...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents were free of any significant medication errors (the observed or identified preparation or administration of medications or biologicals which are not in accordance with the prescriber's order, manufacturer's specifications, and accepted professional standards) by failing to rotate (a method to ensure repeated injections are not administered in the same area) subcutaneous (sq, beneath the skin) insulin (a hormone that removes excess sugar from the blood, can be produced by the body or given artificially via medication) administration sites for three of three sampled residents (Residents 21, 103, and 8) reviewed for insulin use. The deficient practice had the potential for adverse effect (unwanted, unintended result) of the same site subcutaneous administration of insulin such as excessive bruising, lipodystrophy (abnormal distribution of fat) and cutaneous amyloidosis (is a condition in which clumps of abnormal proteins called amyloids build up in the skin). Cross reference F658 Findings: 1.During a review of Resident 21’s admission Record (front page of the chart that contains a summary of basic information about the resident), the admission Record indicated the facility admitted the resident on 12/3/2024, and readmitted the resident on 12/17/2024, with diagnoses including Type two diabetes mellitus (DM 2, a disorder characterized by difficulty in blood sugar control and poor wound healing) with diabetic neuropathy (disease or dysfunction of one or more nerves, typically causing numbness or weakness in the hands and feet), and diabetic chronic kidney disease (a condition where diabetes damages the kidneys, making them less effective at filtering waste from the blood).
During a review of Resident 21’s History and Physical (H&P), dated 12/18/2024, the H&P indicated the resident had the capacity to understand and make decisions.
During a review of Resident 21’s Minimum Data Set (MDS, a resident assessment tool), dated 6/26/2025, the MDS indicated the resident had the ability to make self-understood and understand others and had intact cognition (means that a person's mental abilities are working well and are not impaired). The MDS indicated the resident was on a high-risk drug class hypoglycemic medication (refers to drugs that help lower high blood sugar levels).
During a review of Resident 21’s Order Summary Report, dated 3/14/2025, the Order Summary Report indicated an order for:
Insulin Glargine Subcutaneous Solution (Insulin Glargine). Inject 22 unit (is a way to measure the amount of insulin needed to help the body use blood sugar [glucose] properly) subcutaneously in the evening for DM 2 (Rotate injection site) Hold for blood sugar (BS) less that (<) 100.
Insulin Aspart Injection Solution 100 unit per milliliters (unit/ml, how much insulin is packed into a given volume of liquid) (Insulin Aspart). Inject as per sliding scale (adjusting the amount of insulin a person takes based on their current blood sugar level): if 70 - 150 = 0 unit and follow hypoglycemia (low blood sugar) protocol and call MD; 151 - 200 = 2 unit; 201 - 250 = 4 unit; 251 - 300 = 6 unit; 301 - 350 = 8 unit; 351 - 400 = 10 unit call MD if BS greater than (>) 400, subcutaneously before meals for DM 2 Rotate injection site. Give 8 ounces (oz, a unit of volume) of orange juice for BS <70 and inject 4 unit subcutaneously before meals for DM.
Insulin Aspart Injection Solution (Insulin Aspart). Inject as per sliding scale: if 70 - 150 = 0 unit and follow hypoglycemia protocol and call MD; 151 - 200 = 2 unit; 201 - 250 = 4 unit; 251 - 300 = 6 unit; 301 - 350 = 8 unit; 351 - 400 = 10 unit, call MD if BS >400, subcutaneously at bedtime for DM 2 (rotate injection site). Give 8 oz of orange juice for BS <70 and inject 4 unit subcutaneously at bedtime for dm.
During a review of Resident 21’s Location of Administration Report of insulin for 5/2025 to 7/2025, the Location of Administration Report indicated:
-Insulin Aspart Injection Solution 100 unit/ml was administered on,
7/2/2025 at 11:26 a.m. on the Abdomen – Left Lower Quadrant (LLQ)
7/2/2025 at 11:30 a.m. on the Abdomen – LLQ
7/2/2025 at 5:28 p.m. on the Abdomen – Right Lower Quadrant (RLQ)
7/3/2025 at 12:31 p.m. on the Abdomen – RLQ
7/4/2025 at 4:49 p.m. on the Abdomen - LLQ
7/4/2025 at 4:50 p.m. on the Abdomen – LLQ
7/6/2025 at 2:29 p.m. on the Abdomen – Left Upper Quadrant (LUQ)
7/6/2025 at 6:24 p.m. on the Abdomen – LUQ
7/7/2025 at 4:47 p.m. on the Abdomen – Right Upper Quadrant (RUQ)
7/8/2025 at 8:03 a.m. on the Abdomen – RUQ
7/9/2025 at 5:13 p.m. on the Abdomen - RUQ
7/10/2025 at 6:31 a.m. on the Abdomen - RUQ
7/10/2025 at 6:32 a.m. on the Abdomen – RUQ
7/10/2025 at 5:20 p.m. on the Abdomen - LLQ
7/10/2025 at 5:20 p.m. on the Abdomen – LLQ
7/12/2025 at 6:26 a.m. on the Abdomen - LLQ
7/12/2025 at 6:27 a.m. on the Abdomen - LLQ
7/12/2025 at 4:17 p.m. on the Abdomen – LLQ
7/13/2025 at 11:35 a.m. on the Abdomen - RLQ
7/13/2025 at 11:35 a.m. on the Abdomen - RLQ
7/13/2025 at 4:31 p.m. on the Abdomen - LLQ
7/13/2025 at 4:31 p.m. on the Abdomen – LLQ
7/13/2025 at 11:35 a.m. on the Abdomen - RLQ
7/13/2025 at 11:35 a.m. on the Abdomen - RLQ
7/13/2025 at 4:31 p.m. on the Abdomen - LLQ
7/13/2025 at 4:31 p.m. on the Abdomen – LLQ
7/16/2025 at 4:49 p.m. on the Abdomen - LLQ
7/16/2025 at 4:49 p.m. on the Abdomen - LLQ
7/17/2025 at 7:08 a.m. on the Abdomen - RLQ
7/17/2025 at 7:08 a.m. on the Abdomen - RLQ
7/17/2025 at 11:30 a.m. on the Abdomen - RLQ
7/17/2025 at 2:17 p.m. on the Abdomen – RLQ
7/18/2025 at 11:39 a.m. on the Abdomen - RLQ
7/18/2025 at 1:45 p.m. on the Abdomen – RLQ
7/19/2025 at 11:38 a.m. on the Abdomen - RLQ
7/19/2025 at 1:39 p.m. on the Abdomen – RLQ
7/21/2025 at 5:03 p.m. on the Abdomen - RUQ
7/21/2025 at 5:03 p.m. on the Abdomen - RUQ
7/2220/25 at 11:31 a.m. on the Abdomen - LLQ
7/22/2025 at 11:31 a.m. on the Abdomen - LLQ
7/22/2025 at 4:44 p.m. on the Abdomen - RUQ
7/22/2025 at 4:44 p.m. on the Abdomen – RUQ
7/24/2025 at 5:46 a.m. on the Abdomen - LLQ
7/24/2025 at 5:47 a.m. on the Abdomen - LLQ
7/24/2025 at 11:30 a.m. on the Abdomen - RLQ
7/24/2025 at 2:47 p.m. on the Abdomen – RLQ
7/24/2025 at 4:16 p.m. on the Abdomen - LLQ
7/25/2025 at 4:33 p.m. on the Abdomen – LLQ
7/27/2025 at 5:45 p.m. on the Abdomen - RLQ
7/28/2025 at 7:16 a.m. on the Abdomen - RLQ
7/28/2025 at 7:16 a.m. on the Abdomen - RLQ
7/28/2025 at 11:27 a.m. on the Abdomen - LLQ
7/28/2025 at 11:28 a.m. on the Abdomen – LLQ
During a review of Resident 21’s Care Plan (CP) Report titled “Resident is at risk for hypoglycemia and hyperglycemia related to diabetes mellitus,” last revised on 1/3/2025, the CP Report indicated an intervention to administer medications as ordered.
During concurrent interview and record review on 7/31/2025, at 11:37 a.m., with RN 3, reviewed Resident 21’s Medical Diagnosis, Order Summary Report, Location of Administration of insulin from 5/2025 to 7/2025, and Care Plan. RN 3 stated there were multiple instances where the licensed staff did not rotate the insulin administration sites of insulin on Resident 21. RN 3 stated the sites of insulin administration should be rotated to prevent irritation, pain and discomfort on the frequented sites of administration. RN 3 also stated the sites of administration of insulin was also rotated to prevent lipodystrophy (lump or accumulation of fatty tissue under skin) on residents. RN 3 stated injecting insulin on the sites of lipodystrophy can render the insulin ineffective due to poor absorption that can lead to hyper or hypoglycemia on Resident 21. RN 3 stated their current electronic medication administration record had a capability of checking where the last site of administration of insulin and there was no reason for the licensed staff to repeat the site of insulin administration. RN 3 stated not rotating insulin sites of administration is a medication error.
During an interview on 8/1/2025, at 2:05 p.m., with the Assistant Director of Nursing (ADON), the ADON stated the licensed staff should have rotated the insulin administration sites to Resident 21 to prevent skin irritation and lipodystrophy. The ADON stated that administering insulin on the same site can cause lipodystrophy that could affect the absorption of insulin leaving them ineffective to lower the blood sugar level of Resident 21. The ADON stated not rotating insulin administration sites is considered a medication error.
During a review of the facility's recent policy and procedure (P&P) titled Insulin Administration, last reviewed on 4/24/2025, the P&P indicated to provide guidelines for the safe administration of insulin to residents with diabetes.
Steps in the Procedure (Insulin Injections via Syringe)
8. Select an injection site.
a. Insulin may be injected into the subcutaneous tissue of the upper arm, and the anterior or lateral areas of the thighs and abdomen. Avoid the area approximately 2 inches around the navel.
b. Injection sites should be rotated, preferably within the same general area (abdomen, thigh, upper arm).
During a review of the facility's recent P&P titled Adverse Consequences and Medication Errors, last reviewed on 4/24/2025, the P&P indicated a medication error is defined as the preparation or administration of drugs and biological which is not in accordance with physician's orders, manufacturer specifications, or accepted professional standards and principles of the professional(s) providing services.
During a review of the facility-provided Highlights of Prescribing Information on the use of Insulin Aspart injection, for subcutaneous or intravenous use, with initial U.S. approval in 2000, the Highlights of Prescribing Information indicated to rotate injection sites within the same region from one injection to the next to reduce risk of lipodystrophy and localized cutaneous amyloidosis.
During a review of the facility-provided Highlights of Prescribing Information on the use of Lantus (insulin glargine injection) for subcutaneous injection, with initial U.S. approval in 2000, the Highlights of Prescribing Information indicated to rotate injection sites to reduce the risk of lipodystrophy.
2. During a review of Resident 103’s admission Record, the admission Record indicated the facility admitted the resident on 10/30/2024, with diagnoses including type two diabetes mellitus, end stage renal disease (the final, permanent stage of chronic kidney disease, where kidney function has declined to the point that the kidneys can no longer function on their own), and metabolic encephalopathy (a condition where the brain's function is impaired due to chemical imbalances in the body, often caused by an underlying illness or organ dysfunction).
During a review of Resident 103’s MDS, dated [DATE], the MDS indicated the resident sometimes had the ability to make self-understood and sometimes had the ability to understand others and had short-term and long-term memory problem. The MDS indicated the resident was on a high-risk drug class hypoglycemic medication.
During a review of Resident 103’s Order Summary Report, dated 10/31/2024, the Order Summary Report indicated an order for:
Insulin Aspart Injection Solution 100 unit/ml (Insulin Aspart). Inject as per sliding scale: if 70 - 140 = 0 unit; 141 - 180 = 2 unit; 181 - 220 = 4 unit; 221 - 260 = 6 unit; 261 - 300 = 8 unit; 301 - 350 = 10 unit; 351 - 400 = 12-unit Call /notify MD for BS >400, subcutaneously before meals and at bedtime for DM 2 (Rotate injection site). Give eight (8) oz of orange juice for BS <70.
Insulin Glargine-yfgn Subcutaneous Solution 100 unit/ml (Insulin Glargine-yfgn). Inject 22 unit subcutaneously at bedtime for DM 2 hold for BS <100. Rotate injection site.
