ASISTENCIA VILLA HEALTHCARE CENTER


Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Asistencia Villa Healthcare Center has a Trust Grade of C, which means it is considered average, sitting in the middle of the pack among nursing homes. In terms of rankings, it is #526 out of 1,155 facilities in California, placing it in the top half, and #39 out of 54 in San Bernardino County, indicating that only a few local options are rated higher. The facility shows an improving trend, having reduced its issues from 10 in 2024 to just 3 in 2025. However, staffing is a concern with a poor rating of 1 out of 5 stars and a high turnover rate of 55%. Additionally, the center has faced some serious incidents, including a resident sustaining abrasions due to unsafe mobility equipment during transfer and concerns over food safety standards, such as improper kitchen sanitation and staff not adhering to food service safety protocols, which could potentially expose residents to health risks. Overall, while there are strengths in the facility's recent trends, these serious incidents and staffing issues are important factors for families to consider.
- Trust Score
- C
- In California
- #526/1155
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 55% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $10,033 in fines. Higher than 73% of California facilities. Some compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 34 minutes of Registered Nurse (RN) attention daily — about average for California. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 47 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Near California average (3.1)
Meets federal standards, typical of most facilities
Near California avg (46%)
Higher turnover may affect care consistency
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 47 deficiencies on record
Jul 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure blood pressure medication was not administered in duplicated...
Read full inspector narrative →
Apr 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide the necessary care and services to ensure resi...
Read full inspector narrative →
Jan 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on observation, interviews, and record reviews, the facility failed to follow its policy and procedure regarding medicati...
Read full inspector narrative →
Oct 2024
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on the observation, interview and record review, the facility failed to ensure a Significant Change of Status Assessments ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure Minimum Data Set (MDS- a computerized assessment instrument)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on the observation, interview and record review, the facility failed to store all drugs and biological in accordance with currently accepted professional principles and the facility's policies a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to implement its policy and procedure on antibiotic stewardship (a s...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to implement their infection control program to help prevent the spread of COVID-19 (Corona Virus Disease, a highly infectious d...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record review, the facility failed to ensure their equipment was maintained in safe operating condition when:
The countertop water dispenser was found leaking an...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record review, the facility failed to maintain a sanitary kitchen when:
1. There was a cabinet that stored a juice dispenser, the door to the cabinet had a stick...
Read full inspector narrative →
Jul 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow their policy and procedure to ensure the remov...
Read full inspector narrative →
Jun 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow policy and procedure to ensure the call lights...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure adequate supervision was provided to prevent a...
Read full inspector narrative →
Dec 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure one of three clinically compromised residents (Resident 2) was provided transportation for her medical appointment.
This failure had ...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain a comfortable and homelike environment for o...
Read full inspector narrative →
Aug 2023
12 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure all mobility equipment was safe to be used on ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. During a review of Resident 10's Face Sheet, indicated, Resident 10 was admitted to the facility on [DATE], with diagnoses th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of eight sampled resident (Resident 505), ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to develop a care plan for a resident with an identified...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to follow their policy and procedure when the SBAR (Situation, Backgr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide essential services to increase range of motio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain acceptable parameters of nutrition status fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure safe medication administration to meet the needs of one of seven residents, (Resident 41), when Resident 41 was provide...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During a concurrent observation and interview on August 8, 2023 at 8:36 AM with CNA 7 and CNA 8 for Clostridium Difficile (C....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to follow the approved menus when:
1. Residents on CCHO (Consistent Carbohydrate diet, diet for diabetic residents, residents wh...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to maintain kitchen equipment in operating condition when three pieces of equipment (steamer, convection oven, and industrial mi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to maintain professional standards for food service safety when the [NAME] (Cook 2) was not wearing a facial hair restraint whil...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a medication was administered and or prescribed for a curren...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide a mattress that fit the bedframe for one of three sampled residents (Resident 1). Resident 1 fell to the floor requiring a transfer...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to follow their Policy. The licensed nurses failed to monitor percentage of food eaten daily and did not notify M.D. which resulted in delayed ...
Read full inspector narrative →
Apr 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to follow policy and procedure to provide Activities of D...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure one of 3 sampled residents (Resident 1) was properly assess...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure adequate supervision/assistance was provided t...