During a review of Resident 103’s Location of Administration Report of insulin for 5/2025 to 7/2025, the Location of Administration Report for insulin indicated:
Insulin Glargine-yfgn Subcutaneous Solution 100 unit/ml was administered on,
7/4/2025 at 9:49 p.m. on the Abdomen - RUQ
7/5/2025 at 10:45 p.m. on the Abdomen – RUQ
Insulin Aspart Injection Solution 100 unit/ml was administered on,
7/5/2025 at 11:20 a.m. on the Abdomen - LLQ
7/5/2025 at 4 p.m. on the Abdomen – LLQ
7/5/2025 at 8:06 p.m. on the Abdomen - RLQ
7/6/2025 at 7:23 a.m. on the Abdomen – RLQ
7/6/2025 at 4:09 p.m. on the Abdomen - LUQ
7/6/2025 at 8:45 p.m. on the Abdomen – LUQ
7/14/2025 at 4:55 p.m. on the Abdomen - RLQ
7/14/2025 at 9:08 p.m. on the Abdomen – RLQ
7/17/2025 at 9:34 p.m. on the Abdomen - RUQ
7/18/2025 at 7:34 a.m. on the Abdomen – RUQ
7/22/2025 at 9:41 p.m. on the Abdomen - RLQ
7/23/2025 at 7:13 a.m. on the Abdomen – RLQ
7/25/2025 at 7:27 a.m. on the Abdomen - RLQ
7/25/2025 at 11:38 a.m. on the Abdomen - RLQ
7/26/2025 at 4:03 p.m. on the Arm - left
7/26/2025 at 9:48 p.m. on the Arm – left
During a review of Resident 103’s CP Report titled “Resident is at risk for hypoglycemia and hyperglycemia related to diabetes mellitus,” last revised on 12/3/2024, the CP Report indicated an intervention to administer medications as ordered.
During a concurrent interview and record review on 7/31/2025, at 11:37 a.m., with RN 3, reviewed Resident 103’s Medical Diagnosis, Order Summary Report, Location of Administration of insulin from 5/2025 to 7/2025, and Care Plan. RN 3 stated there were multiple instances where the licensed staff did not rotate the insulin administration sites of insulin on Resident 103. RN 3 stated the sites of insulin administration should be rotated to prevent irritation, pain and discomfort on the frequented sites of administration. RN 3 also stated the sites of administration of insulin was also rotated to prevent lipodystrophy on residents. RN 3 stated injecting insulin on the sites of lipodystrophy can render the insulin ineffective due to poor absorption that can lead to hyper or hypoglycemia on Resident 103. RN 3 stated their current electronic medication administration record had a capability of checking where the last site of administration of insulin and there was no reason for the licensed staff to repeat the site of insulin administration. RN 3 stated not rotating insulin sites of administration is a medication error.
During an interview on 8/1/2025, at 2:05 p.m., with the ADON, the ADON stated licensed staff should have rotated the insulin administration sites for Resident 103 to prevent skin irritation and lipodystrophy. The ADON stated that administering insulin on the same site can cause lipodystrophy that could affect the absorption of insulin leaving them ineffective to lower the blood sugar level of Resident 103. The ADON stated not rotating insulin administration sites is considered a medication error.
During a review of the facility's recent P&P titled Insulin Administration, last reviewed on 4/24/2025, the P&P indicated to provide guidelines for the safe administration of insulin to residents with diabetes.
Steps in the Procedure (Insulin Injections via Syringe)
8. Select an injection site.
a. Insulin may be injected into the subcutaneous tissue of the upper arm, and the anterior or lateral areas of the thighs and abdomen. Avoid the area approximately 2 inches around the navel.
b. Injection sites should be rotated, preferably within the same general area (abdomen, thigh, upper arm).
During a review of the facility's recent P&P titled Adverse Consequences and Medication Errors, last reviewed on 4/24/2025, the P&P indicated a medication error is defined as the preparation or administration of drugs and biological which is not in accordance with physician's orders, manufacturer specifications, or accepted professional standards and principles of the professional(s) providing services.
During a review of the facility-provided Highlights of Prescribing Information on the use of Insulin Aspart injection, for subcutaneous or intravenous use, with initial U.S. approval in 2000, the Highlights of Prescribing Information indicated to rotate injection sites within the same region from one injection to the next to reduce risk of lipodystrophy and localized cutaneous amyloidosis.
During a review of the facility-provided Highlights of Prescribing Information on the use of Lantus (insulin glargine injection) for subcutaneous injection, with initial U.S. approval in 2000, the Highlights of Prescribing Information indicated to rotate injection sites to reduce the risk of lipodystrophy.
3. During a review of Resident 8’s admission Record, the admission Record indicated the facility originally admitted the resident on 5/4/2011 and readmitted in the facility on 5/12/2025, with diagnoses including dependence on respirator (also known as ventilator – a machine used to help a person breath when they are unable to do so on their own) status , contracture of muscle multiple sites, and DM 2.
During a review of Resident 8’s History and Physical (H&P) dated 5/13/2025, the H&P indicated Resident 8 did not have the capacity to understand and make decisions.
During a review of Resident 8’s MDS, dated [DATE], the MDS indicated Resident 8 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and was unable to understand and make her needs known. The MDS further indicated Resident 8 had impairment of both upper extremities and required total assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive). The MDS indicated Resident 8 received insulin.
During a review of Resident 8’s care plan (CP) on risk for hypoglycemia (low level of sugar in the blood) and hyperglycemia (high level of sugar in the blood) related to DM 2 initiated on 4/4/2014 and last revised on 4/16/2023, the CP indicated to administer insulin and medications as ordered as one of the interventions to prevent unrecognized signs and symptoms of hypoglycemia or hyperglycemia.
During a review of Resident 8’ Order Summary Report dated 8/1/2025, the Order Summary Report indicated the following physician’s orders:
- 5/13/2025: Lantus (also known as insulin glargine, a long-acting insulin) subcutaneous solution 100 unit per milliliter (unit/ml – a unit of measurement. Inject ten (10) units subcutaneously at bedtime for DM2. Hold for blood sugar (BS) less than (< - a unit of measurement) 100. Rotate injection site.
- 5/12/2025 and revised on 7/26/2025: Insulin aspart (a short acting insulin) flexpen subcutaneous solution pen-injector 100 unit/ml. Inject subcutaneously every six (6) hours for DM2. Rotate injection site. Inject as per sliding scale: if 70 – 149, zero (0) and may give eight (8) ounces (oz – a unit of measurement) orange juice via gastrostomy (GT - a surgical opening fitted with a device to allow feedings to be administered directly to the stomach common for people with swallowing problems) if BS < 70. Recheck BS after 15 minutes and call physician (MD); for 150 - 199 = two (2) units; 200 - 249 = three (3) units; 250 - 299 = five (5) units; 300 - 349 = seven (7) units; 350 - 400 = 10 units; for BS more than (> - a unit of measurement) 350 notify or call MD; subcutaneously every six (6) hours for DM2. Rotate injection site.
- 7/26/2025: Insulin aspart (a short acting insulin) flexpen subcutaneous solution pen-injector 100 unit/ml. Inject subcutaneously every six (6) hours for DM2. Rotate injection site. Inject as per sliding scale: if 70 – 149, 0 and may give 8 oz orange juice via GT if BS < 70. Recheck BS after 15 minutes and call MD; for 150 - 199 = 2 units; 200 - 249 = 3 units; 250 - 299 = 5 units; 300 - 349 = 7 units; 350 - 400 = 10 units; for BS more than (> - a unit of measurement) 400 call MD; subcutaneously every six (6) hours for DM2. Rotate injection site.
During a concurrent interview and record review on 7/30/2025 at 8:30 a.m. reviewed Resident 8’s physician’s orders, care plans, and location of administration sites for Lantus and insulin aspart from 6/2025 and 7/2025 with Registered Nurse (RN) 4. RN 4 stated Resident 8 had a physician’s order for Lantus and insulin aspart and were administered as follows:
- Lantus subcutaneous solution:
7/2/25 9:28 p.m. subcutaneously Abdomen – right lower quadrant (RLQ)
7/3/25 9:05 p.m. subcutaneously Abdomen – RLQ
7/5/25 8:07 p.m. subcutaneously Abdomen – left upper quadrant (LUQ)
7/6/25 8:07 p.m. subcutaneously Abdomen – LUQ
7/19/25 9:06 p.m. subcutaneously Abdomen – left lower quadrant (LLQ)
7/20/25 8:39 p.m. subcutaneously Abdomen – LLQ
- Insulin aspart flexpen subcutaneous solution:
6/6/25 12:08 a.m. subcutaneously Abdomen – left upper quadrant (LUQ)
6/6/25 5:08 a.m. subcutaneously Abdomen – LUQ
6/13/25 11:33 p.m. subcutaneously Abdomen – LLQ
6/13/25 6:28 a.m. subcutaneously Abdomen – LLQ
RN 4 stated that the administration sites for insulin should be rotated per standards of practice, manufacturer’s guidelines, and per physician’s order to prevent hardening or lumps in the skin. RN 4 stated the location of administration sites for Resident 8’s Lantus and insulin aspart were not rotated. RN 4 stated there was a physician’s order to rotate administration sites. RN 4 stated Resident 8’s administration sites should have been rotated to prevent pain, redness, irritation, and lumps on the resident’s skin which can affect the absorption of the insulin. RN 4 stated that not rotating Resident 8’s insulin administration sites can be considered a medication error by not following physician’s orders, manufacturer’s guidelines, and professional standards of care.
During an interview on 8/1/2025 at 2:05 p.m. with the Assistant Director of Nursing (ADON), the ADON stated that nurses are supposed to rotate the insulin administration sites as indicated in the physician’s order, manufacturer’s guideline, and according to professional standards of practice. The ADON stated Resident 8’s insulin administration sites should have been rotated as it placed Resident 8 at risk for development of lipodystrophy which may affect the absorption of the insulin and lead to hyperglycemia. The ADON stated that not rotating Resident 8’s insulin administration sites can be considered a medication error by not following physician’s orders, manufacturer’s guidelines, and professional standards of care.
During a review of the facility’s policy and procedure (P&P) titled “Insulin Administration,” last reviewed on 4/24/2025, the P&P indicated a purpose to provide guidelines for the safe administration of insulin to residents with diabetes. The P&P further indicated:
- Select an injection site.
a. Insulin may be injected into the subcutaneous tissue of the upper arm, and the anterior or lateral areas of the thighs and abdomen. Avoid the area approximately 2 inches around the navel.
b. Injection sites should be rotated, preferrable within the same general area (abdomen, thigh, upper arm).
- Documentation.
4. Injection site (presence or absence of any bruise, pain, redness, swelling or unusual marks on or near the injection site.
During a review of the facility’s P&P titled, “Adverse Consequences and Medication Errors,” last reviewed on 4/24/2025, the P&P indicated:
- An “adverse consequence” is defined as an unpleasant symptom or event that is due to or associated with a medication and may include adverse drug/medication reaction and side effect.
- A “medication error is defined as the preparation or administration of drugs or biological which is not in accordance with physician’s orders, manufacturer specifications, or accepted professional standards and principles of the professional(s) providing services.
- Examples of medication errors include failure to follow manufacturer instructions and/or accepted professional standards.
During a review of the facility provided manufacturer’s guideline for Insulin Aspart Injection, last revised on 2/2023, the manufacturer’s guideline indicates to rotate injection sites within the same region from one injection to the next to reduce risk of lipodystrophy and localized cutaneous amyloidosis.
During a review of the facility provided manufacturer’s guideline on insulin glargine (Lantus) last revised 5/2019, the manufacturer’s guideline indicated to rotate injection sites to reduce the risk of lipodystrophy. The manufacturer’s guideline further indicated some of the adverse reactions commonly associated with Lantus include hypoglycemia, injection site reactions, lipodystrophy, rash, and edema.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to: 1. Remove one expired admelog insulin (a medication u...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to: 1. Remove one expired admelog insulin (a medication used to control blood sugar) pen from the medication cart affecting Resident 13 in one of three inspected medication carts (Station 2 Cart.) 2. Remove one expired bottle of latanoprost eye drops (a medication used to treat eye problems) from the cart affecting Resident 85 in one of three inspected medication carts (Station 1 Cart). 3. Label an open salmeterol/fluticasone inhaler (a medication used to treat breathing problems) with an open date affecting Resident 82 in one of three inspected medication carts (Station 1 Cart). 4. Store an unopened glargine insulin (a medication used to control blood sugar) pen in the refrigerator per the manufacturer's requirements affecting Resident 81 in one of three medication carts (Sub-Acute Cart 2). The deficient practices of failing to remove expired medication from the medication carts, label open medication, and store medications per the manufacturers' requirements increased the risk that Residents 13, 81, 82, and 85 could have received medication that had become ineffective or toxic due to improper storage possibly leading to health complications resulting in hospitalization or death. Findings: During a concurrent observation and interview on [DATE] at 1:28 p.m. of Station 2 Cart with the Licensed Vocational Nurse (LVN ) 7, the following medications were found either expired, stored in a manner contrary to their respective manufacturer's requirements, or not labeled with an open date as required by their respective manufacturer's specifications: 1. One opened admelog insulin pen was found in the medication cart labeled with an open date of [DATE] According to the product labeling, admelog insulin pens should be used or discarded within 28 days of opening. During a concurrent interview, LVN 7 stated the Admelog pen for Resident 13 is only good for 28 days and since it was opened on [DATE], it is now expired. LVN 7 stated this should have been removed from the cart and replaced. LVN 7 stated because the medication is expired, it may be ineffective at controlling Resident 13's blood sugar which could lead to medical complications or hospitalization. During a concurrent observation and interview on [DATE] at 1:49 p.m. of Station 1 Cart with the Licensed Vocational Nurse (LVN ) 6, the following medications were found either expired, stored in a manner contrary to their respective manufacturer's requirements, or not labeled with an open date as required by their respective manufacturer's specifications: 1. One opened bottle of latanoprost eye drops for Resident 85 were found in the medication cart labeled with an open date of [DATE]. According to the product labeling, latanoprost eye drops should be used or discarded within 42 days of opening. 2. One opened salmeterol/fluticasone inhaler for Resident 82 was found in the medication cart with no labeled open date. According to the product labeling, salmeterol/fluticasone inhalers should be used or discarded within one month of removal from the protective foil pouch. During a concurrent interview, LVN 7 stated the latanoprost for Resident 85 opened on [DATE] is now expired. LVN 7 stated it should have been removed from the cart once it is expired so there is not a risk of giving it to the resident. LVN 7 stated because it is expired, it may not be effective at controlling Resident 85's eye condition which could lead to medical complications possibly threatening her sight. LVN 7 stated the salmeterol/fluticasone inhaler for Resident 82 is opened but not labeled with an open date. LVN 7 stated this inhaler expires one month after opening. LVN 7 stated failing to mark the inhaler with an open date increases the risk that it is used after it is expired. LVN 7 stated this may result in breathing complications including respiratory arrest leading to hospitalization or death. During a concurrent observation and interview on [DATE] at 2:25 p.m. of Sub-Acute Cart 2 with the Registered Nurse (RN ) 4, the following medications were found either expired, stored in a manner contrary to their respective manufacturer's requirements, or not labeled with an open date as required by their respective manufacturer's specifications: 1. One unopened glargine insulin pen for Resident 81 was found in the medication cart stored at room temperature. According to the product labeling, unopened glargine insulin pens should be stored in the refrigerator. During a concurrent interview, RN 4 stated she removed Resident 81's insulin glargine from the medication room this morning because it was not available in the cart. RN 4 stated she was unaware that she needed to date the medication as open once it was stored at room temperature. RN 4 stated she failed to put an open date on it since she did not yet administer it to the resident. RN 4 stated this increases the risk that the insulin could be administered to the resident after it becomes expired. RN 4 stated this may result in poor blood sugar control possibly leading to medical complications such an end-organ damage leading to hospitalization. A review of the facility's policy Medication Storage in the Facility, revised [DATE], indicated Medications and biologicals are stored safely, securely, and properly, following manufacturer's recommendations or those of the supplier. medications requiring ‘refrigeration' are kept in a refrigerator with a thermometer to allow temperature monitoring. outdated, contaminated, or deteriorated medications. are immediately removed from stock, disposed of according to procedures for medication disposal, and reordered from the pharmacy if a current order exists.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure safe and sanitary food storage and food preparation practices in the kitchen when: 1.Food items in the refrigerator we...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to ensure safe and sanitary food storage and food preparation practices in the kitchen when: 1.Food items in the refrigerator were stored without use by date for: -Applesauce -Pineapples -Grape jelly -Vanilla pudding -Cranberry sauce -Fruit cocktail 2.Resident 46's cut raw cactus in a Ziploc bag with no name, received date, use by date stored in a grocery bag with a date of 2/12/2025, was observed in the kitchen refrigerator on 7/29/2025. 3.Biscuit mix and pasta penne in dry storage with no use by date. 4.The following food items were not discarded: -Cinnamon Streusel Topping Mix with use by date of 6/12/2025. -Nilla Wafers with use by date of 7/25/2025. These deficient practices had the potential to result in harmful bacterial growth and cross contamination (transfer of harmful bacteria from one place to another) that could lead to foodborne illness (a disease caused by consuming food or drinks that are contaminated by germs or chemicals) in medically compromised residents who received food from the kitchen. Findings: During a review of Resident 42's admission Record, the admission Record indicated the facility admitted the resident on 8/9/2024 and readmitted the resident on 6/1/2025 with diagnosis that included End Stage Renal Disease (ESRD -irreversible kidney failure), difficult walking, and muscle weakness (generalized). During a review of Resident 42's History and Physical (H&P - comprehensive assessment conducted by a healthcare provider that includes gathering a thorough medical history from the resident and performing a physical examination to assess their overall health and identify any potential medical concern), dated 6/5/2025, the H&P indicated Resident 42 had the capacity to understand and make decisions. During a review of Resident 42's Minimum Data Set (MDS - a resident assessment tool), dated 6/8/2025, the MDS indicated Resident 42 had the ability to understood and understood. During a review of Resident 42's Physician Orders, dated 6/19/2025, the Physician Orders indicated renal 80 grams (g- unit of measurement) Controlled Carbohydrates (CCHO- meal plan where individuals aim to eat roughly the same amount of carbohydrates at each meal, helping to stabilize blood sugar levels) diet regular texture, thin consistency, nonfat milk with meals. During an initial observation tour of the kitchen on 7/29/2025 at 7:53 a.m. with the Dietary Supervisor (DS) of the kitchen refrigerator observed: -Applesauce dated 7/28/2025 -Grape jelly dated 7/28/2025 -Vanilla pudding dated 7/27/2025 -Cranberry sauce dated 7/22/2025 -Fruit cocktail dated 7/24/2025 -Pineapples dated 7/27/2025 The DS stated that the dates on these items are most likely the dates they were opened. The DS stated items should be dated with received date, open date, and best by date. During an observation and interview on 7/29/2025 at 8:01 a.m. of the kitchen freezer with the DS, the DS stated the cut raw cacti in a Ziploc bag inside a grocery bag with no name dated 2/12/2025, belonged to Resident 42. The DS stated the bag should be labeled with the resident's name. The DS stated he does not believe the raw cactus item was expired or has gone bad because it was placed in the freezer. During an observation and interview on 7/29/2025 at 8:10 a.m. with the DS, inside the dry storage area, the DS stated biscuit mix box had a delivery date of 6/24/2025, and an open date of 7/7/2025. The DS stated he does not think biscuit mix expires that is why there is no expiration date placed on the box. The DS reviewed the facility-provided posted Dry Good Storage Guidelines, and stated according to this guideline an opened box of biscuit expires after six months. The DS observed pasta penne with a delivery date of 6/3/2025 and open date of 6/3/2025. However, there was no expiration date placed on the pasta. The DS stated both biscuit mix box and pasta penne should have the expiration dates. During an observation and interview on 7/29/2025 at 8:14 a.m. with the DS, inside dry storage area, the DS stated the box of cinnamon streusel topping mix had a delivery date of 6/6/2025 and had an expiration date of 6/12/2025 and the Nilla wafers had a delivery date of 5/6/2025 with an open date of 5/8/2025 and expiration date of 7/25/2025. During an interview on 8/1/2025 at 8:40 a.m. with Resident 46, Resident 46 stated his niece buys the cactus for him (Resident 46) and the facility keeps and when he (Resident 46) wants it he (Resident 46) just asks for it from the kitchen staff. Resident 46 stated not sure when the raw cacti (in the Ziploc bag in the kitchen freezer) was bought. During an interview on 8/1/2025 at 8:44 a.m. with the DS, the DS stated the food that is prepared must be discarded after 72 hours and protein within 7 days. The DS stated the facility needs to put delivery date, best buy date, open date, prepared date (in the refrigerator), use by date, and item name. The DS stated food must have the use by date so staff know when the item is expired and will not use expired items because it can be a risk to use and the residents will get sick. The DS stated residents' food should be stored in the refrigerator in the activity room not in the kitchen refrigerator. The DS stated Resident 46's cactus, which is a vegetable, should not be in the refrigerator for more than six months. The DS stated that she is the one that buys Resident 46's cactus so it should be okay that she put the cactus in the freezer. The DS stated the issue is when the family brings it (cactus) in the facility. The DS stated she was not aware the family is bringing the cactus in the facility. The DS stated for resident food it must also include a resident identifier, date received and use by date. The DS stated if these are not done, the staff will not know who the item belongs to, how long the item has been in the refrigerator, and if it is expired. The DS stated there is a risk for the item (food) to be expired and the resident to get sick. During a review of the facility's policy and procedures (P&P) titled, Dating and Labeling, last reviewed on 4/24/2025, the P&P indicated to ensure food safety and prevent contamination within the facility, all food items should be properly covered, dated, and labeled in dry storage and refrigerator and freezer areas. 4. All items should be properly covered, dated, and labeled. Food items should have the following appropriate dates: a. delivery date-upon receipt b. open date-open containers c. thaw date-any frozen items 5. Expiration dates: a. dry storage area: all food products will be used in accordance with the specified Food Storage Guidelines posted in the storge area b. Refrigerator and freezer area: dietary staff to refer to Refrigerator and freezer storage chart posted outside the refrigerator 6. no food item that is expired or beyond the best buy date are in stock During an interview on 8/1/2025 at 3:23 p.m. with the Assistant Director of Nursing (ADON), the ADON stated food brought in by family and resident food should not be kept in the kitchen refrigerator. The ADON stated there is a potential for cross contamination and infection control issues. During a review of the facility's P&P titled, Outside food Resident Refrigerator and Freezer Storage, last reviewed on 4/24/2025, the P&P indicated facility will maintain one refrigerator and freezer for resident use. Items will be limited to permissible space. Raw or prepared food are not eligible. All items should be properly covered, dated, and labeled. Food items should have the following information and appropriate dates: -Resident Names -Delivery date- when received by staff, the date the product was opened and expiration date During a review of the facility's P&P titled, Dry Goods Storage Guidelines, last reviewed on 4/24/2025, the P&P indicated: -Biscuits unopened on shelf 6 months, opened on shelf 6 months -Pasta and rice mixes on shelf 6 months, opened on shelf use entire amount.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain accurate clinical records in accordance with...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain accurate clinical records in accordance with accepted professional standards and practices by failing to: 1.Ensure Registered Nurse (RN) 7 accurately documented in the change of condition/ situation, background, assessment, recommendation form (COC/SBAR - a communication tool used by healthcare workers when there is a change of condition among the residents) for one of one sampled resident (Resident 2) the physician's reply when Resident 2 had a fall incident on 6/30/2025. 2.Ensure there were no missing documentation in Resident 8's respiratory therapy electronic Medication Administration Record (eMAR) on 6/19/2025 at 9 p.m. and 7/28/2025 at 9 p.m. 3.Ensure Certified Nursing Assistant (CNA) 1 accurately documented how much Resident 97 ate on 7/25/2025 during lunch. 4.Ensure Licensed Vocational Nurse (LVN) 1 did not document Resident 97's blood pressure (BP - the pressure of circulating blood against the walls of blood vessels) on 7/25/2025 at 12 p.m. using the blood pressure reading LVN 1 obtained on 7/25/2025 at 8 a.m. 5.Ensure LVN 1 accurately documented Resident 97's crying spells on 7/25/2025 in accordance with the physician's order to monitor episodes of depression (a mental health condition that causes persistent sadness and loss of interest in activities) manifested by crying spells. On 7/25/2025, LVN 1 documented Resident 97 had 0 episode. These failures had the potential to result in confusion in the care and services rendered to the residents and resulted in incomplete and inaccurate information entered in the residents' medical record. Findings:
a. During a review of Resident 2’s admission Record (front page of the chart that contains a summary of basic information about the resident), the admission Record indicated the facility admitted the resident on 6/27/2025 with diagnoses including pneumonia (an infection/inflammation in the lungs), tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), acute embolism and thrombosis (blockage in a blood vessel) of deep veins of left lower extremity, and long term use of anticoagulants.