Read full inspector narrative →
Jun 2021
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide personal privacy to one of 20 sampled residents (Resident 425) when she removed her lap blanket exposing her soiled, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that a level II PASRR (Pre admission Screening And Resident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure that one of twenty sampled Residents (Resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to administer enteral tube feeding, (a tube placed int...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the humidification bottle (sterile water used ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to communicate with the Dialysis Center for one of 19 sa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure safe and accurate pharmaceutical services in a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure drugs and biologicals were labeled in accordance with currently accepted standards of practice when:.
1. The contracte...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility staff failed to serve one of 19 sampled residents (Resident 64) food that was w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to assist family and visitors to understand safe food handling practices (such as safe cooling/reheating processes, hot/cold holding temperat...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure proper disposal of garbage and refuse when one of three lids on garbage receptacles, was not fully closed and there wa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to recognize, evaluate and address the needs of seven of...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure safe and sanitary food preparation and storage practices in the kitchen when:
1. There was food debris and dead insect...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to implement their infection control program by not fo...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • 47 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $10,033 in fines. Above average for California. Some compliance problems on record.
- • Grade C (53/100). Below average facility with significant concerns.
About This Facility
What is Asistencia Villa Healthcare Center's CMS Rating?
CMS assigns ASISTENCIA VILLA HEALTHCARE CENTER an overall rating of 3 out of 5 stars, which is considered average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Asistencia Villa Healthcare Center Staffed?
CMS rates ASISTENCIA VILLA HEALTHCARE CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 55%, compared to the California average of 46%. RN turnover specifically is 67%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Asistencia Villa Healthcare Center?
State health inspectors documented 47 deficiencies at ASISTENCIA VILLA HEALTHCARE CENTER during 2021 to 2025. These included: 1 that caused actual resident harm and 46 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Asistencia Villa Healthcare Center?
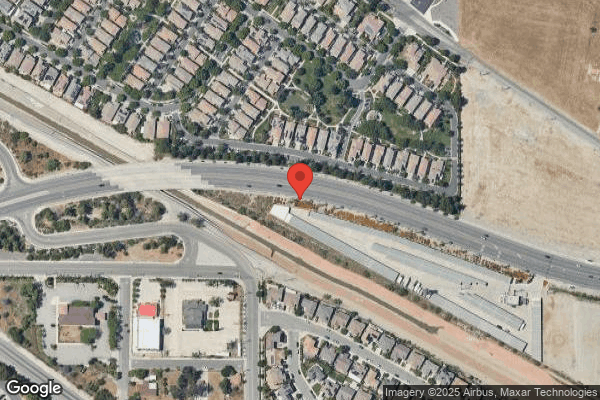
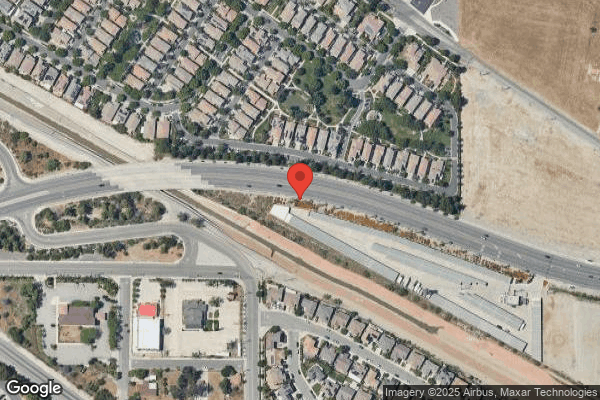
ASISTENCIA VILLA HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by P&M MANAGEMENT, a chain that manages multiple nursing homes. With 99 certified beds and approximately 91 residents (about 92% occupancy), it is a smaller facility located in REDLANDS, California.
How Does Asistencia Villa Healthcare Center Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, ASISTENCIA VILLA HEALTHCARE CENTER's overall rating (3 stars) is below the state average of 3.1, staff turnover (55%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Asistencia Villa Healthcare Center?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Asistencia Villa Healthcare Center Safe?
Based on CMS inspection data, ASISTENCIA VILLA HEALTHCARE CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Asistencia Villa Healthcare Center Stick Around?
ASISTENCIA VILLA HEALTHCARE CENTER has a staff turnover rate of 55%, which is 9 percentage points above the California average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Asistencia Villa Healthcare Center Ever Fined?
ASISTENCIA VILLA HEALTHCARE CENTER has been fined $10,033 across 1 penalty action. This is below the California average of $33,179. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Asistencia Villa Healthcare Center on Any Federal Watch List?
ASISTENCIA VILLA HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.