During a review of Resident 2’s History and Physical (H&P), dated 6/28/2025, the H&P indicated Resident 2 did not have the capacity to understand and make decisions.
During a review of Resident 2’s Minimum Data Set (MDS, a resident assessment tool), dated 7/4/2025, the MDS indicated Resident 2 had an intact cognition (mental action or process of acquiring knowledge and understanding) and was able to understand and make his needs known. The MDS further indicated Resident 2 required partial/moderate assistance from staff with all activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive).
During a review of Resident 2’s COC/SBAR form dated 6/30/2025, the COC/SBAR form indicated Resident 2 had an unwitnessed fall on 6/30/2025 while trying to reach for the bed controller and that the physician was notified on 6/30/2025 at 7 p.m. but the form did not indicate what the reply was from the physician.
During an interview on 7/31/2025 at 10:34 a.m. with RN (8), RN 8 stated documentation for any COC with residents, the nurse in charge of the resident will initiate and complete the form and document the resident’s vital signs, the situation, what time the situation started, and the interventions provided to the resident. RN 8 stated it should also be documented in the COC/SBAR form the date and time the resident’s responsible party was notified and the physician. RN 8 stated the physician’s reply should also be documented in the COC/SBAR form regardless of whether there were any new orders or none.
During a concurrent interview and review on 7/31/2025 at 10:57 a.m., reviewed Resident 2’s COC/SBAR form dated 6/30/2025, physician’s order, and the medication administration record (MAR - a daily documentation record used by a licensed nurse to document medications and treatments given to a resident) for 6/2025 with RN 7. RN 7 stated she was in charge of Resident 2 when the resident had an unwitnessed fall on 6/30/2025 and she initiated and completed the COC/SBAR form. RN 7 stated the physician visited Resident 2 on 6/30/2025 after the fall and ordered to hold Resident 2’s anticoagulant (a type of medication that prevents the blood from clotting too easily) for three days. RN 7 stated the COC/SBAR for did not indicate that an order was received from the physician. RN 7 stated the COC/SBAR should be initiated and completed by the nurse in charge of residents to include the resident’s vital signs, the situation, what time the situation started, and the interventions provided to the resident as well as family and physician notification. RN 7 stated it should be indicated in the COC/SBAR the physician’s reply regardless of whether there were any new orders or none. RN 7 stated she forgot to go back to Resident 2’s COC/SBAR form and complete it with the physician’s reply. RN 7 stated she should have completed and documented in the COC/SBAR to reflect the physician’s reply to hold Resident 2’s anticoagulant for 3 days. RN 7 stated if Resident 2’s COC/SBAR did not indicate the physician’s order, the form was inaccurate, and the staff would not be able to know if additional interventions were provided to Resident 2 to ensure his safety after a fall incident.
During a concurrent interview and record review on 7/31/2025 at 4:30 p.m., reviewed Resident 2’s COC/SBAR form dated 6/30/2025 with the Director of Nursing (DON). The DON stated Resident 2’s COC/SBAR form indicated the physician was notified on 6/30/2025 at 7 p.m. but did not indicate if there were any new orders obtained or no new orders from the physician. The DON stated whenever there is change in resident’s condition, the nurses are supposed to complete accurately the COC/SBAR form to include the situation, background, assessment of the resident to include skin assessment and vital signs, family and physician notification, and recommendation from the physician regardless of whether there is an order obtained or no new orders. The DON stated Resident 2’s COC/SBAR form should have been completed and accurate to reflect if there were any new orders obtained or no new orders from the physician. The DON stated it was important for the COC/SBAR form to be complete and accurate for all staff involved in the resident’s care to be aware that additional interventions were provided to ensure resident 2’s safety.
During a review of of the facility’s recent policy and procedure titled, “Change in a Resident’s Condition or Status,” last reviewed on 4/24/2025, the P&P indicated:
The nurse will notify the resident’s attending physician or physician on call when there has been an accident or incident involving the resident.
The nurse will record in the resident's medical record relative to changes in the resident's medical/medical condition or status.
During a review of the facility’s P&P titled, “Charting and Documentation,” last reviewed on 4/24/2025, the P&P indicated:
All services provided to the resident, progress toward the care plan goals, or any changes in the resident’s medical, physical, functional or psychosocial condition, shall be documented in the resident’s medical record.
The medical record should facilitate communication between the interdisciplinary team regarding the resident’s condition and response to care.
Documentation in the medical record will be objective (not opinionated or speculative), complete, and accurate.
b. During a review of Resident 8’s admission Record, the admission Record indicated the facility originally admitted the resident on 5/4/2011 and readmitted in the facility on 5/12/2025, with diagnoses including tracheostomy, dependence on respirator (also known as ventilator – a machine used to help a person breath when they are unable to do so on their own) status, and type 2 diabetes mellitus (DM 2 - a disorder characterized by difficulty in blood sugar control and poor wound healing).
During a review of Resident 8’s H&P, dated 5/13/2025, the H&P indicated Resident 8 did not have the capacity to understand and make decisions.
During a review of Resident 8’s MDS, dated [DATE], the MDS indicated Resident 8 had severely impaired cognition and was unable to understand and make her needs known. The MDS further indicated Resident 8 had impairment of both upper extremities and required total assistance from staff with all ADLs. The MDS indicated Resident 8 received insulin. The MDS indicated Resident 8 was on continuous oxygen therapy, scheduled suctioning, tracheostomy care, and invasive mechanical ventilator or respirator.
During a review of Resident 8’ Order Summary Report dated 8/1/2025, the Order Summary Report indicated the following physician’s orders:
5/12/2025: Suction to maintain patent airway (the breathing passage is clear and not blocked). Indicate: oral removal of saliva (Yes or No), tracheostomy tie secure (Yes or No), change of condition (Yes or No) – if yes, document in the respiratory progress note eight times per day.
During a review of Resident 8’s care plan (CP) on risk for respiratory distress initiated on 9/30/2015 and last revised on 4/16/2023, the CP indicated to suction secretions as ordered as one of the interventions to reduce episode of and symptoms of respiratory distress thru appropriate interventions.
During a review of Resident 8’s respiratory therapy eMAR for 6/2025 and 7/2025, there were no documentation indicated in the respiratory therapy eMAR for 6/19/2025 at 9 p.m. and 7/28/2025 at 9 p.m.
During a concurrent interview and record review on 7/31/2025 at 8:30 a.m., reviewed Resident 8’s physician’s orders, and respiratory therapy eMAR for 6/2025 and 7/2025 with RN 4. RN 4 stated Resident 8 had a physician’s order to suction Resident 8 to maintain a patent airway 8 times a day and to indicate oral removal of saliva, and tracheostomy tie secure. RN 4 stated there were missing documentation by the respiratory therapist (RT) on 6/19/2025 at 9 p.m. and 7/28/2025 at 9 p.m. RN 4 stated documentation in the eMAR regardless of whether it’s the licensed nurse or RT should be completed after a treatment was completed, or a medication was administered. RN 4 stated the staff are supposed to ensure that all documentation in the resident’s medical records is completed prior to leaving the facility. RN 4 stated the RT in charge of Resident 8 should have completed the documentation on Resident 8’s eMAR on 6/19/2025 and 7/28/2025 at 9 p.m. to ensure accuracy of the medical record and that all the staff involved in the resident’s care were aware that Resident 8 received the care that she need. RN 4 stated if the medical record was not complete and not accurate regarding interventions provided to Resident 8, it placed Resident 8 at risk for developing respiratory distress if not monitored accurately.
During a concurrent interview and record review on 7/31/2025 at 10:30 a.m., reviewed Resident 8’s physician’s orders, and respiratory therapy eMAR for 6/2025 and 7/2025 with Respiratory Therapist (RT) 2. RT 2 stated 8 had a physician’s order to suction Resident 8 to maintain a patent airway 8 times a day and to indicate oral removal of saliva, tracheostomy tie secure and change of condition. RT 2 stated medical records department audits the respiratory eMAR every day and gives him a list of any missed documentation in the eMAR and he will address it with the respiratory therapist (RT) in charge of the residents. RT 2 stated there were missing documentation by the RT on 6/19/2025 at 9 p.m. and 7/28/2025 at 9 p.m. RT 2 stated documentation in the respiratory therapy eMAR should be completed as a treatment was completed. RT 2 stated the staff are supposed to ensure that all documentation in the resident’s medical records is completed prior to leaving the facility. RT 2 stated the RT in charge of Resident 8 should have completed the documentation on Resident 8’s eMAR on 6/19/2025 and 7/28/2025 at 9 p.m. to ensure accuracy of the medical record and that all the staff involved in the resident’s care were aware that Resident 8 received the care. RT 2 stated if the medical record was not complete and accurate regarding interventions provided to Resident 8, it placed Resident 8 at risk for developing respiratory distress if not monitored accurately.
During an interview on 7/31/2025 at 4:30 p.m., with the DON, the DON stated the staff are supposed to ensure that all documentation should be completed in the eMAR regardless of whether it’s the licensed nurse or RT after a treatment was completed, or a medication was administered prior to leaving the facility. The DON stated the RT in charge of Resident 8 should have completed the documentation on Resident 8’s eMAR on 6/19/2025 and 7/28/2025 at 9 p.m. to ensure accuracy of the medical record and that all the staff involved in the resident’s care were aware that Resident 8 received the care that she needed. The DON stated if the medical record was not complete and accurate regarding the interventions provided to Resident 8, it placed Resident 8 at risk for developing respiratory distress if not monitored accurately.
During a review of the facility’s policy and procedures titled, “Charting and Documentation,” last reviewed on 4/24/2025, the P&P indicated:
All services provided to the resident, progress toward the care plan goals, or any changes in the resident’s medical, physical, functional or psychosocial condition, shall be documented in the resident’s medical record.
The medical record should facilitate communication between the interdisciplinary team regarding the resident’s condition and response to care.
Documentation in the medical record will be objective (not opinionated or speculative), complete, and accurate.
c. During a review of Resident 97 admission Record, the admission Record indicated the facility admitted Resident 97 on 4/3/2024 and readmitted the resident on 5/10/2024 with diagnoses included aphasia, dysphagia (difficulty swallowing), history of falling, anxiety (a feeling of unease, worry, or fear), and depression (a mental health condition that makes you feel persistently sad and lose interest in things you usually enjoy).
During a review of Resident 97’s care plan for aspiration, initiated on 5/16/2024 and revised on 3/12/2025, the care plan indicated Resident 97 is at risk for aspiration of food and liquids secondary to dysphagia. The care plan interventions included monitor for sign and symptoms of aspiration (chocking, shortness of breath [SOB], respiration changes, and to monitor tolerance of diet and fluids.
During a review of Resident 97’s care plan for self-care deficits, initiated on 7/29/2024, the care plan indicated Resident 97 needing total assistance with eating. The care plan intervention indicated to provide safe environment.
During a review of Resident 97’s Physician Orders, dated 10/29/2024, the Physician Orders indicated monitor episode of depression manifested by crying spells and tally by hashmarks for Zoloft every shift.
During a review of Resident 97’s Speech Therapy Discharge summary dated [DATE], the Speech Therapy Discharge Summary indicated Resident 97 will tolerate minced and moist nectar thick liquids three (3) meals a day with aspiration precautions, on 12/3/2024 Resident was severe risk for aspiration.
During a review of Resident 97’s care plan for altered behavior patterns related to depression, initiated on 1/2/2025 and revised on 3/12/2025, the care plan indicated Resident 97 had depression manifested by crying spells and inability to sleep. The care plan interventions included assessing what may cause behavior and what may trigger behavior, attempt to reduce and eliminate those triggers if possible.
During a review of Resident 97’s Physician Orders, dated 1/29/2025, the Physician Orders indicated Zoloft oral tablet 50 milligrams (mg- a unit of measurement) give one tablet by mouth one time a day for depression manifested by crying spells.
During a review of Resident 97’s MDS, dated [DATE], the MDS indicated Resident 97 sometimes understood and was sometimes able to be understood. The MDS indicated Resident 97 coughed and choked during meals or when swallowing medications.
During a review of Resident 97’s H&P, dated 5/22/2025, the H&P indicated Resident 97 did not have the capacity to understand and make decisions.
During a review of Resident 97’s Physician Orders, dated 5/30/2025, the Physician Orders indicated to monitor blood pressure every six hours.
During a review of Resident 97’s Physician Orders, dated 7/9/2025, the Physician Orders indicated Controlled Carbohydrates (CCHO- meal plan where individuals aim to eat roughly the same amount of carbohydrates at each meal, helping to stabilize blood sugar levels) no added salt (NAS) diet, dysphagia mechanical soft texture, nectar mild thick consistency, 3 meals, aspiration (breathing in foreign material like food into the lungs) precautions, supervision during meals.
During a review of Resident 97’s task on ADL eating, the task on ADL eating for 7/25/2025 at 12:07 p.m. indicated Resident 97 was provided with setup or clean up assistance (helper sets up or cleans up resident completes activity helper assists only prior or following the activity).
During a review of Resident 97’s task nutritional amount eaten (percent [%)] - one part in a hundred), the task nutritional amount eaten (%) for 7/25/2025 at 12:07 p.m. indicated Resident 97 ate 50% of his (Resident 97) meal.
During a concurrent interview and record review on 7/30/2025 at 11:48 a.m. of Resident 97’s nutritional amount eaten (%) was reviewed with CNA 1. CNA 1 stated for Resident 97, she (CNA 1) sets up the tray and leaves Resident 97’s tray at the bedside table. CNA 1 stated she worked on 7/25/2025 and Resident 97 was her resident that day. CNA 1 stated she went to pick up the lunch tray sometime after 1 p.m. and noted nothing had been eaten. CNA 1 reviewed Resident 97’s nutritional amount eaten (%) and stated she (CNA 1) was the one who documented Resident 97’s food eaten on 7/25/2025. CNA 1 stated Resident 97 did not eat because food was not touched, but she (CNA 1) documented in Resident 97’s record that Resident 97 ate 50%.
During a concurrent interview and record review on 7/30/2025 at 1:29 p.m. of Resident 97’s MAR with LVN 1, LVN 1 stated he was the nurse for Resident 97 on 7/25/2025 for 7 a.m. to 3 p.m. LVN 1 stated Resident 97 does cry and gestures he wants to go home by clinging onto his family members when they show up. LVN 1 reviewed Resident 97’s MAR and stated the blood pressure documented for 12 p.m. was taken from the 8 a.m. blood pressure reading he (LVN 1) took from Resident 97. LVN 1 stated he did not take the blood pressure as ordered every six hours. LVN 1 stated if blood pressure is not checked, staff will not know if Resident 97’s blood pressure is high or low which can result in a delay in the interventions.
During an interview on 7/31/2025 at 8:34 a.m. with CNA 1, CNA 1 stated Resident 97 has depression and on some days he just cries. CNA 1 stated Resident 97 was crying for like three days (dates not indicated). CNA1 stated she would ask Resident 97 if he wanted to see his sister and Resident 97 would nod yes. CNA 1 stated Resident 97 would cry when he would see staff or any person. CNA 1 stated Resident 97 would cry for about 10 minutes and would nod yes when asked if he was sad. CNA1 stated would tell RNs and LVN 1 that Resident 97 would be crying and they would go and see Resident 97. CNA 1 stated she usually documents breakfast around 11 a.m. and lunch at 2 p.m. but on that day she documented Resident 97’s lunch at 12:07p.m. because she wanted to get her documentation done even if Resident 97 had not eaten his lunch. CNA1 stated she had not checked Resident 97’s tray at that time so her documentation that Resident 97 ate 50% of his lunch was inaccurate because she did not look at the tray and Resident 97 had not even eaten. CNA 1 stated she was just trying to catch up on her documentation. CNA 1 stated yes it was on purpose because she already anticipated since Resident 97 usually eats 30 to 50%.
During an interview on 7/31/2025 at 12:19 p.m. with the DON, the DON stated Resident 97 had an order for BP checks every six hours. The DON stated LVN 1 entered a blood pressure reading at 12:54 p.m. for Resident 97. The DON stated at that time Resident 97 was already gone from the facility. The DON stated it was inaccurate documentation. The DON stated if LVN 1 said the blood pressure reading was taken from 8 a.m. and used that BP reading for LVN 1’s documentation at 12:54 p.m., then it is not accurate because LVN 1 should be getting the BP as ordered every 6 hours because Resident 97’s blood pressure can elevate. The DON stated CNA 1 should have documented the amount eaten after checking Resident 97’s tray. The DON stated had CNA 1 checked Resident 97’s tray, CNA 1 would have noted that Resident 97’s food was not eaten and that Resident 97 was already not in the facility. The DON stated it is inaccurate documentation. The DON stated Resident 97 was crying all day on 7/25/2025. The DON, after reviewing Resident 97’s MAR for crying spells, stated that “0” spells of crying is inaccurate documentation.
During an interview on 8/1/2025 at 12:39 p.m. with LVN 1, LVN 1 stated Resident 97 had an order to take blood pressure every six hours. LVN 1 stated he did not take Resident 97’s BP for the 12 p.m. scheduled time instead he used the 8 a.m. BP reading he (LVN 1) took from Resident 97.
During a review of the facility’s policy and P&P titled, “Charting and Documentation,” last reviewed on 4/24/2025, the P&P indicated documentation in the medical record will be objective, complete and accurate.
During a review of the facility’s policy and P&P titled, “Administering Medication,” last reviewed on 4/24/2025, the P&P indicated Medications are administered in a safe and timely manner and as prescribed.
1.Medications are administered in accordance with prescriber orders, including any required time frames.
10. The following information is checked and verified for each resident prior to administering medications:
b. vital signs, if necessary
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0847
(Tag F0847)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the binding arbitration agreement (a resident waives the rig...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the binding arbitration agreement (a resident waives the right to sue the nursing home in court, and instead agrees to have any future disputes handled by a private arbitrator) indicated the resident or anyone else (e.g., resident's representative) were allowed to communicate with federal, state, or local officials such as federal and state surveyors, other federal or state health department employees and representative of the Office of the State Long Term Care Ombudsman for three of three sampled residents (Residents 23, 33, and 51) reviewed for Arbitration Facility Task. This deficient practice had the potential for residents to be unaware of their rights pertaining to Arbitration Agreement. Cross reference F848 Findings: 1.During a review of Resident 23's admission Record, the admission Record indicated the facility admitted the resident on 12/27/2024, with diagnoses including cerebral infarction (occurs as a result of disrupted blood flow to the brain due to problems with the blood vessels that supply it), depression (a low mood or loss of pleasure or interest in activities for long periods of time), and anxiety disorder (a group of mental health conditions characterized by excessive and persistent worry, fear, and nervousness about everyday situations). During a review of Resident 23's History and Physical (H&P), dated 12/27/2024, the H&P indicated the resident had the capacity to understand and make decisions. During a review of Resident 23's Minimum Data Set (MDS, a resident assessment tool), dated 7/6/2025, the MDS indicated the resident had the ability to make self-understood and understand others and had intact cognition (a participant who has sufficient judgment, planning, organization, self-control, and the persistence needed to manage the normal demands of the participant's environment). The MDS indicated that the resident and the family participated in the assessment and goal setting of resident's healthcare management. During a concurrent interview and record review on 8/1/2025, at 8:53 a.m., with the admission Coordinator (AC), reviewed Resident 23's Arbitration Agreement signed by the resident on 12/27/2024. The AC stated that she cannot find the verbiage The arbitration agreement does not contain any language that prohibits or discourages the resident or anyone else from communicating with federal, state or local officials. Residents are never discouraged (verbally, in writing, or otherwise) from communicating with federal, state, or local officials (including federal and state surveyors, state health department employees, or representatives from the Office of the State Long-Term Care Ombudsman on the contract signed by Resident 23. The AC stated it was important to have the above information in the resident's arbitration agreement to ensure they are well aware of their rights when signing an arbitration agreement. During an interview on 8/1/2025, at 2:05 p.m., with the Assistant Director of Nursing (ADON), the ADON stated the contract should include the information The arbitration agreement does not contain any language that prohibits or discourages the resident or anyone else from communicating with federal, state or local officials. Residents are never discouraged (verbally, in writing, or otherwise) from communicating with federal, state, or local officials (including federal and state surveyors, state health department employees, or representatives from the Office of the State Long-Term Care Ombudsman, to ensure Resident 23 is properly informed and they are not violating the resident's right to information. The ADON stated it is important that the arbitration agreement contains all the required information set forth by the federal agency because it can affect the resident or representative's decision making when entering into a binding agreement. During a review of the facility's recent policy and procedure (P&P) titled Binding Arbitration Agreements, last reviewed on 4/24/2025, the P&P Indicated: Policy Interpretation and Implementation 10. The arbitration agreement does not contain any language that prohibits or discourages the resident or anyone else from communicating with federal, state or local officials. Residents are never discouraged (verbally, in writing, or otherwise) from communicating with federal, state, or local officials (including federal and state surveyors, state health department employees, or representatives from the Office of the State Long-Term Care Ombudsman. 2.During a review of Resident 33's admission Record, the admission Record indicated the facility admitted the resident on 6/28/2024, with diagnoses including psychosis (a mental health condition where someone loses touch with reality), generalized anxiety disorder (a mental health disorder that produces fear, worry, and a constant feeling of being overwhelmed), and need for assistance with personal care. During a review of Resident 33's H&P, dated 7/2/2025, the H&P indicated the resident had the capacity to understand and make decisions. During a review of Resident 33's MDS, dated [DATE], the MDS indicated the resident had the ability to make self-understood and understand others and had intact cognition. The MDS indicated that the resident and the family participated in the assessment and goal setting of resident's healthcare management. During a concurrent interview and record review on 8/1/2025, at 8:53 a.m., with the AC, reviewed Resident 33's Arbitration Agreement signed by the resident on 6/28/2024. The AC stated that she cannot find the verbiage The arbitration agreement does not contain any language that prohibits or discourages the resident or anyone else from communicating with federal, state or local officials. Residents are never discouraged (verbally, in writing, or otherwise) from communicating with federal, state, or local officials (including federal and state surveyors, state health department employees, or representatives from the Office of the State Long-Term Care Ombudsman on the contract signed by Resident 33. The AC stated it was important to have the above information in the resident's arbitration agreement to ensure they are well aware of their rights when signing an arbitration agreement. During an interview on 8/1/2025, at 2:05 p.m., with the ADON, the ADON stated the contract should include the information The arbitration agreement does not contain any language that prohibits or discourages the resident or anyone else from communicating with federal, state or local officials. Residents are never discouraged (verbally, in writing, or otherwise) from communicating with federal, state, or local officials (including federal and state surveyors, state health department employees, or representatives from the Office of the State Long-Term Care Ombudsman, to ensure Resident 33 is properly informed and they are not violating the resident's right to information. The ADON stated it is important that the arbitration agreement contains all the required information set forth by the federal agency because it can affect the resident or representative's decision making when entering into a binding agreement. During a review of the facility's recent P&P titled Binding Arbitration Agreements, last reviewed on 4/24/2025, the P&P Indicated: Policy Interpretation and Implementation 10. The arbitration agreement does not contain any language that prohibits or discourages the resident or anyone else from communicating with federal, state or local officials. Residents are never discouraged (verbally, in writing, or otherwise) from communicating with federal, state, or local officials (including federal and state surveyors, state health department employees, or representatives from the Office of the State Long-Term Care Ombudsman. 3.During a review of Resident 51's admission Record, the admission Record indicated the facility admitted the resident on 12/14/2024, and readmitted the resident on 4/12/2025, with diagnoses including visual loss, right eye, and need for assistance with personal care. During a review of Resident 51's MDS, dated [DATE], the MDS indicated the resident had the ability to make self-understood and understand others and had intact cognition. The MDS indicated that the resident and the family participated in the assessment and goal setting of resident's healthcare management. During a concurrent interview and record review on 8/1/2025, at 8:53 a.m., with the AC, reviewed Resident 51's Arbitration Agreement signed by the resident on 12/14/2024. The AC stated that she cannot find the verbiage The arbitration agreement does not contain any language that prohibits or discourages the resident or anyone else from communicating with federal, state or local officials. Residents are never discouraged (verbally, in writing, or otherwise) from communicating with federal, state, or local officials (including federal and state surveyors, state health department employees, or representatives from the Office of the State Long-Term Care Ombudsman on the contract signed by Resident 51. The AC stated it was important to have the above information in the resident's arbitration agreement to ensure they are well aware of their rights when signing an arbitration agreement. During an interview on 8/1/2025, at 2:05 p.m., with the ADON, the ADON stated the contract should include the information The arbitration agreement does not contain any language that prohibits or discourages the resident or anyone else from communicating with federal, state or local officials. Residents are never discouraged (verbally, in writing, or otherwise) from communicating with federal, state, or local officials (including federal and state surveyors, state health department employees, or representatives from the Office of the State Long-Term Care Ombudsman, to ensure Resident 51 is properly informed and they are not violating the resident's right to information. The ADON stated it is important that the arbitration agreement contains all the required information set forth by the federal agency because it can affect the resident or representative's decision making when entering into a binding agreement. During a review of the facility's recent P&P titled Binding Arbitration Agreements, last reviewed on 4/24/2025, the P&P Indicated: Policy Interpretation and Implementation 10. The arbitration agreement does not contain any language that prohibits or discourages the resident or anyone else from communicating with federal, state or local officials. Residents are never discouraged (verbally, in writing, or otherwise) from communicating with federal, state, or local officials (including federal and state surveyors, state health department employees, or representatives from the Office of the State Long-Term Care Ombudsman.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0848
(Tag F0848)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the binding arbitration agreement (a resident waives the rig...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the binding arbitration agreement (a resident waives the right to sue the nursing home in court, and instead agrees to have any future disputes handled by a private arbitrator) indicated the selection of a neutral arbitrator agreed upon by both parties; and the selection of a venue that is convenient to both parties for three of three sampled residents (Residents 23, 33, and 51) reviewed for Arbitration Facility Task. This deficient practice had the potential for residents to be unaware of their rights pertaining to Arbitration Agreement. Cross reference F847 Findings: 1.During a review of Resident 23's admission Record, the admission Record indicated the facility admitted the resident on 12/27/2024, with diagnoses including cerebral infarction (occurs as a result of disrupted blood flow to the brain due to problems with the blood vessels that supply it), depression (a low mood or loss of pleasure or interest in activities for long periods of time), and anxiety disorder (a group of mental health conditions characterized by excessive and persistent worry, fear, and nervousness about everyday situations). During a review of Resident 23's History and Physical (H&P), dated 12/27/2024, the H&P indicated the resident had the capacity to understand and make decisions. During a review of Resident 23's MDS, dated [DATE], the Minimum Data Set (MDS, a resident assessment tool) indicated the resident had the ability to make self understood and understand others and had intact cognition (a participant who has sufficient judgment, planning, organization, self-control, and the persistence needed to manage the normal demands of the participant's environment). The MDS indicated that the resident and the family participated in the assessment and goal setting of resident's healthcare management. During a concurrent interview and record review on 8/1/2025, at 8:53 a.m., with the Admission's Coordinator (AC), reviewed Resident 23's Arbitration Agreement signed by the resident on 12/27/2024. The AC stated that she cannot find the verbiage the selection of a neutral arbitrator agreed upon by both parties; and the selection of a venue that is convenient to both parties on the contract signed by Resident 23. The AC stated it was important to have the above information in the resident's arbitration agreement to ensure they are well aware of their rights when signing an arbitration agreement. During an interview on 8/1/2025, at 2:05 p.m., with the Assistant Director of Nursing (ADON), the ADON stated the contract should include the information the selection of a neutral arbitrator agreed upon by both parties; and the selection of a venue that is convenient to both parties, to ensure Resident 23 is properly informed and they are not violating the resident's right to information. The ADON stated it is important that the arbitration agreement contains all the required information set forth by the federal agency because it can affect the resident or representative's decision making when entering into a binding agreement. During a review of the facility's recent policy and procedure (P&P) titled Binding Arbitration Agreements, last reviewed on 4/24/2025, the P&P Indicated: Arbitrator/Venue Selection 1. Arbitration agreements provide for the selection of a neutral Arbitrator, which is agreed upon by both parties. A neutral arbitrator is an impartial, unbiased, third-party decision maker, without the appearance of any conflicts of interest, contracted with and agreed to by both parties to resolve their dispute. 4. Residents (or representatives) are given the opportunity to suggest an arbitrator and a venue. If the facility disagrees with the resident's suggested arbitrator(s) and/or venue, the facility will document the reason and provide that documentation to the resident (or representative). 2.During a review of Resident 33's admission Record, the admission Record indicated the facility admitted the resident on 6/28/2024, with diagnoses including psychosis (a mental health condition where someone loses touch with reality), generalized anxiety disorder (a mental health disorder that produces fear, worry, and a constant feeling of being overwhelmed), and need for assistance with personal care. During a review of Resident 33's H&P, dated 7/2/2025, the H&P indicated the resident had the capacity to understand and make decisions. During a review of Resident 33's MDS, dated [DATE], the MDS indicated the resident had the ability to make self-understood and understand others and had intact cognition. The MDS indicated that the resident and the family participated in the assessment and goal setting of resident's healthcare management. During a concurrent interview and record review on 8/1/2025, at 8:53 a.m., with the AC, reviewed Resident 33's Arbitration Agreement signed by the resident on 6/28/2024. The AC stated that she cannot find the verbiage the selection of a neutral arbitrator agreed upon by both parties; and the selection of a venue that is convenient to both parties on the contract signed by Resident 33. The AC stated it was important to have the above information in the resident's arbitration agreement to ensure they are well aware of their rights when signing an arbitration agreement. During an interview on 8/1/2025, at 2:05 p.m., with the ADON, the ADON stated the contract should include the information the selection of a neutral arbitrator agreed upon by both parties; and the selection of a venue that is convenient to both parties, to ensure Resident 33 is properly informed and they are not violating the resident's right to information. The ADON stated it is important that the arbitration agreement contains all the required information set forth by the federal agency because it can affect the resident or representative's decision making when entering into a binding agreement. During a review of the facility's recent P&P titled Binding Arbitration Agreements, last reviewed on 4/24/2025, the P&P Indicated: Arbitrator/Venue Selection 1. Arbitration agreements provide for the selection of a neutral Arbitrator, which is agreed upon by both parties. A neutral arbitrator is an impartial, unbiased, third-party decision maker, without the appearance of any conflicts of interest, contracted with and agreed to by both parties to resolve their dispute. 4. Residents (or representatives) are given the opportunity to suggest an arbitrator and a venue. If the facility disagrees with the resident's suggested arbitrator(s) and/or venue, the facility will document the reason and provide that documentation to the resident (or representative). 3.During a review of Resident 51's admission Record, the admission Record indicated the facility admitted the resident on 12/14/2024, and readmitted the resident on 4/12/2025, with diagnoses including visual loss, right eye, and need for assistance with personal care. During a review of Resident 51's MDS, dated [DATE], the MDS indicated the resident had the ability to make self-understood and understand others and had intact cognition. The MDS indicated that the resident and the family participated in the assessment and goal setting of resident's healthcare management. During a concurrent interview and record review on 8/1/2025, at 8:53 a.m., with the AC, reviewed Resident 51's Arbitration Agreement signed by the resident on 12/14/2024. The AC stated that she cannot find the verbiage the selection of a neutral arbitrator agreed upon by both parties; and the selection of a venue that is convenient to both parties on the contract signed by Resident 51. The AC stated it was important to have the above information in the resident's arbitration agreement to ensure they are well aware of their rights when signing an arbitration agreement. During an interview on 8/1/2025, at 2:05 p.m., with the ADON, the ADON stated the contract should include the information the selection of a neutral arbitrator agreed upon by both parties; and the selection of a venue that is convenient to both parties, to ensure Resident 51 is properly informed and they are not violating the resident's right to information. The ADON stated it is important that the arbitration agreement contains all the required information set forth by the federal agency because it can affect the resident or representative's decision making when entering into a binding agreement. During a review of the facility's recent P&P titled Binding Arbitration Agreements, last reviewed on 4/24/2025, the P&P Indicated: Arbitrator/Venue Selection 1. Arbitration agreements provide for the selection of a neutral Arbitrator, which is agreed upon by both parties. A neutral arbitrator is an impartial, unbiased, third-party decision maker, without the appearance of any conflicts of interest, contracted with and agreed to by both parties to resolve their dispute. 4. Residents (or representatives) are given the opportunity to suggest an arbitrator and a venue. If the facility disagrees with the resident's suggested arbitrator(s) and/or venue, the facility will document the reason and provide that documentation to the resident (or representative).
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement appropriate infection control practices by ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement appropriate infection control practices by failing to: 1. Ensure cleanliness of one of two shower rooms (Station 1) was maintained. 2. Ensure the door seal gaskets of two of three dryer tumblers (dryer 1 and dryer 2) were not torn and not covered with tape. 3. Ensure Licensed Vocational Nurse (LVN) 2 implemented Contact Precautions (an infection control measure aimed to prevent spread of infection by direct or indirect contact by the use of personal protective equipment [PPE - clothing and equipment that is worn or used to provide protection against hazardous substances and/or environments]) for one of seven sampled residents (Resident 26) reviewed under the Infection Control task area. 4. Ensure the trash container in the bathroom was clean and free from brown dirt and stains with a yellow substance on the lid for two of seven sampled residents (Resident 1 and 36) reviewed under the Environment task area. 5. Ensure LVN 3 donned (put on) gown while repositioning one of one sampled resident (Resident 12) in bed who was on Enhanced Barrier Precautions (EBP - extra steps taken to prevent the spread of germs in nursing homes, especially for residents at higher risk). These deficient practices had the potential to spread infections and illnesses to other residents, visitors, and staff. Findings:
a.During an interview on 7/30/2025 at 9:03 a.m. with Resident 82, Resident 82 stated the shower room right outside his room had feces in the shower room. Resident 82 stated this happened a week or two ago and the staff did not clean the shower room. Resident 82 stated he does not want to get sick and get infection from it.
During a concurrent observation and interview on 7/30/2025 at 4:28 p.m. with the Maintenance Supervisor (MS), inside the Station 1 Shower Room, the MS stated there are wound dressings on the shower floor and one band-aid behind the shower curtain. The MS stated those should not be there.
During an interview on 8/1/2025 at 12:21 p.m. with the Housekeeping Director (HSKD), the HSKD stated shower rooms are cleaned every day and visually check the shower rooms every two hours and clean what needs to be cleaned up. The HSKD stated when the shower rooms are not cleaned this would be risk for contamination for the residents.
During an interview on 8/1/2025 at 3:20 p.m. with the Assistant Director of Nursing (ADON), the ADON stated when the shower rooms are not kept clean there is a potential for infection to spread among residents.
During a review of the facility’s policy and procedures (P&P) titled, “Cleaning Restrooms, Bathrooms, and Showers,” dated 4/24/2025, the P&P indicated to “clean and dry tile, bathtubs, and showers.” The P&P indicated to “sweep and mop floor, making sure all floor drains and area around them are clean”.
b. During a concurrent observation and interview on 7/31/2025 at 3:27 p.m. with Laundry Staff (LS) 1, in the laundry room, LS 1 stated they have three dryers and three washers. LS 1 stated dryer 1 and dryer 2 has a broken seal gasket. LS 1 stated the gasket has been torn for a while. LS 1 stated this is not good because when the dryer runs the hot air leaks out and it will take longer to dry the clothes. LS 1 stated the dryer temperature would also not be reached at the set temperature.
During an interview on 8/1/2025 at 12:26 p.m. with the HSKD, the HSKD stated the laundry staff checks the dryer and washer and a company outsourced by the facility maintains the equipment. The HSKD stated when the LS finds issue with the dryer or washer, they let him know. The HSKD stated he also checks the laundry area daily, and he was not made aware of the dryer seal gasket issue until yesterday, 7/31/2025. The HSKD stated no one reported to him prior to 7/31/2025. The HSKD stated he found out that two of the three dryers had broken seal gaskets and had taped placed on them. The HSKD stated he does not know who placed the tape and he did not notice it when he does his daily check. The HSKD stated the dryers would not heat sufficiently and would not be able to maintain the heat in the dryer. The HSKD stated it would take longer for the clothes to dry.
During an interview on 8/1/2025 at 3:20 p.m. with the Assistant Director of Nursing (ADON), the ADON stated that when the dryer is not maintained properly it would not dry the clothes properly and could possibly cause molding, which could be a hazard.
During a review of the facility’s P&P regarding Interior General Maintenance, dated 4/24/2025, the P&P indicated to “make sure all belts, parts, bolts, etc. are properly secured and are correctly balanced.”
During a review of the facility’s P&P titled, “Infection Control-Multidrug Resistant Organism (MDRO- microorganisms, mainly bacteria, that are resistant to one or more classes of antibiotics),” dated 4/24/2025, the P&P indicated environmental and equipment protection included the disinfection of soiled surfaces and equipment daily or more frequently by the designated staff member and should be done in order to prevent the spread of MDRO and other pathogenic organisms. The P&P indicated that “contaminated linens should be handled appropriately whether their source was an isolation room or a non-isolation room. All line should be handled as if it were highly infectious.”
c. During a review of Resident 26’s admission Record (AR), the AR indicated the facility admitted the resident on 11/2/2023 and most recently readmitted the resident on 1/22/2025 with diagnoses that included chronic respiratory failure (a serious condition that occurs suddenly when the lungs cannot get enough oxygen), tracheostomy (opening surgically created through the front of the neck and into the trachea [windpipe]), dependence on respiratory ventilator (a medical device to help support or replace breathing), unspecified coma (a state of prolonged loss of consciousness), resistance to carbapenem (a subclass of antibiotics [medication used to treat bacterial infections), and gastrostomy (GT - a tube placed directly into the stomach to give direct access for supplemental feeding, hydration or medicine) placement.
During a review of Resident 26’s Minimum Data Set (MDS – resident assessment tool) dated 5/26/2025, the MDS indicated the resident was in a persistent vegetative state (a person is awake but shows no signs of awareness) with no discernible consciousness (awareness of internal and external existence). The MDS indicated the resident was totally dependent on staff for mobility, dressing, bathing, toilet hygiene, and personal hygiene.
During a review of Resident 26’s Care Plan (CP) titled regarding multidrug-resistant organism [MDRO, microorganisms, mainly bacteria, that are resistant to one or more classes of antibiotics] infection and resident needs contact isolation, initiated 7/18/2024 and last revised on 2/14/2025, the CP indicated a goal that the resident would minimize risk of transmitting infection through appropriate interventions.
During a review of Resident 26’s Order Summary Report, the Order Summary Report indicated a physician’s order for contact isolation for Carbapenem-resistant pseudomonas aeruginosa (CRPA – an infectious bacteria spread through contact with contaminated surfaces, healthcare workers, or equipment), dated 5/31/2025.
During an observation on 7/29/2025 at 12:07 p.m., observed LVN 2 inside Resident 26’s shared room. Observed a contact isolation sign place on the wall at the room entrance indicating to don (put on) a gown and gloves prior to entering the room. Observed LVN 2 was not wearing a gown or gloves inside Resident 26’s shared room. Observed LVN 2 prepared Resident 26’s enteral tube feeding (TF, a form of nutrition that is delivered into the digestive system as a liquid) and connected the TF to the pump (a device used to deliver a TF via the GT at a set rate). LVN 2 did not connect the TF to Resident 26. LVN 2 then exited Resident 26’s shared room.
During a concurrent interview and record review on 7/29/2025 at 12:13 p.m. with LVN 2, LVN 2 stated LVN 2 did not need to wear a gown or gloves while setting up Resident 26’s TF pump. LVN 2 stated that when LVN 2 is just preparing Resident 26’s TF at the pump, LVN 2 does not need to wear a gown or gloves in the resident’s room. LVN 2 then reviewed the contact isolation sign at the entrance to Resident 26’s room. LVN 2 stated the sign indicated to don a gown when entering the room. LVN 2 stated LVN 2 could be wrong about when to use a gown and gloves in a contact isolation room.
During an interview and record review on 7/29/2025 at 12:45 p.m. with LVN 3 reviewed Resident 26’s physician orders and care plans. LVN 3 stated for any resident in a contact isolation room, the staff should don a gown and gloves prior to entering the resident’s room to protect the residents from the transfer of any microbes between staff or residents. LVN 3 stated Resident 26 is on contact isolation and is a high risk for infection. LVN 3 stated even if LVN 2 was touching only the TF and pump, LVN 2 should have donned a gown and gloves prior to entering Resident 26’s room.
During a concurrent interview and record review on 8/1/2025 at 8:34 a.m. with the Infection Preventionist (IP), the IP reviewed the facility policy and procedure regarding Infection Prevention. The IP stated any resident colonized with CRPA is on contact isolation. The IP stated the facility process for contact isolation is to place a contact isolation sign outside the entrance to the resident’s room and anyone entering the room should wear a gown and gloves. The IP stated the gown and gloves are a barrier to prevent cross contamination (the process by which bacteria or other microorganisms are unintentionally transferred from one substance or object to another, with harmful effect) between the resident, surrounding environment, and the nurse’s clothing. The IP stated LVN 2 did not follow the facility P&P when LVN 2 did not don a gown and gloves in Resident 26’s contact isolation room potentially resulting in exposing immunocompromised (a weakened immune system, making it harder for the body to fight off infections and diseases) residents with multiple comorbidities (medical conditions that coexist alongside a primary diagnosis) to MDROs.
During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the ADON, the ADON reviewed the facility P&P regarding infection control. The ADON stated the facility staff have had so many in-services about contact isolation. The ADON stated LVN 2 did not follow the P&P when LVN 2 did not don a gown and gloves in Resident 26’s room potentially resulting in risk for infection in residents.
During a review of the facility P&P titled, “Isolation – Categories of Transmission-Based Precautions (a set of infection control practices used in healthcare settings to prevent the spread of infectious diseases),” last reviewed 4/24/2025, the P&P indicated transmission-based precautions are initiated when a resident develops signs and symptoms of a transmissible infection; arrives for admission with symptoms of an infection; or has a laboratory confirmed infection; and is at risk of transmitting the infection to other residents. Standard precautions are used when caring for residents at all times regardless of their suspected or confirmed infection status. Transmission-based precautions are additional measures that protect staff, visitors and other residents from becoming infected. These measures are determined by the specific pathogen and how it is spread from person to person. When a resident is placed on transmission-based precautions, appropriate notification is placed on the room entrance door so that personnel and visitors are aware of the need for and the type of precaution. The signage informs the staff of the type of precaution(s), instructions for use of PPE, and/or instructions to see a nurse before entering the room. Contact precautions are implemented for residents known or suspected to be infected with microorganisms that can be transmitted by direct contact with the resident or indirect contact with environmental surfaces or resident-care items in the resident's environment. Staff and visitors wear gloves (clean, non-sterile) when entering the room. Staff and visitors wear a disposable gown upon entering the room and remove before leaving the room and avoid touching potentially contaminated surfaces with clothing after gown is removed.
d.1. During a review of Resident 1’s AR, the AR indicated the facility admitted the resident on 5/12/2022 and most recently readmitted the resident on 2/15/2025 with diagnoses that included acute and chronic respiratory failure, tracheostomy, dependence on respiratory ventilator, muscle weakness, and need for assistance with personal care.
During a review of Resident 1’s MDS, dated [DATE], the MDS indicated the resident was totally dependent on staff for mobility, dressing, bathing, toilet hygiene, and personal hygiene.
During a review of Resident 1’s History and Physical (H&P), dated 2/16/2025, the H&P indicated the resident is nonverbal but is awake, alert, responds yes/no appropriately to questions, and is able to move all extremities. The H&P further indicated Resident 1 was able to understand and make decisions.
During a review of Resident 1’s CP regarding risk for infection, last reviewed 6/6/2025, the CP indicated the resident was a high risk for infection with a goal to minimize and reduce the risks with interventions including cleaning and disinfection of equipment as needed.
d.2. During a review of Resident 36’s AR, the AR indicated the facility admitted the resident on 6/3/2015 and most recently admitted the resident on 7/15/2025 with diagnoses that included chronic respiratory failure, tracheostomy, dependence on respiratory ventilator, and urinary tract infection (UTI- an infection in the bladder/urinary tract).
During a review of Resident 36’s MDS, dated [DATE], the MDS indicated the resident was totally dependent on staff for mobility, dressing, bathing, toilet hygiene, and personal hygiene.
During a review of Resident 36’s H&P, dated 1/15/2024, the H&P indicated the resident did not have the capacity to understand and make decisions.
During a review of Resident 36’s CP regarding risk for infection, initiated 7/16/2025 and last reviewed 7/25/2025, the CP indicated the resident was at risk for infection due to the use of an indwelling catheter (a flexible tube placed in the bladder to drain urine) with a goal that the resident would be free from infection / UTI.
During an observation on 7/29/2025 at 11:20 a.m., observed Residents 36 and 1 awake and lying in their beds in their shared room. Observed Family Member (FM) 1 of Resident 36 sitting at Resident 36’s bedside. Observed in the shared restroom a beige colored trashcan with a lid that was covered in brown stains and a yellow substance.
During an interview on 7/29/2025 at 11:40 a.m. with Certified Nursing Assistant (CNA) 5, CNA 5 stated CNA 5 was covering while CNA 6 was on break. CNA 5 entered Residents 36 and 1s’ shared restroom and stated the trash can looked old and stained. CNA 5 stated that CNA 5 would not want a trash can like that in CNA 5’s house.
During an interview on 7/29/2025 at 11:59 a.m. with CNA 6, CNA 6 stated CNA 6 did not know what was on Residents 36 and 1s’ trash can lid, but the lid did not always look brown. CNA 6 stated CNA 6 worked on 7/28/2025 and the trashcan lid was not brown. CNA 6 stated CNA 6 did not report to maintenance or housekeeping that the trash can lid was brown.
During an interview on 7/29/2025 at 12:05 p.m. with FM 1, FM 1 stated Residents 36 and 1s’ trash can lid had been brown since 7/28/2025, but the lid did not always look that way. FM 1 did not respond when the surveyor asked how FM 1 felt about the trash can lid.
During an interview on 7/31/2025 at 2 p.m. with Housekeeper (HSK) 1, HSK 1 stated on 7/30/2025 the Housekeeping Director (HSKD) told HSK 1 to change Residents 36 an 1s’ trash can, because it was “no good”.
During an interview on 7/31/2025 at 2:10 p.m. with the HSKD, the HSKD stated Residents 36 and 1s’ trashcan look dirty and it should not have be in the residents’ bathroom. The HSKD stated it looked like somebody tried to clean the trash can lid, but they were not successful. The HSKD stated any staff that used the trashcan should have reported that it looked dirty, but they did not. The HSKD stated a dirty trashcan should not be in a resident’s room because it looked dirty and is not nice for an inside environment.
During a concurrent interview and record review on 8/1/2025 at 8:58 a.m. with the IP, the IP reviewed the facility P&P regarding infection control, homelike environment, and reviewed a photo of Residents 36 and 1s’ trash can lid from 7/29/2025. The IP stated the trashcan lid looked filthy and there were yellow areas that appeared to be feces. The IP stated any nurse, or housekeeper should have reported the trashcan, but they did not. The IP stated a dirty trashcan, with possible feces on it, should not be in a resident’s room because there is a potential for cross contamination resulting in infection in the residents with e coli (a bacterium that is commonly found in the gut of humans that can cause infections). The IP stated the facility P&P regarding infection control and homelike environment was not followed because the trashcan was not sanitary.
During a concurrent interview and record review on 8/1/2025 at 2:05 p.m. with the ADON, the ADON reviewed the facility P&P regarding infection control, homelike environment, and reviewed a photo of Residents 36 and 1s’ trashcan lid from 7/29/2025. The ADON stated the facility P&Ps were not followed when the trashcan did not look clean and could potentially lead to infections in residents.
During a review of the untitled facility P&P regarding Housekeeping, last reviewed 4/24/2025, the P&P indicated in order to ensure the health and safety of residents, staff and visitors, it is critical that the facility be kept clean, sanitary, and in good repair at all times. Proper and safe methods for cleaning, disinfecting, and sterilizing all areas, surfaces, and equipment shall be employed in the facility as required by law. All rooms of the facility shall be kept clean and as free as possible of germs and other contaminating agents at all times, while maintaining a pleasant and home-like atmosphere for the residents. The facility shall acquire and properly maintain all necessary housekeeping equipment to ensure the proper cleaning of the facility. General duties of the housekeeping staff are to make sure that each room, area, piece of furniture, or equipment is cleaned properly and thoroughly with the correct equipment and cleaning product.
e. During a review of Resident 12’s AR, the AR indicated the facility admitted the resident on 5/14/2024 with diagnoses including tracheostomy (a surgical opening in the neck into the windpipe when a person is unable to breathe thru the nose or mouth), urinary tract infection (UTI- an infection in the bladder/urinary tract), and generalized muscle weakness.
During a review of Resident 12’s H&P, dated 3/26/2025, the H&P indicated Resident 12 did not have the capacity to understand and make decisions.
During a review of Resident 12’s MDS, dated [DATE], the MDS indicated Resident 12 had severely impaired cognition (mental action or process of acquiring knowledge and understanding) and unable to understand and make his needs known. The MDS further indicated Resident 12 required total assistance from staff with tub/shower transfers; supervision or touching assistance with bed mobility; partial/moderate assistance to substantial/maximal assistance with all other activities of daily living (ADLs - basic tasks that must be accomplished every day for an individual to thrive). The MDS
During a review of Resident 12’s Order Summary Report dated 8/1/2025, the Order Summary Report indicated the following physician’s order:
-3/26/2025: Enhance barrier precaution due to presence of gastrostomy (GT - a surgical opening fitted with a device to allow feedings to be administered directly to the stomach common for people with swallowing problems), ostomy (a surgical procedure that creates an opening in the body for the elimination of waste), tracheostomy. [NAME] (put on) personal protective equipment (PPE - clothing and equipment that is worn or used to provide protection against hazardous substances and/or environments)/gown when providing direct patient care.
During a review of Resident 12’s care plan (CP) titled “Enhanced Barrier Precaution,” high risk for infection initiated on 3/26/2025, the CP indicated to observe EBP and use gloves, gowns, and masks to reduce risk for active infection.
During a concurrent observation and interview on 7/29/2025 at 9:42 a.m., inside Resident 12’s room, observed Licensed Vocational Nurse (LVN) 4, reposition Resident 12 with Respiratory Therapist (RT) 1, who was wearing PPEs. Observed LVN 4, who was wearing a mask put on gloves after performing hand hygiene using a hand sanitizer but did not don a gown when repositioning the resident in the bed. LVN 4 stated she did not don a gown while repositioning Resident 12 and the resident was on EBP due to the presence of GT and tracheostomy as indicated by the EBP sign at the door. LVN 4 stated repositioning Resident 12 in bed can be considered a direct patient care and she should have donned a gown while repositioning the resident. LVN 4 stated not wearing the proper PPE during direct patient care of vulnerable residents such as Resident 12 placed the resident at risk for acquiring infection from other sources.
During a concurrent observation and interview on 7/29/2025 at 11:30 a.m. outside Resident 12’s room with Registered Nurse (RN) 4, RN 4 stated Resident 12 had a sign outside the room for EBP and lists the type of care that required putting on PPE. RN 4 stated the staff are supposed to wear gowns, gloves, and masks during high contact activities which include repositioning the residents on EBP. RN 4 stated Resident 12 has GT and tracheostomy, and LVN 4 should have put on a gown after using hand sanitizer and putting on gloves prior to repositioning Resident 12 to prevent the spread of infection to other vulnerable residents and Resident 12 acquiring infection from other sources.
During an interview on 8/1/2025 at 8:54 a.m. with the Infection Preventionist (IP), the IP stated if a resident has a sign outside the door for EBP, the staff should perform hand hygiene, put on gloves, gowns, and masks prior to entering the room and performing direct patient care to residents with GT and tracheostomy which includes repositioning the resident in bed. The IP stated Resident 12 had GT and tracheostomy and LVN 4 should have put on a gown when repositioning Resident with RT 1. The IP stated if LVN 4 did not put on a gown, it placed Resident 12 and other vulnerable residents at risk for acquiring infection due to possible spread of infection in between residents, staff, and/or visitors.
During a review of the facility’s policy and procedure (P&P) titled, “Enhanced Barrier Precautions,” last reviewed on 4/24/2025, the P&P indicated:
-EBP's are utilized to prevent the spread of multidrug resistant organisms (MDRO's - germs, usually bacteria that have become resistant to multiple antibiotics making it difficult to treat with standard medications) to residents.
-EBPs are used as an infection prevention and control intervention to reduce the spread of MDROs to residents.
-EBPs employ targeted gown and glove use during high contact resident care activities when contact precautions do not otherwise apply.
a. gloves and gowns are applied prior to performing the high contact resident care activity (as opposed to before entering the room).
PPE is changed before caring for another resident.
Face protection may be used if there is also a risk of splashes or spray.
Examples of high contact activities requiring the use of gowns and gloves for EBPs include transferring.
EBPs are indicated for residents with wounds and/or indwelling medical devices regardless of MDRO colonization (presence of organism in the body but without causing a disease)
Colonized residents are at risk of developing invasive infections and clinical diseases and can transmit to other residents.
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0638
(Tag F0638)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to complete the Quarterly Minimum Data Set (MDS-a resident assessment...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to complete the Quarterly Minimum Data Set (MDS-a resident assessment tool) Assessment timely for one of two sampled residents (Resident 76) reviewed under the Resident Assessment task. This deficient practice had the potential to negatively affect the provision of necessary care and services needed Resident 76. Findings:During a review of Resident 76's admission Record, the admission Record indicated the facility originally admitted the resident on 1/15/2025 and readmitted on [DATE] with diagnoses including urinary tract infection (UTI- an infection in the bladder/urinary tract), generalized muscle weakness, and dysphagia (difficulty swallowing). During a concurrent interview and record review on 7/31/2025 at 3:40 p.m. with the Director of MDS (DMDS), reviewed Resident 76's MDS Assessments and the Centers of Medicare and Medicaid Services (CMS-a federal agency that administers major healthcare programs) Final Validation Reports (FVR-facility's documentation of successful MDS file submission), the MDS Assessments and the CMS' FVR indicated: - Quarterly MDS, Assessment Reference Date (ARD-observation end date) 4/24/2025; CMS FVR submitted date 5/8/2025, completed late. DMDS stated it should have been completed within 92 days, and it was submitted on the 93rd day on 5/8/2025. During an interview on 7/31/2025 at 4:01 p.m. with the DMDS stated she uses the MDS Scheduler to keep track of when the residents' MDS Assessments are due. The DMDS stated the purpose of completing the MDS Assessments timely is to make sure they have a quarterly review done and if the resident had any change in condition or significant change in condition that they need new care plans to implement. The DMDS stated the MDS Assessments would also show warnings of when they are late or overdue. The DMDS stated when the MDS Assessments are completed and/or submitted late can result in a delay of care especially if the resident had significant change in condition. The DMDS stated this information is transmitted (submitted) to CMS and it shows the facility's quality measures (standardized metrics used by CMS to evaluate quality, safety, and efficiency) that are being updated monthly and made available to the public. During an interview on 8/1/2025 at 3:53 p.m. with the Director of Nursing (DON), the DON stated that MDS Assessments should be submitted according to timeframes. The DON stated this is done for accuracy, completed timely, and for billing purposes. The DON stated when MDS Assessments are completed and/or submitted late there is potential for missed interventions in the resident's care plan and could miss the type of care the resident needs. During a review of the facility's policy and procedures (P&P) titled, MDS Completion and Submission Timeframes, dated 4/24/2025, the P&P indicated that the facility will conduct and submit resident assessments in accordance with current and state submission timeframes. The P&P indicated that Timeframes for completion and submission of assessments is based on the current requirements published in the Resident Assessment Instrument Manual. During a review of the Centers for Medicare &Medicaid Services (CMS, a federal agency that administers major healthcare programs) Long-Term Care Facility Resident Assessment Instrument 3.0 User's Manual, dated 10/2024, the RAI manual indicated the requirement for providers to complete the Quarterly MDS Assessment of the ARD of previous Omnibus Budget Reconciliation Act of 1987 (OBRA-a federal law that sets national minimum standards of care for residents in certified nursing facilities) of any type + 92 calendar days.
MINOR
(B)
Minor Issue - procedural, no safety impact
MDS Data Transmission
(Tag F0640)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure the Minimum Data Set (MDS - a resident assessment tool) was...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure the Minimum Data Set (MDS - a resident assessment tool) was transmitted timely to the Centers for Medicare and Medicaid Services (CMS-a federal agency that administers major healthcare programs) system for one of two sampled residents (Resident 48) reviewed under Resident Assessments facility task. This deficient practice had the potential to negatively affect the provision of necessary care and services needed by Resident 48. Findings:During a review of Resident 48's admission Record, the admission Record indicated the facility originally admitted the resident on 2/5/2025 and readmitted on [DATE] with diagnoses including type two diabetes mellitus (DM-a disorder characterized by difficulty in blood sugar control and poor wound healing) with foot ulcer (a small open sore or wound generally found in the stomach or on the skin), encephalopathy (a broad term describing any disorder or disease that affects the brain's structure or function, leading to impaired brain function), and generalized muscle weakness. During a concurrent interview and record review on 7/31/2025 at 3:55 p.m. with the Director of MDS (DMDS), reviewed Resident 76's MDS Assessments and the Centers of Medicare and Medicaid Services (CMS-a federal agency that administers major healthcare programs) Final Validation Reports (FVR-facility's documentation of successful MDS file submission), the MDS Assessments and the CMS' FVR indicated: - admission MDS, Assessment Reference Date (ARD-observation end date) 2/12/2025; CMS FVR submitted date 2/26/2025, completed late. The CMS FVR indicated the assessment completed late, completion date is more than 13 days after the entry date. The DMDS stated it should have been submitted on 2/24/2025 and after this date it is late. During an interview on 7/31/2025 at 4:01 p.m. with the DMDS stated she uses the MDS Scheduler to keep track of when the residents' MDS Assessments are due. The DMDS stated the purpose completing the MDS Assessments timely is to make sure they have a quarterly review done and if the resident had any change in condition or significant change in condition that they need new care plans to implement. The DMDS stated the MDS Assessments would also show warnings of when they are late or overdue. The DMDS stated when the MDS Assessments are completed and/or submitted late can result in a delay of care especially if the resident had significant change in condition. The DMDS stated this information is transmitted (submitted) to CMS and it shows the facility's quality measures (standardized metrics used by CMS to evaluate quality, safety, and efficiency) that are being updated monthly and made available to the public. During an interview on 8/1/2025 at 3:53 p.m. with the Director of Nursing (DON), the DON stated that MDS Assessments should be submitted according to timeframes. The DON stated this is done for accuracy, completed timely, and for billing purposes. The DON stated when MDS Assessments are completed and/or submitted late there is potential for missed interventions in the resident's care plan and could miss the type of care the resident needs. During a review of the facility's policy and procedures (P&P) titled, MDS Completion and Submission Timeframes, dated 4/24/2025, the P&P indicated that the facility will conduct and submit resident assessments in accordance with current and state submission timeframes. The P&P indicated that Timeframes for completion and submission of assessments is based on the current requirements published in the Resident Assessment Instrument Manual. During a review of the Centers for Medicare &Medicaid Services (CMS, a federal agency that administers major healthcare programs) Long-Term Care Facility Resident Assessment Instrument 3.0 User's Manual, dated 10/2024, the RAI manual indicated the requirement for providers to complete the admission Assessment 14th calendar day of the resident's admission (admission date + 13 calendar days).